Abstract
Introduction
Ankylosing spondylitis (AS) is a familial, heritable disease specified by syndesmophyte formation leading to an ankylosed spine. Endoplasmic reticulum aminopeptidase 1 (ERAP1) genetic variations have been widely proved to be associated with AS in several ethnic populations. The aim of this study was to investigate whether ERAP1 single nucleotide polymorphisms (SNPs) are associated with AS susceptibility and disease severity in Taiwanese.
Methods
Four ERAP1 SNPs (rs27037, rs27980, rs27044 and rs30187) were genotyped in 797 Taiwanese AS patients and 1,150 healthy controls. Distributions of genotype and alleles were compared between AS patients and healthy controls, and among AS patients stratified by clinical parameters.
Results
The SNP rs27037T allele appeared to be a risk factor for AS susceptibility (P = 5.5 × 10-5, OR 1.30, 95% CI: 1.15 to 1.48; GT+TT vs. GG P = 9.3 × 10-5, OR 1.49, 95% CI: 1.22 to 1.82). In addition, the coding SNP (cSNP) rs27044G allele (P = 1.5 × 10-4, OR 1.28, 95% CI: 1.13 to 1.46; CG+GG vs. CC, P = 1.7 × 10-3, OR 1.44, 95% CI: 1.15 to 1.81) and the cSNP rs30187T allele (P = 1.7 × 10-3, OR 1.23, 95% CI: 1.08 to 1.40; CT+TT vs. CC P = 6.1 × 10-3, OR 1.38, 95% CI: 1.10 to 1.74) were predisposing factors for AS. Notably, the rs27044G allele carriers (CG+GG vs. CC, P = 0.015, OR 1.59, 95% CI: 1.33 to 2.30) and rs30187T allele carriers (CT+TT vs. CC, P = 0.011, OR 1.63, 95% CI: 1.12 to 2.38) were susceptible to syndesmophyte formation in AS patients. Furthermore, two cSNPs (rs27044 and rs30187) strongly associated with HLA-B27 positivity in AS patients. Finally, the ERAP1 SNP haplotype TCG (rs27037T/rs27980C/rs27044G) is a major risk factor for AS (adjusted P <0.00001, OR 1.38, 95% CI: 1.12 to 1.58) in Taiwanese.
Conclusions
This study provides the first evidence of ERAP1 SNPs involving syndesmophyte formation. The interactions between ERAP1 SNPs and HLA-B27 play critical roles in pMHC I pathway processing contributing to the pathogenesis of AS in multiple populations.
Similar content being viewed by others
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory arthritis that preferably affects the sacroiliac and spine joints in young males. Chronic inflammation in joints causes the alteration of joint architecture with new bone formations, and joint fusions may occur consequently [1, 2]. The unique structural changes of syndesmophyte formation and ankylosis of the vertebrae are the primary causes of early severe work disability of AS patients during disease progressions [1–4]. Multiple factors and complex biological interactions may be involved in AS development [5–8].
Twin and family studies revealed a substantial proportion of heritability in AS susceptibility. Genetic studies indicate that HLA-B27 in the MHC (major histocompatibility complex) locus confers the greatest risk to AS susceptibility. However, genome wide association studies (GWAS) also reveal that the non-MHC genes contribute to the AS disease process [4, 5, 8–10]. Several genes and genetic regions have now been discovered and known to be associated with AS susceptibility and severity [8–10]. Of note, there were conflicting association results between Caucasians and Asians [9–12].
Endoplasmic reticulum aminopeptidase 1 (ERAP1) (also known as aminopeptidase regulator of TNFR1 shedding 1 or ARTS1) is an important non-MHC gene associated with AS in genetic studies [9, 10]. Functionally, ERAP1 facilitates the antigen peptide loading onto the major histocompatibility complex class I (MHC I) through trimming the fragmented antigen peptides into the optimal length for peptide/MHC I (pMHC I) complex formation, which is necessary for effective immune responses [13–17]. In addition, ERAP1 involves the shedding of pro-inflammatory cytokine receptors for TNFα, IL-1, and IL-6 [18–20]. ERAP1 SNPs are associated with AS in several ethnic populations [9–12, 21–26], but it is unknown whether ERAP1 SNPs have a role in AS development in Taiwanese. The aim of the present study was to examine whether the ERAP1 SNPs are associated with AS susceptibility and have effects on AS disease severity of syndesmophyte development in Taiwanese.
Materials and methods
Study subjects
The present study recruited 797 patients who fulfilled the 1984 revised New York diagnostic criteria for AS [27], and were followed up at Chang Gung Memorial Hospital (a 3,600-bed medical center and university hospital). Radiographs of the cervical, thoracic and lumbar spine were used by rheumatology specialists to evaluate syndesmophyte formations according to modified Stoke's Ankylosing Spondylitis Spinal Score (mSASSS). To ensure the accuracy of evaluation, two rheumatology specialists (Chen and Ho) independently scored the syndensmophyte formations by blindly reading radiographs of AS patients for appropriate inter- and intra-reader reliability. The X-ray observations were further classified into three groups: group 1 patients did not have any syndesmophyte formations (mSASSS <3), group 2 patients had less than four fused syndesmophyte formations (mSASSS <24) and group 3 patients had four or more syndesmophyte formations (mSASSS >24). The rare disagreements of the radiograph-based evaluations were resolved through consultations between two physicians to eliminate any subjectivity. HLA-B27 antigen positivity was determined by flow cytometry analysis and/or PCR assays. In this study, a total of 1,150 healthy normal controls (512 males and 638 females) were recruited, following a questionnaire survey to exclude donors with rheumatoid arthritis (RA), systemic lupus erythematous (SLE), AS and autoimmune thyroiditis, diabetes mellitus (DM), viral hepatitis (HBV and HCV) infections and cardiovascular diseases. The age of healthy control donors ranged from 18 to 64 years-old with a mean age of 40.3 ± 10.7. The local ethics committee of Chang Gung Memorial Hospital approved the present study. Informed consent was obtained from all patients
Nucleic acid isolation
Anti-coagulated peripheral blood was obtained from healthy control donors and AS patients. Genomic DNA was isolated from EDTA anti-coagulated peripheral blood using the Puregene DNA isolation kit (Gentra Systems, Minneapolis, MN, USA) as previously described [28].
TaqMan-based assays for ERAP1 SNPs
ERAP1 SNPs were genotyped with the TaqMan SNP Made to Order Assays from Applied Biosystems (ABI, Foster City, CA, USA). ERAP1 genotypes were determined using ABI TaqMan Genotyper software according to the vendor's instruction (Foster City, CA, USA).
Statistical analysis
We carried out single-locus ERAP1 SNP analyses in 797 AS patients and 1,150 normal, healthy controls. Three chi-square tests (the genotype test, the allele test and Cochran-Armitage trend test) were performed. Associations of SNPs with AS (P <0.05) were identified using Plink [29] and the SAS/Genetics software package release 8.2 (SAS Institute, Cary, NC, USA). For the analysis of risk genotypes/alleles, logistic regression models adjusted for sex were used to calculate P-values, odds ratios (ORs) and their 95% confidence intervals. Linkage disequilibrium (LD) between marker loci was assessed and haplotype blocks were constructed using Haploview 4.1(Broad Institute of MIT, Cambridge, MA, USA). For each haplotype combination estimated, the haplotype-trait association was tested within different subgroups of disease status (case vs. control), HLA B27 positivity, and syndesmophyte formation were tested for the haplotype-trait association using the SAS HAPLOTYPE procedure. To investigate the association of SNPs with clinical characteristics, we controlled for each of clinical characteristics and performed logistic regression analyses. The 5% level of significance (P <0.05) was adopted for all the analyses. To account for the confounding effects between HLA-B27 positivity and syndesmophyte, we performed the stratified analysis with Cochran -Mantel -Haenszel (CMH) tests for ERAP1 SNP and syndesmophyte formation associations, controlling for HLA-B27 positivity. The results of the trend test, genotype and allelic analyses were adjusted for HLA-B27 positivity. We also carried out analyses with CMH tests for ERAP1 SNP and HLA-B27 associations, adjusted by syndesmophytes formation. The P-values, ORs and 95% CIs for the trend test, genotype and allelic analyses adjusted for syndesmophyte formation.
Results
Clinical characteristics of AS study cohort
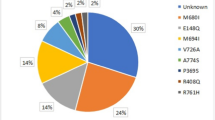
The present study recruited 797 Taiwanese AS patients (667 males and 130 females). The onset ages of 697 AS patients ranged from 5 to 60 years-old. The onset age of a single female was 72 years-old. We were unable to identify exact onset ages of the other 99 AS patients in the study. Among AS patients, 739 (92.7%) patients were HLA-B27 carriers and 393 patients demonstrated syndesmophyte formation (group 2 with mSASSS <24 plus group 3 with mSASSS >24) based on spine radiograph data. Syndesmophyte formation was significantly more common in AS patients positive for HLA-B27 (380 out of 739, 51.4%) as compared to AS patients negative for HLA-B27 (13 of 58, 22.4%) (P <0.0001, OR 3.66, 95% CI: 1.94 to 6.91). Syndesmophyte formation was also significantly enriched in male AS patients (55%, 367 of 667) as compared to the female AS patients (20%, 26 of 130) (P <0.0001, OR 4.89, 95% CI: 3.10 to 7.72). Thus, HLA-B27 positivity and male gender were two major risk factors for AS syndesmophyte formation in our cohort. As shown in Table 1, most AS patients in this cohort had long disease courses (≥5 years) whereas patients with longer disease durations (>20 years) were enriched in AS with the syndesmophyte formation group (54.5%), indicating that the disease duration is also a risk factor for syndesmophyte formation.
Association of ERAP1 SNPs with AS
Four ERAP1 SNPs (rs27037, rs27980, rs27044 and rs30187) were selected based on the SNP locations (chromosome position, coding and regulatory regions) and their functional relevance described in the previous studies. Those four SNPs were genotyped in 797 AS patients and 1,150 healthy controls. The distributions of ERAP1 SNP genotypes were conformed to the Hardy-Weinberg equilibrium in the genotyped subjects (P >0.05). As shown in Table 2, significant differences in the distributions of ERAP1 SNP genotypes and alleles were observed between AS patients and the normal healthy controls. Our analyses indicate that the SNP rs27037T allele is a risk factor for AS susceptibility (Trend test P = 4 × 10-5 with 100,000 permutations; T vs. G, P = 5.5 × 10-5, OR 1.30, 95% CI: 1.15 to 1.48; genotypes GT+TT vs. GG, P = 9.3 × 10-5, OR 1.49, 95% CI: 1.22 to 1.82). On the other hand, the SNP rs27980C allele appears to be a modest risk factor for AS susceptibility (Trend test P = 0.035 with 100,000 permutations; C vs. A, P = 0.033, OR 1.15, 95% CI: 1.01 to 1.31; genotype AC+CC vs. AA, P = 0.024, OR 1.31; 95% CI: 1.04 to 1.65). In addition, both cSNP (coding SNP) rs27044G allele (Trend test P = 1.7 × 10-4 with 100,000 permutations; G vs. C, P = 1.5 × 10-4, OR 1.28, 95% CI: 1.13 to 1.46; genotypes CG+GG vs. CC, P = 1.7 × 10-3, OR 1.44, 95% CI: 1.15 to 1.81), and the cSNP rs30187T allele (Trend test P = 1.6 × 10-3 with 100,000 permutations. T vs. C, P = 1.7 × 10-3, OR 1.23, 95% CI: 1.08 to 1.40; genotype CT+TT vs. CC, P = 6.1 × 10-3, OR 1.38, 95% CI: 1.10 to 1.74) are risk factors for AS susceptibility.
Association of ERAP1 SNPs with AS clinical parameters
AS is a heterogeneous chronic inflammatory disease and present with diverse clinical severity. Subsequently, we stratified AS patients according to clinical characteristics and analyzed the genetic data. As shown in Table 3, we observed that the cSNP rs27044G allele carriers (genotype CG+GG vs. CC, P = 0.015, OR 1.59, 95% CI: 1.33 to 2.30) and the cSNP rs30187T allele carriers (genotype CT+TT vs. CC, P = 0.011, OR 1.63, 95% CI: 1.12 to 2.38) are susceptible to syndesmophyte formation in AS patients. After adjusting for the effect of HLA-B27 positivity, the cSNP rs30187 remains significantly associated with syndesmophyte formation (CMH statistics = 4.236, degree of freedom = 1, P = 0.040) while cSNP rs27044 is marginally associated with syndesmophyte formation (CMH statistics = 3.843, degree of freedom = 1, P = 0.050). The remaining two SNPs did not show any significant associations. Because previous studies demonstrated that human leukocyte antigen HLA-B27 has a causative role in AS pathogenesis, we subsequently investigated whether there is interaction between the ERAP1 SNPs and HLA-B27 positivity. We observed that the distributions of genotypes of four ERAP1 SNPs revealed significant differences between AS patients positive for HLA-B27 and patients negative for HLA-B27 (Table 4). As shown in Table 4, allele distributions of three ERAP1 SNPs (rs27037, rs27044, and rs30187) were significantly different between AS patients positive for HLA-B27 and the patient negative for HLA-B27. Notably, two cSNPs (rs27044 and rs30187) are strongly associated with HLA-B27 positivity. The cSNP rs27044G allele was significantly enriched in AS patients positive for HLA-B27 (Trend test P = 6.3 × 10-3 with 100,000 permutations; G vs. C, P = 5.8 × 10-3, OR 1.70, 95% CI: 1.16 to 2.49; genotypes CG+GG vs. CC, P = 7 × 10-4, OR 2.71, 95% CI: 1.53 to 4.82). The cSNP rs30187T allele was also significantly enriched in AS patients positive for HLA-B27 (Trend test P = 6.1 × 10-3 with 100,000 permutations; T vs. C, P = 5.4 × 10-3, OR 1.71, 95% CI: 1.17 to 2.49; genotypes CT+TT vs. CC, P = 4 × 10-4, OR 2.86, 95% CI: 1.61 to 5.09). We also analyzed associations between ERAP1 SNPs and HLA-B27 positivity after controlling for the syndesmophyte formation. The CMH test results revealed that the significant associations between three ERAP1 SNPs (rs27037, rs27044, and rs30187) and HLA-B27 positivity (P <0.01). Our data indicate that interaction of ERAP1 and HLA-B27 may play a pivotal role in the pathogeneses of AS.
ERAP 1 SNP haplotypes are associated with AS susceptibility
We next examined the influence of ERAP1 SNP haplotypes on AS susceptibility and syndesmophyte formation according to the linkage disequilibrium (LD) block (Figure 1). Due to the fact that two ERAP1 cSNPs (rs27044 and rs30187) are in extremely strong LD (0.99), we selected rs27044 as the representative marker for two cSNPs in the subsequent haplotypes analysis. As shown in Table 5, ERAP1 SNP haplotype TCG (rs27037T/rs27980C/rs27044G) frequency is significantly increased in AS patients (0.475) as compared to healthy controls (0.399) (adjusted P <0.00001, OR 1.38, 95% CI: 1.12 to 1.58), suggesting that the haplotype TCG is a risk marker for AS. On the other hand, haplotype GCC (rs27037G/rs27980C/rs27044C) frequency was significantly increased in healthy controls (0.119) compared to AS patients (0.085) (adjusted P = 1.9 × 10-3, OR 0.69, 95% CI: 0.55 to .87), indicating that the haplotype GCC has a protective role against AS. The haplotype TCG frequency is slightly higher in AS patients positive for syndesmophyte formation as compared to that in AS patients negative for syndesmophyte formation; however, no significant difference was observed (P >0.05)
Discussion
Complex interactions between environmental factors and host immune responses are the origins for AS development [4, 5]. It is clear that genetic factors influence the immune responses and progression of AS. The current study demonstrated the associations of EARP1 SNPs with the AS susceptibility in Taiwanese. Aminopeptidases play a central role in the generation of MHC class I-binding peptides through processing and trimming peptide. As an IFNγ-induced aminopeptidase, ERAP1 breaks down protein antigen precursors and trims the peptides fragments into the suitable length for peptide/MHC I complex formation in ER [13, 14, 30]. In mice, ERAP1 deficiency led to the reduced MHC I expression in splenocytes and the decreased viral peptide presentation by MHC I on fibroblasts [31]. The generation of effective CD8 T cell responses was compromised in ERAP1 deficient mice as self and foreign antigen presentations were disrupted [31–36]. In humans, over-expression of ERAP1 was observed in AS patient dendritic cells (DCs) [37]. ERAP1 also enhances phagocytic activity of human macrophages through generating active peptides [38]. Functionally, ERAP1 may have a substantial role in the AS pathogenesis. Our current study demonstrated the associations of ERAP1 SNPs with the AS susceptibility in Taiwanese, indicating that ERAP1 has a role in AS development in Taiwanese
We observed that >90% of AS patients are HLA-B27 carriers. Our data confirmed that HLA-B27 plays the most critical role in AS disease progression. HLA-B27 may influence AS development through three possible mechanisms: I) HLA-B27 may preferentially bind distinctive arthritogenic peptides, II) inappropriately folded HLA-B27 heavy chain without a docking antigen peptide may lead to the unfolded protein responses (UPRs), and III) HLA-B27 may have a tendency to be expressed as empty MHC I heavy chain homodimers [4, 39]. However, the precise mechanisms underlying the critical role of HLA-B27 in AS development remain to be elucidated [40].
Of great importance, immune surveillance of the CD8 T cell to environmental insults, such as bacterial and viral infections, requires the interaction between T cell receptor (TCR) and peptide/MHC I complex. ERAP1 trims protein antigens to fit for MHC I including HLA-B27. The stability of antigen peptide/MHC I complexes is influenced by both ERAP1 activities and peptide binding groove sequences of MHC I [41]. Very recently, Evans et al. demonstrated the gene-gene interaction between ERAP1 SNP rs30187T allele and HLA-B27 positivity in the pathogenesis of AS [42]. Our study provided further evidence that ERAP1 SNPs are indeed associated with the HLA-B27 positivity in Taiwanese AS patients. Our data support the notion that ERAP1 and HLA-B27 have synergistic roles in AS pathogenesis in humans. Our findings also suggest that abnormal antigen processing by ERAP1 and antigen presentation by HLA-B27 may be critical pathways in AS development. On the other hand, AS patients negative for HLA-B27 may develop pathologic immune responses through the other unidentified biological pathways.
The disease course of AS is heterogeneous and the genetic factors are believed to influence disease susceptibility and severity. Early syndesmophyte formations in AS patients indicate radiologic progression and characteristic structure changes that lead to the decreased spinal mobility, functional impairments and work disability in long-term disease courses [4, 43]. Sacroiliac joint biopsy examinations frequently revealed significant new bone formations and bony ankylosis in AS patients [44]. Spinal inflammation and bone remodeling may be two important factors in the progress of ankylosis but the precise pathogenesis of AS remains unknown [44, 45]. The current study demonstrated that ERAP1 cSNPs rs27044 and rs30187 are modestly associated with AS syndesmophyte formation, suggesting that the ERAP1 cSNPs may affect AS disease severity. Syndesmophyte of AS is more likely to develop at sites of previous inflammation, indicating ankylosis development is strongly correlated with inflammation [44]. The ERAP1 protein also participates in the regulation of proinflammatory cytokine receptor functions. ERAP1 cleaves membrane-associated TNFR1, IL-6R, and interleukin 1 receptor II (IL-1RII) and causes the shedding of those cytokine receptors. Some cellular and molecular signal pathways that regulate the development of hematopoietic cell and bone homeostasis are shared by the immune system and bone development [45]. IL6 and TNFα cytokine networks may affect the Th17 cell development and the plasticity of T cell differentiation, which are critical in the pathogenesis of AS. The serum cytokine receptor levels in AS patients are correlated with the levels ESR and CRP, which are indicators of AS inflammatory activities. Nevertheless, the serum cytokine receptor levels in patients with AS are not influenced by ERAP1 SNPs [46]. Animal models have even suggested that inflammation and new bone formation are uncoupled processes [47, 48]. Clinically, various anti-TNF therapies suppress the inflammation process but do not retard the structural progression according to modified Stoke's Ankylosing Spondylitis Spinal Score (mSASSS) [49–51]. These findings indicate the syndesmophyte development may largely attribute to the intrinsic genetic effects of ERAP 1 on p/MHC I complex formation.
UPRs can cause the activation of NFκB, which could enhance downstream proinflammatory gene expression and promote inflammations. Genetic variations of HLA-B27 and ERAP1 have functional roles in the misfolding and UPR of the heavy chain [4, 40]. HLA-B27 misfolding is triggered in the oxidizing environment in endoplasmic reticulum (ER) by exposing cysteine residues within the heavy chain [40]. ERAP1 is required for efficient enzymatic activities that suggest the polymorphisms at sites remote from the catalytic sites might modify this association [52]. ERAP1 processes peptide substrates with the optimal sizes for MHC I (40, 41). Crystallography analyses suggest that the coding SNP rs30187 changes the amino acid residue that may affect the catalytic activity [53]. Notably, the alleles and genotypes of ERAP1 SNPs in Taiwanese and other Asians showed different distribution and opposite risk results in AS susceptibility compared to Caucasians [9–12, 21–26]. In addition, ERAP1 SNP rs30187C allele carriers (CC+CT) were found to be associated with higher baseline radiographic severity based on mSASSS on univariate analysis [54]. The current study demonstrated that both SNP rs30187T and rs27044G allele carrier were modestly associated with AS disease severity of syndesmophyte formation. Functional studies of ERAP1 SNPs have identified that the rs30187C allele carries less biological enzyme activity, which may decrease aberrant peptide processing and HLA-B27 presentation [42], the rs27044C allele carrier genotype demonstrated significantly higher free heavy chain (FHC) expression but lower intact HLAB27 complexes/FHCs ratio [55], and ERAP1 SNPs (rs30187 and rs27044) showed specific peptide substrate sequence interaction [52]. Moreover, large multifunctional peptidase 2 (LMP2) rs17587 SNP has been demonstrated to associate with AS radiographic severity [54]. These findings indicated multiple gene interactions are involved in the complexity of AS disease susceptibility and severity, and no definite functional roles of ERAP1 cSNPs rs30187 and rs27044 in antigen processing can fully answer the discrepancy results in different ethnic backgrounds. Nevertheless, other ERAP1 SNPs may also affect UPR and subsequent immune responses. Further functional studies are required to understand the precise roles of ERAP1 SNPs contribute to the AS pathogenesis.
In this cross sectional study, some AS patients may not receive enough follow-up in the syndesmophyte formation assessment, which is the main limitation of our study. Therefore, future longitudinal studies are required to estimate the effect of ERAP1 SNPs on the bamboo spine development in large AS patient cohorts.
Conclusion
This study provided further evidence that ERAP1 interaction with HLA-B27 is involved in the development of AS and disease severity, which emphasized the critical role of pMHC I pathway genes in the pathogenesis of AS. Identification of the functional causal alleles of ERAP1 provides a new avenue in understanding the molecular mechanisms of AS pathogenesis, which may lead to novel treatment approaches.
Acknowledgements
The authors would like to thank Shin Chu Blood Donor Center for sample collection. This study was supported by grants from Chang Gung Memorial Hospital (No. CMRPG381082) and National Science Council, Taiwan (NMRPG-97-2314-B182A-025-MY3).
Abbreviations
- AS:
-
ankylosing spondylitis
- CMH:
-
Cochran -Mantel -Haenszel
- DCs:
-
dendritic cells
- DM:
-
diabetes mellitus
- ER:
-
endoplasmic reticulum
- ERAP1:
-
endoplasmic reticulum aminopeptidase 1
- FHC:
-
free heavy chain
- GWAS:
-
genome wide association studies
- IL:
-
interleukin
- LD:
-
linkage disequilibrium
- LMP2:
-
large multifunctional peptidase 2
- MHC:
-
major histocompatibility complex
- mSASSS:
-
modified Stoke's Ankylosing Spondylitis Spinal Score
- ORs:
-
odds ratios
- RA:
-
rheumatoid arthritis
- SLE:
-
systemic lupus erythematous
- SNP:
-
single nucleotide polymorphism
- TCR:
-
T cell receptor
- TNFR1:
-
tumor necrosis factor receptor 1
- UPRs:
-
unfolded protein responses
References
van der Linden SM, van der Heijde D, Maksymowych WP: Ankylosing spondylitis. Kelley's Textbook of Rheumatology. Edited by: Firestein GS, Budd RC, Harris ED Jr, McInnes IB, Ruddy S, Sergent JS. 2008, Philadelphia: Saunders-Elsevier, II: 1169-1190. 8
Braun J, Sieper J: Ankylosing spondylitis. Lancet. 2007, 369: 1379-1390. 10.1016/S0140-6736(07)60635-7.
Lories RJ, Luyten FP, de Vlam K: Progress in spondylarthritis. Mechanisms of new bone formation in spondyloarthritis. Arthritis Res Ther. 2009, 11: 221-10.1186/ar2642.
Tam LS, Gu J, Yu D: Pathogenesis of ankylosing spondylitis. Nat Rev Rheumatol. 2010, 6: 399-405. 10.1038/nrrheum.2010.79.
Brown MA: Genetics and the pathogenesis of ankylosing spondylitis. Curr Opin Rheumatol. 2009, 21: 318-323. 10.1097/BOR.0b013e32832b3795.
Said-Nahal R, Miceli-Richard C, Berthelot JM, Duché A, Dernis-Labous E, Le Blévec G, Saraux A, Perdriger A, Guis S, Claudepierre P, Sibilia J, Amor B, Dougados M, Breban M: The familial form of spondylarthropathy: a clinical study of 115 multiplex families. Arthritis Rheum. 2000, 43: 1356-1365. 10.1002/1529-0131(200006)43:6<1356::AID-ANR20>3.0.CO;2-Y.
Brown MA, Kennedy LG, MacGregor AJ, Darke C, Duncan E, Shatford JL, Taylor A, Calin A, Wordsworth P: Susceptibility to ankylosing spondylitis in twins: the role of genes, HLA, and the environment. Arthritis Rheum. 1997, 40: 1823-1828. 10.1002/art.1780401015.
Reveille JD: The genetic basis of spondyloarthritis. Ann Rheum Dis. 2011, 70 (Suppl 1): 44-50. 10.1136/ard.2010.140574.
Wellcome Trust CaseControl Consortium; Australo-Anglo-American Spondylitis Consortium (TASC), Burton PR, Clayton DG, Cardon LR, Craddock N, Deloukas P, Duncanson A, Kwiatkowski DP, McCarthy MI, Ouwehand WH, Samani NJ, Todd JA, Donnelly P, Barrett JC, Davison D, Easton D, Evans DM, Leung HT, Marchini JL, Morris AP, Spencer CC, Tobin MD, Attwood AP, Boorman JP, Cant B, Everson U, Hussey JM, Jolley JD, Knight AS, Koch K, et al: Association scan of 14,500 nonsynonymous SNPs in four diseases identifies autoimmunity variants. Nat Genet. 2007, 39: 1329-1337. 10.1038/ng.2007.17.
Australo-Anglo-American Spondyloarthritis Consortium(TASC), Reveille JD, Sims AM, Danoy P, Evans DM, Leo P, Pointon JJ, Jin R, Zhou X, Bradbury LA, Appleton LH, Davis JC, Diekman L, Doan T, Dowling A, Duan R, Duncan EL, Farrar C, Hadler J, Harvey D, Karaderi T, Mogg R, Pomeroy E, Pryce K, Taylor J, Savage L, Deloukas P, Kumanduri V, Peltonen L, Ring SM, Whittaker P, et al: Genome-wide association study of ankylosing spondylitis identifies non-MHC susceptibility loci. Nat Genet. 2010, 42: 123-127. 10.1038/ng.513.
Harvey D, Pointon JJ, Evans DM, Karaderi T, Farrar C, Appleton LH, Sturrock RD, Stone MA, Oppermann U, Brown MA, Wordsworth BP: Investigating the genetic association between ERAP1 and ankylosing spondylitis. Hum Mol Genet. 2009, 18: 4204-4212. 10.1093/hmg/ddp371.
Davidson SI, Wu X, Liu Y, Wei M, Danoy PA, Thomas G, Cai Q, Sun L, Duncan E, Wang N, Yu Q, Xu A, Fu Y, Brown MA, Xu H: Association of ERAP1, but not IL23R, with ankylosing spondylitis in a Han Chinese population. Arthritis Rheum. 2009, 60: 3263-3268. 10.1002/art.24933.
Saric T, Chang SC, Hattori AI, York IA, Markant SK, Rock KL, Tsujimoto M, Goldberg AL: An IFN gamma induced aminopeptidase in the ER, ERAP1, trims precursors to MHC class I-presented peptides. Nat Immunol. 2002, 3: 1169-1176. 10.1038/ni859.
York IA, Chang SC, Saric t, Keys A, Favreau JM, Goldberg AL, Rock KL: The ER aminopeptidase ERAP1 enhances or limits antigen presentation by trimming epitopes to 8-9 residues. Nat Immunol. 2002, 3: 1177-1184. 10.1038/ni860.
Hilton C, Kisselev AF, Rock KL, Goldberg AL: 26S proteasomes and immunoproteasomes produce mainly N-extended versions of an antigenic peptide. EMBO J. 2001, 20: 2357-2366. 10.1093/emboj/20.10.2357.
Rock KL, York IA, Goldberg AL: Post-proteasomal antigen processing for major histocompatibility complex class I presentation. Nat Immunol. 2004, 5: 670-677. 10.1038/ni1089.
Serwold T, Gonzalez F, Kim J, Jacob R, Shastri N: ERAAP customizes peptides for MHC class I molecules in the endoplasmic reticulum. Nature. 2002, 419: 480-483. 10.1038/nature01074.
Cui X, Hawari F, Alsaaty S, Lawrence M, Combs CA, Geng W, Rouhani FN, Miskinis D, Levine SJ: Identification of ARTS-1 as a novel TNFR1-binding protein that promotes TNFR1 ectodomain shedding. J Clin Invest. 2002, 110: 515-526.
Cui X, Rouhani FN, Hawari F, Levine SJ: An aminopeptidase, ARTS-1, is required for interleukin-6 receptor shedding. J Biol Chem. 2003, 278: 28677-28685. 10.1074/jbc.M300456200.
Cui X, Rouhani FN, Hawari F, Levine SJ: Shedding of the type II IL-1 decoy receptor requires a multifunctional aminopeptidase, aminopeptidase regulator of TNF receptor type 1 shedding. J Immunol. 2003, 171: 6814-6819.
Tsui FW, Haroon N, Reveille JD, Rahman P, Chiu B, Tsui HW, Inman RD: Association of an ERAP1 ERAP2 haplotype with familial ankylosing spondylitis. Ann Rheum Dis. 2010, 69: 733-736. 10.1136/ard.2008.103804.
Choi CB, Kim TH, Jun JB, Lee HS, Shim SC, Lee B, Pope A, Uddin M, Rahman P, Inman RD: ARTS1 polymorphisms are associated with ankylosing spondylitis in Koreans. Ann Rheum Dis. 2010, 69: 582-584. 10.1136/ard.2008.105296.
Davidson SI, Liu Y, Danoy PA, Wu X, Thomas GP, Jiang L, Sun L, Wang N, Han J, Han H, Australo-Anglo-American Spondyloarthritis Consortium, Visscher PM, Brown MA, Xu H: Association of STAT3 and TNFRSF1A with ankylosing spondylitis in Han Chinese. Ann Rheum Dis. 2011, 70: 289-292. 10.1136/ard.2010.133322.
Li C, Lin Z, Xie Y, Guo Z, Huang J, Wei Q, Li QX, Wang X, Cao S, Liao Z, Xu M, Shen Y, Gu J: ERAP1 is associated with ankylosing spondylitis in Han Chinese. J Rheumatol. 2011, 38: 317-321. 10.3899/jrheum.100013.
Bang SY, Kim TH, Lee B, Kwon E, Choi SH, Lee KS, Shim SC, Pope A, Rahman P, Reveille JD, Inman RD: Genetic studies of ankylosing spondylitis in Koreans confirm associations with ERAP1 and 2p15 reported in white patients. J Rheumatol. 2011, 38: 322-324. 10.3899/jrheum.100652.
Pazár B, Sáfrány E, Gergely P, Szántó S, Szekanecz Z, Poór G: Association of ARTS1 gene polymorphisms with ankylosing spondylitis in the Hungarian population: the rs27044 variant is associated with HLA-B*2705 subtype in Hungarian patients with ankylosing spondylitis. J Rheumatol. 2010, 37: 379-384. 10.3899/jrheum.090806.
van der Linden S, Valkenburg HA, Cats A: Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984, 27: 361-368. 10.1002/art.1780270401.
Chen JY, Wang CM, Ma CC, Luo SF, Edberg JC, Kimberly RP, Wu J: Association of a transmembrane polymorphism of Fcgamma receptor IIb (FCGR2B) with systemic lupus erythematosus in Taiwanese patients. Arthritis Rheum. 2006, 54: 3908-3917. 10.1002/art.22220.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, Sham PC: PLINK: a toolset for whole-genome association and population-based linkage analysis. Am J Hum Genet. 2007, 81: 559-575. 10.1086/519795.
Chang SC, Momburg F, Bhutani N, Goldberg AL: The ER aminopeptidase, ERAP1, trims precursors to lengths of MHC class I peptides by a "molecular ruler" mechanism. Proc Natl Acad Sci USA. 2005, 102: 17107-17112. 10.1073/pnas.0500721102.
York IA, Brehm MA, Zendzian S, Towne CF, Rock KL: Endoplasmic reticulum aminopeptidase 1 (ERAP1) trims MHC class I-presented peptides in vivo and plays an important role in immunodominance. Proc Natl Acad Sci USA. 2006, 103: 9202-9207. 10.1073/pnas.0603095103.
Blanchard N, Kanaseki T, Escobar H, Delebecque F, Nagarajan NA, Reyes-Vargas E, Crockett DK, Raulet DH, Delgado JC, Shastri N: Endoplasmic reticulum aminopeptidase associated with antigen processing defines the composition and structure of MHC class I peptide repertoire in normal and virus-infected cells. J Immunol. 2010, 184: 3033-3042. 10.4049/jimmunol.0903712.
Hammer GE, Gonzalez F, Champsaur M, Cado D, Shastri N: The aminopeptidase ERAAP shapes the peptide repertoire displayed by major histocompatibility complex class I molecules. Nat Immunol. 2006, 7: 103-112. 10.1038/ni1286.
Hammer GE, Gonzalez F, James E, Nolla H, Shastri N: In the absence of aminopeptidase ERAAP, MHC class I molecules present many unstable and highly immunogenic peptides. Nat Immunol. 2006, 8: 101-108.
Yan J, Parekh VV, Mendez-Fernandez Y, Olivares-Villagomez D, Dragovic S, Hill T, Roopenian DC, Joyce S, Van Kaer L: In vivo role of ER-associated peptidase activity in tailoring peptides for presentation by MHC class Ia and class Ib molecules. J Exp Med. 2006, 203: 647-665. 10.1084/jem.20052271.
Firat E, Saveanu L, Aichele P, Staeheli P, Huai J, Gaedicke S, Nil A, Besin G, Kanzler B, van Endert P, Niedermann G: The role of endoplasmic reticulum-associated aminopeptidase 1 in immunity to infection and in cross-presentation. J Immunol. 2007, 178: 2241-2248.
Campbell EC, Fettke F, Bhat S, Morley KD, Powis SJ: Expression of MHC class I dimers and ERAP1 in an ankylosing spondylitis patient cohort. Immunology. 2011, 133: 379-385. 10.1111/j.1365-2567.2011.03453.x.
Goto Y, Ogawa K, Hattori A, Tsujimoto M: Secretion of endoplasmic reticulum aminopeptidase 1 is involved in the activation of macrophages induced by lipopolysaccharide and interferon gamma. J Biol Chem. 2011, 286: 21906-21914. 10.1074/jbc.M111.239111.
Colbert RA, DeLay ML, Klenk EI, Layh-Schmitt G: From HLA-B27 to spondyloarthritis: a journey through the ER. Immunol Rev. 2010, 233: 181-202. 10.1111/j.0105-2896.2009.00865.x.
Haroon N, Inman RD: Endoplasmic reticulum aminopeptidases: biology and pathogenic potential. Nat Rev Rheumatol. 2010, 6: 461-467. 10.1038/nrrheum.2010.85.
Kanaseki T, Blanchard N, Hammer GE, Gonzalez F Shastri N: ERAAP synergizes with MHC class I molecules to make the final cut in the antigenic peptide precursors in the endoplasmic reticulum. Immunity. 2006, 25: 795-806. 10.1016/j.immuni.2006.09.012.
Evans DM, Spencer CC, Pointon JJ, Su Z, Harvey D, Kochan G, Oppermann U, Dilthey A, Pirinen M, Stone MA, Appleton L, Moutsianas L, Leslie S, Wordsworth T, Kenna TJ, Karaderi T, Thomas GP, Ward MM, Weisman MH, Farrar C, Bradbury LA, Danoy P, Inman RD, Maksymowych W, Gladman D, Rahman P, Spondyloarthritis Research Consortium of Canada (SPARCC), Morgan A, Marzo-Ortega H, Bowness P, et al: Interaction between ERAP1 and HLA-B27 in ankylosing spondylitis implicates peptide handling in the mechanism for HLA-B27 in disease susceptibility. Nat Genet. 2011, 43: 761-767. 10.1038/ng.873.
Baraliakos X, Listing J, Rudwaleit M, Haibel H, Brandt J, Sieper J, Braun J: Progression of radiographic damage in patients with ankylosing spondylitis: defining the central role of syndesmophytes. Ann Rheum Dis. 2007, 66: 910-915. 10.1136/ard.2006.066415.
Baraliakos X, Listing J, Rudwaleit M, Sieper J, Braun J: The relationship between inflammation and new bone formation in patients with ankylosing spondylitis. Arthritis Res Ther. 2008, 10: R104-10.1186/ar2496.
Schett G: Joint remodelling in inflammatory disease. Ann Rheum Dis. 2007, 66 (Suppl 3): 42-44.
Haroon N, Tsui FW, Chiu B, Tsui HW, Inman RD: Serum cytokine receptors in ankylosing spondylitis: relationship to inflammatory markers and endoplasmic reticulum aminopeptidase polymorphisms. J Rheumatol. 2010, 37: 1907-1910. 10.3899/jrheum.100019.
Lories RJ, Derese I, Luyten FP: Inhibition of osteoclasts does not prevent joint ankylosis in a mouse model of spondyloarthritis. Rheumatology. 2008, 47: 605-608. 10.1093/rheumatology/ken082.
Lories RJ, Derese I, de Bari C, Luyten FP: Evidence for uncoupling of inflammation and joint remodeling in a mouse model of spondylarthritis. Arthritis Rheum. 2007, 56: 489-497. 10.1002/art.22372.
van der Heijde D, Salonen D, Weissman BN, Landewé R, Maksymowych WP, Kupper H, Ballal S, Gibson E, Wong R: Assessment of radiographic progression in the spines of patients with ankylosing spondylitis treated with adalimumab for up to 2 years. Arthritis Res Ther. 2009, 11: R127-10.1186/ar2794.
van der Heijde D, Landewé R, Einstein S, Ory P, Vosse D, Ni L, Lin SL, Tsuji W, Davis JC: Radiographic progression of ankylosing spondylitis after up to two years of treatment with etanercept. Arthritis Rheum. 2008, 58: 1324-1331. 10.1002/art.23471.
van der Heijde D, Landewé R, Baraliakos X, Houben H, van Tubergen A, Williamson P, Xu W, Baker D, Goldstein N, Braun J: Radiographic findings following two years of infliximab therapy in patients with ankylosing spondylitis. Ankylosing Spondylitis Study for the Evaluation of Recombinant Infliximab Therapy Study Group. Arthritis Rheum. 2008, 58: 3063-3070. 10.1002/art.23901.
Evnouchidou I, Kamal RP, Seregin SS, Goto Y, Tsujimoto M, Hattori A, Voulgari PV, Drosos AA, Amalfitano A, York IA, Stratikos E: Coding single nucleotide polymorphisms of endoplasmic reticulum aminopeptidase 1 can affect antigenic peptide generation in vitro by influencing basic enzymatic properties of the enzyme. J Immunol. 2011, 186: 1909-1913. 10.4049/jimmunol.1003337.
Kochan G, Krojer T, Harvey D, Fischer R, Chen L, Vollmar M, von Delft F, Kavanagh KL, Brown MA, Bowness P, Wordsworth P, Kessler BM, Oppermann U: Crystal structures of the endoplasmic reticulum aminopeptidase-1 (ERAP1) reveal the molecular basis for N-terminal peptide trimming. Proc Natl Acad Sci USA. 2011, 108: 7745-7750. 10.1073/pnas.1101262108.
Haroon N, Maksymowych W, Rahman P, Tsui F, O'Shea F, Inman R: Radiographic severity in ankylosing spondylitis is associated with polymorphism in large multifunctional peptidase 2 (LMP2) in the Spondyloarthritis Research Consortium of Canada cohort. Arthritis Rheum. 2012, 64: 1119-1126. 10.1002/art.33430.
Haroon N, Tsui FW, Uchanska-Ziegler B, Ziegler A, Inman RD: Endoplasmic reticulum aminopeptidase 1 (ERAP1) exhibits functionally significant interaction with HLA-B27 and relates to subtype specificity in ankylosing spondylitis. Ann Rheum Dis. 2012, 71: 589-595. 10.1136/annrheumdis-2011-200347.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
CMW and JYC carried out the design of the study and participated in statistical analysis and manuscript writing. HHH performed clinical evaluation of the patients and participated in the design of the study. SWC performed statistical analysis. YJJW and JCL participated in clinical evaluation of the patients. PYC helped on laboratorial determination. JW participated in the design of study and manuscript revision. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wang, CM., Ho, HH., Chang, SW. et al. ERAP1 genetic variations associated with HLA-B27 interaction and disease severity of syndesmophytes formation in Taiwanese ankylosing spondylitis. Arthritis Res Ther 14, R125 (2012). https://doi.org/10.1186/ar3855
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar3855