Abstract
Introduction
The single nucleotide polymorphism (SNP) rs6822844 within the KIAA1109-TENR-IL2-IL21 gene cluster has been associated with rheumatoid arthritis (RA). Other variants within this cluster, including rs17388568 that is not in linkage disequilibrium (LD) with rs6822844, and rs907715 that is in moderate LD with rs6822844 and rs17388568, have been associated with a number of autoimmune phenotypes, including type 1 diabetes (T1D). Here we aimed to: one, confirm at a genome-wide level of significance association of rs6822844 with RA and, two, evaluate whether or not there were effects independent of rs6822844 on RA at the KIAA1109-TENR-IL2-IL21 locus.
Methods
A total of 842 Australasian RA patients and 1,115 controls of European Caucasian ancestry were genotyped for rs6822844, rs17388568 and rs907715. Meta-analysis of these data with published and publicly-available data was conducted using STATA.
Results
No statistically significant evidence for association was observed in the Australasian sample set for rs6822844 (odds ratio (OR) = 0.95 (0.80 to 1.12), P = 0.54), or rs17388568 (OR = 1.03 (0.90 to 1.19), P = 0.65) or rs907715 (OR = 0.98 (0.86 to 1.12), P = 0.69). When combined in a meta-analysis using data from a total of 9,772 cases and 10,909 controls there was a genome-wide level of significance supporting association of rs6822844 with RA (OR = 0.86 (0.82 to 0.91), P = 8.8 × 10-8, P = 2.1 × 10-8 including North American Rheumatoid Arthritis Consortium data). Meta-analysis of rs17388568, using a total of 6,585 cases and 7,528 controls, revealed no significant association with RA (OR = 1.03, (0.98 to 1.09); P = 0.22) and meta-analysis of rs907715 using a total of 2,689 cases and 4,045 controls revealed a trend towards association (OR = 0.93 (0.87 to 1.00), P = 0.07). However, this trend was not independent of the association at rs6822844.
Conclusions
The KIAA1109-TENR-IL2-IL21 gene cluster, that encodes an interleukin (IL-21) that plays an important role in Th17 cell biology, is the 20th locus for which there is a genome-wide (P ≤ 5 ×10-8) level of support for association with RA. As for most other autoimmune diseases, with the notable exception of T1D, rs6822844 is the dominant association in the locus. The KIAA1109-TENR-IL2-IL21 locus also confers susceptibility to other autoimmune phenotypes with a heterogeneous pattern of association.
Similar content being viewed by others
Introduction
Genetic associations implicate aberrant activation and regulation of autoreactive T-cells as central to RA. In addition to the established human leukocyte antigen locus DRB1, other genes more recently confirmed (either through wide replication or combined analysis at a genome-wide level of significance, P ≤ 10-8) as playing a role in the development of RA are the protein tyrosine phosphatase non-receptor 22 gene (PTPN22) [1], cytotoxic T-lymphocyte associated 4 (CTLA4) [2], an intergenic region on human chromosome 6 [3, 4], signal transducer and activator of transcription 4 (STAT4) [5, 6], the TNF receptor-associated factor 1 region (TRAF/C5) [3, 7, 8], CD40 [9, 10], B-lymphocyte kinase (BLK) and the NF-kB family member c-Rel [11]. Aside from HLA-DRB1 and PTPN22, the effects are weak (odds ratio (OR) < 1.3). Most of these loci are also implicated as risk factors in other autoimmune phenotypes [12].
The KIAA1109-TENR-IL2-IL21 region has been associated with a number of autoimmune phenotypes including type 1 diabetes (T1D) [13], ulcerative colitis [14], Crohn's disease [15], celiac disease [16], Graves' disease (GD) [13], systemic lupus erythematosus (SLE) [17], psoriatic arthritis [18], and juvenile idiopathic arthritis [19] (Table 1). There have been several studies testing this region for association with RA in European Caucasian sample sets, with varying levels of supporting evidence (0.24 > P > 2.8 × 10-4) [6, 12, 20, 21]. There is extensive linkage disequilibrium across the region, hampering fine-mapping efforts [13], however it is clear that there are two independent autoimmune associated regions within the KIAA1109-TENR-IL2-IL21 gene cluster. Here, we aimed to consolidate all available data on two SNPs independently associated with autoimmunity within the KIAA1109-TENR-IL2-IL21 gene cluster: rs6822844 (minor allele protective) and rs17388568 (minor allele susceptible), each into a single meta-analysis of association with RA that included previously published data, new genotype data from Australasia, and publicly-available data from the Wellcome Trust Case Control Consortium (WTCCC) [22].
Materials and methods
Study participants
The Australasian European Caucasian RA samples consist of 842 patients of whom 31% were male. For the RA patients for whom data were available, 81% (601/739) were rheumatoid factor (RF) positive, 68% (333/491) were anti-cyclic citrullinated peptide (CCP) antibody positive and 80% (657/820) carried the HLA-DRB1 shared epitope (SE). RA diagnosis was confirmed in all patients by a rheumatologist using the ACR criteria [23]. Patients were recruited from hospital outpatient clinics in the Auckland, Bay of Plenty, Wellington, Christchurch and Otago regions of New Zealand, and from Adelaide in South Australia. European Caucasian control subjects (n = 505) without RA were recruited from the Otago and Auckland regions of New Zealand and were all > 17 years of age. A further 610 controls recruited from the Otago region had been genome-wide scanned using the Affymetrix Genome-Wide Human SNP Array 6.0 [24]. These elderly controls were > 60 years of age and in good general health. All subjects provided informed written consent and ethical approval for this study was given by the New Zealand Multi-region Ethics Committee and the Lower South Ethics Committee, and the Research and Ethics Committee of the Repatriation General Hospital, Adelaide. Genomic DNA was extracted from peripheral blood samples using a guanidine isothiocyanate-chloroform based (RA patients and controls) or modified salting out (elderly controls) extraction method.
Genotype generation
Study participants were genotyped for rs6822844, rs17388568 and rs907715 using TaqMan®, assays ID C_28983601_10, ID C_33129431_10 and ID C_8949748_10 (Applied Biosystems, Foster City, CA, USA) respectively. Imputed RA and control genotypes were obtained for rs6822844, rs17388568 and rs907715 from 100% of the WTCCC dataset (1,856 cases, 2,933 controls) using the publicly available WTCCC data [22] using the program IMPUTE [25] and HapMap (NCBI Build 36 (db126b)) CEU data as reference haplotype set. Of the Australasian case sample set, 99.1% of subjects for rs6822844, 99.1% of subjects for rs17388568 and 98.9% of subjects for rs9077015 were successfully genotyped and, for the 505 member control sample set, 97.4% of subjects for rs6822844, 99.4% of subjects for rs17388568 and 99.4% of subjects for rs9077015 were successfully genotyped. The remaining New Zealand control genotypes (n = 610) were obtained from the genome-wide data, with 100% successfully genotyped for rs17388568 and 99.6% imputed for rs6822844 and rs907715.
Statistical analysis
Genotype data were managed using the BC|SNPmax system (Biocomputing Platforms Ltd, Espoo, Finland). Testing for departures from Hardy-Weinberg equilibrium, for the significance of any difference in minor allele frequencies between patients and controls, calculating odds ratios and conditional association testing was done using the PLINK software package [26]. Logistic regression analysis was applied to the Australasian case-control sample set to stratify data according to gender, RF, CCP and SE status using the STATA 8.0 data analysis and statistics software package (StataCorp, College Station, Texas, USA). Meta-analysis was done using the STATA 8.0 metan software package and cumulative P- values reported. The Mantel-Haenszel test was used to estimate the average conditional common odds ratio between these two independent cohorts and to test for heterogeneity between the groups. P- values from the North American Rheumatoid Arthritis Consortium (NARAC) study [3], which could not be combined using meta-analysis owing to unavailability of allele counts, were combined using Fisher's method [27].
Results
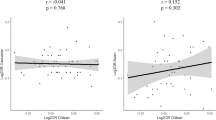
We examined rs6822844, rs17388568 and rs907715. The latter SNP was chosen because it had been associated with risk of the systemic autoimmunity SLE in a single study [17] (OR = 0.78, P = 0.002), was in weak LD with both rs6822844 and rs17388568 and we hypothesized that it could represent a possible third effect within the KIAA1109-TENR-IL2-IL21 cluster, perhaps specific to systemic autoimmunity. The imputed genotype data from the WTCCC RA case-control sample revealed no significant association between rs6822844 and RA (Table 2; OR = 0.91 (0.82 to 1.02); P = 0.10) (the WTCCC samples did not overlap with those analysed in Barton et al. [12]). SNP rs6822844 had been genotyped in the NARAC sample set [3], revealing nominal evidence for a protective effect of the minor allele (Table 2; OR = 0.84 (0.74 to 0.96), P = 0.011). We then genotyped rs6822844 across the Australasian case-control sample set, finding no evidence for association between rs6822844 and RA (Table 2; OR = 0.95 (0.80 to 1.12), P = 0.54) although, consistent with the other association studies, the OR was less than one. Meta-analysis of all available data was undertaken (Figure 1). Zhernakova et al. [21] and Coenen et al. [28] both reported association of the KIAA1109-TENR-IL2-IL21 region with RA in overlapping Dutch case-control cohorts. We used data from the former study, as it was the only one to type rs6822844. The meta-analysis provided very strong (genome-wide) support for rs6822844 playing a role in the development of RA (OR = 0.86 (0.82 to 0.91), P = 8.8 × 10-8). The NARAC GWAS data (OR rs6822844 = 0.84 (0.74-0.96), P = 0.011) [7] were combined with the meta-analysis result, yielding P = 2.1 × 10-8.
Meta-analysis of the KIAA1109-TENR-IL2-IL21 SNP, rs6822844. Combined odds ratio values from data presented in Table 2. There was no evidence for heterogeneity between sample sets (P = 0.25).
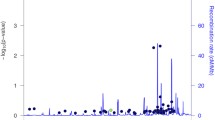
For rs17388568, the genotype data from the WTCCC case-control sample revealed a weak association between rs17388568 and RA, with a susceptibility effect of the minor allele (Table 3; OR = 1.14 (1.04 to 1.25), P = 0.005). We genotyped rs17388568 across the Australasian case-control sample set, finding no evidence for association between rs17388568 and RA (Table 3; OR = 1.03 (0.90 to 1.19), P = 0.66), a result that was consistent with a study of a UK case-control sample set by Barton et al. [12] (Table 3; OR = 0.97 (0.91 to 1.05), P = 0.47). Meta-analysis of all the available data was done (Figure 2), with the combined analysis showing no significant role for rs17388568 in the development of RA (OR = 1.03, (0.98 to 1.09), P = 0.22). At rs907715, the imputed WTCCC genotype data also revealed a weak association (Table 3; OR = 0.92 (0.84 to 1.00), P = 0.055). Genotyping of the Australasian sample set and combined analysis with the WTCCC data (Table 3; Figure 3) slightly weakened the evidence for association of rs907715 with RA (OR = 0.93 (0.87 to 1.00), P = 0.07). Neither rs17388568 nor rs907715 nor any surrogate SNP was present in the NARAC data. Given the moderate LD between rs907715 and rs6822844 (Table 1), rs907715 was tested for association in the combined WTCCC and Australasian samples conditional on genotype at rs6822844. This revealed that the trend towards association seen for rs907715 was not independent of the association seen at rs6822844 (P = 0.38).
Meta-analysis of the KIAA1109-TENR-IL2-IL21 SNP, rs907715. Combined odds ratio values from WTCCC [22] and the Australasian case-control sample sets. There was no evidence for heterogeneity between sample sets (P = 0.48).
The Australasian sample set was further examined by stratifying rs6822844 according to gender, RF, CCP and SE status (Table 4). This revealed no specific association to any particular sub-phenotypes analysed (P > 0.05). It should be noted that the power to detect association with sub-phenotype within the Australasian sample set was limited; for example, in the analysis with the largest amount of data available (RF) there was adequate power (> 70%) to detect an allele frequency difference between RF positive and negative cases only when the difference was equivalent to an OR > 1.5.
Discussion
Here we have combined published studies testing association of two SNPs, rs6822844 and rs17388568, located within the KIAA1109-TENR-IL2-IL21 region with RA: the former with two Dutch [6, 21], one UK [12], and one Western Europe sample set [20]; and the latter with one UK sample set [12] - along with new Australasian data, and data from the WTCCC [22]. Meta-analysis (Figure 1) showed a consistent protective effect for the minor allele of rs6822844 with RA (OR = 0.86, P = 8.8 × 10-8). A similar protective effect was also observed in the NARAC GWAS for rs6822844 (OR = 0.84, P = 0.011), with combined evidence for association with RA of P = 2.1 × 10-8 when combined with our meta-analysis P- value. Our analysis used the same European Caucasian RA sample sets recently meta-analysed by Maita et al. [29], with the addition of the WTCCC, Barton et al. [12], Australasian and NARAC [3] data. Meta-analysis of the T1D-associated SNP rs17385868 (Figure 2) on the other hand, did not reveal any significant association between the minor allele of rs17388568 and RA (OR = 1.03, P = 0.22). Note that SNP rs4505848, in strong LD with rs17385868, is more strongly associated with T1D (Table 1). Whilst there was weak evidence for association at rs907715 (Table 3), in a direction consistent with that previously observed in SLE [17], this effect appears to be dependent on rs6822844. When this paper was under review a genome-wide association scan meta-analysis in RA was published, in 5,539 autoantibody positive cases and 20,169 controls of European descent [30], with P = 7 × 10-4 at rs6822844. We meta-analysed these data with data presented in Table 2 (removing the overlapping WTCCC samples), yielding OR = 0.86 (0.82 to 0.89), P < 1 × 10-10. The rs6822844 data provide compelling evidence supporting a role for the KIAA1109-TENR-IL2-IL21 locus in etiology of RA in Caucasian populations. Including the HLA region and the 10 loci confirmed by Stahl et al. [30] (note that Stahl et al. did not confirm KIAA1109-TENR-IL2-IL21 at a genome-wide level of significance), KIAA1109-TENR-IL2-IL21 is the 20th locus associated with RA at a genome-wide level of significance (P ≤ 5 × 10-8). The association at rs6822844 dominates at this locus, with no evidence for an independent effect at rs17385868, as is seen in T1D (Table 1) [13].
The KIAA1109-TENR-IL2-IL21 region was first implicated in autoimmunity after a GWAS in T1D [13, 22] and has since been associated, also with a genome-wide level of support, with celiac disease [16] and ulcerative colitis [14] and, with lower supporting evidence, with SLE, psoriatic arthritis, Graves' disease and juvenile idiopathic arthritis [13, 17–19] (Table 1). The region is characterized by a high degree of linkage disequilibrium [13], meaning that the underlying disease-causing variant(s) and gene(s) have not yet been determined. Collectively, these data point to at least two independent associations within the KIAA1109-TENR-IL2-IL21 region, with the pattern of association differing between autoimmune phenotypes (Table 1); one marked by rs17388568 (in the TENR gene) and the other by rs6822844 (which maps between IL-2 and IL-21). There is no appreciable linkage disequilibrium between rs17388568 and rs6822844 (r2 = 0.07 in HapMap CEU samples). Different patterns of association are evident in the different autoimmune phenotypes. For example (referring to the risk conferred by the minor allele), susceptibility at rs17388568 and protection at rs6822844 is observed in T1D [13, 21], some evidence for protection is seen at rs17388568 in Graves' disease [13], there is no evidence for association of rs17388568 (or markers in high LD) with RA (Figure 2) whereas rs6822844 confers protection (Table 1). The studies in Crohn's disease, ulcerative colitis, celiac disease, psoriatic arthritis, and JIA are consistent in reporting the rs6822844-mediated minor allele protective effect [14–16, 18, 19] (Table 1), with little data available on rs17388568 in comparison to rs6822844. The single study in SLE [17] did not include SNPs in LD with rs6822844, however there was evidence for a susceptibility effect at rs17388568 (using rs2221903 which is in strong LD with rs17388568, Table 1). Collectively, these studies point to heterogeneity at rs17388568 between RA and other autoimmune phenotypes (T1D, GD, SLE) with which RA shares other genes and clinical features.
Within the KIAA1109-TENR-IL2-IL21 gene cluster, IL-21 is of particular interest in the context of RA, and the Th1/Th17 axis in which IL-23R is involved. IL-21 is required for differentiation of naïve human CD4+ T cells into Th17 cells [31], whereas IL-23 is critical in the expansion and maintenance of Th17 cells [32, 33]. It is important to note that Th17 cells produce a variety of cytokines including IL-17A, IL-17F, IL-21 and IL-22. Human studies have demonstrated that IL-21 receptor (IL-21R)-positive cells are significantly increased in inflamed synovial tissues of RA patients compared to controls and that IL-21 enhances local T-cell activation, proliferation and proinflammatory cytokine secretion [34, 35]. Alongside these findings, animal studies demonstrate that IL-21R deficient mice have normal T-cell and NK cell development but fail to develop spontaneous autoimmune disease suggesting that IL-21 plays a vital role in the development of autoimmune disease in rodents. Studies using arthritic mice and rats also demonstrate that inhibition of IL-21 expression correlates with modulation of serum IL-6 levels and improvements in disease severity [36]. However, it remains to be determined whether inhibition of IL-21 in humans with RA will have a similar beneficial effect given the significant differences between Th17 cell biology in mice and men.
Given the importance of Th17 cells in autoimmunity [37], the differential genetic effects observed in various autoimmune phenotypes mediated by the IL23R and KIAA1109-TENR-IL2-IL21 regions, evidence for genetic interaction between the KIAA1109-TENR-IL2-IL21 region and IL23R (in ulcerative colitis at least) [38], there are reasonable grounds for considering the hypothesis that genetic control of the Th1/Th17 axis is centered on cytokines (and their receptors) important in Th17 biology. It is important to note that not all RA patients have evidence of IL-17A within synovial tissue [39] and the role of IL-17A appears to be as an amplifier of inflammation rather than an absolute requirement for inflammation in RA. One possible explanation is genetic variation in the KIAA1109-TENR-IL2-IL21 locus that results in non-functional IL-21 and hence lack of IL-17A or vice versa. Regulation of this axis may be an important factor in determining the risk to particular autoimmune phenotypes, which may have implications for selection of targeted biological therapies within an individual. What will be important in understanding molecular control of autoimmunity will be association studies in large sample sets from different autoimmune phenotypes that comprehensively capture common variation in the IL23R and KIAA1109-TENR-IL2-IL21 loci, fine-mapping of the genetic effects and analysis of interaction between the disease-associated variants, both within and between loci.
Conclusions
Genotyping of an Australasian RA case-control sample set, and meta-analysis with published and publicly-available data confirm at a genome-wide level of significance the rs6822844 SNP within the KIAA1109-TENR-IL2-IL21 locus to be a risk factor in RA (P = 2.1 × 10-8; OR = 0.86). There was no evidence for an independent effect on RA mediated by other variants within the KIAA1109-TENR-IL2-IL21 locus, as is seen in type 1diabetes.
Abbreviations
- BLK :
-
B-lymphocyte kinase
- CCP:
-
cyclic citrullinated peptide
- GD:
-
Graves' disease
- GWAS:
-
genome-wide association scan
- IL:
-
interleukin
- LD:
-
linkage disequilibrium
- NZ:
-
New Zealand
- OR:
-
odds ratio
- NARAC:
-
North America Rheumatoid Arthritis Consortium
- RA:
-
rheumatoid arthritis
- RF:
-
rheumatoid factor
- SE:
-
shared epitope
- SLE:
-
systemic lupus erythematosus
- SNP:
-
single nucleotide polymorphism
- STAT4 :
-
signal transducer and activator of transcription 4
- T1D:
-
type 1 diabetes
- WTCCC:
-
Wellcome Trust Case Control Consortium
References
Lee YH, Rho YH, Choi SJ, Ji JD, Song GG, Nath SK, Harley JB: The PTPN22 C1858T functional polymorphism and autoimmune diseases--a meta-analysis. Rheumatology (Oxford). 2007, 46: 49-56. 10.1093/rheumatology/kel170.
Plenge RM, Padyukov L, Remmers EF, Purcell S, Lee AT, Karlson EW, Wolfe F, Kastner DL, Alfredsson L, Altshuler D, Gregersen PK, Klareskog L, Rioux JD: Replication of putative candidate-gene associations with rheumatoid arthritis in > 4,000 samples from North America and Sweden: association of susceptibility with PTPN22, CTLA4, and PADI4. Am J Hum Genet. 2005, 77: 1044-1060. 10.1086/498651.
Plenge RM, Cotsapas C, Davies L, Price AL, de Bakker PI, Maller J, Pe'er I, Burtt NP, Blumenstiel B, DeFelice M, Parkin M, Barry R, Winslow W, Healy C, Graham RR, Neale BM, Izmailova E, Roubenoff R, Parker AN, Glass R, Karlson EW, Maher N, Hafler DA, Lee DM, Seldin MF, Remmers EF, Lee AT, Padyukov L, Alfredsson L, Coblyn J, et al: Two independent alleles at 6q23 associated with risk of rheumatoid arthritis. Nat Genet. 2007, 39: 1477-1482. 10.1038/ng.2007.27.
Thomson W, Barton A, Ke X, Eyre S, Hinks A, Bowes J, Donn R, Symmons D, Hider S, Bruce IN, Wellcome Trust Case Control Consortium, Wilson AG, Marinou I, Morgan A, Emery P, YEAR Consortium, Carter A, Steer S, Hocking L, Reid DM, Wordsworth P, Harrison P, Strachan D, Worthington J: Rheumatoid arthritis association at 6q23. Nat Genet. 2007, 39: 1431-1433. 10.1038/ng.2007.32.
Barton A, Thomson W, Ke X, Eyre S, Hinks A, Bowes J, Gibbons L, Plant D, Wellcome Trust Case Control Consortium, Wilson AG, Marinou I, Morgan A, Emery P, YEAR consortium, Steer S, Hocking L, Reid DM, Wordsworth P, Harrison P, Worthington J: Re-evaluation of putative rheumatoid arthritis susceptibility genes in the post-genome wide association study era and hypothesis of a key pathway underlying susceptibility. Hum Mol Genet. 2008, 17: 2274-2279. 10.1093/hmg/ddn128.
Daha NA, Kurreeman FA, Marques RB, Stoeken-Rijsbergen G, Verduijn W, Huizinga TW, Toes RE: Confirmation of STAT4, IL2/IL21, and CTLA4 polymorphisms in rheumatoid arthritis. Arthritis Rheum. 2009, 60: 1255-1260. 10.1002/art.24503.
Plenge RM, Seielstad M, Padyukov L, Lee AT, Remmers EF, Ding B, Liew A, Khalili H, Chandrasekaran A, Davies LR, Li W, Tan AK, Bonnard C, Ong RT, Thalamuthu A, Pettersson S, Liu C, Tian C, Chen WV, Carulli JP, Beckman EM, Altshuler D, Alfredsson L, Criswell LA, Amos CI, Seldin MF, Kastner DL, Klareskog L, Gregersen PK: TRAF1-C5 as a risk locus for rheumatoid arthritis--a genomewide study. N Engl J Med. 2007, 357: 1199-1209. 10.1056/NEJMoa073491.
Chang M, Rowland CM, Garcia VE, Schrodi SJ, Catanese JJ, van der Helm-van Mil AH, Ardlie KG, Amos CI, Criswell LA, Kastner DL, Gregersen PK, Kurreeman FA, Toes RE, Huizinga TW, Seldin MF, Begovich AB: A large-scale rheumatoid arthritis genetic study identifies association at chromosome 9q33.2. PLoS Genet. 2008, 4: e1000107-10.1371/journal.pgen.1000107.
Raychaudhuri S, Remmers EF, Lee AT, Hackett R, Guiducci C, Burtt NP, Gianniny L, Korman BD, Padyukov L, Kurreeman FA, Chang M, Catanese JJ, Ding B, Wong S, van der Helm-van Mil AH, Neale BM, Coblyn J, Cui J, Tak PP, Wolbink GJ, Crusius JB, van der Horst-Bruinsma IE, Criswell LA, Amos CI, Seldin MF, Kastner DL, Ardlie KG, Alfredsson L, Costenbader KH, Altshuler D, et al: Common variants at CD40 and other loci confer risk of rheumatoid arthritis. Nat Genet. 2008, 40: 1216-1223. 10.1038/ng.233.
Orozco G, Eyre S, Hinks A, Ke X, Wilson AG, Bax DE, Morgan AW, Emery P, Steer S, Hocking L, Reid DM, Wordsworth P, Harrison P, Thomson W, Barton A, Worthington J: Association of CD40 with rheumatoid arthritis confirmed in a large UK case-control study. Ann Rheum Dis. 2009
Gregersen PK, Amos CI, Lee AT, Lu Y, Remmers EF, Kastner DL, Seldin MF, Criswell LA, Plenge RM, Holers VM, Mikuls TR, Sokka T, Moreland LW, Bridges SL, Xie G, Begovich AB, Siminovitch KA: REL, encoding a member of the NF-kappaB family of transcription factors, is a newly defined risk locus for rheumatoid arthritis. Nat Genet. 2009, 41: 820-823. 10.1038/ng.395.
Barton A, Eyre S, Ke X, Hinks A, Bowes J, Flynn E, Martin P, YEAR Consortium, BIRAC Consortium, Wilson AG, Morgan AW, Emery P, Steer S, Hocking LJ, Reid DM, Harrison P, Wordsworth P, Thomson W, Worthington J: Identification of AF4/FMR2 family, member 3 (AFF3) as a novel rheumatoid arthritis susceptibility locus and confirmation of two further pan-autoimmune susceptibility genes. Hum Mol Genet. 2009, 18: 2518-2522. 10.1093/hmg/ddp177.
Todd JA, Walker NM, Cooper JD, Smyth DJ, Downes K, Plagnol V, Bailey R, Nejentsev S, Field SF, Payne F, Lowe CE, Szeszko JS, Hafler JP, Zeitels L, Yang JH, Vella A, Nutland S, Stevens HE, Schuilenburg H, Coleman G, Maisuria M, Meadows W, Smink LJ, Healy B, Burren OS, Lam AA, Ovington NR, Allen J, Adlem E, Leung HT, et al: Robust associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet. 2007, 39: 857-864. 10.1038/ng2068.
Festen EA, Goyette P, Scott R, Annese V, Zhernakova A, Lian J, Lefèbvre C, Brant SR, Cho JH, Silverberg MS, Taylor KD, de Jong DJ, Stokkers PC, McGovern D, Palmieri O, Achkar JP, Xavier RJ, Daly MJ, Duerr RH, Wijmenga C, Weersma RK, Rioux JD: Genetic variants in the region harbouring IL2/IL21 associated with ulcerative colitis. Gut. 2009, 58: 799-804. 10.1136/gut.2008.166918.
Márquez A, Orozco G, Martínez A, Palomino-Morales R, Fernández-Arquero M, Mendoza JL, Taxonera C, Díaz-Rubio M, Gómez-García M, Nieto A, López-Nevot MA, de la Concha EG, Martín J, Urcelay E: Novel association of the interleukin 2-interleukin 21 region with inflammatory bowel disease. Am J Gastroenterol. 2009, 104: 1968-1975. 10.1038/ajg.2009.224.
Garner CP, Murray JA, Ding YC, Tien Z, van Heel DA, Neuhausen SL: Replication of celiac disease UK genome-wide association study results in a US population. Hum Mol Genet. 2009, 18: 4219-4225. 10.1093/hmg/ddp364.
Sawalha AH, Kaufman KM, Kelly JA, Adler AJ, Aberle T, Kilpatrick J, Wakeland EK, Li QZ, Wandstrat AE, Karp DR, James JA, Merrill JT, Lipsky P, Harley JB: Genetic association of interleukin-21 polymorphisms with systemic lupus erythematosus. Ann Rheum Dis. 2008, 67: 458-461. 10.1136/ard.2007.075424.
Liu Y, Helms C, Liao W, Zaba LC, Duan S, Gardner J, Wise C, Miner A, Malloy MJ, Pullinger CR, Kane JP, Saccone S, Worthington J, Bruce I, Kwok PY, Menter A, Krueger J, Barton A, Saccone NL, Bowcock AM: A genome-wide association study of psoriasis and psoriatic arthritis identifies new disease loci. PLoS Genet. 2008, 4: e1000041-10.1371/journal.pgen.1000041.
Albers HM, Kurreeman FA, Stoeken-Rijsbergen G, Brinkman DM, Kamphuis SS, van Rossum MA, Girschick HJ, Wouters C, Saurenmann RK, Hoppenreijs E, Slagboom P, Houwing-Duistermaat JJ, Verduijn W, Huizinga TW, Ten Cate R, Toes RE, Schilham MW: Association of the autoimmunity locus 4q27 with juvenile idiopathic arthritis. Arthritis Rheum. 2009, 60: 901-904. 10.1002/art.24296.
Teixeira VH, Pierlot C, Migliorini P, Balsa A, Westhovens R, Barrera P, Alves H, Vaz C, Fernandes M, Pascual-Salcedo D, Bombardieri S, Dequeker J, Radstake TR, Van Riel P, van de Putte L, Lopes-Vaz A, Bardin T, Prum B, Cornélis F, Petit-Teixeira E, European Consortium on Rheumatoid Arthritis Families: Testing for the association of the KIAA1109/Tenr/IL2/IL21 gene region with rheumatoid arthritis in a European family-based study. Arthritis Res Ther. 2009, 11: R45-
Zhernakova A, Alizadeh BZ, Bevova M, van Leeuwen MA, Coenen MJ, Franke B, Franke L, Posthumus MD, van Heel DA, van der Steege G, Radstake TR, Barrera P, Roep BO, Koeleman BP, Wijmenga C: Novel association in chromosome 4q27 region with rheumatoid arthritis and confirmation of type 1 diabetes point to a general risk locus for autoimmune diseases. Am J Hum Genet. 2007, 81: 1284-1288. 10.1086/522037.
Wellcome Trust Case Control Consortium: Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007, 447: 661-678. 10.1038/nature05911.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, Medgser TA, Mitchell DM, Neustadt DH, Pinals RS, Schaller JG, Wilder RL, Hunde GG: The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-324. 10.1002/art.1780310302.
Jones GT, van Rij AM: Regarding "Identification of a genetic variant associated with abdominal aortic aneurysms on chromosome 3p12.3 by genome wide association". J Vasc Surg. 2009, 50: 1246-1247. 10.1016/j.jvs.2009.07.098.
Marchini J, Howie B, Myers S, McVean G, Donnelly P: A new multipoint method for genome-wide association studies by imputation of genotypes. Nature Genetics. 2007, 39: 906-913. 10.1038/ng2088.
PLINK: Whole genome data analysis toolset. [http://pngu.mgh.harvard.edu/~purcell/plink/]
Fisher RA, Mosteller F: Questions and Answers. The American Statistician. 1948, 2: 30-31. 10.2307/2681650.
Coenen MJ, Trynka G, Heskamp S, Franke B, van Diemen CC, Smolonska J, van Leeuwen M, Brouwer E, Boezen MH, Postma DS, Platteel M, Zanen P, Lammers JW, Groen HJ, Mali WP, Mulder CJ, Tack GJ, Verbeek WH, Wolters VM, Houwen RH, Mearin ML, van Heel DA, Radstake TR, van Riel PL, Wijmenga C, Barrera P, Zhernakova A: Common and different genetic background for rheumatoid arthritis and coeliac disease. Hum Mol Genet. 2009, 18: 4195-4203. 10.1093/hmg/ddp365.
Maiti AK, Kim-Howard X, Viswanathan P, Guillén L, Rojas-Villarraga A, Deshmukh H, Direskeneli H, Saruhan-Direskeneli G, Cañas C, Tobön GJ, Sawalha AH, Cherñavsky AC, Anaya JM, Nath SK: Confirmation of an association between rs6822844 at the Il2-Il21 region and multiple autoimmune diseases: evidence of a general susceptibility locus. Arthritis Rheum. 2010, 62: 323-329. 10.1002/art.27222.
Stahl EA, Raychaudhuri S, Remmers EF, Xie G, Eyre S, Thomson BP, Li Y, Kurreeman FA, Zhernakova A, Hinks A, Guiducci C, Chen R, Alfredsson L, Amos CI, Ardlie KG, BIRAC Consortium, Barton A, Bowes J, Brouwer E, Burtt NP, Catanese JJ, Coblyn J, Coenen MJ, Costenbader KH, Criswell LA, Crusius JB, Cui J, de Bakker PI, De Jager PL, Ding B, et al: Genome-wide association study meta-analysis identifies seven new rheumatoid arthritis risk loci. Nature Genetics. 2010
Yang L, Anderson DE, Baecher-Allan C, Hastings WD, Bettelli E, Oukka M, Kuchroo VK, Hafler DA: IL-21 and TGF-beta are required for differentiation of human T(H)17 cells. Nature. 2008, 454: 350-352. 10.1038/nature07021.
Mangan PR, Harrington LE, O'Quinn DB, Helms WS, Bullard DC, Elson CO, Hatton RD, Wahl SM, Schoeb TR, Weaver CT: Transforming growth factor-beta induces development of the T(H)17 lineage. Nature. 2006, 441: 231-234. 10.1038/nature04754.
Veldhoen M, Stockinger B: TGFbeta1, a "Jack of all trades": the link with pro-inflammatory IL-17-producing T cells. Trends Immunol. 2006, 27: 358-361. 10.1016/j.it.2006.06.001.
Jüngel A, Distler JH, Kurowska-Stolarska M, Seemayer CA, Seibl R, Forster A, Michel BA, Gay RE, Emmrich F, Gay S, Distler O: Expression of interleukin-21 receptor, but not interleukin-21, in synovial fibroblasts and synovial macrophages of patients with rheumatoid arthritis. Arthritis Rheum. 2004, 50: 1468-1476. 10.1002/art.20218.
Li J, Shen W, Kong K, Liu Z: Interleukin-21 induces T-cell activation and proinflammatory cytokine secretion in rheumatoid arthritis. Scand J Immunol. 2006, 64: 515-522. 10.1111/j.1365-3083.2006.01795.x.
Young DA, Hegen M, Ma HL, Whitters MJ, Albert LM, Lowe L, Senices M, Wu PW, Sibley B, Leathurby Y, Brown TP, Nickerson-Nutter C, Keith JC, Collins M: Blockade of the interleukin-21/interleukin-21 receptor pathway ameliorates disease in animal models of rheumatoid arthritis. Arthritis Rheum. 2007, 56: 1152-1163. 10.1002/art.22452.
Awasthi A, Kuchroo VK: Th17 cells: from precursors to players in inflammation and infection. Int Immunol. 2009, 21: 489-498. 10.1093/intimm/dxp021.
Glas J, Stallhofer J, Ripke S, Wetzke M, Pfennig S, Klein W, Epplen JT, Griga T, Schiemann U, Lacher M, Koletzko S, Folwaczny M, Lohse P, Göke B, Ochsenkühn T, Müller-Myhsok B, Brand S: Novel genetic risk markers for ulcerative colitis in the IL2/IL21 region are in epistasis with IL23R and suggest a common genetic background for ulcerative colitis and celiac disease. Am J Gastroenterol. 2009, 104: 1737-1744. 10.1038/ajg.2009.163.
Stamp LK, Easson A, Pettersson L, Highton J, Hessian PA: Monocyte derived interleukin (IL)-23 is an important determinant of synovial IL-17A expression in rheumatoid arthritis. J Rheum. 2009, 36: 2403-2408. 10.3899/jrheum.081304.
van Heel DA, Franke L, Hunt KA, Gwilliam R, Zhernakova A, Inouye M, Wapenaar MC, Barnardo MC, Bethel G, Holmes GK, Feighery C, Jewell D, Kelleher D, Kumar P, Travis S, Walters JR, Sanders DS, Howdle P, Swift J, Playford RJ, McLaren WM, Mearin ML, Mulder CJ, McManus R, McGinnis R, Cardon LR, Deloukas P, Wijmenga C: A genome-wide association study for celiac disease identifies risk variants in the region harboring IL2 and IL21. Nat Genet. 2007, 39: 827-829. 10.1038/ng2058.
Romanos J, Barisani D, Trynka G, Zhernakova A, Bardella MT, Wijmenga C: Six new coeliac disease loci replicated in an Italian population confirm association with coeliac disease. J Med Genet. 2009, 46: 60-63. 10.1136/jmg.2008.061457.
Hunt KA, Zhernakova A, Turner G, Heap GA, Franke L, Bruinenberg M, Romanos J, Dinesen LC, Ryan AW, Panesar D, Gwilliam R, Takeuchi F, McLaren WM, Holmes GK, Howdle PD, Walters JR, Sanders DS, Playford RJ, Trynka G, Mulder CJ, Mearin ML, Verbeek WH, Trimble V, Stevens FM, O'Morain C, Kennedy NP, Kelleher D, Pennington DJ, Strachan DP, McArdle WL, et al: Newly identified genetic risk variants for celiac disease related to the immune response. Nat Genet. 2008, 40: 395-402. 10.1038/ng.102.
Barrett JC, Clayton DG, Concannon P, Akolkar B, Cooper JD, Erlich HA, Julier C, Morahan G, Nerup J, Nierras C, Plagnol V, Pociot F, Schuilenburg H, Smyth DJ, Stevens H, Todd JA, Walker NM, Rich SS, The Type 1 Diabetes Genetics Consortium: Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat Genet. 2009
Acknowledgements
We would like to thank all the people who agreed to participate in our study. We also thank the New Zealand Rheumatology Research Network for coordinating the recruitment of RA patients and controls; and Marilyn Merriman, Kerry Rowley, Rachel Rodger, Amanda Phipps-Green, and Dr. Cushla McKinney for their technical and statistical assistance. We thank the Health Research Council of New Zealand and the National Heart Foundation of New Zealand for their financial support of this work. This study makes use of data generated by the Wellcome Trust Case-Control Consortium. A full list of the investigators who contributed to the generation of the data can be found in[22]. Funding for the project was provided by the Wellcome Trust under award 076113.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
JEH-M, MC-X and TRM planned the study design and oversaw its execution. RT provided technical and analytical support. JEH-M, MC-X, ND, PJG, AAH, JH, PBBJ, MN, MDS, AR, GJ and LKS took part in clinical recruitment and data acquisition. JEH-M, MC-X, RT, ND, PJG, AAH, JH, PBBJ, MN, MDS, AR, GJ, LKS and TRM prepared the manuscript.
Jade E Hollis-Moffatt, Michael Chen-Xu contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hollis-Moffatt, J.E., Chen-Xu, M., Topless, R. et al. Only one independent genetic association with rheumatoid arthritis within the KIAA1109-TENR-IL2-IL21 locus in Caucasian sample sets: confirmation of association of rs6822844with rheumatoid arthritis at a genome-wide level of significance. Arthritis Res Ther 12, R116 (2010). https://doi.org/10.1186/ar3053
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar3053