Abstract
Introduction
The gene MICA encodes the protein major histocompatibility complex class I polypeptide-related sequence A. It is expressed in synovium of patients with rheumatoid arthritis (RA) and its implication in autoimmunity is discussed. We analyzed the association of genetic variants of MICA with susceptibility to RA.
Methods
Initially, 300 French Caucasian individuals belonging to 100 RA trio families were studied. An additional 100 independent RA trio families and a German Caucasian case-control cohort (90/182 individuals) were available for replication. As MICA is situated in proximity to known risk alleles of the HLA-DRB1 locus, our analysis accounted for linkage disequilibrium either by analyzing the subgroup consisting of parents not carrying HLA-DRB1 risk alleles with transmission disequilibrium test (TDT) or by implementing a regression model including all available data. Analysis included a microsatellite polymorphism (GCT)n and single-nucleotide polymorphisms (SNPs) rs3763288 and rs1051794.
Results
In contrast to the other investigated polymorphisms, the non-synonymously coding SNP MICA-250 (rs1051794, Lys196Glu) was strongly associated in the first family cohort (TDT: P = 0.014; regression model: odds ratio [OR] 0.46, 95% confidence interval [CI] 0.25 to 0.82, P = 0.007). Although the replication family sample showed only a trend, combined family data remained consistent with the hypothesis of MICA-250 association independent from shared epitope (SE) alleles (TDT: P = 0.027; regression model: OR 0.56, 95% CI 0.38 to 0.83, P = 0.003). We also replicated the protective association of MICA-250A within a German Caucasian cohort (OR 0.31, 95% CI 0.1 to 0.7, P = 0.005; regression model: OR 0.6, 95% CI 0.37 to 0.96, P = 0.032). We showed complete linkage disequilibrium of MICA-250 (D' = 1, r2= 1) with the functional MICA variant rs1051792 (D' = 1, r2= 1). As rs1051792 confers differential allelic affinity of MICA to the receptor NKG2D, this provides a possible functional explanation for the observed association.
Conclusions
We present evidence for linkage and association of MICA-250 (rs1051794) with RA independent of known HLA-DRB1 risk alleles, suggesting MICA as an RA susceptibility gene. However, more studies within other populations are necessary to prove the general relevance of this polymorphism for RA.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a common autoimmune disease characterized by chronic inflammatory changes of joints and inner organs. It is estimated that at least 50% of the risk to develop RA is determined by genetic factors [1]. Considerable efforts have been made to elucidate these genetic factors to better understand the disease. However, even after the advent of genome-wide association studies, only somewhat more than half of the estimated genetic risk for RA has been assigned to specific genetic determinants [2]. There is strong evidence [3–5]. that additional genetic risk factors reside within a genomic region containing the strongest known genetic determinants of RA susceptibility, alleles of the HLA-DRB1 gene. Identification of additional risk factors within the HLA-DRB1 gene region is complicated by the extraordinarily high local linkage disequilibrium (LD): Standard association analyses of genetic variants in candidate gene and genome-wide association studies are prone to confounding due to LD with HLA-DRB1 alleles. Successful identification of additional genetic risk factors in this region needs to account for risk conferred by different HLA-DRB1 alleles. Within the shared epitope (SE) hypothesis, HLA-DRB1 alleles *0101, *0102, *0401, *0404, *0405, *0408, and *1001 are most commonly reported to be associated with risk for RA in European Caucasians [6]. Recently, a new classification of HLA-DRB1 alleles was proposed by du Montcel and colleagues [7], taking into account risk-modifying effects of neighboring amino acids. This classification emerged as especially reproducible and reliable [8].
MICA is located within the same genomic region as HLA-DRB1 (Figure 1). It encodes the protein major histocompatibility complex class I polypeptide-related sequence A. This protein interacts with the C-type lectin activatory receptor NKG2D (also known as KLRK1) found on natural killer cells, γδ T cells, and certain subgroups of αβ T cells. MICA-NKG2D interaction is believed to be important for eliminating infected or tumorous cells [9]. This interaction is also described to increase inflammatory cytokine production and proliferation of a certain subset of T cells. In consequence, implications in autoimmunity have been discussed [9–12]. MICA is expressed in RA synovium but not in osteoarthritis synovium [12]. Local NKG2D expression is induced by tumor necrosis factor and interleukin-15 [12]. These findings make MICA an interesting candidate gene for association studies in RA.
Location of MICA relative to the HLA-DRB1 locus. Despite a distance of more than one megabase from the rheumatoid arthritis risk factor HLA-DRB1 in the major histocompatibility complex (MHC) class II region, there is considerable linkage disequilibrium between markers in both genes. Therefore, HLA-DRB1 status must be considered for interpretation of genetic association data.
The highly polymorphic gene MICA (122 frequency-validated single-nucleotide polymorphisms [SNPs] in SNP database [dbSNP] build 129) was investigated in various RA association studies in different populations. For several SNPs and for a microsatellite marker, associations with protection or risk were shown [4, 13–17]. Results for different MICA variants were not conclusive but point toward association with RA. Heterogeneity between results of these studies may be due at least partially to confounding of results by LD with HLA-DRB1 alleles.
Some studies reported association analyses without controlling for LD of MICA with HLA-DRB1 alleles at all [14, 17]. This makes a conclusion about an independent association of MICA intricate. If association analysis is done under the condition of no significant LD between MICA and HLA-DRB1 alleles [16], the problem prevails: Even weak, non-significant LD may bias MICA association analysis since effect sizes of known HLA-DRB1 risk alleles are considerably large. Other authors restricted analysis to the patient subgroup without HLA-DRB1 risk alleles, ignoring large parts of the data [13]. Alternatively, stratification of data in SE and non-SE subgroups ignores variance of the individual risk of SE alleles within the SE subgroup [15]. In a recent study, case-control pairs were matched 1:1 by HLA-DRB1 genotype to control confounding [4]. However, as a disadvantage of this method, large proportions of typical RA patient and control collections are excluded from analysis since certain HLA-DRB1 genotypes are common in patients but rare in controls and vice versa.
Our aim was to investigate the role of DNA polymorphisms of MICA in French Caucasian RA family trios and in a German Caucasian case-control cohort. Confounding by HLA-DRB1 risk alleles was controlled by analysis of the subgroup negative for known HLA-DRB1 risk alleles and by logistic regression including all data.
Materials and methods
Patients
We analyzed 600 French Caucasian individuals belonging to 200 families grouped in two cohorts of 100 family trios. Characteristics (gender, age at onset, disease duration, erosions, seropositivity, and SE) as well as details on DNA preparation were described previously [18]. Seventy-six percent of French RA index patients were positive for anti-cyclic citrullinated peptide antibodies (CCP+). For case-control analysis, 272 German Caucasians were analyzed. Controls were 182 healthy blood donors (mean age ± standard deviation [SD] was 50 ± 7 years, and 80% were female) from the Institute of Transfusion Medicine, University Hospital Leipzig, Germany, and cases were 90 RA patients from the Medical Clinic IV, University Hospital Leipzig, Germany, with the following characteristics: mean age (± SD) at disease onset was 47.1 ± 15.7 years, mean (± SD) disease duration was 26.7 ± 20.5 years, 92% were RA patients seropositive for rheumatoid factor, and 78% were female. All individuals provided informed consent, and the ethics committees of Hôpital Bicêtre (Kremlin-Bicêtre, AP-HP, France) and of the University of Leipzig (Leipzig, Germany) approved the study.
Genotyping
We investigated three polymorphisms spanning MICA for association with RA. For SNP selection, we required frequency validation, a map weight of 1, and a minor allele frequency exceeding 5% in Caucasians. Among 775 SNPs available within the MICA region in Ensemble version 24, 7 were frequency-validated and had a map weight of 1. Within the promoter region, defined as within 5 kb upstream of the start of the gene, we selected MICA-300 (rs3763288). According to TESS (Transcription Element Search System) [19], MICA-300 co-localizes with a binding site for the transcription factor ETV4. Within the coding region, we selected the non-synonymously coding SNP MICA-250 (rs1051794, Lys196Glu) as validation information for this variant was previously published [20, 21]. In addition, variant MICA-210 (a trinucleotide repeat (GCT)n microsatellite polymorphism within the transmembrane domain) was selected as various associations of this variant with RA were reported previously [15–17, 22].
Genotyping was done by applying single-base extension followed by mass spectrometry ('GenoSNIP') as described [23] but with the following modifications: polymerase chain reaction (PCR) and genotyping primers for MICA-210: CCTTTTTTTCAGGGAAAGTGC, CCTTACCATCTCCAGAAACTGC [22], and bioCCATGTTTCTGCTG(L)TGCTGCT; MICA-300: GGAAGGCTGTGCAGTAATCTAGG, TCCCTTTTCCAGCCTGCC, and bioCTGTGCAGT(L)ATCTAGGCTGAAGG; and MICA-250: AAGGTGATGGGTTCGGGAA, TCTAGCAGAATTGGAGGGAG [21], and bioCTCAGGAC(L)ACGCCGGATT. For the MICA-250 assay, a genotyping primer bioCTCCAGAG [L]TCAGACCTTGGC, differentiating between a paralogue sequence variant of MICA and MICB, was genotyped in 558 (63.8%) samples. This assay always indicated amplification of MICA and never of MICB. PCR products were checked by agarose gel electrophoresis for correct size and sufficient yield. Within the studied population, no Mendel error occurred. No significant departure (P ≤ 0.05) from Hardy-Weinberg equilibrium was observed in controls (French samples: P = 0.240 for non-transmitted chromosomes; German controls: P = 0.233; chi-square test with one degree of freedom).
HLA-DRB1 was genotyped previously using sequence-specific PCR primers and hybridization of PCR products with probes specific for HLA-DRB1 alleles, as described for the French family sample [18] and the German case-control sample [24]. Distribution of HLA-DRB1 alleles can be found in the online supplement (Additional data file 1).
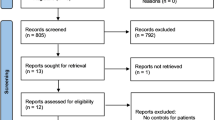
Statistical analysis
For association analysis, we chose a multistep approach. In a first cohort of 100 family trios, selected polymorphisms were tested for association with RA. Those showing nominal association at a significance level of 0.05 or below were tested in a second cohort of 100 French family trios. A decrease in P value in the combined French cohorts was taken as strong evidence in favor of association. These polymorphisms were further analyzed in a German Caucasian case-control cohort.
Haplotypes were estimated using the software HAPLORE (HAPLOtype REconstruction) [25]. For these estimations, data of SNPs located between MICA and HLA-DRB1 were included (rs1800629, rs909253, rs3093553, and rs3093562 for the second French cohort and additionally rs1043618, rs2075800, rs1799964, rs1800630, rs3093662, and rs3093664 for the first French cohort; data available online [26]). We successfully assigned haplotypes for 95% of all families (minimum posterior probability was 90% and mean posterior probability was greater than 99.9%).
Transmission disequilibrium test (TDT) for association and linkage with RA was calculated as described by Spielman and colleagues [27]. For subgroup analyses, the subgroup without HLA-DRB1 risk alleles was defined by the absence of SE alleles. This is identical with allele L according to the classification by du Montcel and colleagues [7]. Derived haplotype information allowed identification of transmitted and non-transmitted chromosomes.
For conditional logistic regression analysis of families, LogXact (Cytel Inc., Cambridge, MA, USA) was used. Within this analysis, HLA-DRB1 allele classification was according to du Montcel and colleagues [7]. The S3P allele consisted of alleles *0101, *0102, *0404, *0405, *0408, and *1001, and the S2 allele consisted of *0401. We applied the convention that allele L denotes alleles S1, S3D, and X as the associated risk for RA of the latter three alleles was found to be of similar magnitude [7, 8]. Of the index patients of all 200 French families, 53% and 45% contributed to allele groups S3P and S2, respectively. Twenty-one percent were homozygous for allele L. In regression analysis, we modeled the transmission probability of a haplotype toward affected children given the competitive haplotype of a parent. This method is known as conditional logistic regression. To include HLA-DRB1 alleles in the model, allele L was used as the reference group. To ensure independence of MICA association from HLA-DRB1 risk alleles, a likelihood ratio test (LRT) was done. Here, the likelihood of the model including HLA-DRB1 alleles and MICA was compared with a model including HLA-DRB1 alleles only. A significant increase of the model's likelihood that includes polymorphism MICA (that is, an LRT P value of less than 0.05) indicates an association of the MICA polymorphism independent of the known association of HLA-DRB1 alleles. Analogously, we checked for interactions between MICA and HLA-DRB1. Additional methodological remarks to this method are given in the online supplement (Additional data file 2).
Within the case-control cohort, haplotyping was not resolvable with the same accuracy as for the family cohorts. Hence, the logistic regression model was based on unphased data of MICA-250 and HLA-DRB1. It included all case-control individuals, accounting for HLA-DRB1 risk alleles. HLA-DRB1 classification according to du Montcel and colleagues [7] as described above was applied. Cases of the case-control cohort contributed to allele groups S3P (42%) and S2 (36%). Twenty-one percent were homozygous for allele L. Within the model, genotypes were coded (0, 1, and 2), with 2 coding for the homozygous minor allele. Thus, an additive model was implemented. LRTs were done similarly to the conditional logistic regression model described above. Multimarker LD analysis was done using the software MIDAS (Multiallelic Interallelic Disequilibrium Analysis Software) [28]. For the exact Mantel-Haenszel test, the software StatsDirect was used [29]. If not indicated otherwise, P values were not corrected for multiple testing.
Results
Association of MICAwith rheumatoid arthritis within the first French family cohort
We analyzed three polymorphisms within the gene MICA: MICA-300 (rs3763288) within the 5' region of the gene (promoter region), MICA-210 (trinucleotide repeat (GCT)n microsatellite polymorphism within the transmembrane domain), and MICA-250 (non-synonymously coding SNP, rs1051794, Lys196Glu).
In standard analysis (TDT without accounting for linkage with HLA-DRB1), we found significant undertransmission of MICA-250A in the first French family cohort (Table 1a). Our first strategy to account for potential LD with HLA-DRB1 was to restrict analysis to parents negative for HLA-DRB1 risk alleles. Here, we also found protective association of MICA-250A and RA (Table 1b). In our second strategy, we controlled for LD with HLA-DRB1 risk alleles by conditional logistic regression. MICA-250A again emerged as a protective factor as haplotypes including MICA-250A were significantly undertransmitted to affected children. The LRT was significant, demonstrating that MICA-250 is associated with RA independent of known HLA-DRB1 risk alleles (Table 1c).
Association of MICA-250 with RA was stronger compared with association of other analyzed single markers (Table 1) and with three-marker haplotypes consisting of MICA-300, MICA-250, and MICA-210 (data not shown). Therefore, only MICA-250 was included in further validation studies within a second independent French Caucasian family cohort and a case-control cohort of German Caucasian origin.
Association analysis within the second and combined first and second French family cohorts
Within the second French family cohort, we found the same trend for protective association of MICA-250A with RA in standard analysis and in both the HLA-DRB1 risk allele-negative subgroup analysis and conditional logistic regression (Table 2). In combined analysis of both French family cohorts, association of MICA-250 was comparable with the association in the first French family cohort in standard analysis and in analysis of the subgroup negative for HLA-DRB1 risk alleles. In conditional logistic regression analysis, association in the combined cohorts was even more significant than in the first cohort alone (Tables 1c and 2c). Additionally, conditional logistic regression was done with a model in which S3P alleles were differentiated into three groups as described [8], accounting for potential differences in risk of these three groups for RA. Within this analysis, 79, 56, and 15 individuals contributed to the S3P*01, S3P*04, and S3P*10 alleles, respectively. This analysis gave similar results (data not shown). Interactions between MICA-250 and HLA-DRB1 alleles were not significant (data not shown). Full details of the regression model are shown in the online supplement (Additional data file 3). When the analysis of the combined first and second French cohorts was restricted to CCP+ RA, the protective association with MICA-250 A was also found (odds ratio [OR] 0.53, 95% confidence interval [CI] 0.33 to 0.83, P = 0.005; LRT P value = 0.003).
Association analysis within the case-control cohort
After demonstrating association of MICA with RA in French Caucasian family trios and its independence from HLA risk alleles, we analyzed the effect of MICA within a German Caucasian case-control cohort. Frequencies of MICA-250A were similar within the German and French populations (33% in controls). Again, we found protective association of MICA-250A with RA in standard analysis and within the subgroup of the case-control cohort not carrying SE alleles (Tables 3a and 3b). Logistic regression including all individuals demonstrated a significant protective effect as well. Significance in the LRT showed that this association was independent of HLA-DRB1 risk alleles (Table 3c). Details of the regression model are given in the online supplement (Additional data file 4). Additionally, conditional logistic regression was done with a model in which S3P alleles were differentiated into three groups (S3P*01, S3P*04, and S3P*10) as described [8], accounting for potential differences of these three groups in risk for RA. This analysis resulted in similar results (data not shown).
Analysis of linkage disequilibrium
LD was analyzed within parents of the family cohorts and in the case-control cohort. As the German cohort was smaller, power to detect LD was decreased compared with power to detect LD within the French cohorts. Significant LD was found between HLA-DRB1-S3P and MICA-250A within parents of the French family cohorts (D' = +0.21, P < 0.001). Interestingly, this LD was positive between HLA-DRB1 risk alleles of subgroup S3P and the protective allele MICA-250A. In-depth analysis of the S3P group revealed that this resulted mainly from LD between HLA-DRB1*01 and MICA-250A, which was significant within parents of the family cohorts and cases from the case-control cohort (D' = +0.38 and +0.25 with P values of 2 × 10-7 and 0.047, respectively). Significant negative LD was found between HLA-DRB1-S2 and MICA-250A (D' = -0.51, P < 0.01) in French parents. No significant LD was found between HLA-DRB1-L within the family cohorts and individuals of the case-control cohort. In consequence, there was no significant correlation of carriage of MICA-250A with carriage of positive or negative SE status. LD was also analyzed between MICA-250 and rs1051792, another coding SNP with functional implications [30]. Within a representative sample of 182 French Caucasian and 181 German Caucasian cases and controls, both polymorphisms were in perfect LD (r2= 1, D' = 1).
Representation of association analysis in all informative families controlling for linkage disequilibrium with HLA-DRB1
An advantage of the conditional logistic regression approach is the integration of all data from all informative parents with respect to HLA-DRB1 and MICA. A single statistic reveals independent association of MICA-250. However, it is of interest to compare subgroup analysis of parents negative for HLA-DRB1 risk alleles with results of the regression model analyzing all data in detail (Tables 2b and 2c). A major difference is that the regression model additionally includes information of parents that are informative (that is, heterozygous) for MICA and that are also heterozygous for HLA-DRB1 risk alleles. How can the effect of MICA-250 on transmission be represented within these parents, devoid of the effect of HLA-DRB1 risk alleles? We propose to stratify HLA-DRB1 heterozygous parents according to their genotype. The transmission ratio under the null hypothesis of no association within these parents will differ from a 50/50 ratio reflecting the different risk levels of both HLA-DRB1 alleles. However, under the null hypothesis of no association of MICA-250, a two-marker haplotype consisting of MICA-250A and a certain HLA-DRB1 allele should have the same transmission rate as a two-marker haplotype consisting of MICA-250G and the same HLA-DRB1 allele. A deviation from this transmission rate represents an independent effect of MICA-250A quantifiable as an OR of MICA-250A transmission. As we applied the classification of du Montcel and colleagues [7] of HLA-DRB1 alleles, three different independent strata of HLA-DRB1 heterozygote parents exist: S3P/S2, S2/L, and S3P/L. Within all of these strata, we always found a decreased transmission of haplotypes carrying MICA-250A compared with the respective haplotype carrying MICA-250G (OR 0.33, 95% CI 0.02 to 5.11; OR 0.45, 95% CI 0.04 to 6.76; and OR 0.44, 95% CI 0.04 to 2.73, respectively, data of all families) (Additional data file 5). These observations are consistent with the significant protective association of MICA-250A revealed by conditional logistic regression (Table 2).
When we additionally include data from parents homozygous for HLA-DRB1, we can analyze the OR of MICA-250A on transmission within these parents when we compare the observed transmission ratio of MICA-250A versus the expected transmission ratio (Additional data file 5). The expected transmission ratio is 50/50 (transmitted/non-transmitted) within these parents under the null hypothesis of no effect of MICA-250A. We now can combine information from all parents informative for MICA-250 by combining all four ORs of all four independent strata with exact Mantel-Haenszel methodology. This analysis confirmed a significant undertransmission of MICA-250A within all data of all families (OR 0.48, 95% CI 0.25 to 0.91, P = 0.02, Fisher exact test).
Discussion
The aim of this study was to analyze the association of polymorphisms of MICA with risk for RA while controlling for the effects of HLA-DRB1 risk alleles. We successfully identified MICA-250A as a new independent marker associated with protection from RA susceptibility. We analyzed the association of three genetic variants of the gene MICA with susceptibility to RA in a French Caucasian family cohort. In validation studies (including an additional independent French Caucasian family cohort and a German Caucasian case-control cohort), we focused on the non-synonymously coding SNP MICA-250 (rs1051794, Lys196Glu). In our first French family cohort, this SNP presented with the strongest evidence for association in terms of P values and transmission rate (Table 1). Association of three-marker haplotypes of MICA with RA was not statistically significant. Therefore, we did not investigate haplotype association further. However, it cannot be excluded that association of MICA-250 with RA may be related to an unknown allelic variant in linkage with these haplotypes as haplotypes were inferred and have error margins.
Within all combined French families, we found a significant undertransmission of MICA-250A in the TDT (Table 2). Therefore, we hereby provide evidence for linkage and association of MICA-250A with RA. This transmission analysis within trio families would not be affected by hidden population stratification. The association was also evident in conditional logistic regression analyses including all parents informative for MICA-250A and controlling for LD with HLA-DRB1 risk alleles (Table 2c). We did not find any indication that the observed protective effect of MICA-250A is especially present on the background of certain HLA-DRB1 alleles as interaction analyses of MICA-250 and HLA-DRB1 alleles in the regression model did not result in a significantly increased likelihood (data not shown). Additionally, detailed transmission analysis of MICA-250 within parents heterozygous or homozygous for HLA-DRB1 always resulted in a protective effect of MICA-250A of comparable magnitude irrespective of present HLA-DRB1 alleles (Additional data file 5). Analysis of the CCP+ subset showed that MICA-250 also associates with CCP+ RA. We confirmed the protective effect in a German Caucasian RA case-control cohort (Table 3), which indicates that the protective effect may not be restricted to the French Caucasian population alone.
True association of MICA-250 with RA may be either feigned or masked by LD with known risk alleles. Therefore, we controlled for the separate contributions of MICA-250 and HLA-DRB1 alleles (S3P, S2, and L) to the observed effect by logistic regression. This allowed us to make use of data from all patients. However, it could be argued that this logistic regression might be affected by stratification of the individual HLA-DRB1 risk alleles in the groups used in the model. Hence, we also analyzed the subgroup of patients not carrying HLA-DRB1 risk alleles. Naturally, this subgroup does not contain data from all patients, but results are completely independent from the excluded HLA-DRB1 risk alleles. Both methods showed association of MICA-250A with RA.
In this context, it is of interest that, within all genome-wide association studies of RA published thus far, MICA-250 was found to be nominally associated: MICA-250A had a protective effect (OR 0.82, 95% CI 0.73 to 0.92, P = 0.0008, not corrected for genome-wide testing) within CCP+ RA in North American samples [31]. Similar findings result from a genome-wide study in a British RA cohort, in which data for an SNP in perfect LD with MICA-250 are available (rs1051792: OR 0.85, 95% CI 0.77 to 0.93, P = 0.0008, not corrected for genome-wide testing) [32]. These findings corroborate our observation of a protective effect of MICA-250A in CCP+ RA. MICA-250 was also associated with RA in a genome-wide study in a Spanish Caucasian cohort (P = 0.02, not corrected for genome-wide testing) [33]. In these genome-wide studies, association analysis was reported without controlling for LD of MICA alleles with HLA-DRB1 alleles. If LD structure in Caucasians in these genome-wide studies was similar to that in our study (that is, if positive LD between HLA-DRB1*0101 and MICA-250A was present), LD-corrected protective association of MICA-250A would be even stronger than reported.
The microsatellite polymorphism MICA-210 was studied in different populations. In Spanish [15] and Canadian [17] Caucasians, a protective effect was seen for allele MICA-210 6.0, whereas in Korean Asians [16], a protective effect was seen for MICA-210 9.0. No association of MICA-210 was seen in another Spanish Caucasian RA study [14]. None of these studies additionally analyzed MICA-250. However, in our study, strong LD between MICA-210 9.0 and MICA-250A was found (D' = 0.98, P < 10-15). Therefore, previous findings in Koreans are in accordance with our results. It is of interest that in this study only a single HLA-DRB1 RA susceptibility allele (*0405) predominates and no LD was found with *0405 and MICA-210 9.0, so that association analysis was hardly influenced by linkage with known HLA-DRB1 risk alleles. This is different from the Caucasian studies of the (GCT)n polymorphism: In our data, we found considerable LD between various MICA-210 alleles and HLA-DRB1 risk alleles (data not shown). We might speculate that complex LD structure between MICA-210 alleles and HLA-DRB1 alleles may at least partially explain differing results in Caucasian association studies of MICA-210 and RA. This is especially relevant as these studies either did not account at all or only partially accounted for LD with HLA-DRB1 alleles.
In recently published work, HLA-DRB1-matched cases and controls were analyzed mainly in American Caucasians in order to identify genetic factors associated with CCP+ RA in addition to known HLA-DRB1 risk alleles [4]. Within the MICA genomic region, significant evidence for independent association with RA was found with a maximum association within HLA-C. This association was attributed to the risk of the A1-B8-DRB1*03 haplotype. Additionally, haplotypes carrying HLA-DRB1*0404 were described to be HLA-DRB1-independent risk factors. An analysis of MICA-250 was not reported in this study. There is evidence that association of MICA-250A in our data represents an additional disease-modifying factor, independent of described risk factors in the American Caucasian study. This evidence results from the observation that a protective association of MICA-250A is still observed when all parents carrying either HLA-DRB1*03 or HLA-DRB1*0404 were excluded (OR 0.56, 95% CI 0.35 to 0.89, P = 0.013; LRT P value = 0.009).
Generally, an observed association of a polymorphism with a phenotype need not arise from a direct functional effect of this polymorphism. It may simply originate from LD with a functional polymorphism. Therefore, it is of interest that the amino acid change due to MICA-250A (Lys196Glu) is predicted to influence Hsp70 binding [34]. Possibly even more relevant, SNP rs1051792, in perfect LD with MICA-250 in Caucasian HapMap data and in our data, was experimentally shown to influence binding of the NKG2D receptor [30]. Variant rs1051792A, corresponding to MICA-250A, was shown to strongly bind NKG2D. All other alleles lead to weaker binding. Several studies show that NKG2D expression is modulated by MICA expression level with consequences for immune reactions. Wiemann and colleagues [35] showed that persistent expression of MICA in transgenic mice resulted in downregulation of the amount of surface NKG2D. As a consequence, impaired immune reaction against bacteria and MICA-expressing tumors was observed. In a different context, Mincheva-Nilsson and colleagues [36] observed elevated levels of soluble MICA/MICB and a decreased level of NKG2D within maternal blood of healthy pregnant women. The authors showed that soluble MICA/MICB downregulates NKG2D levels and immune reactions [36]. Therefore, we speculate that an increased affinity of MICA to NKG2D, as must be present in carriers of MICA-250A, may have similar effects as increased expression of MICA, resulting in decreased NKG2D expression levels.
In this context, the observation of RA remission during pregnancy may be of interest [37]. Apparently, decrease of NKG2D plays a central role in decreased immune response. During pregnancy, this seems to be triggered by increased levels of MICA/MICB and appears to contribute to tolerance against the fetus and disease remission in women with RA. As pregnant women show both downregulation of NKG2D due to increased MICA expression and remission of RA, it can be speculated that there may be a functional link between these two observations. If MICA-250A reports on stronger binding of MICA and if this also results in downregulation of NKG2D levels, this would be consistent with the observed protective effect of MICA-250A in our data. As there are many links between the innate and adaptive immune systems and involvement of pathogens in the initiation of RA is discussed (reviewed by Falgarone and colleagues [38]), differences in NKG2D levels induced by functional variants of MICA are not unlikely to have consequences for RA etiology.
Conclusions
In summary, we present evidence for linkage and association of MICA-250 (rs1051794) with RA independently of known HLA-DRB1 association in French Caucasians and evidence for association in a German Caucasian population, suggesting MICA as an RA susceptibility gene. The association might be explained by functional evidence of rs1051792, an SNP in perfect LD with MICA-250. However, more studies within other populations are necessary to prove the general relevance of this polymorphism with RA.
Abbreviations
- CCP+:
-
positive for anti-cyclic citrullinated peptide antibodies
- CI:
-
confidence interval
- LD:
-
linkage disequilibrium
- LRT:
-
likelihood ratio test
- OR:
-
odds ratio
- PCR:
-
polymerase chain reaction
- RA:
-
rheumatoid arthritis
- SD:
-
standard deviation
- SE:
-
shared epitope
- SNP:
-
single-nucleotide polymorphism
- TDT:
-
transmission disequilibrium test.
References
Turesson C, Weyand CM, Matteson EL: Genetics of rheumatoid arthritis: is there a pattern predicting extraarticular manifestations?. Arthritis Rheum. 2004, 51: 853-863. 10.1002/art.20693.
Barton A, Thomson W, Ke X, Eyre S, Hinks A, Bowes J, Gibbons L, Plant D, Wellcome Trust Case Control Consortium, Wilson AG, Marinou I, Morgan A, Emery P, YEAR consortium, Steer S, Hocking L, Reid DM, Wordsworth P, Harrison P, Worthington J: Re-evaluation of putative rheumatoid arthritis susceptibility genes in the post-genome wide association study era and hypothesis of a key pathway underlying susceptibility. Hum Mol Genet. 2008, 17: 2274-2279. 10.1093/hmg/ddn128.
Jawaheer D, Li W, Graham RR, Chen W, Damle A, Xiao X, Monteiro J, Khalili H, Lee A, Lundsten R, Begovich A, Bugawan T, Erlich H, Elder JT, Criswell LA, Seldin MF, Amos CI, Behrens TW, Gregersen PK: Dissecting the genetic complexity of the association between human leukocyte antigens and rheumatoid arthritis. Am J Hum Genet. 2002, 71: 585-594. 10.1086/342407.
Lee HS, Lee AT, Criswell LA, Seldin MF, Amos CI, Carulli JP, Navarrete C, Remmers EF, Kastner DL, Plenge RM, Li W, Gregersen PK: Several regions in the major histocompatibility complex confer risk for anti-CCP- antibody positive rheumatoid arthritis, independent of the DRB1 locus. Mol Med. 2008, 14: 293-300. 10.2119/2007-00123.Lee.
Newton JL, Harney SM, Timms AE, Sims AM, Rockett K, Darke C, Wordsworth BP, Kwiatkowski D, Brown MA: Dissection of class III major histocompatibility complex haplotypes associated with rheumatoid arthritis. Arthritis Rheum. 2004, 50: 2122-2129. 10.1002/art.20358.
Reviron D, Perdriger A, Toussirot E, Wendling D, Balandraud N, Guis S, Semana G, Tiberghien P, Mercier P, Roudier J: Influence of shared epitope-negative HLA-DRB1 alleles on genetic susceptibility to rheumatoid arthritis. Arthritis Rheum. 2001, 44: 535-540. 10.1002/1529-0131(200103)44:3<535::AID-ANR101>3.0.CO;2-Z.
du Montcel ST, Michou L, Petit-Teixeira E, Osorio J, Lemaire I, Lasbleiz S, Pierlot C, Quillet P, Bardin T, Prum B, Cornelis F, Clerget-Darpoux F: New classification of HLA-DRB1 alleles supports the shared epitope hypothesis of rheumatoid arthritis susceptibility. Arthritis Rheum. 2005, 52: 1063-1068. 10.1002/art.20989.
Morgan AW, Haroon-Rashid L, Martin SG, Gooi HC, Worthington J, Thomson W, Barrett JH, Emery P: The shared epitope hypothesis in rheumatoid arthritis: Evaluation of alternative classification criteria in a large UK Caucasian cohort. Arthritis Rheum. 2008, 58: 1275-1283. 10.1002/art.23432.
Schrambach S, Ardizzone M, Leymarie V, Sibilia J, Bahram S: In vivo expression pattern of MICA and MICB and its relevance to auto-immunity and cancer. PLoS ONE. 2007, 2: e518-10.1371/journal.pone.0000518.
Martin-Pagola A, Perez-Nanclares G, Ortiz L, Vitoria JC, Hualde I, Zaballa R, Preciado E, Castano L, Bilbao JR: MICA response to gliadin in intestinal mucosa from celiac patients. Immunogenetics. 2004, 56: 549-554. 10.1007/s00251-004-0724-8.
Capraru D, Müller A, Csernok E, Gross WL, Holl-Ulrich K, Northfield J, Klenerman P, Herlyn K, Holle J, Gottschlich S, Voswinkel J, Spies T, Fagin U, Jabs WJ, Lamprecht P: Expansion of circulating NKG2D+ effector memory T-cells and expression of NKG2D-ligand MIC in granulomaous lesions in Wegener's granulomatosis. Clin Immunol. 2008, 127: 144-150. 10.1016/j.clim.2007.12.004.
Groh V, Bruhl A, El Gabalawy H, Nelson JL, Spies T: Stimulation of T cell autoreactivity by anomalous expression of NKG2D and its MIC ligands in rheumatoid arthritis. Proc Natl Acad Sci USA. 2003, 100: 9452-9457. 10.1073/pnas.1632807100.
Kochi Y, Yamada R, Kobayashi K, Takahashi A, Suzuki A, Sekine A, Mabuchi A, Akiyama F, Tsunoda T, Nakamura Y, Yamamoto K: Analysis of single-nucleotide polymorphisms in Japanese rheumatoid arthritis patients shows additional susceptibility markers besides the classic shared epitope susceptibility sequences. Arthritis Rheum. 2004, 50: 63-71. 10.1002/art.11366.
López-Arbesu R, Ballina-García FJ, Alperi-López M, López-Soto A, Rodríguez-Rodero S, Martínez-Borra J, López-Vázquez A, Fernández-Morera JL, Riestra-Noriega JL, Queiro-Silva R, Quiñones-Lombraña A, López-Larrea C, González S: MHC class I chain-related gene B (MICB) is associated with rheumatoid arthritis susceptibility. Rheumatology (Oxford). 2007, 46: 426-430. 10.1093/rheumatology/kel331.
Martinez A, Fernandez-Arquero M, Balsa A, Rubio A, Alves H, Pascual-Salcedo D, Martin-Mola E, de la Concha EG: Primary association of a MICA allele with protection against rheumatoid arthritis. Arthritis Rheum. 2001, 44: 1261-1265. 10.1002/1529-0131(200106)44:6<1261::AID-ART217>3.0.CO;2-L.
Mok JW, Lee YJ, Kim JY, Lee EB, Song YW, Park MH, Park KS: Association of MICA polymorphism with rheumatoid arthritis patients in Koreans. Hum Immunol. 2003, 64: 1190-1194. 10.1016/j.humimm.2003.09.010.
Singal DP, Li J, Zhang G: Microsatellite polymorphism of the MICA gene and susceptibility to rheumatoid arthritis. Clin Exp Rheumatol. 2001, 19: 451-452.
Dieude P, Garnier S, Michou L, Petit-Teixeira E, Glikmans E, Pierlot C, Lasbleiz S, Bardin T, Prum B, Cornelis F: Rheumatoid arthritis seropositive for the rheumatoid factor is linked to the protein tyrosine phosphatase nonreceptor 22–620W allele. Arthritis Res Ther. 2005, 7: R1200-R1207. 10.1186/ar1812.
Schug J: Using TESS to predict transcription factor binding sites in DNA sequence. Curr Protoc Bioinformatics. 2008, Chapter 2 (Unit 2.6):
Fodil N, Laloux L, Wanner V, Pellet P, Hauptmann G, Mizuki N, Inoko H, Spies T, Theodorou I, Bahram S: Allelic repertoire of the human MHC class I MICA gene. Immunogenetics. 1996, 44: 351-357. 10.1007/BF02602779.
Powell E, Shi L, Drummond P, Smith EJ: Frequency and distribution in three ethnic populations of single nucleotide polymorphisms in the MICA gene. Mutat Res. 2001, 432: 47-51.
Mizuki N, Ota M, Kimura M, Ohno S, Ando H, Katsuyama Y, Yamazaki M, Watanabe K, Goto K, Nakamura S, Bahram S, Inoko H: Triplet repeat polymorphism in the transmembrane region of the MICA gene: a strong association of six GCT repetitions with Behcet disease. Proc Natl Acad Sci USA. 1997, 94: 1298-1303. 10.1073/pnas.94.4.1298.
Kirsten H, Teupser D, Weissfuss J, Wolfram G, Emmrich F, Ahnert P: Robustness of single-base extension against mismatches at the site of primer attachment in a clinical assay. J Mol Med. 2007, 85: 361-369. 10.1007/s00109-006-0129-2.
Pierer M, Kaltenhauser S, Arnold S, Wahle M, Baerwald C, Hantzschel H, Wagner U: Association of PTPN22 1858 single-nucleotide polymorphism with rheumatoid arthritis in a German cohort: higher frequency of the risk allele in male compared to female patients. Arthritis Res Ther. 2006, 8: R75-10.1186/ar1945.
Zhang K, Sun F, Zhao H: HAPLORE: a program for haplotype reconstruction in general pedigrees without recombination. Bioinformatics. 2005, 21: 90-103. 10.1093/bioinformatics/bth388.
GenHotel – EA3886 Laboratoire de Recherche Européen pour la Polyarthrite Rhumatoïde. [http://www.polyarthrite.info]
Spielman RS, McGinnis RE, Ewens WJ: Transmission test for linkage disequilibrium: the insulin gene region and insulin-dependent diabetes mellitus (IDDM). Am J Hum Genet. 1993, 52: 506-516.
Gaunt TR, Rodriguez S, Zapata C, Day IN: MIDAS: software for analysis and visualisation of interallelic disequilibrium between multiallelic markers. BMC Bioinformatics. 2006, 7: 227-10.1186/1471-2105-7-227.
StatsDirect Statistical Software. [http://www.statsdirect.com]
Steinle A, Li P, Morris DL, Groh V, Lanier LL, Strong RK, Spies T: Interactions of human NKG2D with its ligands MICA, MICB, and homologs of the mouse RAE-1 protein family. Immunogenetics. 2001, 53: 279-287. 10.1007/s002510100325.
Plenge RM, Seielstad M, Padyukov L, Lee AT, Remmers EF, Ding B, Liew A, Khalili H, Chandrasekaran A, Davies LR, Li W, Tan AK, Bonnard C, Ong RT, Thalamuthu A, Pettersson S, Liu C, Tian C, Chen WV, Carulli JP, Beckman EM, Altshuler D, Alfredsson L, Criswell LA, Amos CI, Seldin MF, Kastner DL, Klareskog L, Gregersen PK: TRAF1-C5 as a risk locus for rheumatoid arthritis – a genomewide study. N Engl J Med. 2007, 357: 1199-1209. 10.1056/NEJMoa073491.
Wellcome Trust Case Control Consortium: Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007, 447: 661-678. 10.1038/nature05911.
Julià A, Ballina J, Cañete JD, Balsa A, Tornero-Molina J, Naranjo A, Alperi-López M, Erra A, Pascual-Salcedo D, Barceló P, Camps J, Marsal S: Genome-wide association study of rheumatoid arthritis in the Spanish population: KLF12 as a risk locus for rheumatoid arthritis susceptibility. Arthritis Rheum. 2008, 58: 2275-2286. 10.1002/art.23623.
Reumers J, Maurer-Stroh S, Schymkowitz J, Rousseau F: SNPeffect v2.0: a new step in investigating the molecular phenotypic effects of human non-synonymous SNPs. Bioinformatics. 2006, 22: 2183-2185. 10.1093/bioinformatics/btl348.
Wiemann K, Mittrucker HW, Feger U, Welte SA, Yokoyama WM, Spies T, Rammensee HG, Steinle A: Systemic NKG2D down-regulation impairs NK and CD8 T cell responses in vivo. J Immunol. 2005, 175: 720-729.
Mincheva-Nilsson L, Nagaeva O, Chen T, Stendahl U, Antsiferova J, Mogren I, Hernestal J, Baranov V: Placenta-derived soluble MHC class I chain-related molecules down-regulate NKG2D receptor on peripheral blood mononuclear cells during human pregnancy: a possible novel immune escape mechanism for fetal survival. J Immunol. 2006, 176: 3585-3592.
Keeling SO, Oswald AE: Pregnancy and rheumatic disease: "by the book" or "by the doc". Clin Rheumatol. 2009, 28: 1-9. 10.1007/s10067-008-1031-9.
Falgarone G, Jaen O, Boissier MC: Role for innate immunity in rheumatoid arthritis. Joint Bone Spine. 2005, 72: 17-25. 10.1016/j.jbspin.2004.05.013.
Acknowledgements
We are grateful to the RA patients, their families, control individuals, and rheumatologists for participating in this study. We thank Laetitia Michou for previous work in HLA typing and classification of alleles, Jörg Reichhardt for supporting statistical analysis, Knut M Wittkowski for valuable discussion, and Grit Wolfram for expert technical assistance. This project was supported by grants from the German Federal Ministry for Education and Research 'Hochschul-Wissenschafts-Programm' (to PA), the Saechsische Aufbaubank (7692/1187), the European Fund for Regional Development (EFRE 4212/04-04) (to PA), the German Federal Ministry for Education and Research (01KN0702) (to PA and MS), and the German Federal Ministry for Education and Research (0313909) (to HK). This work was also supported by Association Française des Polyarthritiques, Association Rhumatisme et Travail, Association Polyarctique, Groupe Taitbout, Genopole®, Université Evry-Val d'Essonne, and the European Union (AutoCure).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
HK helped to carry out the molecular genetic studies, performed acquisition of the data, helped to perform analysis and interpretation of the data, and drafted the manuscript. HH and JB helped to carry out the molecular genetic studies. MS, DHe, BP, CP, EP-T, and FC helped to perform analysis and interpretation of the data. DHa and PA helped to perform analysis and interpretation of the data and to draft the manuscript. VHT and UW (and the European Consortium on Rheumatoid Arthritis Families) contributed to the recruitment of families and to the acquisition of clinical data. FE and US helped to draft the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
13075_2008_2523_MOESM2_ESM.pdf
Additional data file 2: Background information for the conditional logistic regression method applied for family based analysis. (PDF 80 KB)
13075_2008_2523_MOESM3_ESM.pdf
Additional data file 3: A table providing detailed results of conditional logistic regression models of all French families. (PDF 11 KB)
13075_2008_2523_MOESM4_ESM.pdf
Additional data file 4: A table providing detailed results of logistic regression models of the German case control cohort. (PDF 21 KB)
13075_2008_2523_MOESM5_ESM.pdf
Additional data file 5: A table providing a representation of association analysis in all informative families controlling for LD with DRB1. (PDF 20 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kirsten, H., Petit-Teixeira, E., Scholz, M. et al. Association of MICA with rheumatoid arthritis independent of known HLA-DRB1risk alleles in a family-based and a case control study. Arthritis Res Ther 11, R60 (2009). https://doi.org/10.1186/ar2683
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar2683