Abstract
Introduction
Clinical trials have demonstrated that treatment-to-target (T2T) is effective in achieving remission in early rheumatoid arthritis (RA). However, the concept of T2T has not been fully implemented yet and the question is whether a T2T strategy is feasible in daily clinical practice. The objective of the study was to evaluate the adherence to a T2T strategy aiming at remission (Disease Activity Score in 28 joints (DAS28) < 2.6) in early RA in daily practice. The recommendations regarding T2T included regular assessment of the DAS28 and advice regarding DAS28-driven treatment adjustments.
Methods
A medical chart review was performed among a random sample of 100 RA patients of the DREAM remission induction cohort. At all scheduled visits, it was determined whether the clinical decisions were compliant to the T2T recommendations.
Results
The 100 patients contributed to a total of 1,115 visits. The DAS28 was available in 97.9% (1,092/1,115) of the visits, of which the DAS28 was assessed at a frequency of at least every three months in 88.3% (964/1,092). Adherence to the treatment advice was observed in 69.3% (757/1,092) of the visits. In case of non-adherence when remission was present (19.5%, 108/553), most frequently medication was tapered off or discontinued when it should have been continued (7.2%, 40/553) or treatment was continued when it should have been tapered off or discontinued (6.2%, 34/553). In case of non-adherence when remission was absent (42.1%, 227/539), most frequently medication was not intensified when an intensification step should have been taken (34.9%, 188/539). The main reason for non-adherence was discordance between disease activity status according to the rheumatologist and DAS28.
Conclusions
The recommendations regarding T2T were successfully implemented and high adherence was observed. This demonstrates that a T2T strategy is feasible in RA in daily clinical practice.
Similar content being viewed by others
Introduction
New insights into the treatment of rheumatoid arthritis (RA) have led to better care for RA patients, thereby strongly improving outcome [1, 2]. Herewith, clinical remission has become the ultimate therapeutic goal in RA [3]. Several studies have demonstrated that a treatment approach including tight control of disease activity is more effective in lowering disease activity and, ultimately, reaching remission, compared with usual care [4–8]. The major keystones of such a treat-to-target (T2T) strategy are: 1) regular assessment of the disease activity using a validated outcome measure, 2) subsequent adjustments of treatment in case of persistent disease activity, preferably following a medication protocol where therapeutic consequences are predefined [9], and 3) aiming at a predefined target.
Current recommendations and guidelines on the management of RA address the importance of treating RA to a target of remission or low disease activity [3, 10]. In this context, the European League Against Rheumatism (EULAR) has formulated a set of 10 international recommendations on how to achieve optimal outcomes of RA by providing guidance for T2T [11]. Although the rheumatology community worldwide endorses the importance of T2T [12], a lack of compliance with this issue is presumed in daily clinical practice. It is assumed that disease activity is not consistently measured by validated measures and medication is often not intensified or changed when disease is active in the routine care setting [6, 13–15].
The implementation of guidelines and the translation of beneficial results of clinical trials to daily clinical practice are considered to be difficult [16–19]. The question is whether a T2T strategy, including protocolized treatment adjustments will be feasible in a real-life setting, which is characterized by a more heterogeneous patient population [20], variation in prescription behavior of specialists [19, 21], and restriction of time, costs and resources.
In 2006, six of the Dutch Rheumatoid Arthritis Monitoring (DREAM) consortium hospitals implemented a T2T strategy in the so-called DREAM remission induction cohort. Four of these six hospitals successfully implemented the strategy and included at least 20 patients. Since the day of diagnosis, very early RA patients were treated according to a T2T strategy aiming at remission (defined as a Disease Activity Score in 28 joints (DAS28) < 2.6 [22]), including a treatment advice regarding subsequent DAS28-driven therapeutic steps [23]. The aim of the present study was to evaluate the adherence to these T2T recommendations. We examined whether these recommendations resulted in regular assessment of the disease activity with the DAS28 and whether medication was adapted according to the treatment advice. Moreover, we explored reasons for non-adherence to the T2T recommendations.
Materials and methods
Patients
Recommendations regarding T2T were implemented in six hospitals in The Netherlands in January 2006, as part of the DREAM remission induction cohort. Inclusion of patients into the cohort and data collection are still on-going. The cohort consists of consecutive patients newly diagnosed with RA who met the following inclusion criteria: clinical diagnosis of RA, age ≥ 18, symptom duration (defined as time from first reported symptom to diagnosis of RA by rheumatologist) of one year or less, a DAS28 ≥ 2.6, and no previous treatment with disease-modifying antirheumatic drugs (DMARDs) and/or prednisolone. Under Dutch law, this descriptive evaluation does not need approval from an ethical review board. Nonetheless, patients were fully informed, and informed consent was obtained.
For the present study, a random sample of 100 patients of the DREAM remission induction cohort was taken using the 'random sample of cases' function in SPSS. We selected patients who had a minimal follow-up of six months to ensure that every patient had at least three follow-up evaluations.
Treatment
After inclusion, visits were scheduled at weeks 8, 12, 20, 24, 36 and 52, and every three months thereafter. Patients could visit the rheumatologist in between the scheduled cohort visits when necessary. The T2T recommendations included systematic monitoring of the disease activity with the DAS28 in combination with a treatment advice regarding predefined treatment adjustments aiming at remission (defined as a DAS28 < 2.6). Therapy consisted of initial methotrexate monotherapy (MTX), followed by the addition of sulfasalazine (SSZ) in case of non-remission, and thereafter, sulfasalazine was exchanged for anti-tumor necrosis factor (TNF)-α agents in case of moderate or high disease activity (Table 1). If the target of DAS28 < 2.6 was reached, medication was not changed. In case of sustained remission (six months or more), medication was gradually tapered and eventually discontinued. The last introduced medication was tapered off first (that is, MTX was always tapered off as the last medication). The tapering steps were as follows (all lasting six months): MTX in mg/week, 25 to 15 to 7.5 to stop; SSZ in mg/day, 3,000 to 2,000 to 1,000 to stop; adalimumab 40 mg, every week to every two weeks to stop; etanercept 50 mg, every week to every two weeks to stop; infliximab 3 mg/kg, every four weeks to every eight weeks to stop. In case of a disease flare-up (DAS28 ≥ 2.6), the most recently effective medication (dosage) was reintroduced and treatment could be subsequently intensified.
Deviations from the protocol were allowed on clinical indication. In patients with a sulfa allergy, SSZ was replaced by hydroxychloroquine at 400 mg per day. Nonsteroidal anti-inflammatory drugs, prednisolone ≤ 10 mg per day and intra-articular corticosteroid injections were allowed at clinical indication. Details of the protocol were reported earlier [23]. All clinical data on patient characteristics, clinical and laboratory measures, and medication use were prospectively stored in an electronic database.
Measures
The following variables were collected at baseline: age, sex, symptom duration, fulfilment of the American College of Rheumatology (ACR) 1987 criteria for the classification of RA [24], rheumatoid factor (RF) status, anti-cyclic citrullinated peptide antibody status, C-reactive protein (CRP), patient's global assessment of pain on a 100-mm visual analogue scale (VAS), the disability index of the Dutch version of the Health Assessment Questionnaire [25, 26], and component summary scores for physical and mental health of the 36-item Short Form Health Survey [27].
At every visit, joint counts were performed by trained rheumatology nurses, erythrocyte sedimentation rate (ESR) was measured and general health was filled out on a 100-mm VAS by the patient. The nurse calculated the DAS28 score and provided this, including the values of its components, to the rheumatologist.
Remission was defined as a DAS28 < 2.6. Remission according to the provisional ACR/EULAR Boolean-based definition of remission in RA was also examined, which required a tender joint count in 28 joints (TJC28) ≤ 1, swollen joint count in 28 joints (SJC28) ≤ 1, CRP ≤ 1 mg/dl and patient global assessment (PGA, on a 0 to 10 scale) ≤ 1 [28].
Data extraction
All scheduled clinical visits were retrieved from the database and parameters for disease activity and medication were extracted. A medical chart review was performed to determine whether the clinical decisions were compliant to the above described recommendations.
Deviations from the treatment advice were classified as: not intensifying (that is, continuing/tapering off/discontinuing) instead of intensifying treatment; intensifying instead of not intensifying (that is, continuing/tapering off/discontinuing) treatment; continuing instead of tapering off/discontinuing treatment; tapering off/discontinuing instead of continuing treatment; and other deviations. We registered whether the deviations concerned conventional DMARDs or anti-TNF therapy. Possible reasons for non-adherence were retrieved from the medical chart. Medication use outside the treatment advice (including the use of prednisolone dosages > 10 mg per day) was registered.
Statistical analysis
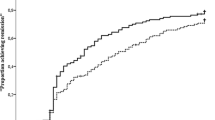
The primary outcome measures were the number of cohort visits in which the DAS28 was assessed and the number of these visits in which therapy was adapted according to the treatment advice, stratified by remission state (yes/no). The various deviations were reported as numbers with corresponding percentages. Pie charts were used to graphically present the extent to which the medication protocol was followed.
To test differences in the patient baseline characteristics between hospitals, we used independent t tests for normally distributed variables, chi-square tests for categorical variables and Mann-Whitney U tests for non-normally distributed variables.
The level of significance was set at a P-value < 0.05. Statistical analyses were performed using the statistical software package SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
Results
Study sample
The baseline characteristics of the 100 patients whose medical charts were examined are presented in Table 2. This study group reflects a normal early RA population with 61.0% of the patients being female, a mean (standard deviation, SD) age of 57.7 (15.4), 61.0% RF positivity, and a mean DAS28 (SD) of 4.9 (1.1). Patients' baseline characteristics were comparable between hospitals (data not shown), except for symptom duration which differed between two hospitals; median (interquartile range, IQR) of 10.0 (6.5 to 16.0) versus 21.0 (9.8 to 30.3) weeks, P = 0.012. The baseline characteristics of the patients who were not included in this study did not differ significantly or clinically relevantly from the random sample of patients who were included in this study (not shown).
The 100 patients contributed to a total of 1,115 visits. The mean (SD) follow-up time at the time of data collection in these patients was 28.0 (10.0) months. The mean (SD) number of cohort visits per patient was 10.9 (3.6).
Monitoring of disease activity
The DAS28 was available in 97.9% (1,092/1,115) of the scheduled cohort visits. The main reasons for the DAS28 score being missing were that the ESR was not (yet) available or the patient's general health was not assessed (data not shown). Since the level of disease activity could not be evaluated in these visits, we could not determine whether adherence to the medication protocol was accomplished. Therefore, these 23 visits (2.1%) were excluded from further analyses.
According to the T2T strategy, disease activity should be assessed using the DAS28 at least every three months. In 88.3% (964/1,092) of the visits, this recommendation was met. In the remaining 128 cases, DAS28 remission was present at the previous visit in 71.1% (91/128), and, therefore, the attending rheumatologist scheduled the next visit in six months in 93.4% (85/91) of these visits.
Adherence treatment advice
Adherence to the treatment advice was observed in 69.3% (757/1,092) of the visits. Non-adherence at least at one visit was experienced by 91.0% of patients (91/100).
Remission
Remission was present in 50.6% (553/1,092) of the visits. The treatment advice was followed in 80.5% (445/553) of these visits, that is, medication was continued or, in case of sustained remission (DAS28 < 2.6 for at least six months), tapered off or discontinued (Figure 1A). The various deviations in the non-adherence cases (19.5%, 108/553) are also depicted in Figure 1A. Most frequently, medication was tapered off or discontinued when it should have been continued according to the treatment advice (7.2%, 40/553), or treatment was continued when it should have been tapered off or discontinued (6.2%, 34/553). Furthermore, medication was intensified in 4.3% (24/553) in spite of DAS28 remission. In 9 of these 24 cases, the patient had at least one swollen joint. Other deviations were observed in 1.8% (10/553). In 12.0% (13/108) of these non-adherence cases, the deviation concerned anti-TNF therapy.
Adherence to the treatment advice of the treat-to-target strategy. The pie charts illustrate how often the treatment advice was followed in A) 553 visits in which remission (Disease Activity Score in 28 joints (DAS28) < 2.6) was present and B) 539 visits in which no remission (DAS28 ≥ 2.6) was present of 100 patients with early rheumatoid arthritis.
The reasons for non-adherence are presented in Table 3. The most frequently observed reasons for non-adherence were the presence of active disease according to the rheumatologist (that is, based on the presentation of the patient's overall disease activity, in particular, the degree of arthritis) and drug side effects.
Remission according to the provisional ACR/EULAR definition of remission was observed in 42.9% (237/524) of these visits (remission could not be evaluated in all visits due to missing values for CRP).
Non-remission
In case of non-remission, the treatment advice was followed in 57.9% (312/539) of the visits (Figure 1B), meaning that therapy was intensified. Figure 1B also shows the various deviations in case of non-adherence (42.1%, 227/539). The most frequently observed deviation was that medication was not intensified (that is, continued, tapered off or discontinued) when an intensification step should have been taken according to the treatment advice (34.9%, 188/539). Other deviations were observed in 7.2% (39/539). In 21.6% (49/227) of the non-adherence cases, the deviation concerned anti-TNF therapy.
In the non-adherence cases, disease activity was low (2.6 ≤ DAS28 ≤ 3.2) in 43.2% (98/227), moderate (3.2 < DAS28 ≤ 5.1) in 49.8% (113/227), and high (DAS28 > 5.1) in 7.0% (16/227).
Table 3 presents the reasons for non-adherence. The most frequently observed reason for deviation was that clinical remission was present according to the rheumatologist, even though the DAS28 was 2.6 or higher. In these 108 visits, the distribution of the clinical variables was as follows: median (IQR) SJC28 of 1.0 (0.0 to 3.0), median (IQR) TJC28 of 0.0 (0.0 to 3.0), mean (SD) ESR of 22.6 (14.9), and median (IQR) CRP of 5.0 (4.0 to 8.0). The mean (SD) DAS28 was 3.3 (0.7) and 54.6% (59/108) of these patients had a DAS28 ≤ 3.2. The mean (SD) scores of the patient's assessment of pain was 31.6 (21.4) and of general health 34.6 (21.1).
Non-remission according to the provisional ACR/EULAR definition of remission was observed in 94.2% (508/514) of these visits (remission could not be evaluated in all visits due to missing values for CRP).
Other medication
Disease modifying medication outside the treatment advice was prescribed in 8.0% (8/100) of the patients; 1 patient received leflunomide and 7 patients received at least one intra-muscular corticosteroid injection. Prednisolone dosages > 10 mg per day were given to 7.0% (7/100) of the patients at least at one visit.
Drug side effects
Adherence to the treatment advice was prevented by drug side effects in 71 visits. Table 4 presents the various side effects that were registered in the medical charts. If the patient experienced more than one side effect, we listed only the first reported side effect.
Discussion
This descriptive evaluation demonstrated that a T2T strategy is possible in daily clinical practice. The recommendations regarding T2T were successfully implemented in the participating rheumatology clinics of the DREAM remission induction cohort. Disease activity was regularly and systematically measured using the DAS28 and adherence to the treatment advice was high. In case of non-adherence to the recommendations, valid arguments for deviating were observed in the majority of these cases.
Real-life observational data regarding the adherence to a T2T strategy in daily clinical practice were analyzed. These are valuable data because T2T strategies are often conducted in the setting of randomized controlled trials (RCTs), which entails a more controlled environment compared to routine care. This was a retrospective evaluation and, therefore, the attending physicians were not influenced by the goal of this analysis.
The successful implementation of T2T in the DREAM hospitals can be explained by several factors. First, the evidence from RCTs and, subsequently, the fact that current guidelines and recommendations underline the importance of T2T has raised rheumatologists' awareness about the effectiveness of T2T. Second, the recommendations regarding the frequency of monitoring and the therapeutic regimen in the present study were fit in as close as possible with the conventional management of RA in daily clinical practice. Prior to the implementation of T2T, consensus was reached on the recommendations by all rheumatologists of the participating hospitals. Third, the organization of care was arranged as such that the treatment approach did not require extra effort and time from the rheumatologist during the clinical visit. Prior to the visit to the rheumatologist, RA disease activity according to the DAS28 was evaluated by a trained rheumatology nurse. The rheumatology nurses take part in annual DAS28 training sessions, which guarantee the uniformity of the DAS28 assessment. A previous study by Van Hulst et al. suggests that nurse-led care, including DAS28 measurement, may be helpful in making DAS28 assessments more feasible for daily clinical practice settings [13]. Furthermore, general practitioners are aware of the importance of early referral of patients with symptoms of arthritis to the rheumatologist, thereby making an early diagnosis possible.
At a percentage of 69%, the observed level of adherence to the T2T recommendations was probably optimal, as striving for 100% adherence is not realistic because treatment of patients is subject to side effects and comorbidities. Moreover, it is obvious that patients are involved in their treatment decision making process. Previous studies have shown that discordance exists between the patients' and rheumatologists' rating of disease activity [29, 30] and that they approach the decision to intensify medication differently [31, 32]. Moreover, patients may be reluctant to change medications frequently and fear side effects. In the present study, the main reason for non-adherence was discordance between disease activity status according to the rheumatologist and the DAS28, which might be explained by properties of the DAS28 algorithm. The feet are omitted in the DAS28; however, disease activity in the foot joints is frequently observed in RA, even in patients who are considered to be in DAS28 remission [33]. This among other factors has led to the debate of whether the cut-off point for DAS28 remission reflects true clinical remission [34, 35]. In the therapeutic decision making, rheumatologists do not always rely solely on the DAS28 [36], but also other markers of inflammation and/or progression [31, 37] and patients' characteristics [38] are taken into account. The DAS28 is suggested to be a tool to guide decision making in RA; nevertheless, it cannot always replace the clinical judgement in the context of an individual patient. Therefore, T2T should be performed with thoughtful consideration.
This study has some drawbacks. First, adherence to the recommendations of the T2T strategy was evaluated in only 100 patients of the total cohort, which includes more than 700 patients at the time of data collection. However, a random sample was taken which we believe was representative for the total cohort. Second, it was not explicitly requested to report the reason for protocol deviations, and, therefore, not all reasons could be retrieved. Third, this T2T strategy reflects the effects of only one medication strategy; no other treatment strategies were included. Several therapeutic regimes and treatment approaches have been introduced over the last decade, but the most optimal strategy for patients newly diagnosed with RA remains undecided. Moreover, after the initiation of the DREAM remission induction cohort, it emerged that the dose increase of anti-TNF therapy might have limited effectiveness [39] and also the effectiveness of a third anti-TNF agent in case of failure of two previous anti-TNF agents has been debated. This might have led to deviations from the advised anti-TNF therapy steps. Fourth, it was not investigated whether failure to be adherent to the strategy had any impact on whether patients achieved remission.
Conclusions
In conclusion, this study showed that the implementation of T2T is feasible in very early RA in daily clinical practice. We demonstrated a high adherence to the T2T recommendations, which comprised regular assessment of the DAS28 and treatment advice regarding subsequent DAS28-driven therapeutic steps.
Abbreviations
- ACR:
-
American College of Rheumatology
- Anti-CCP:
-
anti-cyclic citrullinated peptide
- Anti-TNF:
-
anti-tumor necrosis factor
- CRP:
-
C-reactive protein
- DAS28:
-
Disease Activity Score in 28 joints
- DMARDs:
-
disease-modifying antirheumatic drugs
- DREAM:
-
Dutch Rheumatoid Arthritis Monitoring
- ESR:
-
erythrocyte sedimentation rate
- EULAR:
-
European League Against Rheumatism
- HAQ:
-
Health Assessment Questionnaire
- IQR:
-
interquartile range
- MCS:
-
mental component summary
- MTX:
-
methotrexate
- PCS:
-
physical component summary
- PGA:
-
patient global assessment
- RA:
-
rheumatoid arthritis
- RCTs:
-
randomized controlled trials
- RF:
-
rheumatoid factor
- SD:
-
standard deviation
- SF-36:
-
Short-Form 36 health survey
- SJC28:
-
swollen joint count in 28 joints
- SSZ:
-
sulfasalazine
- T2T:
-
treat-to-target
- TJC28:
-
tender joint count in 28 joints
- TNF:
-
tumor necrosis factor
- VAS:
-
visual analogue scale.
References
Klarenbeek NB, Allaart CF, Kerstens PJ, Huizinga TW, Dijkmans BA: The BeSt story: on strategy trials in rheumatoid arthritis. Curr Opin Rheumatol. 2009, 21: 291-298. 10.1097/BOR.0b013e32832a2f1c.
McInnes IB, O'Dell JR: State-of-the-art: rheumatoid arthritis. Ann Rheum Dis. 2010, 69: 1898-1906. 10.1136/ard.2010.134684.
Smolen JS, Landewé R, Breedveld FC, Dougados M, Emery P, Gaujoux-Viala C, Gorter S, Knevel R, Nam J, Schoels M, Aletaha D, Buch M, Gossec L, Huizinga T, Bijlsma JW, Burmester G, Combe B, Cutolo M, Gabay C, Gomez-Reino J, Kouloumas M, Kvien TK, Martin-Mola E, McInnes I, Pavelka K, van Riel P, Scholte M, Scott DL, Sokka T, Valesini G, et al: EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs. Ann Rheum Dis. 2010, 69: 964-975. 10.1136/ard.2009.126532.
Grigor C, Capell H, Stirling A, McMahon AD, Lock P, Vallance R, Kincaid W, Porter D: Effect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomised controlled trial. Lancet. 2004, 364: 263-269. 10.1016/S0140-6736(04)16676-2.
Verstappen SM, Jacobs JW, van der Veen MJ, Heurkens AH, Schenk Y, ter Borg EJ, Blaauw AA, Bijlsma JW: Intensive treatment with methotrexate in early rheumatoid arthritis: aiming for remission. Computer Assisted Management in Early Rheumatoid Arthritis (CAMERA, an open-label strategy trial). Ann Rheum Dis. 2007, 66: 1443-1449. 10.1136/ard.2007.071092.
Fransen J, Moens HB, Speyer I, van Riel PL: Effectiveness of systematic monitoring of rheumatoid arthritis disease activity in daily practice: a multicentre, cluster randomised controlled trial. Ann Rheum Dis. 2005, 64: 1294-1298. 10.1136/ard.2004.030924.
Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Kerstens PJ, Nielen MM, Vos K, van Schaardenburg D, Speyer I, Seys PE, Breedveld FC, Allaart CF, Dijkmans BA: DAS-driven therapy versus routine care in patients with recent-onset active rheumatoid arthritis. Ann Rheum Dis. 2010, 69: 65-69. 10.1136/ard.2008.097683.
Schipper L, Vermeer M, Kuper H, Hoekstra M, Haagsma C, den Broeder A, van Riel P, Fransen F, van de Laar M: A tight control treatment strategy aiming for remission in early rheumatoid arthritis is more effective than usual care treatment in daily clinical practice: a study of two cohorts in the Dutch Rheumatoid Arthritis Monitoring (DREAM) registry. Ann Rheum Dis. 2012, 71: 845-850. 10.1136/annrheumdis-2011-200274.
Schipper LG, van Hulst LT, Grol R, van Riel PL, Hulscher ME, Fransen J: Meta-analysis of tight control strategies in rheumatoid arthritis: protocolized treatment has additional value with respect to the clinical outcome. Rheumatology (Oxford). 2010, 49: 2154-2164. 10.1093/rheumatology/keq195.
American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines: Guidelines for the management of rheumatoid arthritis: 2002 Update. Arthritis Rheum. 2002, 46: 328-346.
Smolen JS, Aletaha D, Bijlsma JW, Breedveld FC, Boumpas D, Burmester G, Combe B, Cutolo M, de Wit M, Dougados M, Emery P, Gibofsky A, Gomez-Reino JJ, Haraoui B, Kalden J, Keystone EC, Kvien TK, McInnes I, Martin-Mola E, Montecucco C, Schoels M, van der Heijde D, T2T Expert Committee: Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis. 2010, 69: 631-637. 10.1136/ard.2009.123919.
Haraoui B, Smolen JS, Aletaha D, Breedveld FC, Burmester G, Codreanu C, Da Silva JP, de Wit M, Dougados M, Durez P, Emery P, Fonseca JE, Gibofsky A, Gomez-Reino J, Graninger W, Hamuryudan V, Jannaut Peña MJ, Kalden J, Kvien TK, Laurindo I, Martin-Mola E, Montecucco C, Santos Moreno P, Pavelka K, Poor G, Cardiel MH, Stanislawska-Biernat E, Takeuchi T, van der Heijde D, Treat to Target Taskforce: Treating Rheumatoid Arthritis to Target: multinational recommendations assessment questionnaire. Ann Rheum Dis. 2011, 70: 1999-2002. 10.1136/ard.2011.154179.
van Hulst LT, Creemers MC, Fransen J, Li LC, Grol R, Hulscher ME, van Riel PL: How to improve DAS28 use in daily clinical practice?--a pilot study of a nurse-led intervention. Rheumatology (Oxford). 2010, 49: 741-748. 10.1093/rheumatology/kep407.
Littlejohn G, Tymms KE: Multi-centre, observational study shows high proportion of Australian rheumatoid arthritis patients have inadequate disease control. Arthritis Rheum. 2010, 62 (Suppl 10): 320-
Tymms K, Littlejohn G: The MDA study - a multi-centre, cross-sectional, study of barriers to optimal control for rheumatoid arthritis patients with moderate and high disease activity. Ann Rheum Dis. 2011, 70 (Suppl 3): 76-
Lacaille D, Anis AH, Guh DP, Esdaile JM: Gaps in care for rheumatoid arthritis: a population study. Arthritis Rheum. 2005, 53: 241-248. 10.1002/art.21077.
Kievit W, Fransen J, Oerlemans AJ, Kuper HH, van der Laar MA, de Rooij DJ, De Gendt CM, Ronday KH, Jansen TL, van Oijen PC, Brus HL, Adang EM, van Riel PL: The efficacy of anti-TNF in rheumatoid arthritis, a comparison between randomised controlled trials and clinical practice. Ann Rheum Dis. 2007, 66: 1473-1478. 10.1136/ard.2007.072447.
Verschueren P, Westhovens R: Optimal care for early RA patients: the challenge of translating scientific data into clinical practice. Rheumatology (Oxford). 2011, 50: 1194-1200. 10.1093/rheumatology/ker131.
Harrold LR, Harrington JT, Curtis JR, Furst DE, Bentley MJ, Shan Y, Reed G, Kremer J, Greenberg JD: Prescribing practices in a US cohort of rheumatoid arthritis patients before and after publication of the American College of Rheumatology treatment recommendations. Arthritis Rheum. 2012, 64: 630-638. 10.1002/art.33380.
Sokka T, Pincus T: Most patients receiving routine care for rheumatoid arthritis in 2001 did not meet inclusion criteria for most recent clinical trials or American College of Rheumatology criteria for remission. J Rheumatol. 2003, 30: 1138-1146.
Hoekstra M, van de Laar MA, Bernelot Moens HJ, Kruijsen MW, Haagsma CJ: Longterm observational study of methotrexate use in a Dutch cohort of 1022 patients with rheumatoid arthritis. J Rheumatol. 2003, 30: 2325-2329.
Prevoo ML, van 't Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL: Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995, 38: 44-48. 10.1002/art.1780380107.
Vermeer M, Kuper HH, Hoekstra M, Haagsma CJ, Posthumus MD, Brus HL, van Riel PL, van de Laar MA: Implementation of a treat-to-target strategy in very early rheumatoid arthritis: results of the Dutch Rheumatoid Arthritis Monitoring remission induction cohort study. Arthritis Rheum. 2011, 63: 2865-2872. 10.1002/art.30494.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, et al: The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-324. 10.1002/art.1780310302.
Fries JF, Spitz P, Kraines RG, Holman HR: Measurement of patient outcome in arthritis. Arthritis Rheum. 1980, 23: 137-145. 10.1002/art.1780230202.
Siegert CE, Vleming LJ, Vandenbroucke JP, Cats A: Measurement of disability in Dutch rheumatoid arthritis patients. Clin Rheumatol. 1984, 3: 305-309. 10.1007/BF02032335.
Ware JE, Sherbourne CD: The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992, 30: 473-483. 10.1097/00005650-199206000-00002.
Felson DT, Smolen JS, Wells G, Zhang B, van Tuyl LH, Funovits J, Aletaha D, Allaart CF, Bathon J, Bombardieri S, Brooks P, Brown A, Matucci-Cerinic M, Choi H, Combe B, de Wit M, Dougados M, Emery P, Furst D, Gomez-Reino J, Hawker G, Keystone E, Khanna D, Kirwan J, Kvien TK, Landewé R, Listing J, Michaud K, Martin-Mola E, Montie P, et al: American College of Rheumatology/European League against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Ann Rheum Dis. 2011, 70: 404-413. 10.1136/ard.2011.149765.
Barton JL, Imboden J, Graf J, Glidden D, Yelin EH, Schillinger D: Patient-physician discordance in assessments of global disease severity in rheumatoid arthritis. Arthritis Care Res (Hoboken). 2010, 62: 857-864. 10.1002/acr.20132.
Khan NA, Spencer HJ, Abda E, Aggarwal A, Alten R, Ancuta C, Andersone D, Bergman M, Craig-Muller J, Detert J, Georgescu L, Gossec L, Hamoud H, Jacobs JW, Laurindo IM, Majdan M, Naranjo A, Pandya S, Pohl C, Schett G, Selim ZI, Toloza S, Yamanaka H, Sokka T: Determinants of discordance in patients' and physicians' rating of rheumatoid arthritis disease activity. Arthritis Care Res (Hoboken). 2012, 64: 206-214. 10.1002/acr.20685.
van Hulst LT, Kievit W, van Bommel R, van Riel PL, Fraenkel L: Rheumatoid arthritis patients and rheumatologists approach the decision to escalate care differently: results of a maximum difference scaling experiment. Arthritis Care Res (Hoboken). 2011, 63: 1407-1414. 10.1002/acr.20551.
Wolfe F, Michaud K: Resistance of rheumatoid arthritis patients to changing therapy: discordance between disease activity and patients' treatment choices. Arthritis Rheum. 2007, 56: 2135-2142. 10.1002/art.22719.
van der Leeden M, Steultjens MP, van Schaardenburg D, Dekker J: Forefoot disease activity in rheumatoid arthritis patients in remission: results of a cohort study. Arthritis Res Ther. 2010, 12: R3-10.1186/ar2901.
Makinen H, Kautiainen H, Hannonen P, Sokka T: Is DAS28 an appropriate tool to assess remission in rheumatoid arthritis?. Ann Rheum Dis. 2005, 64: 1410-1413. 10.1136/ard.2005.037333.
Landewe R, van der Heijde D, van der Linden S, Boers M: Twenty-eight-joint counts invalidate the DAS28 remission definition owing to the omission of the lower extremity joints: a comparison with the original DAS remission. Ann Rheum Dis. 2006, 65: 637-641. 10.1136/ard.2005.039859.
Taylor WJ, Harrison AA, Highton J, Chapman P, Stamp L, Dockerty J, McQueen F, Jones PB, Ching D, Porter D, Rajapakse C, Rudge SR, Taylor G, Kumar S, Macedo T, Hoy MS: Disease Activity Score 28-ESR bears a similar relationship to treatment decisions across different rheumatologists, but misclassification is too frequent to replace physician judgement. Rheumatology (Oxford). 2008, 47: 514-518.
Lindsay K, Ibrahim G, Sokoll K, Tripathi M, Melsom RD, Helliwell PS: The composite DAS Score is impractical to use in daily practice: evidence that physicians use the objective component of the DAS in decision making. J Clin Rheumatol. 2009, 15: 223-225. 10.1097/RHU.0b013e3181b126b1.
Kievit W, van Hulst L, van Riel P, Fraenkel L: Factors that influence rheumatologists' decisions to escalate care in rheumatoid arthritis: results from a choice-based conjoint analysis. Arthritis Care Res (Hoboken). 2010, 62: 842-847. 10.1002/acr.20123.
Blom M, Kievit W, Kuper HH, Jansen TL, Visser H, den Broeder AA, Brus HL, van de Laar MA, van Riel PL: Frequency and effectiveness of dose increase of adalimumab, etanercept, and infliximab in daily clinical practice. Arthritis Care Res (Hoboken). 2010, 62: 1335-1341. 10.1002/acr.20211.
Acknowledgements
We would like to thank all patients, rheumatology nurses, and rheumatologists who participated in this study.
An unrestricted educational grant was provided by Abbott, The Netherlands, which was used to support MV.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MV contributed to the design of the study, data collection, analysis and interpretation, and drafted the manuscript. HHK contributed to the design of the study, data collection and interpretation, and drafted the manuscript. HJBM, MH and MDH contributed to data collection and interpretation, and critically revised the manuscript. PLCMvR contributed to the design of the study, data interpretation, and critically revised the manuscript. MvdL contributed to the design of the study, data collection and interpretation, and drafted the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Vermeer, M., Kuper, H.H., Bernelot Moens, H.J. et al. Adherence to a treat-to-target strategy in early rheumatoid arthritis: results of the DREAM remission induction cohort. Arthritis Res Ther 14, R254 (2012). https://doi.org/10.1186/ar4099
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar4099