Abstract
Recently, we reported that genetic polymorphisms within the human IL18 gene were associated with disease susceptibility to adult-onset Still's disease (AOSD), which is characterized by extraordinarily high serum levels of IL-18. Because high serum IL-18 induction has also been observed in the systemic type of juvenile idiopathic arthritis (JIA), we investigated whether similar genetic skewing is present in this disease. Three haplotypes, S01, S02, and S03, composed of 13 genetic polymorphisms covering two distinct promoter regions, were determined for 33 JIA patients, including 17 with systemic JIA, 10 with polyarthritis, and 6 with oligoarthritis. Haplotypes were also analyzed for 28 AOSD patients, 164 rheumatoid arthritis (RA) patients, 102 patients with collagen diseases, and 173 healthy control subjects. The frequency of individuals carrying a diplotype configuration (a combination of two haplotypes) of S01/S01 was significantly higher in the JIA patients, including all subgroups, than in the healthy controls (P = 0.0045, Fischer exact probability test; odds ratio (OR) = 3.55, 95% confidence interval (CI) = 1.55–8.14). In patients with systemic JIA, its frequency did not differ statistically from that of normal controls. Nevertheless, it is possible that haplotype S01 is associated with the phenotype of high IL-18 production in systemic JIA because the patients carrying S01/S01 showed significantly higher serum IL-18 levels compared with patients with other diplotype configurations (P = 0.017, Mann-Whitney U test). We confirmed that the frequency of the diplotype configuration of S01/S01 was significantly higher in AOSD patients than in healthy control subjects (P = 0.011, OR = 3.45, 95% CI = 1.42–8.36). Furthermore, the RA patients were also more predisposed to have S01/S01 (P = 0.018, OR = 2.00, 95% CI = 1.14–3.50) than the healthy control subjects, whereas the patients with collagen diseases did not. In summary, the diplotype configuration of S01/S01 was associated with susceptibility to JIA as well as AOSD and RA, and linked to significantly higher IL-18 production in systemic JIA. Possession of the diplotype configuration of S01/S01 would be one of the genetic risk factors for susceptibility to arthritis in the Japanese population.
Similar content being viewed by others
Introduction
IL-18 is produced by a wide range of immune cells, such as monocytes, macrophages, and dendritic cells. Initially thought to be an IFN-γ-inducing factor of T cells and natural killer cells [1, 2], IL-18 has been found to have multiple biological functions. Interestingly, IL-18 is a unique cytokine that stimulates both T helper (Th)1- and Th2-type immune responses, depending on its cytokine milieu [3]. In combination with IL-12, IL-18 induces IFN-γ production in Th1 cells, B cells, and natural killer cells, promoting Th1-type immune responses [4]. When cultured with IL-2, however, IL-18 induces Th2 lineage in CD4+ T cells [5]. In basophils and mast cells, IL-18 together with IL-3 also induces production of Th2 cytokines [6]. In vivo, IL-18 regulates innate and acquired immune responses, controlling either Th1 or Th2 cytokine balance. To date, inappropriate IL-18 production has been reported both in chronic inflammatory diseases such as Crohn's disease [7] and rheumatoid arthritis (RA) [8, 9], and in allergic diseases such as bronchial asthma and atopic dermatitis [10].
We previously reported that serum IL-18 levels were significantly elevated and well correlated with disease activity and severity [11] in adult-onset Still's diseases (AOSD), which is characterized by high spiking fever, polyarthralgia, evanescent salmon-colored rash, liver dysfunction, splenomegaly and hyper ferritinemia [12]. Although serum levels of inflammatory cytokines are generally high in AOSD patients [13], the levels of IL-18 were enormously high, reaching more than 1,000 times the levels found in normal controls and other chronic inflammatory diseases such as RA [11, 14]. Therefore, we have suggested that IL-18 is closely involved in the pathogenesis of AOSD.
Juvenile idiopathic arthritis (JIA) is a chronic arthritis of childhood and belongs to a group of clinically heterogeneous disorders including oligoarthritis, polyarthritis, systemic arthritis, secondary arthritis, and other arthritis types. According to the International League of Associations for Rheumatology (ILAR) classification criteria, oligoarthritis is further subdivided into persistent and extended oligoarthritis, and polyarthritis is further subdivided into rheumatoid factor-positive and negative polyarthritis. Thus, JIA is categorized into seven clinically distinct presentations [15], and the pathogenesis differs among the subgroups. Systemic JIA is characterized by systemic involvement, such as high spiking fever, skin rash, serositis and hepatosplenomegaly, and overproduction of inflammatory cytokines [16, 17]. Maeno and colleagues [18] reported the serum levels of IL-18 were strikingly high in systemic JIA compared with other JIA subgroups and other childhood inflammatory disorders. Among systemic JIA patients, individuals with hepatosplenomegaly or serositis showed higher serum IL-18 levels than those without such manifestations [18]. In addition to similar clinical findings, aberrant production of IL-18 is a characteristic feature in both AOSD and systemic JIA, which is the reason why many investigators may consider these two diseases to be the same entity.
The human IL18 gene is located on chromosome 11q22.2 – q22.3 [19] and is composed of six exons; the translation-starting site is present in exon 2 [20]. It lacks a TATA box, and its expression is regulated by at least two distinct promoter regions, one of which is located upstream of untranslated exon 1 (promoter 1) [20–24], and the other upstream of exon 2 (promoter 2) [23]. Promoter 1 is up-regulated by various stimulants in macrophages [20], intestinal epithelial cells [21], and epithelial-like cell lines [24]. A 108 base-pair (bp) 5' flanking region upstream of exon 1 contains a PU.1 (purine-rich sequence) consensus-binding site and a GC-rich region; this region is critical for the sodium butyrate-stimulated promoter 1 activity [21, 25]. Promoter 2 is considered to act constitutively [23], but regulation of human IL18 gene expression has not been fully examined.
We speculated that genetic polymorphisms within the promoter region of the IL18 gene might contribute to the high IL-18 production in AOSD. Thus, in the previous study, we performed a systematic search for polymorphisms in a 6.7 kb sequence, including a putative promoter region of the IL18 gene, and then identified 10 single nucleotide polymorphisms (SNPs) and a single 9 bp insertion [26]. The region had been reported to be upstream of exon 2 (intron 1) [24]. Later, Kalina and colleagues [20] determined that the 6.7 kb sequence was upstream of exon 1 instead of exon 2 by using 5' rapid amplification of cDNA ends; thus, this 6.7 kb region includes promoter 1 of the IL18 gene. We identified some of these polymorphisms as components of haplotypes and found there were three major haplotypes in the Japanese population (S01, S02, and S03). Furthermore, the frequency of haplotype S01, especially the diplotype configuration of S01/S01, was significantly higher in AOSD than in RA as well as in normal controls [26].
In the present study, we conducted a case-control study to evaluate possible associations of haplotype S01 of the IL18 gene with susceptibility to JIA, especially to systemic JIA.
Materials and methods
Patients and control subjects
The present study has been approved by the institutional Genome-Ethics Committee of Tokyo Women's Medical University and Kagoshima University. We examined 33 patients with JIA who were followed at the Pediatric Department of Kagoshima University Hospital, with informed consent. Of these patients, 17 had systemic JIA (female, 47.1%), 10 had polyarthritis (female, 70%), and 6 had oligoarthritis (female, 100%). All the patients satisfied the ILAR classification criteria for JIA [15]. We also examined 28 patients with AOSD (female, 79%), 164 patients with RA (female, 81%), and 102 patients with collagen diseases (female, 84%) who were followed at the Institute of Rheumatology, Tokyo Women's Medical University, with informed consent, as well as 173 healthy individuals (female, 64.7%). All the patients with AOSD met the criteria for AOSD of both Cush and colleagues [12] and Yamaguchi and colleagues [27]. All the RA patients fulfilled the 1987 classification criteria for RA of the American College of Rheumatology [28]. The patients with collagen diseases included 38 patients with systemic lupus erythematosus, 38 patients with scleroderma, and 26 patients with polymyositis/dermatomyositis. All the patients with these three diseases fulfilled the 1982 revised criteria of the American Rheumatology Association for the classification of systemic lupus erythematosus [29], the American College of Rheumatology criteria for scleroderma [30] and the diagnostic criteria of Bohan and Peter for polymyositis/dermatomyositis [31]. All subjects were Japanese.
DNA isolation and genotyping
Genomic DNA was isolated from peripheral blood. For all the patients and control individuals, the genotype of SNPs 1, 2, 4, 5, 6, 9, 11, 12, 13, and 14 were determined by allelic discrimination chemistry using the ABI PRISM 7900HT Sequence Detection System (Applied Biosystems, Foster City, CA, USA). In the present study, we typed these 10 polymorphic sites for each individual because they were sufficient to estimate the haplotype and a diplotype configuration. As listed in Table 2, a set of forward and reverse primers and fluorescent-labeled probes were prepared. The probe designed to hybridize specifically to allele 1 was labeled by VIC, while that for allele 2 was labeled by FAM. A 10 μl portion of PCR mixture contained 9 pM each of the forward and reverse primers, 2 pM each of probes, 10 ng of genomic DNA as a template, and TaqMan PCR Universal Master Mix containing AmpliTaq Gold DNA polymerase (Applied Biosystems). During PCR, each probe annealed specifically to complementary sequences between the forward and reverse primer sites. AmpliTaq Gold DNA polymerase cleaved probes that hybridize to the target, and the cleavage separated the reporter dye from the probe. By comparing the fluorescent signals generated during PCR amplification, we determined the sequences present in the sample. When the fluorescent signal was VIC only, the sample was homozygous for allele 1. Similarly, with FAM fluorescence only, the sample was homozygous for allele 2. When both fluorescent signals were increased, the sample was heterozygous.
Serum IL-18 measurement
Serum concentrations of IL-18 were measured by enzyme-linked immunosorbent assay (ELISA) with the use of a commercial kit (IL-18 ELISA Kit; MBL, Nagoya, Japan).
Statistical analysis
To compare the frequencies of the haplotype or the diplotype configurations, we used the Fisher exact probability test. Differences were considered to be significant at P < 0.05. Odds ratios (ORs) were determined for disease susceptibility in carriers of a specific haplotype or a diplotype configuration. The 95% confidence intervals (CI) for ORs were also calculated. The data on serum IL-18 levels were expressed as the mean ± standard deviation, and the statistical significance of differences between two groups was determined by the Mann-Whitney U test.
Results
Polymorphisms of the human IL18gene
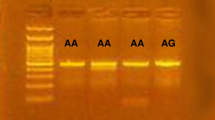
In the previous study, we have reported the presence of 10 SNPs (SNP1 to SNP10) and a single 9 bp (AACAGGACA) insertion in a 6.7 kb sequence upstream of exon 1 of the IL18 gene [26]. Of these, SNPs 1, 2, 4, 5, 6, 9, and 10 and the single 9 bp insertion are components of three major haplotypes, S01, S02, and S03, in the Japanese population. We also investigated previously reported SNPs by other investigators [22, 32] within the IL18 gene and, with the use of a PENHAPLO computer program [33], found that some of them were also components of these haplotypes. SNP9 and SNP10 corresponded to SNPs previously reported by Giedraitis and colleagues [22] as -656 G/T and -607 C/A, respectively. They also reported three additional SNPs spanning from promoter 1 to exon 1. In this manuscript, we tentatively refer to -137 G/C as SNP11, +113 T/G as SNP12, and +127 C/T as SNP13. Furthermore, Kuruse and colleagues [32] reported three SNPs located upstream of exon 2, of which -920 T/C and -133 C/G were also components of three haplotypes, and are tentatively called SNP14 and SNP15, respectively. Thus, a single 9 bp insertion and SNPs 1, 2, 4, 5, 6, 9, 10, 11, 12, 13, 14, and 15 are the components of three haplotypes (Figure 1). The position of each SNP, allelic frequencies, and functions are summarized in Table 1. Nucleotides at the 12 SNP sites and presence or absence of the 9 bp insertion were as follows: haplotype S01, T, G, C, G, C, T, A, G, T, C, T, and C with the 9 bp insertion; haplotype S02, C, A, T, C, T, G, C, G, T, C, C, and C without the 9 bp insertion; haplotype S03, T, A, T, C, C, T, A, C, G, T, C, and G with the 9 bp insertion (Figure 1). The 9 bp insertion, and SNPs 1, 6, 9, and 10 were in complete linkage disequilibrium (D' = 1), while SNPs 2, 4, 5, and 14 were also in complete linkage disequilibrium (D' = 1). Furthermore, SNPs 11, 12, 13, and 15 were in complete linkage disequilibrium (D' = 1). These haplotypes spanned from the 5' 6.7 kb flanking exon 1 to intron 1, and included both promoter 1 and promoter 2 regions of the human IL18 gene.
A unique combination of 13 polymorphisms comprising three different haplotypes: S01, S02 and S03. The 9 bp insertion, single nucleotide polymorphisms (SNPs) 1, 6, 9, and 10 (open box); SNP2, 4, 5, and 14 (dark gray box), and SNP11, 12, 13, and 15 (gray box) are in linkage disequilibrium. An underline indicates a minor allele in the normal Japanese population. +, 9 bp (AACAGGACA) is inserted; -, 9 bp is not inserted.
The frequencies of haplotypes and diplotype configurations in JIA
The allelic frequencies of three haplotypes of the IL18 gene in patients with JIA and healthy control subjects are summarized in Table 3. The frequency of haplotype S01 was significantly higher in the JIA patients as a whole than the healthy controls (P = 0.011, Fisher exact probability test; OR = 1.97, 95% CI = 1.16–3.35). With regard to the JIA subgroups, the patients with oligoarthritis were predisposed to have haplotype S01 (P = 0.0021, Fisher exact probability test; OR = 8.21, 95% CI = 1.77–38.04). In the polyarthritis and systemic subgroups, the frequency of haplotype S01 did not differ statistically from that of healthy controls. The frequency of haplotype S01 was also significantly higher in the patients with AOSD than in healthy controls (P = 0.028, Fisher exact probability test; OR = 1.89, 95% CI = 1.07–3.34). Furthermore, the patients with RA were also predisposed to have haplotype S01, compared with the healthy controls (P = 0.013, Fisher exact probability test; OR = 1.49, 95% CI = 1.10–2.02).
The six diplotype configurations in the Japanese population include S01/S01, S01/S02, S01/S03, S02/S02, S02/S03, and S03/S03. As shown in Table 4, the frequency of the S01/S01 diplotype configuration was significantly higher in the JIA patients than the healthy controls (P = 0.0045, Fischer exact probability test; OR = 3.55, 95% CI = 1.55–8.14). For the JIA subgroups, the frequency of the S01/S01 diplotype configuration was significantly higher in the patients with oligoarthritis (P = 0.0059, Fisher exact probability test; OR = 12.42, 95% CI = 2.15–71.55) and polyarthritis (P = 0.048, Fisher exact probability test; OR = 4.14, 95% CI = 1.09–15.75) than healthy controls. The frequency of S01/S01 in patients with systemic JIA did not differ statistically from that of healthy controls. In comparison with the normal controls, the frequency of S01/S01 also was significantly higher in the AOSD (P = 0.011, Fisher exact probability test; OR = 3.45, 95% CI = 1.42–8.36) and RA patients (P = 0.018, Fisher exact probability test; OR = 2.00, 95% CI = 1.14–3.50).
Association of the S01/S01 diplotype configuration with serum IL-18 levels
Serum IL-18 levels were measured for each patient with JIA before immunosuppressive treatment. As reported previously [18], serum IL-18 levels were enormously high in patients with systemic JIA compared to other subgroups of JIA. In the 17 patients with systemic JIA, serum IL-18 levels were significantly higher in the patients carrying S01/S01 (n = 4) than in those carrying other diplotype configurations (n = 13) (78,683 ± 22,778 pg/ml versus 10,122 ± 28,210 pg/ml; P = 0.017 by Mann-Whitney U test; Figure 2). In the other JIA subgroups, mean IL-18 levels in patients with and without the S01/S01 diplotype configuration were 572 ± 327 pg/ml versus 325 ± 302 pg/ml in those with polyarthritis, and 252 ± 124 pg/ml versus 219 ± 48 pg/ml in those with oligoarthritis. The IL-18 levels did not differ statistically among the diplotype configurations in the patients with polyarthritis and oligoarthritis.
Discussion
The present study has demonstrated a strong association between the haplotype S01 of the IL18 gene and JIA as well as AOSD and RA in the Japanese population. Initially, we speculated that haplotype S01 is specific to systemic JIA because of previous studies that showed enormously high IL-18 production both in AOSD and systemic JIA [11, 14, 18] and genetic skewing of the haplotype S01 in AOSD [26]. However, haplotype S01 was associated with all the subgroups of JIA in the Japanese population, and we did not find the expected statistically significant correlation of haplotype S01 with susceptibility to systemic JIA. Furthermore, haplotype S01 was found to be associated with the whole group of arthritis diseases, including JIA, ASOD and RA.
Genetic polymorphisms of the human IL18 gene have been associated with a wide variety of diseases, including allergic diseases and inflammatory diseases [32, 34–36]. These observations might reflect the redundancy of the IL-18 protein, which has multiple biological functions promoting both Th1- and Th2-type immune responses. Previously reported polymorphic sites concentrated on two promoter regions and the untranslated exon 1 of the IL18 gene. Most of the investigators have compared the frequency of each allele in the disease population with that of a healthy population. In a previous study [26], we demonstrated that all of these genetic polymorphisms comprised a haplotype. We therefore checked the genotypic data reported by other investigators and estimated the carrying rate of each haplotype in the disease populations. Interestingly, we found differently genetically skewed haplotypes in each disorder. For example, in the white population of Germany, patients with atopic phenotypes were predisposed to have -137 C in promoter 1, +113 G in exon 1, +127 T in exon 1, and -133 G in promoter 2 [32], and each allele corresponded to the minor allele of SNPs 11, 12, 13, and 15, respectively. All of these were the components of haplotype S03. Other investigators reported that SNPs specific for haplotype S03 are linked to susceptibility to atopic eczema in Germany [34], and asthma in Japanese [35]. It was likely that haplotype S03 of the IL18 gene was associated with atopic disorders, typical of Th2-dominant disease. On the other hand, Japanese patients with sarcoidosis were reported to be associated with polymorphisms specific for haplotype S02 [36]. The present study shows that haplotype S01 is associated with JIA as well as AOSD and RA in the Japanese population, with each having arthritis as a phenotype. In view of imbalanced immune responses, these diseases may be considered as Th1-dominant disorders [37–39]. By analyzing haplotypes, it became clear that haplotypes S01 and S03 of the IL18 gene are involved in the susceptibility of quite different types of disorders.
It is important to note there is an essential racial difference in the distribution of haplotypes. According to our data, the frequency of haplotype S01 of the IL18 gene is 37.9% and that of the S01/S01 diplotype configuration is 13.9% in the Japanese population. We also estimated the frequency of haplotypes and/or the diplotype configurations in the different ethnic groups of previous reports. The frequency of the S01/S01 diplotype configuration was considered to be only 1% in the healthy Swedish population [22] and only 0.05% in the Chinese population [38], much lower than that of the Japanese population. Also, in German whites, the frequency of haplotype S01 was 13% [40]. Interestingly, the existence of the fourth major haplotype, which we tentatively call haplotype S04, was reported in the Polish population [41]. The haplotype S04 is composed of combinations of nucleotides of SNP 10 C and SNP 11 C [41]; we have never observed this haplotype in the Japanese population. As described, the carrying rate of each haplotype is quite different among ethnic groups, which would be one reason why a disease-associated haplotype is not necessarily common among them. Indeed, no increase in the frequency of the S01/S01 diplotype configuration was observed in RA patients in Chinese patients [42] and in JIA patients in Germany [40]. One reason why haplotype S01 of the IL18 gene is skewed in Japanese arthritis patients is due to a basal high frequency of the haplotype S01 in the Japanese population.
The findings in the present study raise the question of how these genetic polymorphisms within the human IL18 gene influence the phenotype. One consideration is that nucleotide substitution directly influences the transcription of the gene. SNP11 is located at the GATA3 binding site, which is involved strongly in Th2 differentiation [43]. The C allele of SNP11 is specific to the haplotype S03, which might be a good explanation for the association of haplotype S03 and atopic disorders. As for haplotype S01, there have been few good explanations as to why it is linked to extraordinarily high IL-18 production. Nucleotide substitutions specific for haplotype S01 (SNP2, 4, 5 and 14) do not create known nucleotide factor-binding sequences; however, it is still possible that undefined genetic polymorphisms in linkage disequilibrium with haplotype S01 exist in other regions of the IL18 gene and influence the expression of IL-18 protein.
The aim of the present study was to examine whether haplotype S01 of the IL18 gene was skewed in systemic JIA. The frequency of the S01/S01 diplotype configuration seemed to be higher in patients with systemic JIA than in healthy controls (23.5% versus 13.9%), but the difference was not statistically significant, probably because of the relatively small study populations. Although we could not prove haplotype S01 was associated with disease susceptibility, the haplotype was linked to some clinical features. The patients carrying the S01/S01 diplotype configuration showed significantly higher IL-18 protein levels than those without it (P = 0.017). Thus, it is possible that haplotype S01 of the IL18 gene is linked to the phenotype of high IL-18 production. Because serum IL-18 levels indicate disease severity [18], the haplotype S01 might be a marker of severe disease condition in systemic JIA. In addition, although the differences were not statistically significant, the patients with the S01/S01 diplotype configuration tended to be younger at disease onset, need immunosuppressive drugs in addition to high doses of corticosteroids to control severe disease activity, and have the complication macrophage-activating syndrome (data not shown). Similarly, in AOSD, the S01/S01 diplotype configuration correlated with disease severity (unpublished data).
The mechanism of induction of enormously high IL-18 protein production in AOSD and systemic JIA is unclear, but it is likely that infectious agents such as viruses trigger the activation of macrophages and induce IL-18 production, and that some immunological breakdowns fail to control sustained activation of macrophages and consequently cause continuous IL-18 production. Several candidate genes would be involved in these phenomena besides the IL18 gene itself. They might include factors regulating IL-18 mRNA transcription or translation and caspase-1, which cleaves pro-IL-18 into a mature form [44]. We suggest that haplotype S01 of the IL18 gene might influence IL-18 protein production via unknown mechanisms, which explains in part the enormously high IL-18 production in systemic JIA. Furthermore, homozygosity for S01 would be more important for susceptibility to JIA as well as AOSD and RA than only carrying the S01 haplotype, since the P value for the former was smaller than that of the latter.
The present study also shows that haplotype S01 of the IL18 gene is widely linked to susceptibility to arthritis in the Japanese population. As described above, IL-18 is a key cytokine involved in the pathogenesis of both AOSD and systemic JIA [11, 14, 18]. High IL-18 protein could induce liver injury [45] or arthritis [8]. In RA, several lines of evidences suggest that IL-18 plays a role in the pathogenesis because IL-18 is up-regulated and induces production of inflammatory cytokines such as tumor necrosis factor-alpha in synovium [8, 9]. In collagen-induced arthritis, IL-18 promotes arthritis via tumor necrosis factor-alpha induction [46]. In another study, IL-18 knockout mice showed a reduced degree of inflammation, and the administration of recombinant IL-18 reversed collagen-induced arthritis [47]. In these disorders, including JIA, AOSD and RA, overproduction of IL-18, probably together with IL-12, would shift the immune response to the Th1 lineage. Indeed, peripheral blood obtained from AOSD patients showed more IFN-γ producing Th cells and a higher Th1/Th2 ratio than in healthy controls [37]. Th1 cytokine expression has been demonstrated in the synovium of RA and JIA [38, 39]. As described, IL-18 would be involved in the pathogenesis of arthritis directly or via production of other cytokines, and probably would promote a Th1-type immune response. Among three haplotypes of the IL18 gene, haplotype S01 might contribute genetically to the development of arthritis in the Japanese population. This is supported by the observation that the frequency of the S01/S01 diplotype configuration was significantly higher in arthritis patients as a whole, including JIA, AOSD and RA, than normal controls (P = 0.0013, OR = 2.36, 95% CI = 1.36–4.12) or patients with collagen diseases (P = 0.0069, OR = 2.39, 95% CI = 1.22–4.75, data not shown).
Conclusion
The frequency of haplotype S01 of the IL18 gene, which has been shown to be the genetic risk factor for susceptibility to AOSD, is also high in Japanese patients with JIA. The diplotype configuration of S01/S01 further increases the risk for the disease susceptibility. Although the frequency of the S01/S01 diplotype configuration did not differ statistically from that of normal controls in patients with systemic JIA, individuals carrying this diplotype configuration showed significantly higher serum IL-18 levels. The skewing of haplotype S01 and the S01/S01 diplotype configuration was also observed in patients with RA as well as in those with AOSD. In conclusion, having the S01/S01 diplotype configuration in the IL18 gene would be one genetic risk factor for susceptibility of the Japanese population to JIA, as well as RA and AOSD, and might contribute to high IL-18 protein production in systemic JIA.
Abbreviations
- AOSD:
-
= adult-onset Still's disease
- bp:
-
= base-pair
- CI:
-
= confidence interval
- IFN:
-
= interferon
- IL:
-
= interleukin
- ILAR:
-
= International League of Associations for Rheumatology
- JIA:
-
= juvenile idiopathic arthritis
- OR:
-
= odds ratio
- RA:
-
= rheumatoid arthritis
- SNP:
-
= single nucleotide polymorphism
- Th:
-
= T helper.
References
Okamura H, Tsutsi H, Komatsu T, Yutsudo M, Hakura A, Tanimoto T, Torigoe K, Okura T, Nukada Y, Hattori K: Cloning of a new cytokine that induces IFN-γ production by T cells. Nature. 1995, 378: 88-91. 10.1038/378088a0.
Ushio S, Namba M, Okura T, Hattori K, Nukada Y, Akita K, Tanabe F, Konishi K, Micallef M, Fujii M: Cloning of the cDNA for human IFN-gamma-inducing factor, expression in Escherichia coli, and studies on the biologic activities of the protein. J Immunol. 1996, 156: 4274-4279.
Nakanishi K, Yoshimoto T, Tsutsui H, Okamura H: Interleukin-18 regulates both Th1 and Th2 responses. Annu Rev Immunol. 2001, 19: 423-474. 10.1146/annurev.immunol.19.1.423.
Yoshimoto T, Takeda H, Tanaka T, Ohkusu K, Kawashima S, Okamura H, Akira S, Nakanishi K: IL-12 up-regulates IL-18 receptor expression on T cells, Th1 cells and B cells: synergism with IL-18 for IFN-gamma production. J Immunol. 1998, 161: 3400-3407.
Yoshimoto T, Mizutani H, Tsutsui H, Noben-Trauth N, Yamanaka M, Izumi S, Okamura H, Paul WE, Nakanishi K: IL-18 induction of IgE: dependence on CD4+ T cells, IL-4 and STAT6. Nat Immunol. 2000, 1: 132-137. 10.1038/77811.
Yoshimoto T, Tsutsui H, Tominaga K, Hoshino K, Okamura H, Akira S, Paul WE, Nakanishi K: IL-18, although antiallergic when administered with IL-12, stimulates IL-4 and histamine release by basophils. Proc Natl Acad Sci USA. 1999, 96: 13962-13966. 10.1073/pnas.96.24.13962.
Pizarro TT, Michie MH, Bentz M, Woraratanadharm J, Smith MF, Foley E, Moskaluk CA, Bickston SJ, Cominelli F: IL-18, a novel immunoregulatory cytokine, is up-regulated in Crohn's disease: expression and localization in intestinal mucosal cells. J Immunol. 1999, 162: 6829-6835.
Gracie JA, Forsey RJ, Chan WL, Gilmour A, Leung BP, Greer MR, Kennedy K, Carter R, Wei XQ, Xu D, et al: A proinflammatory role for IL-18 in rheumatoid arthritis. J Clin Invest. 1999, 104: 1393-1401.
Tanaka M, Harigai M, Kawaguchi Y, Ohta S, Sugiura T, Takagi K, Ohsako-Higami S, Fukasawa C, Hara M, Kamatani N: Mature form of interleukin 18 is expressed in rheumatoid arthritis synovial tissue and contributes to interferon-γ production by synovial T cells. J Rheumatol. 2001, 28: 1779-1787.
El-Mezzein RE, Matsumoto T, Nomiyama H, Miike T: Increased secretion of IL-18 in vitro by peripheral boold mononuclear cells of patients with bronchial asthma and atopic dermatitis. Clin Exp Immunol. 2001, 126: 193-198. 10.1046/j.1365-2249.2001.01664.x.
Kawaguchi Y, Terajima H, Harigai M, Hara M, Kamatani N: Interleukin-18 as a novel diagnostic marker and indicator of disease severity in adult-onset Still's disease. Arthritis Rheum. 2001, 44: 1716-1718. 10.1002/1529-0131(200107)44:7<1716::AID-ART298>3.0.CO;2-I.
Cush JJ, Medsger TA, Christy WC, Herbert DC, Cooperstein LA: Adult-onset Still's disease: clinical course and outcome. Arthritis Rheum. 1987, 30: 186-194.
Hoshino T, Ohta A, Yang D, Kawamoto M, Kikuchi M, Inoue Y, Kamizono S, Ota T, Itoh K, Oizumi K: Elevated serum interleukin 6, interferon-γ and tumor necrosis factor-α levels in patients with adult Still's disease. J Rheumatol. 1998, 25: 396-398.
Kawashima M, Yamamura M, Taniai M, Yamauchi H, Tanimoto T, Kurimoto M, Miyawaki S, Amano T, Takeuchi T, Makino H: Levels of interleukin-18 and its binding inhibitors in the blood circulation of patients with adult-onset Still's disease. Arthritis Rheum. 2001, 44: 550-560. 10.1002/1529-0131(200103)44:3<550::AID-ANR103>3.0.CO;2-5.
Petty RE, Southwood TR, Baum J, Bhettay E, Glass DN, Manners P, Maldonado-Cocco J, Suarez-Almazor M, Orozco-Alcala J, Prieur AM: Revision of the proposed classification criteria for juvenile idiopathic arthritis: Durban, 1997. J Rheumatol. 1998, 25: 1991-1994.
de Benedetti F, Massa M, Robbioni P, Ravelli A, Burgio GR, Martini A: Correlation of serum interleukin-6 levels with joint involvement and thrombocytosis in systemic juvenile rheumatoid arthritis. Arthritis Rheum. 1991, 34: 1158-1163.
de Benedetti F, Pignatti P, Massa M, Sartirana P, Ravelli A, Cassani G, Corti A, Martini A: Soluble tumor necrosis factor receptor levels reflect coagulation abnormalities in systemic juvenile chronic arthritis. Br J Rheumatol. 1997, 36: 581-588. 10.1093/rheumatology/36.5.581.
Maeno N, Takei S, Nomura Y, Imanaka H, Hokonohara M, Miyata K: Highly elevated serum levels of interleukin-18 in systemic juvenile idiopathic arthritis but not in other juvenile idiopathic arthritis subtypes or in Kawasaki disease. Arthritis Rheum. 2002, 46: 2539-2541. 10.1002/art.10389.
Nolan KF, Greaves DR, Waldmann H: The human interleukin 18 gene IL18 maps to 11q22.2-q22.3, closely linked to the DRD2 gene locus and distinct from mapped IDDM loci. Genomics. 1998, 51: 161-163. 10.1006/geno.1998.5336.
Kalina U, Ballas K, Koyama N, Kauschat D, Miething C, Arnemann H, Martin H, Hoelzer D, Ottmann OG: Genomic organization and regulation of the human interleukin-18 gene. Scand J Immunol. 2000, 52: 525-530. 10.1046/j.1365-3083.2000.00836.x.
Kalina U, Koyama N, Hosoda T, Nuernberger H, Sato K, Hoelzer D, Herweck F, Manigold T, Singer MV, Rossol S: Enhanced production of IL-18 in butyrate-treated intestinal epithelium by stimulation of the proximal promoter region. Eur J Immunol. 2002, 32: 2635-2643. 10.1002/1521-4141(200209)32:9<2635::AID-IMMU2635>3.0.CO;2-N.
Giedraitis V, He B, Huang WX, Hillert J: Cloning and mutation analysis of the human IL-18 promoter: a possible role of polymorphisms in expression regulation. J Neuroimmunol. 2001, 112: 146-152. 10.1016/S0165-5728(00)00407-0.
Tone M, Thompson SA, Tone Y, Fairchild PJ, Waldmann H: Regulation of IL-18 (IFN-gamma-inducing factor) gene expression. J Immunol. 1997, 159: 6156-6163.
Takeuchi M, Okura T, Mori T, Akita K, Ohta T, Ikeda M, Ikegami H, Kurimoto M: Intracellular production of interleukin-18 in human epithelial-like cell lines is enhanced by hyperosmotic stress in vitro. Cell Tissue Res. 1999, 297: 467-473. 10.1007/s004410051373.
Koyama N, Hoelzer D, Ottmann OG: Regulation of human IL-18 gene expression: interaction of PU.1 with GC-box binding protein is involved in human IL-18 expression in myeloid cells. Eur J Immunol. 2004, 34: 817-826. 10.1002/eji.200324420.
Sugiura T, Kawaguchi Y, Harigai M, Terajima-Ichida H, Kitamura Y, Furuya T, Ichikawa N, Kotake S, Tanaka M, Hara M, et al: Association between adult-onset Still's disease and interleukin-18 gene polymorphisms. Genes Immun. 2002, 3: 394-399. 10.1038/sj.gene.6363922.
Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, Kashiwazaki S, Tanimoto K, Matsumoto Y, Ota T, et al: Preliminary criteria for classification of adult Still's disease. J Rheumatol. 1992, 19: 424-430.
Arnett FC, Edworthy SM, Bloch DA: The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-324.
Tan EM, Cohen AS, Fries JF, Masi A, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ: The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982, 25: 1271-1277.
Subcommittee for Scleroderma Criteria of the American Rheumatism Association Diagnosis and Therapeutic Criteria Committee: Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum. 1980, 23: 581-590.
Bohan A, Peter JB: Polymyositis and dermatomyositis: parts 1 and 2. New Engl J Med. 1975, 292: 344-347.
Kuruse S, Kuehr J, Moseler M, Kopp MV, Kurz T, Deichmann KA, Foster PS, Mattes J: Polymorphisms in the IL18 gene are associated with specific sensitization to common allergens and allergic rhinitis. J Allergy Clin Immunol. 2003, 111: 117-122. 10.1067/mai.2003.43.
Ito T, Inoue E, Kamatani N: Association test algorithmbetween a qualitative phenotype and a haplotype or haplotype setusing simultaneous estimation of haplotype frequencies, diplotypeconfigurations and diplotype-based penetrances. Genetics. 2004, 168: 2339-2348. 10.1534/genetics.103.024653.
Novak N, Kruse S, Potreck J, Maintz L, Jenneck C, Weidinger S, Fimmers R, Bieber T: Single nucleotide polymorphisms of the IL18 gene are associated with atopic eczema. J Allergy Clin Immunol. 2005, 115: 828-833. 10.1016/j.jaci.2005.01.030.
Higa S, Hirano T, Mayumi M, Hirohata M, Ohshima Y, Nambu M, Yamaguchi E, Hizawa N, Kondo N, Matsui E: Association between interleukin-18 gene polymorphism 105A/C and asthma. Clin Exp Allergy. 2003, 33: 1097-1102. 10.1046/j.1365-2222.2003.01739.x.
Takada T, Suzuki E, Morohashi K, Geiyo F: Association of single nucleptide polymorphisms in the IL-18 gene with sarcoidosis in a Japanese population. Tissue Antigens. 2002, 60: 36-42. 10.1034/j.1399-0039.2002.600105.x.
Chen DY, Lan JL, Lin FJ, Hsieh TY, Wen MC: Predominance of Th1 cytokine in peripheral blood and pathological tissues of patients with active untreated adult onset Still's disease. Ann Rheum Dis. 2004, 63: 1300-1306. 10.1136/ard.2003.013680.
Kusaba M, Honda J, Fukuda T, Oizumi K: Analysis of type 1 and type 2 cells in synovial fluid and peripheral blood of patients with rheumatoid arthritis. J Rheumatol. 1998, 25: 1466-1471.
Scola MP, Thompson SD, Brunner HI, Tsoras MK, Witte D, Van Dijk D, Grom AA, Passo MH, Glass DN: Interferon-γ:interleukin-4 ratios and associated type 1 cytokine expression in juvenile rheumatoid arthritis synovial tissue. J Rheumatol. 2002, 29: 369-378.
Heinzmann A, Gerhold K, Ganter K, Kurz T, Schuchmann L, Keitzer R, Berner R, Deichmann KA: Association study of polymorphisms within interleukin-18 in juvenile idiopathic arthritis and bronchial asthma. Allergy. 2004, 59: 845-849. 10.1111/j.1398-9995.2004.00538.x.
Kretowski A, Mironczuk K, Karpinska A, Bojaryn U, Kinalski M, Puchalski Z, Kinalska I: Interleukin-18 promoter polymorphisms in type 1 diabetes. Diabetes. 2002, 51: 3347-3349.
Sivalingam SP, Yoon KH, Koh DR, Fong KY: Single-nucleotide polymorphisms of the interleukin-18 gene promoter region in rheumatoid arthritis patients: protective effect of AA genotype. Tissue Antigens. 2003, 62: 498-504. 10.1046/j.1399-0039.2003.00137.x.
Ray A, Cohn L: Th2 cells and GATA-3 in asthma: new insights into the regulation of airway inflammation. J Clin Invest. 1999, 104: 985-993.
Gu Y, Kuida K, Tsutui H, Ku G, Hsiao K, Fleming MA, et al: Activation of interferon-γ inducing factor mediated by interleukin-1β converting enzyme. Science. 1997, 275: 206-209. 10.1126/science.275.5297.206.
Tsutsui H, Kayagaki N, Kuida K, Nakano H, Hayashi N, Takeda K, Matsui K, Kashiwamura S, Hada T, Akira S: Caspase-1-independent, Fas/Fas ligand- mediated IL-18 secretion from macrophages causes acute liver injury in mice. Immunity. 1999, 11: 359-367. 10.1016/S1074-7613(00)80111-9.
Leung BP, McInnes IB, Esfandiari E, Wei XQ, Liew FY: Combined effects of IL-12 and IL-18 on the induction of collagen-induced arthritis. J Immunol. 2000, 15: 6965-6502.
Wei XQ, Leung BP, Arthur HM, McInnes IB, Liew FY: Reduced incidence and severity of collagen-induced arthritis in mice lacking IL-18. J Immunol. 2001, 166: 517-521.
Japanese Single Nucleotide polymorphisms Database. [http://snp.ims.u-tokyo.ac.jp/]
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
TS conceived the study and drafted the manuscript. NM was responsible for the recruitment and classification of patients, performed ELISA, and helped to draft the manuscript. Y Kawaguchi participated in the design and coordination of the study, and recruited a subset of the patients. ST conceived the study together with Y Kawano and participated in the design of the study. HI and HTI recruited a subset of patients. MH recruited a subset of patients and participated in coordination of the study. NK participated in the design and coordination of the study. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Sugiura, T., Maeno, N., Kawaguchi, Y. et al. A promoter haplotype of the interleukin-18gene is associated with juvenile idiopathic arthritis in the Japanese population. Arthritis Res Ther 8, R60 (2006). https://doi.org/10.1186/ar1930
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar1930