Abstract
Rheumatic diseases are a diverse group of disorders. Most of these diseases are heterogeneous in nature and show varying responsiveness to treatment. Because our understanding of the molecular complexity of rheumatic diseases is incomplete and criteria for categorization are limited, we mainly refer to them in terms of group averages. The advent of DNA microarray technology has provided a powerful tool to gain insight into the molecular complexity of these diseases; this technology facilitates open-ended survey to identify comprehensively the genes and biological pathways that are associated with clinically defined conditions. During the past decade, encouraging results have been generated in the molecular description of complex rheumatic diseases, such as rheumatoid arthritis, systemic lupus erythematosus, Sjögren syndrome and systemic sclerosis. Here, we describe developments in genomics research during the past decade that have contributed to our knowledge of pathogenesis, and to the identification of biomarkers for diagnosis, patient stratification and prognostication.
Similar content being viewed by others
Introduction
Rheumatic diseases are a diverse group of disorders that involve the musculoskeletal system. Generally, the cause of these disorders is unknown and their pathogenesis poorly understood. Although these diseases involve the synovial joints, they also have many systemic features. For example, rheumatoid arthritis (RA) is a chronic inflammatory disease that – in addition to its systemic manifestations – primarily affects the joints. On the other hand, systemic lupus erythematosus (SLE) is a typical systemic disease with secondary involvement of multiple organs.
The aetiology of the rheumatic diseases is largely unknown. Clinical and laboratory observations suggest an immune-mediated attack directed against self-antigens in a number of these diseases. This is highlighted by the association between many of these diseases and human leucocyte antigen (HLA) loci, and by the expression of autoantibodies such as antibodies against nuclear components in SLE, Sjögren's syndrome (SS) and systemic sclerosis (SSc), and rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs) in RA. That these diseases have an immune-mediated background is corroborated by the ameliorative effect of immunosuppressive therapies.
Most of the rheumatic disorders are heterogeneous diseases with a clinical spectrum that ranges from mild to severe, and variability in secondary organ system involvement (for example, heart failure). The heterogeneous nature is reflected by variation in responsiveness to virtually all treatment modalities. The heterogeneity probably has its origin in the mutifactorial nature of the diseases, in which it is likely that specific combinations of environmental factor(s) and varying polygenic background influence not only susceptibility but also severity and disease outcome. The fact that we generally refer to these diseases in terms of group averages may hamper progress in our understanding of pathogenic mechanisms, genetic background and the efficacy of treatment in subsets of patients. Unfortunately, our understanding of the molecular complexity of these disorders is incomplete, and criteria for subtyping patients (for example, in order to select those patients who will benefit from a specific treatment) are currently lacking.
By definition, nearly every aspect of a disease phenotype should be represented in the pattern of genes and proteins that are expressed in the patient. This molecular signature typically represents the contributions made by and interactions between specific factors and distinct cells that are associated with disease characteristics and subtypes, and thus it defines the samples' unique biology. A very powerful way to gain insight into the molecular complexity of cells and tissues has arisen with the advent of DNA microarray technology, which facilitates open-ended survey to identify comprehensively the fraction of genes that are differentially expressed among patients with clinically defined disease. The differentially expressed gene sets may then be used to determine the involvement of a particular biological pathway in disease, and may serve to identify disease classifiers for diagnosis, prognosis, prediction analysis and patient stratification (Figure 1). Hence, the identification of differentially expressed genes and proteins may provide a comprehensive molecular description of disease heterogeneity that can reveal clinically relevant biomarkers.
Schematic outline for genomics in rheumatic diseases. Patients with rheumatic diseases exhibited striking heterogeneity, based on clinical, biological and molecular criteria. Categorization of patients is expected to be of the utmost importance for decision making in clinical practice. Application of high-throughput screening technologies such as genomics allows us to characterize patients based on their molecular profile. The procedure starts with collecting different types of material such as serum, peripheral blood (PB) cells, RNA from blood (using, for example, Paxgene tubes), tissue biopsies and isolated mesenchymal cells from the same patients. Gene expression profiles of this material can be determined using genomics technology. When associated with clinical readouts, we could select the clinically useful molecular markers and apply these in routine clinical practice. In addition, these data may help to elucidate the distinct pathological mechanisms that are at play, potentially explaining the inter-patient variation in clinical presentation, disease progression and treatment response. Ultimately, knowledge of the different pathogenic mechanisms may help us to identify new drug targets for selected patient subgroups.
Initially, several pitfalls were experienced in the use this multistage and relatively expensive technology, which depends critically on perfectly standardized conditions. First of all, handling of blood and tissue samples may differ considerably between laboratories. Usage of different platforms and the lack of standardized procedures limit consistency of study results. For example, variability in the amount and quality of starting RNA; amplification and labelling strategies employed; and dyes, probe sequences and hybridization conditions may all influence the sensitivity, reproducibility and compatibility of datasets. In addition, lack of standardized approaches to normalization and data analysis can influence the outcome of research. Moreover, the high costs associated with use of this technology can impede ability to conduct well powered studies. Therefore, verification of results became an essential step in microarray studies. In order to establish quality criteria for performing and publishing microarray studies, standards for microarray experiments and data analysis were created [1].
Now, after a decade of technical and analytical improvement, the technology and algorithms for data analysis have been shown to be robust and reproducible across properly designed and controlled experiments, and different research groups. The Paxgene (PreAnalytix, GmbH, Germany) whole blood isolation system, which directly lyses cells and stabilizes the RNA in the aspiration tube, excludes ex vivo processing artifacts and forms a crucial step in the standardization of procedures. Although this approach does not a priori account for cell subset differences, the gene expression data generated may provide important information from which extrapolations regarding relative distributions and phenotypic differences can be made. Careful standardization is still required for cell subsets and tissues that are obtained via ex vivo manipulation.
Encouraging results have been generated with the use of microarray technology in the identification of predictors for disease outcome and metastasis, and underlying pathways in breast cancer and lymphoma [2, 3]. The perceived importance and support for large-scale and well powered gene expression profiling studies in oncology have been considerable, and this may account for the success in this area. However, transcriptomics approaches have lagged behind in the field of rheumatology. We believe that collaborative efforts between groups to increase samples size in order to create high-power studies are of critical importance to move the field forward. Equally important is implementation of standardized sample processing procedures and use of the technology, and data analysis and algorithms between different sites. Moreover, to maximize the usage of information from different laboratories, full and open access to genomics data is essential.
Here, we describe novel developments in genomics research conducted to identify biological pathways that contribute to disease and biomarkers for diagnosis, prognosis and patient stratification in rheumatic diseases. An overview of the genomics studies in rheumatic diseases discussed in this review is provided in Table 1. The findings of these studies will also improve our understanding of the underlying biology of the diseases and refine their clinical management. Ultimately, this information may help clinicians to optimise treatment by identifying subgroups of patients who are most likely to respond.
Gene expression profiling in affected target tissues
One of the first studies of gene expression profiles in rheumatic diseases was conducted in RA biopsy tissues, and used a combination of subtractive hybridization and high-density cDNA arrays [4]. This study identified increased expression of genes involved in chronic inflammation, such as immunoglobulins and HLA-DR, in RA synovium as compared with normal synovium. However, because the investigators used pooled tissues from three patients with RA and three healthy control individuals, it was not possible to consider heterogeneity in RA.
Devauchelle and coworkers [5] studied differences in gene expression profiles between the synovial tissue of patients with RA (n = 5) and those with osteoarthritis (OA; n = 10). A total of 63 (48 known genes and 15 expressed sequence tags) were differentially regulated between RA and OA samples.
Comparative analysis of synovial biopsy tissue from RA, OA and SLE patients with active disease partly confirmed and extended previous observations that distinct diseases were characterized by distinct molecular signatures [6]. Whereas genes involved in T-cell and B-cell regulation were upregulated in RA tissues, in SLE tissues IFN-induced genes were more highly expressed and genes involved in homeostasis of the extracellular matrix were downregulated. Histological analysis confirmed that in RA the synovium was characterized by greater numbers of infiltrating T cells and B cells as compared with SLE and OA synovium.
Molecular tissue markers for heterogeneity within rheumatic diseases
Recently, Lindberg and coworkers [7] studied variability in gene expression levels in synovial tissues within and between RA patients. This study demonstrated that different arthro-scopic biopsies taken from one joint yield gene expression signatures that are more similar within the joint of one patient than between patients.
A large-scale gene expression profiling study of synovial tissues from patients with erosive RA revealed considerable heterogeneity between different patients [8, 9]. A systematic characterization of the differentially expressed genes highlighted the existence of at least two molecularly distinct forms of RA tissues. One group exhibited abundant expression of clusters of genes indicative of ongoing inflammation and involvement of the adaptive immune response. This subgroup was referred to as the RA high inflammation group. The increased expression of immunoglobulin genes was shown to be one of the main discriminators between high and low inflammatory tissues. Further analyses of the genes involved in the high inflammation tissues provided evidence for a prominent role for genes indicative of an activated IFN/signal transducer and activator of transcription (STAT)-1 pathway. These findings were confirmed at the protein level [10, 11]. From the 16 genes that overlapped between the microarray used in this study and the one used by Devauchelle and colleagues [5], seven had comparable gene expression profiles (TIMP2, PDGFRA, GBP1, Fos, CTSL, TUBB and BHLHB2). Two of these (GBP1 and CTSL) are known to be regulated by type I IFN.
The expression profiles of the second group of RA tissues were reminiscent of those of tissues from patients with OA. These profiles exhibited a low inflammatory gene expression signature and increased expression of genes involved in tissue remodelling activity, which is associated with fibroblast dedifferentiation. In contrast to the high inflammation tissues, these tissues had increased levels of matrix metalloproteinase (MMP)11 and MMP13 expression, and low expression levels of MMP1 and MMP3 [9].
Histological analyses revealed that the differences observed in global gene expression between the different groups of patients are related to differences in cell distribution. Tissues that contain germinal centre-like structures were selectively found among the high inflammation tissues. The increased immunoglobulin transcript expression is in accordance with the presence of B cells and/or plasma cells, and may reflect local production of antibodies. Increased immunoglobulin transcripts were also found in target tissues of other rheumatic diseases such as SLE [12], SS [13] and SSc [14]. Germinal centre-containing tissues in RA also exhibited enhanced expression of the chemokines C-X-C chemokine ligand-12 and C-C chemokine ligand-19 and the associated receptors C-X-C chemokine receptor-4 and C-X-C chemo-kine receptor-5, which are important for the attraction of T cells, B cells and dendritic cells. Pathway analysis revealed increased expression of genes involved in Janus kinase/STAT signalling, T-cell and B-cell specific pathways, Fc receptor type I signalling in mast cells, and IL-7 signal transduction in the tissues with ectopic lymphoid follicles, accompanied by increased expression of IL-7 receptor α, IL-2 receptor γ chains and IL-7. Protein expression of IL-7 in RA tissues was localized within fibroblast-like synoviocytes, macrophages and blood vessels, and was co-localized with extracellular matrix structures around the B-cell follicles. These findings indicate that activation of the IL-7 pathway may play an important role in lymphoid neogenesis, analogous to its role in the development of normal lymphoid tissue [15]. Tissues with a diffuse type of infiltrate exhibited a profile that indicated repression of angiogenesis and increased extracellular matrix remodelling.
Tsubaki and colleagues [16] demonstrated that tissue heterogeneity within RA can already be observed in the early phase of RA. In this study, gene expression profiles were analyzed from synovial lining tissues from 12 patients with early RA (duration < 1 year after diagnosis) and four with longstanding RA (duration > 3 years after diagnosis). As seen in the previous study using biopsies from longstanding RA patients, the early RA patients could be divided into at least two different groups based on their gene expression profiles.
A study conducted in minor salivary gland tissue from 10 patients with primary SS and 10 healthy control individuals identified 200 genes that were differentially expressed [13]. Clear upregulation of IFN-inducible genes (ISGF3G, IFIT3, G1P2 and IRF1) was identified, besides increased expression of genes related to lymphocyte development and activation, and antigen processing and signal transduction. Other studies confirmed that genes in the IFN pathway were upregulated in salivary glands of SS patients [17, 18].
Upregulated IFN-induced gene expression has also been reported in affected skin of SSc patients [19]. In addition, Milano and coworkers [14] described distinct patterns of gene expression profiles in skin tissues when patients were grouped into those with diffuse SSc and those with limited SSc. Moreover, these data provided evidence for the existence of three different subgroups of patients with SSc: one in those with diffuse SSc and two among those with limited SSc.
Two main subgroups of lupus nephritis biopsies were identified based on clustering of genes with the highest interbiopsy variance [12]. One patient subgroup was characterized by high expression of fibrosis-related genes in the absence of an IFN signature. The other subgroup had high expression of IFN signature genes but low expression of the fibrosis cluster. The clinical features of the patients were not significantly different, although the fibrosis subgroup tended to have higher indices of activity (acute, reversible damage) and chronicity (irreversible damage), whereas the IFN subgroup generally had lower activity/chronicity indices. These results hint at a molecular and biological explanation for severity of renal injury.
Overall, tissue profiling in rheumatic diseases has led to an increase in our understanding of disease pathogenesis. In particular, an IFN signature was observed in target tissues of subsets of patients with RA, SLE, SS and SSc. This provides insights that will facilitate assessment of disease activity and identification of therapeutic targets. Moreover, this information will provide a basis for categorization of patients with rheumatic diseases.
Gene expression in mesenchymal cells derived from affected target tissues
Fibroblasts are ubiquitous mesenchymal cells that play important roles in organ development, inflammation, wound healing, fibrosis and pathology [20]. In chronic inflammation, fibroblasts are considered sentinel cells that contribute to leucocyte migration and local immune response through the production of various immune modulators [21]. These observations suggest that these fibroblasts may acquire the capacity to modulate the immune response [22, 23].
Fibroblast-like synoviocytes (FLSs) are major players in joint destruction in RA. One of the first gene expression profile analyses of FLSs revealed over-expression of genes responsible for tumour-like growth of rheumatoid synovium [24]. In this study a cDNA array membrane containing 588 cDNA fragments of known cancer-related genes was used to compare the gene expression profiles of FLSs from five patients with RA with those of five traumatic control patients. Increased expression levels were found for PDGFRα, PAI-1 and SDF1A in FLSs derived from rheumatoid synovium when compared with normal FLSs. Because the sample size was very small in this study, heterogeneity between FLSs derived from different RA patients was not considered. Other investigators studied the influence of tumour necrosis factor (TNF) on FLSs [25, 26]. TNF has been shown to be of primary importance in the pathogenesis of chronic inflammatory diseases. These studies are instrumental in defining TNF-α response signatures for application in pharmacology studies to monitor the effects of TNF blockade.
We recently profiled FLSs derived from 19 RA patients using microarrays with a complexity of 24,000 cDNA elements. Correlation studies of paired synovial tissue and FLS clustering revealed that heterogeneity at the synovial tissue level is associated with a specific phenotypic characteristic of the cultured resident FLSs [27]. The high inflammation tissues were associated with an FLS subtype that exhibits similarity with so-called myofibroblasts. The myofibroblast is a specialized fibroblast that has acquired the capacity to express α-smooth muscle actin, an actin isoform that is typical of vascular smooth muscle cells. It is now well accepted that the myofibroblast is a key cell for connective tissue remodelling and contributes to cell infiltration. These cells are characterized by a markedly increased expression of genes that represent the transforming growth factor (TGF)-β response programme. Among these response genes were SMA, SERPINE1, COL4A1 (type IV collagen-α chain), IER3 (immediate early response 3), TAGLN (transgelin) and the gene encoding activin A, which is a potential agonist for the induction of the TGF-β response programme. Similar cells were recently identified in the human TNF+/-transgenic mouse model of arthritis [28]. Studies in the field of oncology indicate that myofibroblasts present in tumours play a crucial role in angiogenesis through the production of extracellular matrix proteins, chemokines and growth factors. Hence, it is hypothesized that myofibroblast-like synoviocytes in RA synovial tissue contribute to angiogenesis.
These data support the notion that cellular variation between target tissues is reflected in the stromal cells, and provide evidence for a link between an increased myofibroblast-like phenotype and high inflammation in the target tissue.
Genes characteristically expressed in fibroblasts are differentially expressed between SSc and normal tissue biopsies [29]. Detectable abnormalities in the expression of genes involved extracellular matrix formation, fibrillogenesis, complement activation and angiogenesis are also present in dermal fibroblasts cultured from nonlesional skin of SSc patients [30]. No significant differences in gene expression levels were observed between lesional and nonlesional fibroblasts [31]. The finding that fibroblasts from discordant monozygotic SSc twin pairs were not significantly different indicates that there is a strong genetic predisposition to the SSc phenotype [31].
Gene expression in peripheral blood cells
Although the gene expression analysis of tissue samples of affected organs offers insights into the genes that are instrumental in patient stratification and primarily involved in disease activity and pathogenesis, it is not feasible to use this approach to study large cohorts of patients. Because of the systemic nature of a number of rheumatic diseases and the communication between the systemic and organ-specific compartments, we and others also have studied whole blood and/or peripheral blood mononuclear cells (PBMCs) to obtain disease-related gene expression profiles. The peripheral blood may not have direct implications for our understanding of disease pathogenesis, but it is especially suitable for analyzing gene expression profiles that can be used as biomarkers to permit improved diagnosis and individualized therapy.
Gene expression profiling in the peripheral blood of patients with SLE revealed the presence of an IFN signature in approximately half of the patients studied [32–34]. This signature included well known IFN-regulated genes (for example, the anti-viral MX1 [myxovirus {influenza virus} resistance 1, interferon-inducible protein p78 {mouse}]) as well as additional IFN response genes. The group of patients carrying the IFN signature had a significant higher frequency of certain severe manifestations of disease (renal, central nervous system and haematological involvement) as compared with those who did not. Furthermore, the expression of these genes was significantly correlated with the number of American College of Rheumatology criteria for SLE. Pascual and colleagues [32] also noted that IFN genes were among those most highly correlated with the Systemic Lupus Erythematosus Disease Activity Index. The same molecular signature is found in SLE synovial tissue [6]. The imbalance between IFN molecules and other molecules in SLE synovial tissue might be of interest pathophysiologically during the course of SLE arthritis.
RA has systemic manifestations, and a number of investigators have studied gene expression levels in peripheral blood cells to address the issue of whether disease characteristics correlate with gene expression levels in peripheral blood cells. Bovin and colleagues [35] studied the gene expression profiles of PBMCs in RA patients (n = 14; seven RF positive and seven RF negative) and healthy control individuals (n = 7) using DNA microarrays. Using two independent mathematical methods, 25 genes were selected that discriminated between RA patients and healthy control individuals. These genes reflected changes in the immune/inflammatory responses in RA patients, and among these were the genes encoding the calcium-binding proteins S100A8 and S100A12. No significant differences between RF-positive and RF-negative RA were observed.
Batliwalla and colleagues [36] studied gene expression differences between PBMCs from RA patients (n = 29) and those from healthy control individuals (n = 21). They identified 81 differentially expressed genes, including those encoding glutaminyl cyclase, IL-1 receptor antagonist, S100A12 and Grb2-associated binding protein, as the main discriminators. This profile was associated with increased monocyte count in RA. Szodoray and colleagues [37] studied gene expression differences in peripheral blood B cells from eight RA patients and eight healthy control individuals. A total of 305 genes were upregulated, whereas 231 genes were downregulated in RA B cells. However, the investigators did not address heterogeneity in peripheral blood gene expression profiles among patients with RA.
Olsen and colleagues [38] studied gene expression levels in PBMCs in order to identify differentially expressed genes between early (disease duration < 2 years) and established RA (with an average disease duration of 10 years). Out of 4,300 genes analyzed, nine were expressed at threefold higher levels in the early RA group, including the genes encoding colony stimulating factor 3 receptor, cleavage stimulation factor, and TGF-β receptor II, which affect B-cell function. A total of 44 genes were expressed at threefold lower levels. These genes were involved in immunity and cell cycle regulation. The observation that a quarter of the early arthritis genes overlapped with an influenza-induced gene set led the authors to suggest that the early arthritis signature may partly reflect the response to an unknown infectious agent.
We examined the gene expression profiles of whole blood cells and also identified clear and significant differences between RA patients (n = 35) and healthy individuals (n = 15) [39]. The microarray data confirmed previous observations of increased expression of, for instance, the calcium-binding proteins S100A8 and S100A12. Application of pathway analysis algorithms revealed increased expression of immune defence genes, including type I IFN response genes, which indicates that this pathway is also activated systemically in RA. This type I IFN signature may be a direct reflection of increased activity of type I IFN. However, it cannot be excluded that another ligand known to activate the IFN/STAT-1 pathway is involved. The increased expression of the type I IFN response genes was characteristic of not all but approximately half of the patients. Moreover, the immune defence gene programme that was activated in a subgroup of RA patients was reminiscent of that of poxvirus-infected macaques [40]. This subgroup of RA patients expressed significantly increased titres of anti-cyclic citrullinated peptide antibodies (anti-CCP/ACPA). Based on these findings, we conclude that activation of an immune response, with a type I IFN signature among the gene sets, defines a subgroup of RA patients characterized by increased autoreactivity against citrullinated proteins.
The gene expression analyses in peripheral blood of individuals at high risk for developing RA (RF and/or ACPA positive arthralgia patients) that we performed provide a framework for the identification of predictive biomarkers that may permit identification of individuals who will develop arthritis within 2 years [41].
Tan and coworkers reported increased IFN-response gene expression in SSc [42]. Similar observations were made by York and coworkers [43], who described increased expression of Siglec-1, an IFN-response gene, in both the diffuse and the limited cutaneous type of disease as compared with healthy individuals. Recent findings from our group indicate an association between the IFN response signature and anti-centromer autoantibodies and digital ulcers in SSc [44].
An analysis of significance across several febrile inflammatory disease (44 paediatric systemic onset juvenile idiopathic arthritis [SoJIA], 94 paediatric infections, 38 paediatric SLE, six PAPA [a familial autoinflammatory disease that causes pyogenic sterile arthritis, pyoderma gangrenosum and acne] and 39 healthy children) revealed a SoJIA-specific signature composed of 88 genes in peripheral blood [45].
Common denominators
Upregulation of IFN-response genes has now been observed in peripheral blood cells and/or target tissues of (a subset of) patients with autoimmune diseases such as RA, SLE, SSc, SS, multiple sclerosis and type 1 diabetes. These findings suggest that an activated IFN response gene expression programme is a common denominator in rheumatic diseases, and autoimmune diseases in general.
Type I IFNs, which are the early mediators of the innate immune response that influences the adaptive immune response through direct and indirect actions on dendritic cells (DCs), T and B cells, and natural killer cells, could affect the initiation or amplification of autoimmunity and tissue damage through their diverse and broad actions on almost every cell type and promotion of T-helper-1 responses. It is speculated that the IFN response programme could be associated with activation of immature monocyte-derived DCs, which regulate deletion of autoreactive lymphocytes. Subsequently, IFN-matured DCs may activate autoreactive T cells, leading to autoreactive B-cell development, representing the first level of autoimmunity [46]. Loss of tolerance may lead to autoantibody production. In the case of SLE, autoantigen/autoantibody complexes may trigger pathogen recognition receptors (such as Toll-like receptors) that induce IFN-α production and thereby perpetuate the IFN response programme.
Apart from a role for the IFN response programme as a common denominator in autoimmune diseases, other gene profiles have been identified that are shared by autoimmune diseases. In particular, Maas and colleagues [47] studied the overlap of gene expression profiles between different diseases. They identified 95 genes that were increased and 117 genes that were decreased in the PBMCs of all patients with RA, SLE, type 1 diabetes and multiple sclerosis. These genes were involved in, for example, inflammation, signalling, apoptosis, ubiquitin/proteasome function and cell cycle. Hierarchical cluster analysis on the basis of gene signatures in PBMCs revealed that RA and SLE patients were intermixed with one another. Moreover, they reported that from the genes that were differentially expressed between PBMCs from patients and those from unrelated unaffected individuals, the gene expression profile of 127 genes was shared between patients with autoimmune diseases and unaffected first-degree relatives. This commonality between affected and unaffected first-degree relatives suggests a genetic basis for these shared gene expression profiles. Accordingly, the investigators showed that these genes are clustered in chromosomal domains, supporting the hypothesis that there is some genetic logic to this commonality [48].
Pharmacogenomics in rheumatic diseases
Given the destructive nature of most rheumatic diseases, it would be highly desirable to predict at an early stage the most beneficial treatment for those patients at risk. If we rely solely on clinical or radiographic manifestations, we will probably be responding too late and failing to maximize protection. Ideally, it would be desirable to make predictions on success before the start of therapy. Ultimately, this may lead to a personalized form of medicine, whereby a specific therapy will be applied that is best suited to an individual patient.
TNF antagonists are approved worldwide for the treatment of various rheumatic diseases. Clinical experience indicates that there are 'responders' as well as 'nonresponders', but clear criteria for such classification are still lacking. For RA, treatment is only effective for approximately two-thirds of patients [49], which has attracted interest in the pharmacology and mechanisms of action of the available therapies. We present the results of studies assessing progress in exploiting pharmacogenomics (in particular transcriptomics for disease profiling) and pharmacodynamics to predict response to therapy. The term 'pharmacogenomics' emerged in the late 1990s and pertains to the application of genomics in drug development. 'Pharmacogenomics' is defined as, 'The investigation of variations of DNA and RNA characteristics as related to drug response'. Here, we focus on transcriptomics studies.
Until now a few pharmacogenomics studies have been conducted to gain insight into pharmacodynamics and to identify genes predictive of responsiveness to TNF blockers.
The pharmacogenomics of RA patients (n = 15) before and 1 month after the start of infliximab treatment revealed a similar change in the expression of a pharmacogenomic response gene set in the peripheral blood compartment of all patients treated, irrespective of clinical response. This result indicates that all RA patients exhibit an active TNF response programme that contributes to disease pathogenesis [50].
Lequerre and colleagues [51] studied 13 patients (six responders and seven nonresponders) who began treatment with an infliximab/methotrexate combination. Treatment response, determined after 3 months, was based on a difference in Disease Activity Score using 28 joint counts (DAS28) of 1.2 or more. Gene expression analysis of the PBMCs identified a preselected set of 2,239 transcripts out of 10,000 transcripts screened, which exhibited abnormal expression in at least one out of the 13 patients. Subsequent statistical (t-test and serial analysis of microarrays) analysis identified a total of 41 transcripts, covering a diverse set of proteins and functions, which discriminated between responders and nonresponders. In a validation study conducted in 20 patients (10 responders and 10 nonresponders) and with a set of 20 transcripts, correct classification of 16 out of the 20 patients was found (90% sensitivity and 70% specificity). Koczan and colleagues [52] determined pharmacogenomic differences after 72 hours in 19 RA patients (12 responders and seven nonresponders) using a microarray with a complexity of about 18,400 genuine transcripts after administration of etanercept. They identified an informative set of genes, including NFKBIA, CCLA4, IL8, IL1B, TNFAIP3, PDE4B, PP1R15 and ADM, which are involved in nuclear factor-κB and cAMP signalling, whose expression changes after 72 hours was associated with good clinical responses (DAS28 > 1.2). Comparative analysis did not reveal an overlap between the two gene sets.
Lindberg and colleagues [53] studied synovial tissue gene expression profiles in 10 infliximab-treated patients (three responders, five with moderate response and two non-responders). The data revealed 279 genes that were significantly differentially expressed between the good responding and nonresponding patients (false discovery rate < 0.025). Among the identified genes was that encoding MMP3. Moreover, their data revealed that TNF-α could be an important biomarker for successful infliximab treatment.
We conducted a gene expression profiling study in synovial biopsies from 18 patients (12 responders and six non-responders, based on DAS28 ≥ 1.2 after 16 weeks). Several biological processes related to inflammation that were upregulated in patients who responded to therapy, as compared with those who did not show clinical improvement, were identified. These findings indicate that patients with a high level of tissue inflammation are more likely to benefit from anti-TNF-α treatment [54].
Overall, identification of biomarkers before treatment to predict response to anti-TNF treatment in RA has not yet yielded consistent results. Therefore, additional studies using large cohorts of patients and more stringent response criteria are necessary.
A comparative microarray analysis of PBMCs from eight SoJIA patients without anti-TNF therapy and five SoJIA patients undergoing therapy with infliximab [55] revealed over-expression of IFN-α-regulated genes after TNF blockade. Conversely, the addition of IFN to stimulated human PBMCs inhibits the production of both IL-1 and TNF, and induces the production of IL-1 receptor antagonist [56]. These findings indicate that cross-regulation of type I IFNs and TNF plays an important role in the regulation of pathological inflammatory responses. Because TNF plays a critical role in the pathogenesis of certain rheumatic diseases (such as RA) and because IFN-α plays a pivotal role in another set of diseases (including SLE), the cross-regulation of TNF and IFN might have clinical relevance for the blockade of TNF in, for instance, patients with RA. It is speculated that these results provide a mechanistic explanation for the development of anti-double-stranded DNA antibodies and lupus-like syndrome in patients undergoing anti-TNF therapy. However, recent gene expression studies in whole blood of RA patients before and 1, 2 and 3 months after the start of TNF blockade (infliximab) revealed a variable effect on the expression of IFN response genes upon treatment. Therefore, the positive effect of TNF blockade on IFN is not consistently observed in RA [57].
Conclusion
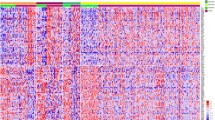
Genomic profiling approaches have fuelled insight to the possibility of finding expression patterns that correlate with disease characteristics and therefore provide a promising tool for future clinical applications. Molecular profiling of blood cells and affected target tissues has already revealed important pathways that contribute to the spectrum of rheumatic diseases (Figure 2). Both disease-specific and subgroup-specific signatures and common signatures are emerging. The latter is reflected by the observation that clinically distinct rheumatic diseases, and even autoimmune diseases in general, all show evidence of a dysregulation of the type I IFN response pathway. Together, the developments support the notion that there is a basis for a molecular subcategorization of clinically defined rheumatic diseases. Moreover, the results indicate that innate immune pathways remain of critical importance throughout the course of rheumatic diseases. The clinical implications of these observations require further definition and independent validation.
Discovery of molecular rheumatic disease subtypes. Schematic overview of the discovery of rheumatic disease subtypes in peripheral blood cells and affected target tissues. Heterogeneity in rheumatic diseases have been demonstrated at peripheral blood as well as tissue level using high-throughput genomics technology. Several studies have described the presence of at least two subgroups of patients based on the presence or absence of an activated type I interferon (IFN) induced gene expression profile in peripheral blood as well as in affected tissues. In addition, peripheral blood cells of rheumatic patients exhibit heterogeneous expression levels for genes involved in granulopoiesis and monocyte activation, as well as for genes encoding the inflammatory S100 proteins. Moreover, subsets of patients exhibit gene expression profiles similar to pathogen-induced profiles. Apart from type I IFN, tissue heterogeneity is reflected at the level of lymphoid neogenesis, fibrosis, myofibroblasts, tissue remodelling and transforming growth factor (TGF)-β signalling. The exact relationship between the peripheral blood profile and tissue profile needs to be further investigated.
Pharmacogenomics studies are just emerging, and the results obtained thus far indicate promise for the future. The finding of biomarkers and gene signatures before the start of targeted therapies paves the way to more individualized treatment strategies. However, caution must be exercised in the interpretation of these results because of small sample sizes and differences in measures of treatment response. To increase the sample sizes, collaborative efforts from different groups are essential. Moreover, agreement on usage of standardized objective measures of treatment responses is of critical importance because this will make data from different studies comparable.
To maximize the usage of information from different laboratories, full and open access to genomics data is important. Moreover, standardization of sample processing procedures and use of the technology, and data analysis and algorithms used are of critical importance. This will ultimately allow a systems biology approach, whereby genomics, proteomics and clinical datasets from different sources are integrated to assign and validate clinically relevant markers that reflect disease pathogenesis (diagnosis), prognosis and heterogeneity, and will facilitate selection of patients with a high likelihood of responding to therapy.
Note
The Scientific Basis of Rheumatology: A Decade of Progress
This article is part of a special collection of reviews, The Scientific Basis of Rheumatology: A Decade of Progress, published to mark Arthritis Research & Therapy's 10th anniversary.
Other articles in this series can be found at: http://arthritis-research.com/sbr
Abbreviations
- ACPA:
-
anti-citrullinated protein antibody
- DAS28:
-
Disease Activity Score using 28 joint counts
- DC:
-
dendritic cell
- FLS:
-
fibroblast-like synoviocyte
- HLA:
-
human leucocyte antigen
- IFN:
-
interferon
- IL:
-
interleukin
- MMP:
-
matrix metalloproteinase
- OA:
-
osteoarthritis
- PBMC:
-
peripheral blood mononuclear cell
- RA:
-
rheumatoid arthritis
- RF:
-
rheumatoid factor
- SLE:
-
systemic lupus erythematosus
- SoJIA:
-
systemic onset juvenile idiopathic arthritis
- SS:
-
Sjögren's syndrome
- SSc:
-
systemic sclerosis
- STAT:
-
signal transducer and activator of transcription
- TNF:
-
tumour necrosis factor.
References
Brazma A, Hingamp P, Quackenbush J, Sherlock G, Spellman P, Stoeckert C, Aach J, Ansorge W, Ball CA, Causton HC, Gaasterland T, Glenisson P, Holstege FC, Kim IF, Markowitz V, Matese JC, Parkinson H, Robinson A, Sarkans U, Schulze-Kremer S, Stewart J, Taylor R, Vilo J, Vingron M: Minimum information about a microarray experiment (MIAME)-toward standards for microarray data. Nat Genet. 2001, 29: 365-371. 10.1038/ng1201-365.
Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A, Boldrick JC, Sabet H, Tran T, Yu X, Powell JI, Yang L, Marti GE, Moore T, Hudson J, Lu L, Lewis DB, Tibshirani R, Sherlock G, Chan WC, Greiner TC, Weisenburger DD, Armitage JO, Warnke R, Levy R, Wilson W, Grever MR, Byrd JC, Botstein D, Brown PO, Staudt LM: Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000, 403: 503-511. 10.1038/35000501.
Vijver van de MJ, He YD, van't Veer LJ, Dai H, Hart AA, Voskuil DW, Schreiber GJ, Peterse JL, Roberts C, Marton MJ, Parrish M, Atsma D, Witteveen A, Glas A, Delahaye L, Velde van der T, Bartelink H, Rodenhuis S, Rutgers ET, Friend SH, Bernards R: A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002, 347: 1999-2009. 10.1056/NEJMoa021967.
Zanders ED, Goulden MG, Kennedy TC, Kempsell KE: Analysis of immune system gene expression in small rheumatoid arthritis biopsies using a combination of subtractive hybridization and high-density cDNA arrays. J Immunol Methods. 2000, 233: 131-140. 10.1016/S0022-1759(99)00126-X.
Devauchelle V, Marion S, Cagnard N, Mistou S, Falgarone G, Breban M, Letourneur F, Pitaval A, Alibert O, Lucchesi C, Anract P, Hamadouche M, Ayral X, Dougados M, Gidrol X, Fournier C, Chiocchia G: DNA microarray allows molecular profiling of rheumatoid arthritis and identification of pathophysiological targets. Genes Immun. 2004, 5: 597-608. 10.1038/sj.gene.6364132.
Nzeusseu TA, Galant C, Theate I, Maudoux AL, Lories RJ, Houssiau FA, Lauwerys BR: Identification of distinct gene expression profiles in the synovium of patients with systemic lupus erythematosus. Arthritis Rheum. 2007, 56: 1579-1588. 10.1002/art.22578.
Lindberg J, af KE, Ulfgren AK, Stark A, Andersson T, Nilsson P, Klareskog L, Lundeberg J: Variability in synovial inflammation in rheumatoid arthritis investigated by microarray technology. Arthritis Res Ther. 2006, 8: R47-10.1186/ar1903.
Pouw Kraan van der TC, van Gaalen FA, Huizinga TW, Pieterman E, Breedveld FC, Verweij CL: Discovery of distinctive gene expression profiles in rheumatoid synovium using cDNA microarray technology: evidence for the existence of multiple pathways of tissue destruction and repair. Genes Immun. 2003, 4: 187-196. 10.1038/sj.gene.6363975.
Pouw Kraan van der TC, van Gaalen FA, Kasperkovitz PV, Verbeet NL, Smeets TJ, Kraan MC, Fero M, Tak PP, Huizinga TW, Pieterman E, Breedveld FC, Alizadeh AA, Verweij CL: Rheumatoid arthritis is a heterogeneous disease: evidence for differences in the activation of the STAT-1 pathway between rheumatoid tissues. Arthritis Rheum. 2003, 48: 2132-2145. 10.1002/art.11096.
Kasperkovitz PV, Verbeet NL, Smeets TJ, van Rietschoten JG, Kraan MC, Pouw Kraan van der TC, Tak PP, Verweij CL: Activation of the STAT1 pathway in rheumatoid arthritis. Ann Rheum Dis. 2004, 63: 233-239. 10.1136/ard.2003.013276.
Lorenz P, Ruschpler P, Koczan D, Stiehl P, Thiesen HJ: From transcriptome to proteome: differentially expressed proteins identified in synovial tissue of patients suffering from rheumatoid arthritis and osteoarthritis by an initial screen with a panel of 791 antibodies. Proteomics. 2003, 3: 991-1002. 10.1002/pmic.200300412.
Peterson KS, Huang JF, Zhu J, D'Agati V, Liu X, Miller N, Erlander MG, Jackson MR, Winchester RJ: Characterization of heterogeneity in the molecular pathogenesis of lupus nephritis from transcriptional profiles of laser-captured glomeruli. J Clin Invest. 2004, 113: 1722-1733.
Hjelmervik TO, Petersen K, Jonassen I, Jonsson R, Bolstad AI: Gene expression profiling of minor salivary glands clearly distinguishes primary Sjogren's syndrome patients from healthy control subjects. Arthritis Rheum. 2005, 52: 1534-1544. 10.1002/art.21006.
Milano A, Pendergrass SA, Sargent JL, George LK, McCalmont TH, Connolly MK, Whitfield ML: Molecular subsets in the gene expression signatures of scleroderma skin. PLoS ONE. 2008, 3: e2696-10.1371/journal.pone.0002696.
Timmer TC, Baltus B, Vondenhoff M, Huizinga TW, Tak PP, Verweij CL, Mebius RE, Pouw Kraan van der TC: Inflammation and ectopic lymphoid structures in rheumatoid arthritis synovial tissues dissected by genomics technology: identification of the interleukin-7 signaling pathway in tissues with lymphoid neogenesis. Arthritis Rheum. 2007, 56: 2492-2502. 10.1002/art.22748.
Tsubaki T, Arita N, Kawakami T, Shiratsuchi T, Yamamoto H, Takubo N, Yamada K, Nakata S, Yamamoto S, Nose M: Characterization of histopathology and gene-expression profiles of synovitis in early rheumatoid arthritis using targeted biopsy specimens. Arthritis Res Ther. 2005, 7: R825-R836. 10.1186/ar1751.
Gottenberg JE, Cagnard N, Lucchesi C, Letourneur F, Mistou S, Lazure T, Jacques S, Ba N, Ittah M, Lepajolec C, Labetoulle M, Ardizzone M, Sibilia J, Fournier C, Chiocchia G, Mariette X: Activation of IFN pathways and plasmacytoid dendritic cell recruitment in target organs of primary Sjogren's syndrome. Proc Natl Acad Sci USA. 2006, 103: 2770-2775. 10.1073/pnas.0510837103.
Hu S, Wang J, Meijer J, Ieong S, Xie Y, Yu T, Zhou H, Henry S, Vissink A, Pijpe J, Kallenberg C, Elashoff D, Loo JA, Wong DT: Salivary proteomic and genomic biomarkers for primary Sjogren's syndrome. Arthritis Rheum. 2007, 56: 3588-3600. 10.1002/art.22954.
Mondini M, Vidali M, De Andrea M, Azzimonti B, Airò P, D'Ambrosio R, Riboldi P, Meroni PL, Albano E, Shoenfeld Y, Gariglio M, Landolfo S: A novel autoantigen to differentiate limited cutaneous systemic sclerosis from diffuse cutaneous systemic sclerosis: the interferon-inducible gene IFI16. Arthritis Rheum. 2006, 54: 3939-3944. 10.1002/art.22266.
Chang HY, Chi JT, Dudoit S, Bondre C, van de RM, Botstein D, Brown PO: Diversity, topographic differentiation, and positional memory in human fibroblasts. Proc Natl Acad Sci USA. 2002, 99: 12877-12882. 10.1073/pnas.162488599.
Smith RS, Smith TJ, Blieden TM, Phipps RP: Fibroblasts as sentinel cells. Synthesis of chemokines and regulation of inflammation. Am J Pathol. 1997, 151: 317-322.
Brouty-Boye D, Pottin-Clemenceau C, Doucet C, Jasmin C, Azzarone B: Chemokines and CD40 expression in human fibroblasts. Eur J Immunol. 2000, 30: 914-919. 10.1002/1521-4141(200003)30:3<914::AID-IMMU914>3.0.CO;2-D.
Hogaboam CM, Steinhauser ML, Chensue SW, Kunkel SL: Novel roles for chemokines and fibroblasts in interstitial fibrosis. Kidney Int. 1998, 54: 2152-2159. 10.1046/j.1523-1755.1998.00176.x.
Watanabe N, Ando K, Yoshida S, Inuzuka S, Kobayashi M, Matsui N, Okamoto T: Gene expression profile analysis of rheumatoid synovial fibroblast cultures revealing the overexpression of genes responsible for tumor-like growth of rheumatoid synovium. Biochem Biophys Res Commun. 2002, 294: 1121-1129. 10.1016/S0006-291X(02)00608-3.
Gallagher J, Howlin J, McCarthy C, Murphy EP, Bresnihan B, FitzGerald O, Godson C, Brady HR, Martin F: Identification of Naf1/ABIN-1 among TNF-alpha-induced expressed genes in human synoviocytes using oligonucleotide microarrays. FEBS Lett. 2003, 551: 8-12. 10.1016/S0014-5793(03)00823-8.
Taberner M, Scott KF, Weininger L, Mackay CR, Rolph MS: Overlapping gene expression profiles in rheumatoid fibroblast-like synoviocytes induced by the proinflammatory cytokines interleukin-1 beta and tumor necrosis factor. Inflamm Res. 2005, 54: 10-16. 10.1007/s00011-004-1315-8.
Kasperkovitz PV, Timmer TC, Smeets TJ, Verbeet NL, Tak PP, van Baarsen LG, Baltus B, Huizinga TW, Pieterman E, Fero M, Firestein GS, Pouw Kraan van der TC, Verweij CL: Fibroblast-like synoviocytes derived from patients with rheumatoid arthritis show the imprint of synovial tissue heterogeneity: evidence of a link between an increased myofibroblast-like phenotype and high-inflammation synovitis. Arthritis Rheum. 2005, 52: 430-441. 10.1002/art.20811.
Aidinis V, Carninci P, Armaka M, Witke W, Harokopos V, Pavelka N, Koczan D, Argyropoulos C, Thwin MM, Möller S, Waki K, Gopalakrishnakone P, Ricciardi-Castagnoli P, Thiesen HJ, Hayashizaki Y, Kollias G: Cytoskeletal rearrangements in synovial fibroblasts as a novel pathophysiological determinant of modeled rheumatoid arthritis. PLoS Genet. 2005, 1: e48-10.1371/journal.pgen.0010048.
Whitfield ML, Finlay DR, Murray JI, Troyanskaya OG, Chi JT, Pergamenschikov A, McCalmont TH, Brown PO, Botstein D, Connolly MK: Systemic and cell type-specific gene expression patterns in scleroderma skin. Proc Natl Acad Sci USA. 2003, 100: 12319-12324. 10.1073/pnas.1635114100.
Tan FK, Hildebrand BA, Lester MS, Stivers DN, Pounds S, Zhou X, Wallis DD, Milewicz DM, Reveille JD, Mayes MD, Jin L, Arnett FC: Classification analysis of the transcriptosome of nonlesional cultured dermal fibroblasts from systemic sclerosis patients with early disease. Arthritis Rheum. 2005, 52: 865-876. 10.1002/art.20871.
Zhou X, Tan FK, Xiong M, Arnett FC, Feghali-Bostwick CA: Monozygotic twins clinically discordant for scleroderma show concordance for fibroblast gene expression profiles. Arthritis Rheum. 2005, 52: 3305-3314. 10.1002/art.21355.
Bennett L, Palucka AK, Arce E, Cantrell V, Borvak J, Banchereau J, Pascual V: Interferon and granulopoiesis signatures in systemic lupus erythematosus blood. J Exp Med. 2003, 197: 711-723. 10.1084/jem.20021553.
Baechler EC, Batliwalla FM, Karypis G, Gaffney PM, Ortmann WA, Espe KJ, Shark KB, Grande WJ, Hughes KM, Kapur V, Gregersen PK, Behrens TW: Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus. Proc Natl Acad Sci USA. 2003, 100: 2610-2615. 10.1073/pnas.0337679100.
Nikpour M, Dempsey AA, Urowitz MB, Gladman DD, Barnes DA: Association of a gene expression profile from whole blood with disease activity in systemic lupus erythaematosus. Ann Rheum Dis. 2008, 67: 1069-1075. 10.1136/ard.2007.074765.
Bovin LF, Rieneck K, Workman C, Nielsen H, Sorensen SF, Skjodt H, Florescu A, Brunak S, Bendtzen K: Blood cell gene expression profiling in rheumatoid arthritis. Discriminative genes and effect of rheumatoid factor. Immunol Lett. 2004, 93: 217-226. 10.1016/j.imlet.2004.03.018.
Batliwalla FM, Baechler EC, Xiao X, Li W, Balasubramanian S, Khalili H, Damle A, Ortmann WA, Perrone A, Kantor AB, Gulko PS, Kern M, Furie R, Behrens TW, Gregersen PK: Peripheral blood gene expression profiling in rheumatoid arthritis. Genes Immun. 2005, 6: 388-397. 10.1038/sj.gene.6364209.
Szodoray P, Alex P, Frank MB, Turner M, Turner S, Knowlton N, Cadwell C, Dozmorov I, Tang Y, Wilson PC, Jonsson R, Centola M: A genome-scale assessment of peripheral blood B-cell molecular homeostasis in patients with rheumatoid arthritis. Rheumatology (Oxford). 2006, 45: 1466-1476. 10.1093/rheumatology/kel095.
Olsen N, Sokka T, Seehorn CL, Kraft B, Maas K, Moore J, Aune TM: A gene expression signature for recent onset rheumatoid arthritis in peripheral blood mononuclear cells. Ann Rheum Dis. 2004, 63: 1387-1392. 10.1136/ard.2003.017194.
Pouw Kraan van der TC, Wijbrandts CA, van Baarsen LG, Voskuyl AE, Rustenburg F, Baggen JM, Ibrahim SM, Fero M, Dijkmans BA, Tak PP, Verweij CL: Rheumatoid arthritis subtypes identified by genomic profiling of peripheral blood cells: assignment of a type I interferon signature in a subpopulation of patients. Ann Rheum Dis. 2007, 66: 1008-1014. 10.1136/ard.2006.063412.
Pouw Kraan van der TC, van Baarsen LG, Wijbrandts CA, Voskuyl AE, Rustenburg F, Baggen JM, Dijkmans BA, Tak PP, Verweij CL: Expression of a pathogen-response program in peripheral blood cells defines a subgroup of rheumatoid arthritis patients. Genes Immun. 2008, 9: 16-22. 10.1038/sj.gene.6364438.
van Baarsen EGM, Bos WH, Rustenburg F, Pouw Kraan van der TCTM, Wolbink GJ, Horst-Bruinsma van der IE, Dijkmans BAC, van Schaardenburg D, Verweij CL: Altered innate immune response in a subgroup of individuals at risk for rheumatoid arthritis [abstract 1206]. Arthritis Rheum. 2008, 58: S616-
Tan FK, Zhou X, Mayes MD, Gourh P, Guo X, Marcum C, Jin L, Arnett FC: Signatures of differentially regulated interferon gene expression and vasculotrophism in the peripheral blood cells of systemic sclerosis patients. Rheumatology (Oxford). 2006, 45: 694-702. 10.1093/rheumatology/kei244.
York MR, Nagai T, Mangini AJ, Lemaire R, van Seventer JM, Lafyatis R: A macrophage marker, Siglec-1, is increased on circulating monocytes in patients with systemic sclerosis and induced by type I interferons and toll-like receptor agonists. Arthritis Rheum. 2007, 56: 1010-1020. 10.1002/art.22382.
Bos CL, van Baarsen LGM, Timmer TCG, Basoski NM, Rustenburg F, Baggen JMC, Thiesen HJ, Dijkmans BAC, Pouw Kraan van der TCTM, Voskuyl AE, Verweij CL: Molecular subtypes of systemic sclerosis in association with anti-centromer antibodies and digital ulcers. Genes Immun. 2009
Allantaz F, Chaussabel D, Stichweh D, Bennett L, Allman W, Mejias A, Ardura M, Chung W, Wise C, Palucka K, Ramilo O, Punaro M, Banchereau J, Pascual V: Blood leukocyte microarrays to diagnose systemic onset juvenile idiopathic arthritis and follow the response to IL-1 blockade. J Exp Med. 2007, 204: 2131-2144.
Banchereau J, Pascual V: Type I interferon in systemic lupus erythematosus and other autoimmune diseases. Immunity. 2006, 25: 383-392. 10.1016/j.immuni.2006.08.010.
Maas K, Chen H, Shyr Y, Olsen NJ, Aune T: Shared gene expression profiles in individuals with autoimmune disease and unaffected first-degree relatives of individuals with autoimmune disease. Hum Mol Genet. 2005, 14: 1305-1314. 10.1093/hmg/ddi141.
Aune TM, Maas K, Parker J, Moore JH, Olsen NJ: Profiles of gene expression in human autoimmune disease. Cell Biochem Biophys. 2004, 40: 81-96. 10.1385/CBB:40:2:081.
Maini R, St Clair EW, Breedveld F, Furst D, Kalden J, Weisman M, Smolen J, Emery P, Harriman G, Feldmann M, Lipsky P: Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial. Lancet. 1999, 354: 1932-1939. 10.1016/S0140-6736(99)05246-0.
van Baarsen EGM, Wijbrandts CA, Rustenburg F, Pouw Kraan van der TCTM, Dijkmans BAC, Tak PP, Verweij CL: Pharmacogenomics of anti-TNF treatment in rheumatoid arthritis reveals an active baseline TNF response profile in all patients [abstract 1650]. Arthritis Rheum. 2008, 58: S776-
Lequerré T, Gauthier-Jauneau AC, Bansard C, Derambure C, Hiron M, Vittecoq O, Daveau M, Mejjad O, Daragon A, Tron F, Le Loët X, Salier JP: Gene profiling in white blood cells predicts infliximab responsiveness in rheumatoid arthritis. Arthritis Res Ther. 2006, 8: R105-10.1186/ar1924.
Koczan D, Drynda S, Hecker M, Drynda A, Guthke R, Kekow J, Thiesen HJ: Molecular discrimination of responders and non-responders to anti-TNFalpha therapy in rheumatoid arthritis by etanercept. Arthritis Res Ther. 2008, 10: R50-
Lindberg J, af KE, Catrina AI, Nilsson P, Klareskog L, Ulfgren AK, Lundeberg J: Effect of infliximab on mRNA expression profiles in synovial tissue of rheumatoid arthritis patients. Arthritis Res Ther. 2006, 8: R179-10.1186/ar2090.
Pouw Kraan van der TC, Wijbrandts CA, van Baarsen LG, Rustenburg F, Baggen JM, Verweij CL, Tak P: Responsiveness to anti-tumour necrosis factor alpha therapy is related to pre-treatment tissue inflammation levels in rheumatoid arthritis patients. Ann Rheum Dis. 2008, 67: 563-566. 10.1136/ard.2007.081950.
Palucka AK, Blanck JP, Bennett L, Pascual V, Banchereau J: Cross-regulation of TNF and IFN-alpha in autoimmune diseases. Proc Natl Acad Sci USA. 2005, 102: 3372-3377. 10.1073/pnas.0408506102.
Rothuizen LE, Buclin T, Spertini F, Trinchard I, Munafo A, Buchwalder PA, Ythier A, Biollaz J: Influence of interferon beta-1a dose frequency on PBMC cytokine secretion and biological effect markers. J Neuroimmunol. 1999, 99: 131-141. 10.1016/S0165-5728(99)00029-6.
van Baarsen EGM, Wijbrandts CA, Rustenburg F, Cantaert T, Pouw Kraan van der TC, Baeten D, Dijkmans B, Tak PP, Verweij CL: IFN/TNF cross-regulation in vivo during infliximab treatment in rheumatoid arthritis [abstract 1356]. Arthritis Rheum. 2008, 58: S670-
Aune TM, Maas K, Moore JH, Olsen NJ: Gene expression profiles in human autoimmune disease. Curr Pharm Des. 2003, 9: 1905-1917. 10.2174/1381612033454360.
Maas K, Chan S, Parker J, Slater A, Moore J, Olsen N, Aune TM: Cutting edge: molecular portrait of human autoimmune disease. J Immunol. 2002, 169: 5-9.
Acknowledgements
We are grateful to Drs Pat Brown and David Botstein, in whose laboratories part of the work described in this report was performed.
Supported in part by the Howard Hughes Medical Institute, EU Marie Curie trainings network EURO-RA, EU-integrated programme AUTO-CURE, and the Centre for Medical Systems Biology (a centre of excellence approved by the Netherlands Genomics Initiative/Netherlands Organization for Scientific Research), and grants from the National Cancer Institute, the Netherlands Organization for Scientific Research (NWO) and the Dutch Arthritis Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The VU University Medical Center has filed a patent applications that is based on the present work (Patent file no. P086657EP00, 'Predicting clinical response to treatment with a soluble TNF-antagonist or TNF, or a TNF receptor agonist'; patent file no. EP08167570.4, 'Preclinical biomarkers for predicting the development of chronic auto-immune diseases'. CL Verweij, W Bos, LGM van Baarsen, D van Schaardenburg). CV and LvB are listed as inventors on the patent applications, and are stakeholders in Preselect Diagnostics BV.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
van Baarsen, L.G., Bos, C.L., Pouw Kraan, T.C.v.d. et al. Transcription profiling of rheumatic diseases. Arthritis Res Ther 11, 207 (2009). https://doi.org/10.1186/ar2557
Published:
DOI: https://doi.org/10.1186/ar2557