Abstract
Osteoarthritis (OA) is characterized by alterations to subchondral bone as well as articular cartilage. Changes to bone in OA have also been identified at sites distal to the affected joint, which include increased bone volume fraction and reduced bone mineralization. Altered bone remodelling has been proposed to underlie these bone changes in OA. To investigate the molecular basis for these changes, we performed microarray gene expression profiling of bone obtained at autopsy from individuals with no evidence of joint disease (control) and from individuals undergoing joint replacement surgery for either degenerative hip OA, or fractured neck of femur (osteoporosis [OP]). The OP sample set was included because an inverse association, with respect to bone density, has been observed between OA and the low bone density disease OP. Compugen human 19K-oligo microarray slides were used to compare the gene expression profiles of OA, control and OP bone samples. Four sets of samples were analyzed, comprising 10 OA-control female, 10 OA-control male, 10 OA-OP female and 9 OP-control female sample pairs. Print tip Lowess normalization and Bayesian statistical analyses were carried out using linear models for microarray analysis, which identified 150 differentially expressed genes in OA bone with t scores above 4. Twenty-five of these genes were then confirmed to be differentially expressed (P < 0.01) by real-time PCR analysis. A substantial number of the top-ranking differentially expressed genes identified in OA bone are known to play roles in osteoblasts, osteocytes and osteoclasts. Many of these genes are targets of either the WNT (wingless MMTV integration) signalling pathway (TWIST1, IBSP, S100A4, MMP25, RUNX2 and CD14) or the transforming growth factor (TGF)-β/bone morphogenic protein (BMP) signalling pathway (ADAMTS4, ADM, MEPE, GADD45B, COL4A1 and FST). Other differentially expressed genes included WNT (WNT5B, NHERF1, CTNNB1 and PTEN) and TGF-β/BMP (TGFB1, SMAD3, BMP5 and INHBA) signalling pathway component or modulating genes. In addition a subset of genes involved in osteoclast function (GSN, PTK9, VCAM1, ITGB2, ANXA2, GRN, PDE4A and FOXP1) was identified as being differentially expressed in OA bone between females and males. Altered expression of these sets of genes suggests altered bone remodelling and may in part explain the sex disparity observed in OA.
Similar content being viewed by others

Introduction
Osteoarthritis (OA) is a complex, multifactorial, age-dependent degenerative disease of the synovial joints. It affects the knee and the hip most commonly, and females at a higher rate than males, particularly after the menopause [1]. OA is characterized by changes to all components of the joint, with degeneration and loss of articular cartilage and changes to the subchondral bone being constant factors in disease progression [2]. Along with the breakdown of the cartilage and joint space narrowing, there is thickening and sclerosis of subchondral bone, development of cysts and bony overgrowth at the margins of the joint. Despite an increase in bone volume fraction, the subchondral bone is mechanically weaker in OA because of hypomineralization, increased collagen metabolism and altered bone remodelling [3, 4]. Evidence from animal models of OA suggests that the changes in the density and metabolism of subchondral bone develop concomitantly with the signs of cartilage damage [5–7]. In addition, there is now evidence in animal OA models that antiresorptive agents, which inhibit subchondral bone remodelling, also prevent the bone changes and loss of cartilage seen in OA, thus reducing joint damage [8, 9]. A human trial of an antiresorptive agent also showed clear trends toward improvement in both joint structure and symptoms in patients with primary knee OA [10]. These findings are consistent with the hypothesis that OA is a bone disease, rather than – or in addition to – a cartilage disease, and that the structural and compositional changes seen in OA subchondral bone, brought about by altered bone remodelling, contribute to the breakdown of the articular cartilage at the joint [11–14].
There is also evidence that the osteoblasts in subchondral bone can influence chondrocyte and cartilage metabolism more directly, leading to abnormal remodelling of OA cartilage [15, 16]. In articular joints there is a complex juxtaposition of vascular elements, subchondral bone and the different cartilage layers, with important communication between these tissues [17]. These observations point to a clear interplay between bone and cartilage at articular joints and show that these tissues represent a functional cellular and molecular unit [18]. Altered angiogenesis could also be contributing to the changes seen in OA bone and cartilage, because important inter-relationships between bone remodelling, chondrogenic and angiogenic processes are now emerging [19–21].
In addition to the changes observed in subchondral bone, there is growing evidence for generalized involvement of bone in the pathogenesis of OA. Studies investigating bone at sites distal to the joint cartilage degeneration, such as the intertrochanteric (IT) and medial principal compressive regions of the proximal femur, and the iliac crest, have yielded evidence of altered bone composition and increased bone volume in OA compared with control individuals [22–25]. It has been proposed that these structural and compositional changes reflect systemic differences in OA bone remodelling compared with control bone, and when these changes operate in subchondral bone they can contribute to the breakdown of the articular cartilage and eventual failure of the joint [11–14]. Furthermore, an inverse association between OA and the low bone density disease osteoporosis (OP) has been observed. OA patients rarely proceed to osteoporotic fracture, suggesting that OA has a protective effect on progression of OP. Conversely, OA is reported to be rare in OP individuals [26].
The structural and compositional changes seen in OA bone are likely to have considerable genetic input because there is a significant heritable component to OA, as judged by genetic studies [27]. Interestingly, many of the candidate susceptibility genes for OA identified by genetic screening approaches have bone-related functions, further suggesting the involvement of bone in OA. Primary OA candidate genes identified, with bone-related functions, include COL1A1, VDR, ESR1, IGF1, SFRP3, BMP5 and TGFB1 [27–30]. SFRP3 encodes a decoy receptor for WNT (wingless MMTV integration) ligands and plays a role in osteoblast differentiation [31]. The WNT signalling pathway is a major developmental pathway that is involved in cell fate, differentiation and proliferation. This signalling pathway has also been linked to skeletal development and bone pathologies such as OP [32]. The identification of TGFB1 and BMP5, a member of the transforming growth factor (TGF)-β superfamily, as OA susceptibility loci has implicated the TGF-β/BMP signalling pathway in OA pathogenesis. The TGF-β/BMP signalling pathway plays important roles in development, cell proliferation and differentiation, and it has also been shown to influence bone mass and bone remodelling [33, 34].
Complementing the human genetic studies described above, and in support of altered bone remodelling at sites distal to the active subchondral disease site, we previously identified differences in the expression of known skeletally active genes in human trabecular bone obtained from the IT region from individuals with hip OA, as compared with bone from the same site in control individuals. Genes identified as differentially expressed include downregulated osteoclastogenic factor genes (RANKL, RANK, IL6 and IL11) and upregulated bone formation marker genes (ALPL, BGLAP, SPP1 and COL1A2) [35–37]. Others have identified in OA individuals altered levels of insulin-like growth factor-1, insulin-like growth factor-2 and TGF-β1 in cortical bone from the iliac crest [38]; matrix metalloproteinase (MMP)2 and liver alkaline phosphatase in subchondral bone [4]; and IL-1β, IL-6 and TGF-β1 in human primary subchondral osteoblasts [39].
In the present study, we used microarray analysis to survey comprehensively the expression levels of many thousands of genes simultaneously in trabecular bone from the IT region of the proximal femur and to compare gene expression in bone from OA, control and OP individuals. We identified altered expression of WNT and TGF-β/BMP signalling pathway and target genes in OA bone. The genes include those with known or suspected roles in osteoblast, osteocyte and osteoclast differentiation and function, supporting a role for altered bone remodelling in OA pathogenesis.
Materials and methods
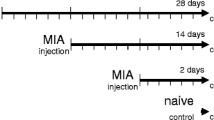
Human bone samples
For the OA and OP groups, tube saw bone biopsies (10 mm diameter and 20 to 40 mm long) were obtained from the IT region of the proximal femur. These were obtained from 24 patients (14 females [age range 49 to 83 years] and 10 males [50 to 85 years]) undergoing hip arthroplasty for primary OA and from 10 patients (10 females [74 to 87 years]) undergoing hip arthroplasty for a fractured neck of femur (designated OP). For the control group, trabecular bone from the IT region was obtained during 21 autopsies (11 females [43 to 85 years] and 10 males [50 to 85 years]) of individuals who were known not to have suffered from any chronic condition or disease that may have affected the skeleton. In selecting the OA, OP and control individuals, those with a known history of medication that might have affected bone metabolism were excluded. Informed consent was obtained for the collection of these specimens, with approval from the Royal Adelaide Hospital Research Ethics Committee (protocol number 030309).
The surgical and autopsy femoral heads were graded for OA according to the criteria of Collins [40]. Primary OA femoral heads were either grade III or IV, and the graded autopsy femoral heads were not worse than grade II and predominantly were grade I. Surgical IT trabecular bone specimens from OA and OP individuals were collected within 12 to 24 hours (stored at 4°C in sterile RNase-free phosphate-buffered saline). Control bone was collected within 24 to 72 hours after death.
Trabecular bone in the IT region of the proximal femur, including the marrow, was sampled, permitting analysis of the total contribution of the bone microenvironment. The IT region was also chosen because the trabecular structure in this region depends on stresses in the proximal femoral shaft, while being unaffected by the secondary sclerotic and cystic changes that are often seen in the OA femoral head as the destruction of the cartilage proceeds. By comparing the OA and OP samples with control samples, the contribution to changes in gene expression associated with surgery as opposed to autopsy could be assessed.
RNA extraction
For total RNA extraction, the trabecular bone samples were rinsed briefly in diethylpyrocarbonate-treated water and then separated into small fragments, containing bone and bone marrow, using bone cutters. Total RNA was extracted as described previously [35, 41]. Briefly, bone fragments were placed in 4 mol/l guanidinium thiocyanate solution and homogenized using an Ultra-Turrax (TP 18–10; Janke & Kunkel, IKA-WERK, Staufen, Germany), and the mixture was clarified by centrifugation (1,000 × g for 5 min). After addition of 0.1 vol of 2 mol/l sodium acetate (pH 4.0), the mixture was vortexed and the RNA extracted with 1 vol of phenol and 0.2 vol of chloroform/isoamylalcohol (49:1). Total RNA was precipitated with isopropanol, resuspended in 1 × 10 mmol/l Tris-HCl/1 mmol/l EDTA containing 0.1 vol of 3 mol/l sodium acetate (pH 5.2) and then re-extracted with 0.5 vol phenol, followed by 0.5 vol chloroform/isoamylalcohol. The RNA was then precipitated with 3 vol of 4 mol/l sodium acetate (pH 7.0), to remove contaminating proteoglycans, at -20°C overnight. Total RNA was recovered by centrifugation, washed with 75% ethanol, air dried, dissolved in diethylpyrocarbonate-treated water, and stored at -80°C until further use. RNA concentration and purity (260/280 absorbance ratio) were determined by spectrophotometry. RNA integrity was confirmed by visualization on ethidium bromide stained 1% weight/vol agarose-formaldehyde gels.
Microarray
RNA was further purified using RNeasy columns (Qiagen, Hilden, Germany), in accordance with the manufacturer's instructions. RNA (5 μg) was amplified using a Message Amp II kit (Ambion, Austin, TX, USA) with indirect, amino allyl mediated incorporation of either Cy3 or Cy5 dyes (Amersham Biosciences, Piscataway, NJ, USA), in accordance with the manufacturer's instructions. A Compugen Human 19K-oligo library (Jamesburg, NJ, USA) spotted onto Corning glass slides (Lowell, MA, USA) by the Adelaide Microarray facility (AMF) was used in this study. The Compugen human oligo library consisted of 17,260 oligonucleotide 65-mers each representing a single human gene. The slides were interrogated by competitive hybridization with 5 μg each of Cy3 and Cy5 labelled pairs of OA-control, OA-OP, or OP-control amplified RNA samples. The sample pairs used in the microarray analysis are listed in Table 1. Sample pairs were age-matched as closely as possible.
A biological dye-swap strategy was employed rather than a replicate dye swap strategy. This involved swapping of Cy3 and Cy5 labelling of the samples in each pair for each group of paired samples to balance for potential dye incorporation and signal intensity bias. It also reduced the number of slides required for the experiment and maximized the statistical power of the experiment with regard to analyzing the biological differences between samples.
Hybridization and washing of slides was carried out according to methods described on the AMF website [42]. The microarray slides were scanned twice at slightly different PMT voltage using a GenePix 4000B Scanner driven by GenePix Pro 4.0 (Axon Instruments, Foster City, CA, USA). All analyses were performed using the statistical programming and graphics environment R [43]. The 'SPOT' software package [44] was used to identify spots using the adaptive segmentation method and subtract backgrounds utilizing the morphological opening approach [45, 46]. Data analysis was performed in R using Bioconductor [47]. The Loess print tip method was used to correct for dye bias and intensity within each group of adjacent spots printed by one pin [48]. Linear modelling was performed using the linear models for microarray analysis (LIMMA) package of Bioconductor [49]. Differentially expressed genes were ranked on moderated t statistics, and those with t scores above 3 were followed up further. The moderated t-statistic score is based on the ratio of the log2 fold change to its standard error. Because there is no consensus on appropriate adjustment of P values in the context of microarrays, genes of interest were chosen based on a combination of statistical and biological indicators. Microarray data have been deposited in the Gene Expression Omnibus [50] and are accessible through Gene Expression Omnibus series number GSE8406.
Real-time PCR
First-strand reverse transcription cDNA synthesis was performed on 1 μg amplified RNA from each sample using a first-strand cDNA synthesis kit with Superscript II (Invitrogen, Carlsbad, CA, USA) and 250 ng random hexamer primer (Geneworks, Adelaide, SA, Australia), in accordance with the manufacturer's instructions. Template cDNA (1 μl of 1/100 dilution of cDNA) was amplified using iQ SYBR Green Supermix (BioRad, Hercules, CA, USA) on a Rotor-Gene thermocycler (Corbett Research, Mortlake, NSW, Australia). The reactions were incubated at 94°C for 10 min for 1 cycle, and then 94°C (20 seconds), 60°C, or 65°C (ADAMTS4 and MMP25 only; 20 seconds) and 72°C (30 seconds) for 40 cycles. This set of cycles was followed by an additional extension step at 72°C for 5 minutes. All PCR reactions were validated by the presence of a single peak in the melt curve analysis, and amplification of a single specific product was further confirmed by electrophoresis on a 2.5% weight/vol agarose gel. Primers were designed for each gene that primed in separate exons and spanned at least one intron to avoid contaminating amplification from genomic DNA. Primers were obtained from Geneworks. Amplicons were designed to be in the 100 to 200 base pairs size range. GenBank accession numbers for gene sequences and primer sequences are provided in Table 2. Real-time PCR validation was carried out using the 2-ΔΔCT method [51]. Reactions were performed in duplicate. Normalized gene expression values for each gene based on cycle threshold (CT) values for each of the genes and the housekeeping gene GAPDH were generated. Mean ± standard deviation (SD) values were generated from eight samples from each group of either OA or control samples tested.
Statistical analysis
The statistical significance of the differences between the means of the OA and control or OP gene expression values was determined using Student's t-test. The critical value for significance was chosen as P < 0.05.
Results
Microarray analysis of OA, control and OP bone samples
This study used Compugen human 19K-oligo human microarray slides to compare the gene expression profiles of OA, control and OP bone samples, with the aim being to identify altered gene expression in OA bone. Microarray analysis was conducted in four sets of samples (39 comparisons in total), comprising 10 OA-control female sample pairs, 10 OA-control male sample pairs, 10 OA-OP female sample pairs and 9 OP-control female sample pairs. Samples from individuals with a range of ages were analyzed in each group, but with sample pairs age-matched as closely as possible (Table 1). Bayesian statistical analysis was carried out using LIMMA to identify statistically significant differentially expressed genes between OA, control and OP bone. Log odds score versus log2 fold change volcano plots of differentially expressed genes from each of the four groups of sample pair comparisons are shown in Figure 1. The log odds (or B statistic) score is the log odds that that gene is differentially expressed. The log2 fold change represents the fold change in expression of the gene. Small levels of differential expression (ranging from 0.38-fold to 2.83-fold change in expression) were detected, with several hundred differentially expressed genes present in each grouping, with t scores above 6. The moderated t-statistic score is based on the ratio of the log2 fold change to its standard error.
Bayesian statistical analysis of differentially expressed genes using LIMMA. Log odds (LOD) score versus log2 fold change volcano plots of differentially expressed genes from each of the four groups of sample pair comparisons. CTL, control; LIMMA, linear models for microarray analysis; OA, osteoarthritis; OP, osteoporosis.
Identification and functional classification of top-ranking differentially expressed genes in OA bone
By comparing the lists of ranked differentially expressed genes from each of the four initial groupings, we were able to identify a group of differentially expressed genes that was more likely to be associated with the OA disease process. This group of genes was assembled by filtering out genes that were similarly regulated between OA-control and OP-control samples in order to remove genes that were more likely to be differentially expressed because of potential differences caused by sourcing bone at surgery versus autopsy. Because there were also very few significant differences in gene expression between the male and female OA-control groups, these data were combined because it strengthened the statistical significance of the genes identified as differentially expressed. Using these selection processes, several hundred genes from each initial grouping was reduced to a list of 150 differentially expressed genes in OA bone with t scores above 4.
Gene function and pathway analyses were carried out by searching the National Centre for Biotechnology Information database [52] and by using various analysis programs including OntoExpress [53] and Gostat [54]. We were able to identify a group of 62 top-ranking OA differentially expressed genes from within the initial list of 150 genes, which have known or suspected roles (direct or indirect via angiogenesis) in influencing bone development or bone remodelling (Table 3). For many of the genes both osteogenic and angiogenic roles have been described. In addition, a subset of these genes, particularly those that encode secreted, cell surface and extracellular matrix molecules, also have potential chondrogenic functions, consistent with the proposal that an altered OA subchondral bone microenvironment could interfere with cartilage metabolism.
Although many of the genes identified in this analysis have pleiotropic effects in bone and other tissues, it was of interest that many of the top-ranking differentially expressed genes in OA bone have known or suspected roles in osteoblast and osteocyte differentiation and function. These genes included ADAMTS4, ADM, GADD45B, IBSP, MMP25, MT2A, STC1, MEPE, TWIST1, IGFBP3, S100A4, AKT3 and COL4A1. There was also a group of differentially expressed genes in OA bone that have known or potential roles in osteoclast function, such as the previously mentioned osteoblast-related genes ADAMTS4, GADD45B, STC1 and IGFB3, as well as ADAM8, CCR2, CSTA, RAC2, CRYAB and CYP1B. Functionally, within the list of genes given in Table 3, there are genes encoding secreted molecules (ADM, ANGPTL4, STC1, CORT, IGFBP3 and MIF), cell surface molecules (SELL, ICAM3, SELP, CRIM1, CLECSF6, CLECSF2, CCR2 and SLC14A1), intracellular signalling molecules (RAB20, YWHAG, RAC2, NHERF1, GNA11 and SNX9), protein kinases (AKT3 and PRKCD), calcium and metal ion binding proteins (S100A4, S100A6, MT1L, MT2A and MT1G), transcription factors (TWIST1, FMR2, KLF6, NR4A2 and DEC1), and both enzymatic (ADAMTS4, MMP25, ADAM8, TIMP4, GALNT4 and CTSG) and structural (TGFBI, IBSP, MEPE, MFAP3L and COL4A1) extracellular matrix molecules.
Because of the small absolute differences in gene expression between the bone tissue samples, real-time PCR was used to confirm a selection of the differentially expressed genes identified by the microarray analysis of OA, control and OP bone. The real-time PCR results (depicted as fold differential expression) are shown alongside the microarray results in Table 3. In total, the differential expression levels of 20 genes were examined using real-time PCR. Results for 16 genes reached statistical significance (P < 0.01) for differential expression between OA and control bone. The differential expression of four genes (TGFBI, S100A6, SLC14A1 and SNX9) could not be confirmed. The female control samples 1–8 (age range 56 to 85 years, mean [ ± SD] age 70.5 ± 10 years) and female OA samples 12–19 (age range 56 to 83 years; mean age 73 ± 10.8 years) were used to confirm the microarray data by real-time PCR (Table 1). The mean age of the OA group did not differ significantly from that in the control group. Interestingly, although the microarray expression ratios were quite small (ranging from 0.62-fold change to 1.47-fold change in expression), the fold difference in expression identified using the real-time PCR reactions was significantly greater in most cases (ranging from 0.08-fold change to 2.6-fold change in expression). This probably reflects differences in sensitivity between the two techniques [55, 56]. The difference is probably also accentuated by the competitive pair-wise comparison of samples used by the microarray platform in this study compared with the individual gene/GAPDH CT expression ratio values generated using real-time PCR. Encouragingly, there was a high confirmation rate with the real-time PCR and consistency between the microarray and PCR detection of expression ratio differences for each of the genes analyzed, suggesting that the majority of the genes identified by the microarray are bona fide differentially expressed genes in OA bone.
Altered expression of WNT and TGF-β/BMP signalling pathway component and target genes in OA bone
A significant number of the top-ranking differentially expressed genes in OA bone were identified as WNT signalling pathway targets (Table 3). WNT targets included upregulated genes such as MMP25 and S100A4, and downregulated genes such as IBSP, TWIST1 and TIMP4. The altered expression of these genes suggests that WNT signalling may be perturbed in the OA bone microenvironment. This was apparently borne out by closer examination of the extended list of differentially expressed genes in OA bone, which revealed further WNT signalling pathway components and modulators such as WNT5B, FZD3, SFRP5, APC, AXIN2, PTEN and NHERF1. These genes, and additional WNT target genes such as CD14, APOE, ID1, IL6, FST and RUNX2, are listed in Table 4. The differences in expression of this group of genes (t scores above 3) in general were not as pronounced as that seen for the target genes identified from within the top-ranking 150 genes.
In addition, a significant number of TGF-β/BMP signalling pathway target genes were identified as being differentially expressed in OA bone (Table 3). TGF-β/BMP signalling pathway targets included downregulated genes such as ADAMTS4, ADM, GADD45B, MEPE and COL4A1. The altered expression of these genes also suggests that TGF-β/BMP signalling may be perturbed in the OA bone microenvironment. Additional evidence for this was that genes for TGF-β/BMP signalling pathway components and modulators, such as TGFB1, BMP5, INHBA, SMAD3 and FST, were also identified in the extended list of differentially expressed genes in OA bone. These genes, and additional TGF-β/BMP target genes identified, such as COL1A2, GSN, DMP1 and ITGB2, are listed in Table 4. The differences in expression of this group of genes (t scores above 3) was not as pronounced as the target genes identified from within the top-ranking 150 genes.
Like the top-ranking list of 150 differentially expressed genes in OA bone, many of the WNT and TGF-β/BMP signalling pathway related genes identified in Table 4 also have known or suspected roles in either osteoblast (WNT5B, PTEN, CD14, SMAD3, RUNX2, ID1, HDAC4, TGFB1, BMP5, INHBA, DMP1 and FST) or osteoclast (CD14, PTEN, FOXP1, ANXA2, ITGB2, IL6 and GSN) differentiation and function.
The differential expression of a selection of these WNT and TGF-β/BMP signalling pathway component and target genes was confirmed by real-time PCR. In total, the differential expression of 11 genes was examined by real-time PCR (Table 4). The differential expression of two genes (LRP1 and IGFBP7) could not be confirmed. However, results for the other nine genes reached statistical significance (P < 0.01) for differential expression between OA and control bone. CTNNB1 was assayed directly by real-time PCR because it was not represented on the Compugen H19K library. Seven of the remaining nine genes (with FST and RUNX2 being the exceptions) were represented in the top-ranking 300 genes differentially regulated in OA bone. These genes were tested, like those listed in Table 3, using female control samples 1 to 8 and female OA samples 12 to 19 (Table 1). The range of fold difference in expression identified by the real-time PCR reactions was slightly smaller (ranging from 0.3-fold change to 3.47-fold change in expression) than for the group of genes tested from the top ranking 150 genes in Table 3.
Identification of differentially expressed OA genes between females and males
There is a higher incidence of primary hip OA in females than in males [1], and we were interested in identifying differences in gene expression between females and males that may contribute to this disparity. Therefore, we tested for differences between the OA-control female and male microarray datasets. Genes with the greatest difference in expression between females and males in the OA-control microarray comparisons are listed in Table 5. There were very few significant differences in gene expression between females and males. However, approximately 50 genes with t scores above 3, which included the top-ranking 20 genes with t scores above 4, were identified as being differentially expressed between females and males. Interestingly, a significant proportion of these genes have known or suspected roles in osteoclast-lineage cells and osteoclasts (GSN, PTK9, VCAM1, ITGB2, GRN, ANXA2, PDE4A and FOXP1). There are also genes with known roles in osteoblasts (LTF, DF, PRKCG and TGFB1). A number of the highest ranking differentially expressed genes between females and males in OA bone also involve WNT signalling pathway components, including WNT5B, along with the EAF2 and CTBP2 genes, which encode transcription factors that are involved in mediating WNT signalling.
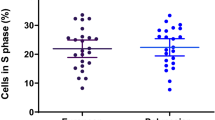
The differential expressions of WNT5B and ITGB2 (along with MMP25) between females and males in OA bone were confirmed by real-time PCR (Figure 2). MMP25 was not originally identified as being differentially expressed between females and males in OA bone by microarray analysis. WNT5B, ITGB2 and MMP25 were all found to be differentially expressed only in females, and not in males, between OA and control bone. The OA/control ratios of expression for the WNT5B gene were 2.52 in female samples (P < 0.01) and 0.92 in male samples (P = 0.7486); those for the ITGB2 gene were 2.95 (P < 0.01) and 1.35 (P = 0.1173), respectively; and those for the MMP25 gene were 2.60 (P < 0.01) and 1.01 (P = 0.4748), respectively. There was also a significant difference in the total expression levels of these three genes between females and males, being approximately 6-fold, 14-fold and 23-fold higher for WNT5B, MMP25 and ITGB2, respectively, in females than in males in OA bone. Thirteen other genes (ADAM8, ADM, ADAMTS4, ADFP, CD14, COL14A1, GADD45B, LRP1, S100A4, SMAD3, TGFBI, TIMP4 and TWIST1) were also tested for differential expression between females and males in OA bone, but none of these was found to be differently expressed (data not shown). Genes were tested using female control samples 1 to 8 and OA samples 12 to 19 as compared with male control samples 37 to 44 (age range 60 to 85 years; mean [ ± SD] age 70.4 ± 7.3 years) and OA samples 47 to 54 (62 to 85 years; 70.3 ± 8 years; Table 1). The mean ages of the female and male OA groups did not significantly differ from those of the control groups. Of the other 13 genes examined by PCR, only SMAD3 had significant differences in total expression levels between males and females, being approximately 2-fold higher in males than in females (Figure 2). However, SMAD3 was similarly differentially regulated between OA and control bone in both females and males (ratio of OA/control: 2.64 in females [P < 0.01] and 2.08 in males [P < 0.01]).
PCR analysis of WNT5B, ITGB2, MMP25 and SMAD3 expression between females and males in OA bone. For each gene, a graph depicts relative real-time PCR product/GAPDH cycle threshold (CT) ratios generated from osteoarthritis (OA) and control (CTL) female and male intertrochanteric bone samples analyzed. The mean of eight samples for each sample group analyzed is represented by black diamonds (mean values given alongside). Asterisks signify statistical significance (P < 0.01) for differential gene expression between OA and CTL bone. F, female; M, male.
Discussion
In this study we identified altered expression of WNT and TGF-β/BMP signalling pathway component and target genes in OA bone distal to the disease site (from the IT region of the proximal femur). This was accomplished by using microarray analysis to compare gene expression in bone from individuals with end-stage OA disease and individuals without obvious OA (control or OP). The genes identified include those with known or suspected roles in osteoblast, osteocyte and osteoclast differentiation and function, as well as angiogenesis, suggesting perturbation of these processes and a role for altered bone remodelling in OA pathogenesis.
The trabecular bone sampled in this study included all of the cellular elements of bone, including the bone marrow. This has provided a 'snapshot' of the gene expression in OA bone, with contributions from all of the different cells in the bone microenvironment. Although the specific cell type(s) contributing to the altered gene expression cannot readily be identified, osteoblasts and osteocytes, which represent the most abundant cells in the trabecular bone [57], would be expected to contribute significantly to the altered gene expression measured. In addition, because we have analyzed bone from end-stage OA, it is difficult to determine unequivocally that the altered gene expression detected in the OA bone is causal or secondary to the disease. However, by sampling the IT region we have avoided secondary pathogenic changes that the subchondral bone undergoes at the joint as the disease progresses (such as sclerosis, osteophytes and cysts), which could confound identification of altered gene expression potentially responsible for the underlying subchondral bone remodelling. Therefore, we suggest that the altered gene expression identified in the IT region from OA bone may be informative about underlying systemic OA disease mechanisms that also operate at the joint in the subchondral bone.
The first main finding of this study is that many of the top-ranking differentially expressed genes in OA bone (Table 3) have known or suspected roles in osteoblast and osteocyte differentiation and function. (Also see Table 6 for descriptions of the functions of selected genes: MEPE, IBSP, MT2A, ADM, STC1, IGFBP3, GADD45B, ADAMTS4, S100A4 and MMP25.) Significantly, the changes in expression of these genes as a group suggest altered osteoblast and osteocyte activity in OA bone, which is consistent with increased bone volume fraction and under-mineralization previously reported in OA bone [3, 4, 11, 22–25]. For instance, MEPE (matrix extracellular phosphoglycoprotein), which is highly expressed in osteoblasts and osteocytes, appears to be an important regulator of bone formation and mineralization. Targeted disruption of MEPE has been found to result in increased bone formation and bone mass [58]. MEPE was found to be downregulated in OA bone, which is consistent with the increased trabecular bone volume in OA. MMP25 (upregulated in OA bone) encodes a metalloproteinase that plays a role in MMP2 activation [59], and MMP2 is a major effector in osteocytes, with MMP2-/- mice exhibiting disrupted osteocytic networks and altered bone remodelling and mineralization [60]. The MMP2-/- mice have a complex bone phenotype that includes reduced bone volume in the long bones. Upregulation of MMP25 in OA bone is consistent with increased activity of MMP2 and increased bone volume.
Interestingly, and in contrast to the large number of differentially expressed genes identified in OA bone with osteoblast-related and osteocyte-related roles, a substantial group of top-ranking differentially expressed genes identified in OP bone (data not shown) have known or suspected roles in osteoclast-lineage cells. The change in expression of these genes as a group is consistent with increased osteoclast numbers, activity and bone resorption, leading to the reduction of bone volume seen in OP. There was also a group of differentially expressed genes identified in OA bone that have known or potential roles in osteoclast function (Tables 3 to 5). However, the overall change in expression of these genes, as a group, was not as consistent as for those genes identified with osteoblast-related functions. For instance, the change in expression of a subset of these genes (ADAMTS4, GADD45B, IGFBP3 and CSTA) is consistent with decreased osteoclast activity and increased bone volume in OA, whereas the change in expression of another subset of these osteoclast-related genes (ADAM8, STC1, CCR2, RAC2, CRYAB, CYP1B, CD14, PTEN, ANXA2 and GSN) suggests upregulated osteoclast activity (Table 6). It is now becoming clear that, in addition to osteoblasts being intimately involved in influencing osteoclast-lineage cell differentiation and function [61], the converse may also be true [62, 63]. As a result, perturbed osteoblast or osteoclast gene expression could lead to complex changes in communication between these bone cell types and their remodelling behaviour in OA bone. Therefore, differential expression of a subset of the osteoclast-related genes, suggesting upregulated osteoclast activity, is consistent with the increased levels of bone remodelling seen in OA bone and perhaps a net gain of under-mineralized bone rather than the net loss of bone volume seen in OP.
Important inter-relationships between bone remodelling and angiogenesis are also now emerging, and so perturbations to angiogenic molecular pathways could contribute to the changes seen in OA bone. Consistent with a role for increased angiogenesis in OA bone, leading to increased bone volume and potentially turnover, is the upregulation of a group of top-ranking differentially expressed genes with recognized pro-angiogenic functions (MMP25, S100A4, FOSB, TFF3, CTSG and LTB) and downregulation of a group of genes that negatively influence angiogenesis (HIG2, ADAMTS4, ANGPTL4, STC1, KLF6, IGFBP3, TIMP4 and GDF15).
In addition, a subset of the genes with roles in osteoblasts, particularly those that encode secreted, cell surface and extracellular matrix molecules, including ADM, IBSP, MMP25, STC1, IGFBP3, WNT5B, FST, TGFB1, BMP5 and INHBA, also have potential chondrogenic functions. Altered expression of many of these genes is consistent with the proposal that similar altered expression of these genes in osteoblasts in the subchondral bone microenvironment could interfere with chondrocyte or cartilage metabolism. For instance, ADM, which is downregulated in OA bone has a pro-chondrogenic role [64]. Reduced levels of ADM could negatively affect chondrocyte/cartilage metabolism.
The second significant and connected observation from this study was that many of the top-ranking differentially expressed genes identified in OA bone (with osteoblast, osteocyte and osteoclast related roles) were WNT or TGF-β/BMP signalling pathway target genes. This observation, on closer examination of the ranked list of differentially expressed in OA bone, led to the identification of additional sets of differentially expressed genes that were WNT or TGF-β/BMP signalling pathway component or modulator genes. These data together suggest that the WNT and TGF-β/BMP signalling pathways are altered in OA bone and may play a role(s) in OA pathogenesis. Both the WNT and TGF-β/BMP signalling pathways have been implicated in influencing bone mass and bone remodelling [32–34] and have been demonstrated to do this by controlling both osteoblast and osteoclast differentiation and function [65–67].
WNT signalling, in terms of bone mass and bone remodelling, is a very complex process that depends on the interplay of a large number of WNT ligands, the receptors they complex with, prevailing antagonists and particular combinations of β-catenin/transcription factor complexes that ultimately control the expression of the target genes. Interestingly, the only gene encoding a WNT ligand, WNT5B, that was identified as being differentially expressed (upregulated in OA bone) in the present study was recently demonstrated to increase in expression during in vitro osteoblast differentiation [68]. The protein encoded by WNT5B is known to have both stimulatory and inhibitory effects on bone and cartilage cells, and signals through both the canonical and noncanonical WNT signalling pathways, depending on the receptor it complexes with at the cell surface [68–70]. Along with WNT5B, there were also several other important WNT pathway related genes that were altered in their expression in OA bone. Genes for the WNT5B co-receptor FZD3 and extracellular WNT antagonist SFRP5 were under-expressed, relative to controls, suggesting increased WNT signalling. Downregulation of the intracellular signalling cascade genes PTEN, APC and AXIN2, and upregulation of CTNNB1, AKT3 and NHERF1 are also consistent with increased WNT signalling. CTNNB1 encodes β-catenin, which is the central downstream mediator of canonical WNT signalling, which forms a complex with lymphoid enhancer factor/T cell factor (LEF/TCF) transcription factors to modulate target gene expression [71], whereas PTEN, APC, AXIN2, AKT3 and NHERF1 gene products modulate β-catenin activity (Table 6).
Like WNT signalling, TGF-β/BMP signalling is similarly complex, with a large family of ligands, cognate receptors and intracellular signalling molecules involved in the pathway, exerting both stimulatory and inhibitory effects on bone remodelling. Several TGF-β/BMP signalling pathway component and modulator genes that influence osteoblast function, bone remodelling and bone mineralization were identified as altered in OA bone. These included TGFB1, INHBA, ACVR1, BMP5, FST and SMAD3 (Table 6).
There is significant crosstalk between the WNT and TGF-β/BMP signalling pathways. β-Catenin, SMAD3 and runt-related transcription factor (RUNX)2 potentially play important roles in mediating the crosstalk between the WNT and TGF-β/BMP signalling pathways via direct interactions and in complexes with the TCF/LEF transcription factor family members in the nucleus [72–75]. We observed increased RUNX2 expression in OA bone in this study, which is consistent with increased osteoblast differentiation and activity in OA bone. RUNX2, which is a WNT inducible gene, encodes a transcription factor that plays roles in mediating both WNT and TGF-β/BMP signalling, and is essential for osteoblast differentiation and skeletal development [66, 75–77]. Intriguingly, decreased expression of RUNX2 has been shown to reduce cartilage destruction and subchondral bone changes in a mouse joint instability OA model [78], suggesting a role for increased RUNX2 expression in OA pathogenesis. An important role for RUNX2 in OA pathogenesis is supported by our microarray data. The products of several of the top-ranking differentially expressed genes identified, such as TWIST1 (twist homologue 1) [79], FOXF1 (forkhead box F1), ID1 (inhibitor of DNA binding 1), HDAC4 (histone deacetylase 4) and SMAD3, modify RUNX2 expression or interact with and modify RUNX2 function. SMAD3 is an important mediator of TGF-β regulation of bone mechanical properties and composition [80]. TGF-β represses RUNX2, and one of the ways it does this is through recruitment of the histone deacetylase HDAC4 by SMAD3 [81]. However, SMAD3 over-expression (SMAD3 was upregulated in OA bone in the present study) has also been reported to induce RUNX2 expression and osteoblast differentiation [82]. Significantly, several of the highest ranking differentially expressed genes identified in this study in OA bone are targets of RUNX2 and SMAD3, such as GADD45B [83], ADAMTS4 [84] and MEPE [82].
Finally, the molecular mechanisms that are responsible for the greater incidence of OA in females are not known. Genes may operate differently in the two sexes, at different body sites and on different disease features within body sites [27]. Interestingly, of the relatively small number of differences between females and males in OA bone identified in this study, there were significant numbers of genes that were involved in both osteoclast (for example, ANXA2, GSN, ITGB2, FOXP1 and PDE4A) and osteoblast (LTF, DF and TGFB1) function and hence bone remodelling (Tables 5 and 6). Collectively, the differential expression of these genes is consistent with increased bone turnover in OA females compared with males, suggesting an OA disease mechanism and perhaps partly accounting for a greater incidence of OA in females than in males.
A number of the highest ranking differentially expressed genes between OA females and males include WNT signalling pathway components such as WNT5B and the transcription factor genes EAF2 and CTBP2. In addition MMP25 and ITGB2 are WNT target genes, suggesting a difference between females and males in WNT signalling that may have an impact on the OA bone microenvironment. There is also evidence of crosstalk between WNT and oestrogen signalling pathways via functional interaction between β-catenin and oestrogen receptor-α [85]. A number of the genes identified in our study, including WNT5B, ITGB2, GSN, VCAM1, LTF and DF, are affected by oestrogen, potentially providing a mechanism by which they are differentially expressed in females compared with males. Examples of sexual dimorphism in mammalian gene expression related to different responses to disease by females and males are beginning to be identified [86]. The differences in expression levels of WNT5B, ITGB2 and MMP25 detected between females and males in OA bone is of interest and marks these genes as good candidates for further investigation into the sex disparity in OA.
In this study we observed small gene expression ratios in both microarray and real-time PCR analyses. These are probably contributed by the complex mix of cells being assayed, along with the subtle changes to bone that are observed in OA distal to the affected joint, and the often slow, age-dependent onset of the disease. Furthermore, OA is a multifactorial, multigene disorder (and perhaps even a heterogenous group of disorders that lead to similar bone changes, cartilage degeneration and ultimately loss of joint function). Therefore, it is to be expected that many genes and small changes in the expression of these genes would be involved in OA pathogenesis. Microarray analysis is able to reliably detect small (<2-fold) changes that prove to be biologically relevant [87], and in our study we were able to confirm the large majority of the differentially expressed genes by real-time PCR analysis. Furthermore, the power of the microarray analysis approach lies in its ability to detect genome-wide, coordinated, or similarly regulated differential gene expression, pointing to perturbed signalling pathways and importantly downstream molecular processes. Our study has identified such relationships between commonly regulated target genes (via WNT and TGF-β/BMP signalling pathways) that play roles, in particular, in osteoblasts, osteocytes and osteoclasts, potentially influencing bone formation, mineralization and remodelling.
Conclusion
In conclusion, we identified altered gene expression in bone from individuals with primary hip OA at a site distal to the diseased joint. This information is of interest because it identifies genes that potentially play roles in systemic physiological bone turnover or in skeletal disease processes, and implicate altered WNT and TGF-β/BMP signalling in OA pathogenesis. Further work sampling from individuals with early OA will be required to determine whether the genes identified as differentially expressed in OA bone are causal or secondary to the altered bone seen in OA.
Abbreviations
- AMF:
-
= Adelaide Microarray facility
- BMP:
-
= bone morphogenic protein
- CT:
-
= cycle threshold
- IL:
-
= interleukin
- IT:
-
= intertrochanteric
- LEF:
-
= lymphoid enhancer factor
- LIMMA:
-
= linear models for microarray analysis
- MMP:
-
= matrix metalloproteinase
- OA:
-
= osteoarthritis
- OP:
-
= osteoporosis
- PCR:
-
= polymerase chain reaction
- RUNX:
-
= runt-related transcription factor
- SD:
-
= standard deviation
- TCF:
-
= T-cell factor
- TGF:
-
= transforming growth factor
- WNT:
-
= wingless MMTV integration.
References
Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM, Kington RS, Lane NE, Nevitt MC, Zhang Y, et al: Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000, 133: 635-646.
Hough AJ: Pathology of osteoarthritis. Arthritis and Allied Conditions: a Text Book of Rheumatology. Edited by: Koopman WJ. 2001, Philadelphia, PA: Lippincott Williams and Wilkins, 2: 2167-2194. 14
Li B, Aspden RM: Composition and mechanical properties of cancellous bone from the femoral head of patients with osteoporosis or osteoarthritis. J Bone Miner Res. 1997, 12: 641-651. 10.1359/jbmr.1997.12.4.641.
Mansell JP, Tarlton JF, Bailey AF: Biochemical evidence for altered subchondral bone collagen metabolism in osteoarthritis of the hip. Br J Rheumatol. 1997, 36: 16-19. 10.1093/rheumatology/36.1.16.
Carlson CS, Loeser RF, Jayo MJ, Weaver DS, Adams MR, Jerome CP: Osteoarthritis in cynomolgus macaques: a primate model of naturally occurring disease. J Orthop Res. 1994, 12: 331-339. 10.1002/jor.1100120305.
Watson PJ, Hall LD, Malcolm A, Tyler JA: Degenerative joint disease in the guinea pig. Use of magnetic resonance imaging to monitor progression of bone pathology. Arthritis Rheum. 1996, 39: 1327-1337. 10.1002/art.1780390810.
Hayami T, Pickarski M, Zhuo Y, Wesolowski GA, Rodan GA, Duong le T: Characterization of articular cartilage and subchondral bone changes in the rat anterior cruciate ligament transection and meniscectomized models of osteoarthritis. Bone. 2006, 38: 234-243. 10.1016/j.bone.2005.08.007.
Hayami T, Pickarski M, Wesolowski GA, McLane J, Bone A, Destefano J, Rodan GA, Duong le T: The role of subchondral bone remodeling in osteoarthritis: reduction of cartilage degeneration and prevention of osteophyte formation by alendronate in the rat anterior cruciate ligament transection model. Arthritis Rheum. 2004, 50: 1193-1206. 10.1002/art.20124.
Behets C, Williams JM, Chappard D, Devogelaer JP, Manicourt DH: Effects of calcitonin on subchondral trabecular bone changes and on osteoarthritic cartilage lesions after acute anterior cruciate ligament deficiency. J Bone Miner Res. 2004, 19: 1821-1826. 10.1359/JBMR.040609.
Spector TD, Conaghan PG, Buckland-Wright JC, Garnero P, Cline GA, Beary JF, Valent DJ, Meyer JM: Effect of risedronate on joint structure and symptoms of knee osteoarthritis: results of the BRISK randomized, controlled trial [ISRCTN01928173]. Arthritis Res Ther. 2005, 7: R625-R633. 10.1186/ar1716.
Dequeker J, Luyten FP: Bone mass and osteoarthritis. Clin Exp Rheumatol. 2000, 18: S21-S26.
Radin EL, Rose RM: Role of subchondral bone in the initiation and progression of cartilage damage. Clin Orthop Relat Res. 1986, 213: 34-40.
Bailey AJ, Buckland-Wright C, Metz D: The role of bone in osteoarthritis. Age Ageing. 2001, 30: 374-378. 10.1093/ageing/30.5.374.
Lajeunesse D: The role of bone in the treatment of osteoarthritis. Osteoarthritis Cartilage. 2004, 12: S34-S38. 10.1016/j.joca.2003.09.013.
Westacott CI, Webb GR, Warnock MG, Sims JV, Elson CJ: Alteration of cartilage metabolism by cells from osteoarthritic bone. Arthritis Rheum. 1997, 40: 1282-1291.
Sanchez C, Deberg MA, Piccardi N, Msika P, Reginster JY, Henrotin YE: Osteoblasts from the sclerotic subchondral bone downregulate aggrecan but upregulate metalloproteinases expression by chondrocytes. This effect is mimicked by interleukin-6, -1beta and oncostatin M pre-treated non-sclerotic osteoblasts. Osteoarthritis Cartilage. 2005, 13: 979-987. 10.1016/j.joca.2005.03.008.
Lyons TJ, McClure SF, Stoddart RW, McClure J: The normal human chondro-osseous junctional region: evidence for contact of uncalcified cartilage with subchondral bone and marrow spaces. BMC Musculoskelet Disord. 2006, 7: 52-10.1186/1471-2474-7-52.
Imhof H, Sulzbacher I, Grampp S, Czerny C, Youssefzadeh S, Kainberger F: Subchondral bone and cartilage disease: a rediscovered functional unit. Invest Radiol. 2000, 35: 581-588. 10.1097/00004424-200010000-00004.
Gerber HP, Vu TH, Ryan AM, Kowalski J, Werb Z, Ferrara N: VEGF couples hypertrophic cartilage remodeling, ossification and angiogenesis during endochondral bone formation. Nat Med. 1999, 5: 623-628. 10.1038/9467.
Fang TD, Salim A, Xia W, Nacamuli RP, Guccione S, Song HM, Carano RA, Filvaroff EH, Bednarski MD, Giaccia AJ, et al: Angiogenesis is required for successful bone induction during distraction osteogenesis. J Bone Miner Res. 2005, 20: 1114-1124. 10.1359/JBMR.050301.
Meury T, Verrier S, Alini M: Human endothelial cells inhibit BMSC differentiation into mature osteoblasts in vitro by interfering with osterix expression. J Cell Biochem. 2006, 98: 992-1006. 10.1002/jcb.20818.
Gevers G, Dequeker J, Martens M, Van Audekercke R, Nyssen-Behets C, Dhem A: Biomechanical characteristics of iliac crest bone in elderly women according to osteoarthritis grade at the hand joints. J Rheumatol. 1989, 16: 660-663.
Fazzalari NL, Vernon-Roberts B, Manthey BA, Parkinson IH: Relationship between changes in articular cartilage and bone in the femoral head in osteoarthritis of the hip. J Orthopaed Rheumatol. 1990, 3: 155-169.
Fazzalari NL, Parkinson IH: Femoral trabecular bone of osteoarthritic and normal subjects in an age and sex matched group. Osteoarthritis Cartilage. 1998, 6: 377-382. 10.1053/joca.1998.0141.
Nevitt MC, Lane NE, Scott JC, Hochberg MC, Pressman AR, Genant HK, Cummings SR: Radiographic osteoarthritis of the hip and bone mineral density. The Study of Osteoporotic Fractures Research Group. Arthritis Rheum. 1995, 38: 907-916. 10.1002/art.1780380706.
Dequeker J, Boonen S, Aerssens J, Westhovens R: Inverse relationship osteoarthritis-osteoporosis: what is the evidence? What are the consequences?. Br J Rheumatol. 1996, 35: 813-818. 10.1093/rheumatology/35.9.813.
Spector TD, MacGregor AJ: Risk factors for osteoarthritis: genetics. Osteoarthritis Cartilage. 2004, 12: S39-S44. 10.1016/j.joca.2003.09.005.
Brandi ML, Gennari L, Cerinic MM, Becherini L, Falchetti A, Masi L, Gennari C, Reginster JY: Genetic markers of osteoarticular disorders: facts and hopes. Arthritis Res. 2001, 3: 270-280. 10.1186/ar316.
Peach CA, Carr AJ, Loughlin J: Recent advances in the genetic investigation of osteoarthritis. Trends Mol Med. 2005, 11: 186-191. 10.1016/j.molmed.2005.02.005.
Loughlin J, Dowling B, Chapman K, Marcelline L, Mustafa Z, Southam L, Ferreira A, Ciesielski C, Carson DA, Corr M: Functional variants within the secreted frizzled-related protein 3 gene are associated with hip osteoarthritis in females. Proc Natl Acad Sci USA. 2004, 101: 9757-9762. 10.1073/pnas.0403456101.
Chung YS, Baylink DJ, Srivastava AK, Amaar Y, Tapia B, Kasukawa Y, Mohan S: Effects of secreted frizzled-related protein 3 on osteoblasts in vitro. J Bone Miner Res. 2004, 19: 1395-1402. 10.1359/JBMR.040412.
Krishnan V, Bryant HU, Macdougald OA: Regulation of bone mass by Wnt signaling. J Clin Invest. 2006, 116: 1202-1209. 10.1172/JCI28551.
Canalis E, Economides AN, Gazzerro E: Bone morphogenetic proteins, their antagonists, and the skeleton. Endocr Rev. 2003, 24: 218-235. 10.1210/er.2002-0023.
Janssens K, ten Dijke P, Janssens S, Van Hul W: Transforming growth factor-beta1 to the bone. Endocr Rev. 2005, 26: 743-774. 10.1210/er.2004-0001.
Kuliwaba JS, Findlay DM, Atkins GJ, Forwood MR, Fazzalari NL: Enhanced expression of osteocalcin mRNA in human osteoarthritic trabecular bone of the proximal femur is associated with decreased expression of interleukin-6 and interleukin-11 mRNA. J Bone Miner Res. 2000, 15: 332-341. 10.1359/jbmr.2000.15.2.332.
Fazzalari NL, Kuliwaba JS, Atkins GJ, Forwood MR, Findlay DM: The ratio of messenger RNA levels of receptor activator of nuclear factor kappaB ligand to osteoprotegerin correlates with bone remodeling indices in normal human cancellous bone but not in osteoarthritis. J Bone Miner Res. 2001, 16: 1015-1027. 10.1359/jbmr.2001.16.6.1015.
Truong LH, Kuliwaba JS, Tsangari H, Fazzalari NL: Differential gene expression of bone anabolic factors and trabecular bone architectural changes in the proximal femoral shaft of primary hip osteoarthritis patients. Arthritis Res Ther. 2006, 8: R188-10.1186/ar2101.
Dequeker J, Mohan S, Finkelman RD, Aerssens J, Baylink DJ: Generalized osteoarthritis associated with increased insulin-like growth factor types I and II and transforming growth factor beta in cortical bone from the iliac crest. Possible mechanism of increased bone density and protection against osteoporosis. Arthritis Rheum. 1993, 36: 1702-1708. 10.1002/art.1780361209.
Massicotte F, Lajeunesse D, Benderdour M, Pelletier JP, Hilal G, Duval N, Martel-Pelletier J: Can altered production of interleukin-1beta, interleukin-6, transforming growth factor-beta and prostaglandin E2 by isolated human subchondral osteoblasts identify two subgroups of osteoarthritic patients. Osteoarthritis Cartilage. 2002, 10: 491-500. 10.1053/joca.2002.0528.
Collins D: The Pathology of Articular and Spinal Diseases. 1949, London, UK: Edward Arnold and Co
Kuliwaba JS, Fazzalari NL, Findlay DM: Stability of RNA isolated from human trabecular bone at post-mortem and surgery. Biochim Biophys Acta. 2005, 1740: 1-11.
Adelaide Microarray Facility. [http://www.microarray.adelaide.edu.au]
The Comprehensive R Archive Network. [http://cran.r-project.org]
Spot: Software for Analysis of Microarray Images. [http://experimental.act.cmis.csiro.au/Spot/index.php]
Yang YH, Buckley MJ, Speed TP: Analysis of cDNA microarray images. Brief Bioinform. 2001, 2: 341-349. 10.1093/bib/2.4.341.
Ritchie ME: Quantitative quality control and background correction for two-colour microarray data. PhD thesis. 2004, University of Melbourne, Department of Medical Biology
Gentleman RC, Carey VJ, Bates DM, Bolstad B, Dettling M, Dudoit S, Ellis B, Gautier L, Ge Y, Gentry J, et al: Bioconductor: open software development for computational biology and bioinformatics. Genome Biol. 2004, 5: R80-10.1186/gb-2004-5-10-r80.
Yang YH, Dudoit S, Luu P, Lin DM, Peng V, Ngai J, Speed TP: Normalization for cDNA microarray data: a robust composite method addressing single and multiple slide systematic variation. Nucleic Acids Res. 2002, 30: e15-10.1093/nar/30.4.e15.
Smyth GK: Linear models and empirical bayes methods for assessing differential expression in microarray experiments. Stat Appl Genet Mol Biol. 2004, 3: Article 3
Gene Expression Omnibus (GEO). [http://www.ncbi.nlm.nih.gov/geo/]
KJ Livak, TD Schmittgen: Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta CT) Method. Methods. 2001, 25: 402-408. 10.1006/meth.2001.1262.
National Centre for Biotechnology Information. [http://www.ncbi.nlm.nih.gov]
Draghici S, Khatri P, Bhavsar B, Shah A, Krawetz SA, Tainsky MA: Onto-Tools, the toolkit of the modern biologist: Onto-Express, Onto-Compare, Onto-Design and Onto-Translate. Nucleic Acids Res. 2003, 31: 3775-3781. 10.1093/nar/gkg624.
Beissbarth T, Speed TP: GOstat: find statistically overrepresented Gene Ontologies within a group of genes. Bioinformatics. 2004, 20: 1464-1465. 10.1093/bioinformatics/bth088.
Dallas PB, Gottardo NG, Firth MJ, Beesley AH, Hoffmann K, Terry PA, Freitas JR, Boag JM, Cummings AJ, Kees UR: Gene expression levels assessed by oligonucleotide microarray analysis and quantitative real-time RT-PCR: how well do they correlate?. BMC Genomics. 2005, 6: 59-10.1186/1471-2164-6-59.
Wang Y, Barbacioru C, Hyland F, Xiao W, Hunkapiller KL, Blake J, Chan F, Gonzalez C, Zhang L, Samaha RR: Large scale real-time PCR validation on gene expression measurements from two commercial long-oligonucleotide microarrays. BMC Genomics. 2006, 7: 59-10.1186/1471-2164-7-59.
Franz-Odendaal TA, Hall BK, Witten PE: Buried alive: how osteoblasts become osteocytes. Dev Dyn. 2006, 235: 176-190. 10.1002/dvdy.20603.
Gowen LC, Petersen DN, Mansolf AL, Qi H, Stock JL, Tkalcevic GT, Simmons HA, Crawford DT, Chidsey-Frink KL, Ke HZ, et al: Targeted disruption of the osteoblast/osteocyte factor 45 gene (OF45) results in increased bone formation and bone mass. J Biol Chem. 2003, 278: 1998-2007. 10.1074/jbc.M203250200.
Nie J, Pei D: Direct activation of pro-matrix metalloproteinase-2 by leukolysin/membrane-type 6 matrix metalloproteinase/matrix metalloproteinase 25 at the asn(109)-Tyr bond. Cancer Res. 2003, 63: 6758-6762.
Inoue K, Mikuni-Takagaki Y, Oikawa K, Itoh T, Inada M, Noguchi T, Park JS, Onodera T, Krane SM, Noda M, et al: A crucial role for matrix metalloproteinase 2 in osteocytic canalicular formation and bone metabolism. J Biol Chem. 2006, 281: 33814-33824. 10.1074/jbc.M607290200.
Atkins GJ, Kostakis P, Welldon KJ, Vincent C, Findlay DM, Zannettino AC: Human trabecular bone-derived osteoblasts support human osteoclast formation in vitro in a defined, serum-free medium. J Cell Physiol. 2005, 203: 573-582. 10.1002/jcp.20255.
Kim HJ, Zhao H, Kitaura H, Bhattacharyya S, Brewer JA, Muglia LJ, Ross FP, Teitelbaum SL: Glucocorticoids suppress bone formation via the osteoclast. J Clin Invest. 2006, 116: 2152-2160. 10.1172/JCI28084.
Karsdal MA, Martin TJ, Bollerslev J, Christiansen C, Henriksen K: Are nonresorbing osteoclasts sources of bone anabolic activity?. J Bone Miner Res. 2007, 22: 487-494. 10.1359/jbmr.070109.
Cornish J, Naot D: Amylin and adrenomedullin: novel regulators of bone growth. Curr Pharm Des. 2002, 8: 2009-2021. 10.2174/1381612023393341.
Glass DA, Bialek P, Ahn JD, Starbuck M, Patel MS, Clevers H, Taketo MM, Long F, McMahon AP, Lang RA, et al: Canonical Wnt signaling in differentiated osteoblasts controls osteoclast differentiation. Dev Cell. 2005, 8: 751-764. 10.1016/j.devcel.2005.02.017.
Alliston T, Choy L, Ducy P, Karsenty G, Derynck R: TGF-beta-induced repression of CBFA1 by Smad3 decreases cbfa1 and osteocalcin expression and inhibits osteoblast differentiation. Embo J. 2001, 20: 2254-2272. 10.1093/emboj/20.9.2254.
Karst M, Gorny G, Galvin RJ, Oursler MJ: Roles of stromal cell RANKL, OPG, and M-CSF expression in biphasic TGF-beta regulation of osteoclast differentiation. J Cell Physiol. 2004, 200: 99-106. 10.1002/jcp.20036.
Hurson CJ, Butler JS, Keating DT, Murray DW, Sadlier DM, O'Byrne JM, Doran PP: Gene expression analysis in human osteoblasts exposed to dexamethasone identifies altered developmental pathways as putative drivers of osteoporosis. BMC Musculoskelet Disord. 2007, 8: 12-10.1186/1471-2474-8-12.
Church V, Nohno T, Linker C, Marcelle C, Francis-West P: Wnt regulation of chondrocyte differentiation. J Cell Sci. 2002, 115: 4809-4818. 10.1242/jcs.00152.
Shea CM, Edgar CM, Einhorn TA, Gerstenfeld LC: BMP treatment of C3H10T1/2 mesenchymal stem cells induces both chondrogenesis and osteogenesis. J Cell Biochem. 2003, 90: 1112-1127. 10.1002/jcb.10734.
Logan CY, Nusse R: The Wnt signaling pathway in development and disease. Annu Rev Cell Dev Biol. 2004, 20: 781-810. 10.1146/annurev.cellbio.20.010403.113126.
Jian H, Shen X, Liu I, Semenov M, He X, Wang XF: Smad3-dependent nuclear translocation of beta-catenin is required for TGF-beta1-induced proliferation of bone marrow-derived adult human mesenchymal stem cells. Genes Dev. 2006, 20: 666-674. 10.1101/gad.1388806.
Reinhold MI, Naski MC: Direct interactions of Runx2 and canonical Wnt signaling induce FGF18. J Biol Chem. 2007, 282: 3653-3663. 10.1074/jbc.M608995200.
Labbe E, Letamendia A, Attisano L: Association of Smads with lymphoid enhancer binding factor 1/T cell-specific factor mediates cooperative signaling by the transforming growth factor-beta and wnt pathways. Proc Natl Acad Sci USA. 2000, 97: 8358-8363. 10.1073/pnas.150152697.
Kahler RA, Westendorf JJ: Lymphoid enhancer factor-1 and beta-catenin inhibit Runx2-dependent transcriptional activation of the osteocalcin promoter. J Biol Chem. 2003, 278: 11937-11944. 10.1074/jbc.M211443200.
Komori T: Regulation of osteoblast differentiation by transcription factors. J Cell Biochem. 2006, 99: 1233-1239. 10.1002/jcb.20958.
Gaur T, Lengner CJ, Hovhannisyan H, Bhat RA, Bodine PV, Komm BS, Javed A, van Wijnen AJ, Stein JL, Stein GS, et al: Canonical WNT signaling promotes osteogenesis by directly stimulating Runx2 gene expression. J Biol Chem. 2005, 280: 33132-33140. 10.1074/jbc.M500608200.
Kamekura S, Kawasaki Y, Hoshi K, Shimoaka T, Chikuda H, Maruyama Z, Komori T, Sato S, Takeda S, Karsenty G, et al: Contribution of runt-related transcription factor 2 to the pathogenesis of osteoarthritis in mice after induction of knee joint instability. Arthritis Rheum. 2006, 54: 2462-2470. 10.1002/art.22041.
Bialek P, Kern B, Yang X, Schrock M, Sosic D, Hong N, Wu H, Yu K, Ornitz DM, Olson EN, et al: A twist code determines the onset of osteoblast differentiation. Dev Cell. 2004, 6: 423-435. 10.1016/S1534-5807(04)00058-9.
Balooch G, Balooch M, Nalla RK, Schilling S, Filvaroff EH, Marshall GW, Marshall SJ, Ritchie RO, Derynck R, Alliston T: TGF-beta regulates the mechanical properties and composition of bone matrix. Proc Natl Acad Sci USA. 2005, 102: 18813-18818. 10.1073/pnas.0507417102.
Kang JS, Alliston T, Delston R, Derynck R: Repression of Runx2 function by TGF-beta through recruitment of class II histone deacetylases by Smad3. Embo J. 2005, 24: 2543-2555. 10.1038/sj.emboj.7600729.
Kaji H, Naito J, Sowa H, Sugimoto T, Chihara K: Smad3 differently affects osteoblast differentiation depending upon its differentiation stage. Horm Metab Res. 2006, 38: 740-745. 10.1055/s-2006-955085.
Major MB, Jones DA: Identification of a gadd45beta 3' enhancer that mediates SMAD3- and SMAD4-dependent transcriptional induction by transforming growth factor beta. J Biol Chem. 2004, 279: 5278-5287. 10.1074/jbc.M311517200.
Thirunavukkarasu K, Pei Y, Moore TL, Wang H, Yu XP, Geiser AG, Chandrasekhar S: Regulation of the human ADAMTS-4 promoter by transcription factors and cytokines. Biochem Biophys Res Commun. 2006, 345: 197-204. 10.1016/j.bbrc.2006.04.023.
Kouzmenko AP, Takeyama K, Ito S, Furutani T, Sawatsubashi S, Maki A, Suzuki E, Kawasaki Y, Akiyama T, Tabata T, et al: Wnt/beta-catenin and estrogen signaling converge in vivo. J Biol Chem. 2004, 279: 40255-40258. 10.1074/jbc.C400331200.
Rinn JL, Snyder M: Sexual dimorphism in mammalian gene expression. Trends Genet. 2005, 21: 298-305. 10.1016/j.tig.2005.03.005.
Yao B, Rakhade RN, Li Q, Ahmed S, Krauss R, Draghici S, Loeb JA: Accuracy of cDNA microarray methods to detect small gene expression changes induced by neuregulin on breast epithelial cells. BMC Bioinformatics. 2004, 5: 99-10.1186/1471-2105-5-99.
Duarte WR, Shibata T, Takenaga K, Takahashi E, Kubota K, Ohya K, Ishikawa I, Yamauchi M, Kasugai S: S100A4: a novel negative regulator of mineralization and osteoblast differentiation. J Bone Miner Res. 2003, 18: 493-501. 10.1359/jbmr.2003.18.3.493.
Mathisen B, Lindstad RI, Hansen J, El-Gewely SA, Maelandsmo GM, Hovig E, Fodstad O, Loennechen T, Winberg JO: S100A4 regulates membrane induced activation of matrix metalloproteinase-2 in osteosarcoma cells. Clin Exp Metastasis. 2003, 20: 701-711. 10.1023/B:CLIN.0000006819.21361.03.
Ogata Y, Niisato N, Furuyama S, Cheifetz S, Kim RH, Sugiya H, Sodek J: Transforming growth factor-beta 1 regulation of bone sialoprotein gene transcription: identification of a TGF-beta activation element in the rat BSP gene promoter. J Cell Biochem. 1997, 65: 501-512. 10.1002/(SICI)1097-4644(19970615)65:4<501::AID-JCB6>3.0.CO;2-S.
Dohi Y, Shimaoka H, Ikeuchi M, Ohgushi H, Yonemasu K, Minami T: Role of metallothionein isoforms in bone formation processes in rat marrow mesenchymal stem cells in culture. Biol Trace Elem Res. 2005, 104: 57-70. 10.1385/BTER:104:1:057.
Liu AL, Zhang ZM, Zhu BF, Liao ZH, Liu Z: Metallothionein protects bone marrow stromal cells against hydrogen peroxide-induced inhibition of osteoblastic differentiation. Cell Biol Int. 2004, 28: 905-911. 10.1016/j.cellbi.2004.09.004.
Cornish J, Grey A, Callon KE, Naot D, Hill BL, Lin CQ, Balchin LM, Reid IR: Shared pathways of osteoblast mitogenesis induced by amylin, adrenomedullin, and IGF-1. Biochem Biophys Res Commun. 2004, 318: 240-246. 10.1016/j.bbrc.2004.04.020.
Bodegas E, Martinez A, Ozbun LL, Garayoa M, Letterio JJ, Montuenga LM, Jakowlew SB: Depressed adrenomedullin in the embryonic transforming growth factor-beta1 null mouse becomes elevated postnatally. Int J Dev Biol. 2004, 48: 67-70. 10.1387/ijdb.15005577.
Wu S, Yoshiko Y, De Luca F: Stanniocalcin 1 acts as a paracrine regulator of growth plate chondrogenesis. J Biol Chem. 2006, 281: 5120-5127. 10.1074/jbc.M506667200.
Filvaroff EH, Guillet S, Zlot C, Bao M, Ingle G, Steinmetz H, Hoeffel J, Bunting S, Ross J, Carano RA, et al: Stanniocalcin 1 alters muscle and bone structure and function in transgenic mice. Endocrinology. 2002, 143: 3681-3690. 10.1210/en.2001-211424.
Silha JV, Mishra S, Rosen CJ, Beamer WG, Turner RT, Powell DR, Murphy LJ: Perturbations in bone formation and resorption in insulin-like growth factor binding protein-3 transgenic mice. J Bone Miner Res. 2003, 18: 1834-1841. 10.1359/jbmr.2003.18.10.1834.
Ijiri K, Zerbini LF, Peng H, Correa RG, Lu B, Walsh N, Zhao Y, Taniguchi N, Huang XL, Out H, et al: A novel role for GADD45beta as a mediator of MMP-13 gene expression during chondrocyte terminal differentiation. J Biol Chem. 2005, 280: 38544-38555. 10.1074/jbc.M504202200.
Wang K, Vishwanath P, Eichler GS, Al-Sebaei MO, Edgar CM, Einhorn TA, Smith TF, Gerstenfeld LC: Analysis of fracture healing by large-scale transcriptional profile identified temporal relationships between metalloproteinase and ADAMTS mRNA expression. Matrix Biol. 2006, 25: 271-281. 10.1016/j.matbio.2006.02.001.
Sone S, Nakamura M, Maruya Y, Takahashi I, Mizoguchi I, Mayanagi H, Sasano Y: Expression of versican and ADAMTS during rat tooth eruption. J Mol Histol. 2005, 36: 281-288. 10.1007/s10735-005-5534-2.
Cornish J, Callon KE, Naot D, Palmano KP, Banovic T, Bava U, Watson M, Lin JM, Tong PC, Chen Q, et al: Lactoferrin is a potent regulator of bone cell activity and increases bone formation in vivo. Endocrinology. 2004, 145: 4366-4374. 10.1210/en.2003-1307.
Zayzafoon M, Gathings WE, McDonald JM: Modeled microgravity inhibits osteogenic differentiation of human mesenchymal stem cells and increases adipogenesis. Endocrinology. 2004, 145: 2421-2432. 10.1210/en.2003-1156.
Choi SJ, Han JH, Roodman GD: ADAM8: a novel osteoclast stimulating factor. J Bone Miner Res. 2001, 16: 814-822. 10.1359/jbmr.2001.16.5.814.
Kim MS, Magno CL, Day CJ, Morrison NA: Induction of chemokines and chemokine receptors CCR2b and CCR4 in authentic human osteoclasts differentiated with RANKL and osteoclast like cells differentiated by MCP-1 and RANTES. J Cell Biochem. 2006, 97: 512-518. 10.1002/jcb.20649.
Razzouk S, Lieberherr M, Cournot G: Rac-GTPase, osteoclast cytoskeleton and bone resorption. Eur J Cell Biol. 1999, 78: 249-255.
Sorensen MG, Henriksen K, Schaller S, Henriksen DB, Nielsen FC, Dziegiel MH, Karsdal MA: Characterization of osteoclasts derived from CD14+ monocytes isolated from peripheral blood. J Bone Miner Metab. 2007, 25: 36-45. 10.1007/s00774-006-0725-9.
Johnson GB, Riggs BL, Platt JL: A genetic basis for the 'Adonis' phenotype of low adiposity and strong bones. Faseb J. 2004, 18: 1282-1284.
Li F, Chung H, Reddy SV, Lu G, Kurihara N, Zhao AZ, Roodman GD: Annexin II stimulates RANKL expression through MAPK. J Bone Miner Res. 2005, 20: 1161-1167. 10.1359/JBMR.050207.
Chellaiah M, Kizer N, Silva M, Alvarez U, Kwiatkowski D, Hruska KA: Gelsolin deficiency blocks podosome assembly and produces increased bone mass and strength. J Cell Biol. 2000, 148: 665-678. 10.1083/jcb.148.4.665.
Tani-Ishii N, Penninger JM, Matsumoto G, Teranaka T, Umemoto T: The role of LFA-1 in osteoclast development induced by co-cultures of mouse bone marrow cells and MC3T3-G2/PA6 cells. J Periodontal Res. 2002, 37: 184-191. 10.1034/j.1600-0765.2002.00610.x.
Miura Y, Miura M, Gronthos S, Allen MR, Cao C, Uveges TE, Bi Y, Ehirchiou D, Kortesidis A, Shi S, et al: Defective osteogenesis of the stromal stem cells predisposes CD18-null mice to osteoporosis. Proc Natl Acad Sci USA. 2005, 102: 14022-14027. 10.1073/pnas.0409397102.
Sugatani T, Alvarez U, Hruska KA: PTEN regulates RANKL- and osteopontin-stimulated signal transduction during osteoclast differentiation and cell motility. J Biol Chem. 2003, 278: 5001-5008. 10.1074/jbc.M209299200.
Shi C, Zhang X, Chen Z, Sulaiman K, Feinberg MW, Ballantyne CM, Jain MK, Simon DI: Integrin engagement regulates monocyte differentiation through the forkhead transcription factor Foxp1. J Clin Invest. 2004, 114: 408-418. 10.1172/JCI200421100.
Gantner F, Kupferschmidt R, Schudt C, Wendel A, Hatzelmann A: In vitro differentiation of human monocytes to macrophages: change of PDE profile and its relationship to suppression of tumour necrosis factor-alpha release by PDE inhibitors. Br J Pharmacol. 1997, 121: 221-231. 10.1038/sj.bjp.0701124.
Holmen SL, Zylstra CR, Mukherjee A, Sigler RE, Faugere MC, Bouxsein ML, Deng L, Clemens TL, Williams BO: Essential role of beta-catenin in postnatal bone acquisition. J Biol Chem. 2005, 280: 21162-21168. 10.1074/jbc.M501900200.
Almeida M, Han L, Bellido T, Manolagas SC, Kousteni S: Wnt proteins prevent apoptosis of both uncommitted osteoblast progenitors and differentiated osteoblasts by beta-catenin-dependent and -independent signaling cascades involving Src/ERK and phosphatidylinositol 3-kinase/AKT. J Biol Chem. 2005, 280: 41342-41351. 10.1074/jbc.M502168200.
Liu X, Bruxvoort KJ, Zylstra CR, Liu J, Cichowski R, Faugere MC, Bouxsein ML, Wan C, Williams BO, Clemens TL: Lifelong accumulation of bone in mice lacking Pten in osteoblasts. Proc Natl Acad Sci USA. 2007, 104: 2259-2264. 10.1073/pnas.0604153104.
Sneddon WB, Syme CA, Bisello A, Magyar CE, Rochdi MD, Parent JL, Weinman EJ, Abou-Samra AB, Friedman PA: Activation-independent parathyroid hormone receptor internalization is regulated by NHERF1 (EBP50). J Biol Chem. 2003, 278: 43787-43796. 10.1074/jbc.M306019200.
Kulkarni NH, Halladay DL, Miles RR, Gilbert LM, Frolik CA, Galvin RJ, Martin TJ, Gillespie MT, Onyia JE: Effects of parathyroid hormone on Wnt signaling pathway in bone. J Cell Biochem. 2005, 95: 1178-1190. 10.1002/jcb.20506.
Katoh M: WNT/PCP signaling pathway and human cancer [review]. Oncol Rep. 2005, 14: 1583-1588.
Liu B, Yu HM, Hsu W: Craniosynostosis caused by Axin2 deficiency is mediated through distinct functions of beta-catenin in proliferation and differentiation. Dev Biol. 2007, 301: 298-308. 10.1016/j.ydbio.2006.10.018.
Shore EM, Xu M, Feldman GJ, Fenstermacher DA, Cho TJ, Choi IH, Connor JM, Delai P, Glaser DL, LeMerrer M, et al: A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nat Genet. 2006, 38: 525-527. 10.1038/ng1783.
Maeda Y, Tsuji K, Nifuji A, Noda M: Inhibitory helix-loop-helix transcription factors Id1/Id3 promote bone formation in vivo. J Cell Biochem. 2004, 93: 337-344. 10.1002/jcb.20154.
de Jong DS, van Zoelen EJ, Bauerschmidt S, Olijve W, Steegenga WT: Microarray analysis of bone morphogenetic protein, transforming growth factor beta, and activin early response genes during osteoblastic cell differentiation. J Bone Miner Res. 2002, 17: 2119-2129. 10.1359/jbmr.2002.17.12.2119.
Wiater E, Vale W: Inhibin is an antagonist of bone morphogenetic protein signaling. J Biol Chem. 2003, 278: 7934-7941. 10.1074/jbc.M209710200.
Abe Y, Abe T, Aida Y, Hara Y, Maeda K: Follistatin restricts bone morphogenetic protein (BMP)-2 action on the differentiation of osteoblasts in fetal rat mandibular cells. J Bone Miner Res. 2004, 19: 1302-1307. 10.1359/JBMR.040408.
Acknowledgements
The authors thank the donors and donors' families for their kind donation of bone tissue used for this study. The authors thank the orthopaedic surgeons and nursing staff of The Department of Orthopaedics and Trauma in the Royal Adelaide Hospital for support and cooperation in the collection of femoral specimens and the mortuary staff of the Institute of Medical and Veterinary Science for the collection of autopsy specimens. Thanks to Julia Kuliwaba and Helen Tsangari for processing and preparation of RNA from a subset of the samples used in this work. This work was supported by the National Health and Medical Research Council (NHMRC). The Compugen human oligonucleotide library for the microarray was purchased with Australian Cancer Research Foundation (ACRF) funds through the AMF. We thank Ashley Connolly and Mark Van der Hoek from the AMF for their guidance with the microarray experiments. We thank Tina Vincent from Discipline of Orthopaedics and Trauma, University of Adelaide, for advice with real-time PCR experiments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
NLF and DMF conceived the study. BH contributed to study design and performed the acquisition of the microarray and real-time PCR data. AT advised on the microarray experiment design and performed the statistical analyses of the microarray data. BH and AT analyzed and interpreted the data. BH, DMF and NLF prepared the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hopwood, B., Tsykin, A., Findlay, D.M. et al. Microarray gene expression profiling of osteoarthritic bone suggests altered bone remodelling, WNT and transforming growth factor-β/bone morphogenic protein signalling. Arthritis Res Ther 9, R100 (2007). https://doi.org/10.1186/ar2301
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar2301