Abstract
Juvenile rheumatoid arthritis (JRA) comprises a group of chronic systemic inflammatory disorders that primarily affect joints and can cause long-term disability. JRA is likely to be a complex genetic trait, or a series of such traits, with both genetic and environmental factors contributing to the risk for developing the disease and to its progression. The HLA region on the short arm of chromosome 6 has been intensively evaluated for genetic contributors to JRA, and multiple associations, and more recently linkage, has been detected. Other genes involved in innate and acquired immunity also map to near the HLA cluster on 6p, and it is possible that variation within these genes also confers risk for developing JRA. We examined the TPSN gene, which encodes tapasin, an endoplasmic reticulum chaperone that is involved in antigen processing, to elucidate its involvement, if any, in JRA. We employed both a case–control approach and the transmission disequilibrium test, and found linkage and association between the TPSN allele (Arg260) and the systemic onset subtype of JRA. Two independent JRA cohorts were used, one recruited from the Rheumatology Clinic at Cincinnati Children's Hospital Medical Center (82 simplex families) and one collected by the British Paediatric Rheumatology Group in London, England (74 simplex families). The transmission disequilibrium test for these cohorts combined was statistically significant (χ2 = 4.2, one degree of freedom; P = 0.04). Linkage disequilibrium testing between the HLA alleles that are known to be associated with systemic onset JRA did not reveal linkage disequilibrium with the Arg260 allele, either in the Cincinnati systemic onset JRA cohort or in 113 Caucasian healthy individuals. These results suggest that there is a weak association between systemic onset JRA and the TPSN polymorphism, possibly due to linkage disequilibrium with an as yet unknown susceptibility allele in the centromeric part of chromosome 6.
Similar content being viewed by others
Introduction
Juvenile rheumatoid arthritis (JRA) is the most common chronic arthritic condition of childhood, encompassing pauciarticular, polyarticular, and systemic-onset disease subtypes. JRA is typically considered autoimmune in etiology, with characteristic T-cell abnormalities and chronic synovitis. The extent of synovitis may range from minimal to severe, and vary in terms of number of joints involved, with systemic onset disease typically associated with the greatest morbidity. JRA is probably a collection of diseases with complex overlapping etiologies, with each subtype influenced by multiple genetic susceptibility loci and mediated by environmental effects [1]. The MHC on the short arm of chromosome 6 has been intensively analyzed, and associations with both HLA and non-HLA genes have been reported. Genetic associations with MHC alleles have been documented primarily within the HLA class II region, but also with certain class I alleles. These associations are largely JRA subtype and age specific [2], and are strongest for pauciarticular and polyarticular disease [1]. For systemic onset JRA (SoJRA), associations with HLA-B8, HLA-Bw35 [3, 4] and HLA-DR4 [3, 5] have been observed, whereas HLA-DPB1*0401 was reported to have a protective effect in one Caucasian population [6]. Associations with HLA-DRB1*0401 and HLA-DRB1*0405 have been reported in a Japanese population [7]. Most of these associations have not been replicated.
In the present study we targeted the tapasin gene (TPSN), which is in the class II region of the MHC, 180 kilobases centromeric of HLA-DP. The tapasin protein is necessary for the proper assembly and peptide-presenting function of HLA class I molecules [8]. The TPSN gene has a polymorphism in exon 4 that results in a nonconservative amino acid substitution of Arg/Thr at amino acid 260 (ref SNP ID: rs2071888) [9, 10]. Three intronic polymorphisms of TPSN have also been described, none of which appear to be in linkage disequilibrium (LD) with HLA class I alleles or the extended HLA-A1, HLA-B8, HLA-DR3 haplotype, in at least one healthy Caucasian population [11]. Furthermore, using a large UK Caucasian sample, Ahmad and coworkers [12] recently reported that TPSN polymorphisms are not in LD with more telomeric MHC haplotypes. In the present study we report an association between the exon 4 TPSN polymorphism and susceptibility to SoJRA, involving the TPSN allele Arg260 (01 allele).
Methods
The study cohort included 88 SoJRA affected families recruited in Cincinnati (US cohort) and 74 simplex (with one affected offspring) SoJRA families identified by the British Paediatric Rheumatology Study Group (UK cohort). Unaffected siblings were available for analysis in the US but not in the UK cohort. An additional 113 healthy unrelated control individuals, primarily Caucasians from the Midwest and New England, resembled the SoJRA-affected families in terms ethnicity and served as the control population. Ethics approvals were obtained from the participating institutions, and informed consent was obtained from parents and/or children.
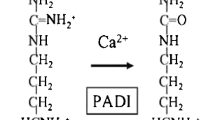
All affected children met American College of Rheumatology criteria for a diagnosis of JRA; they were subgrouped as pauciarticular, polyarticular, or SoJRA. Genomic DNA was purified from peripheral blood cells by standard techniques and analyzed for TPSN alleles (Arg260/01 and Thr260/02) by polymerase chain reaction and restriction site enzyme digestion. Briefly, a 298-base-pair fragment of exon 4 of the TPSN gene containing the polymorphism was amplified and then digested with BfaI, which recognizes the 01 allele, and SfcI, which recognizes the 02 allele. The primers used were Tsn 479 forward (5'-CCC ACC CTC TAC CCC TGG A-3') and Tsn 641 reverse (5'-CAG CAC CTG GGT AAG GGA CA-3'). HLA types were determined for a subgroup of the participants using DNA-based low-resolution methodology (Geno-Vision Inc., Exton, PA, USA), and serologically using standard typing sera and microcytotoxicity assays.
Preliminary association analysis was conducted by χ2 testing on contingency tables comparing the three genotypic frequencies between cases and control individuals to yield a χ2 with two degrees of freedom. Family-based association analysis was performed using the transmission disequilibrium test (TDT). The TDT [13, 14] is a family-based association test that compares within a cohort the number of times a particular parental allele is transmitted to an affected offspring versus the number of times it is not transmitted. To allow inclusion of families with missing data for a single parent, the Transmit program http://www-gene.cimr.cam.ac.uk/clayton/software/[15], which uses population allele frequencies to weight the possible parental genotypes, was used for the TDT analysis. In the Transmit program, genotypes of unaffected siblings (or siblings whose disease status is unknown) are used to infer parental genotypes, thus increasing the power to detect association. We applied this test first to the combined US and the UK data and then to each set separately. The significance level of the combined results was also calculated using Fisher's method of combining P values for two independent analyses that test the same hypothesis. LD between TPSN and the HLA region (limited to the Cincinnati cohort) was evaluated using the EH program http://linkage.rockefeller.edu/ott/eh.htm[16, 17]. The Geno-Pdt test in the PdT 5.1 program http://wwwchg.duhs.duke.edu/software/pdt.html was also used as a test for association and linkage in the US SoJRA-affected families [18–20].
Results
The distribution of tapasin genotypes among SoJRA-affected children was compared with that in their healthy siblings, as well as with that in unrelated healthy control individuals using a two degrees of freedom χ2 test in the US cohort (Table 1). The differences did not reach statistical significance. The allelic frequencies of tapasin in the independent cohorts from the USA (Table 1) were in Hardy–Weinberg equilibrium (healthy individuals from the USA: χ2 = 0.3049, P = 0.58; SoJRA-affected individuals from the USA: χ2 = 2.004, P = 0.156). In the UK data only SoJRA-affected individuals were available for Hardy–Weinberg equilibrium testing, and the result was borderline (χ2 = 5.26, P = 0.02).
We then tested for evidence of linkage of TPSN to JRA by applying the family-based TDT only to the cohorts of affected individuals for whom parental and sibling information was available. These families included 82 US SoJRA familes (389 individuals, including family members) and 74 UK SoJRA families. The TDT test, as implemented in the Transmit program, detected the preferential transmission of the TPSN 01 allele in the UK and US SoJRA families (n = 156; χ2 = 4.2, 1 degree of freedom [df]; P = 0.04; Table 2). When the US SoJRA cohort was analyzed alone, this preferential transmission for the TPSN allele 01 was even more significant (χ2 = 6.0, 1 df; P = 0.01; Table 2).
However, SoJRA families from the UK alone as a subgroup failed to show significant preference for TPSN allele 01 transmission (χ2 = 0.075, 1 df; P = 0.78; Table 2). When the SoJRA UK cohort was analyzed, it was recognized that information for one of the parents was missing in 22 families (29.7% of the total). There was no information from unaffected siblings of the probands for these UK families, which is necessary for the Transmit program to narrow down the range of the possible parental genotypes. When one parent is missing, the Transmit program assigns and weights possible haplotypes to the missing parent using the information from the known parent and the siblings of the proband, and averages the probability of all transmissions to the proband. Because there were no data regarding the genotypes of unaffected siblings for the UK families, the Transmit program was unable to infer parental genotypes and thus had less power to detect the preferential transmission of the 260Arg allele. In the US SoJRA-affected cohort parental information was missing for 32 of the 82 families (39%), but for 12 of these (14.6%) there was information regarding unaffected siblings. Although 24.4% of the cohort was unavailable for TDT calculation, 62 families (75.6%) were available.
We combined the two P values using Fisher's method [21] to obtain a χ2 with four degrees of freedom and found the combination of the two analyses to be significant (χ2 = 9.7, 4 df; P = 0.05). Overall, when the two cohorts were analyzed together the tapasin 260Arg allele was transmitted more often than the 260Thr allele, suggesting association and linkage between the TPSN polymorphism and SoJRA. In order to include information from the unaffected siblings for association testing, we also applied an alternative association test to the US SoJRA population – the pedigree disequilibrium test (PDT) [18, 19]. A new version of PDT, the genotype-based association test for pedigrees (Genotype-PDT), was applied to the data. Genotype-PDT [20] tests for linkage and underlying patterns of association at the genotypic level. It is more conservative and has lesser type 1 error when compared with the TDT test implemented in the Transmit program. Genotype-PDT also uses information from affected individuals, unaffected siblings, and their nuclear families. Therefore, we were only able to apply this test to the US SoJRA cohort. The genotype-PDT test revealed association and linkage of the tapasin 260Arg allele with SoJRA at the genotypic level (χ2 = 6.727, 1 df; P = 0.034) in the US SoJRA cohort.
Furthermore, we wished to control for possible transmission distortion of tapasin 260Arg allele in SoJRA-affected families. This allele could also be preferentially transmitted to the unaffected siblings of the SoJRA-affected individuals from their parents, and our statistical significance could be falsely inflated because of allele-specific segregation bias (altered transmission of an allele independent of its role in disease). We therefore applied the TDT test to the unaffected siblings from the US SoJRA cohort. In contrast to the affected siblings, there was no significant preference toward 260Arg allele transmission to healthy siblings, suggesting no segregation bias (χ2 = 1.043, 1 df; P = 0.3; Table 2). These data provide evidence of a genotypic association and linkage between the TPSN 260Arg allele and susceptibility to SoJRA.
Discussion
Although JRA is the most common rheumatologic disease in childhood, the SoJRA subtype comprises less then 20% of cases and is a rare disease. In the past, because of the small sample sizes, studies conducted by single centers failed to establish strong genetic associations. The present study was therefore done with collaboration between two different centers. These two centers recruited mainly Caucasian families with one SoJRA-affected offspring. An association of the TPSN allele 260Arg with SoJRA was detected when both cohorts were analyzed and in the US cohort by itself. In the UK cohort the statistical analysis did not reveal a significant association. This discrepancy may be due to the limited sample size for the UK data, the different ethnic backgrounds of the two cohorts, and/or gene–environment interactions.
In general, it is suggested that studies using independent controls are more powerful than those using related (family-based) controls, but they may be biased if cases and controls have different ethnic backgrounds because of population stratification. Family-based control studies are less powerful because of overmatching, but they are robust to population stratification. In the present study we used family-based control association tests, which allowed us to analyze SoJRA family cohorts recruited by two different centers (US and UK).
Statistical programs designed to test genetic linkage based on TDTs (i.e. linkage in the presence of association) calculate the transmission of alleles from heterozygous parents to affected individuals. In the absence of one parent, the family becomes uninformative regarding single nucleotide polymorphisms and cannot be included in the analysis. This decreases the sample size, thus reducing the power to detect association or genetic linkage in rare diseases. Recently, programs such as Transmit and PDT have become available that are designed to calculate the possible genotypes of the missing parent from unaffected children or other family members such as grandparents. However, in cohorts consisting of simplex families (mother, father and the affected child), which do not have unaffected siblings or grandparents, and when there are families with missing parents, these programs are unable to achieve as much power to detect genetic association. The TDT test in the Transmit program was unable to infer the missing parental information (22 families, 29% of the data) from the UK cohort, which decreased the sample size to 52 families (71% of the cohort). In contrast, in the US SoJRA cohort the presence of unaffected siblings made 62 families (75.6% of the cohort) available for testing and increased the power to detect linkage in the presence of association.
In order to detect whether the group of children with earlier age at onset of SoJRA (<6 years at onset) is in association with TPSN allele 260Arg, both cohorts were dichotomized by age at disease onset and analyzed using the Transmit program. TPSN allele 260Arg was still preferentially transmitted in both of the age onset groups but there was no statistical significance at the 5% level. When the age at onset groups <6 years and ≥6 years were pooled together from US and UK cohorts and analyzed, there was still no statistically significant association with TPSN allele 260Arg.
The other possible reason for the lack of significant linkage in the UK cohort when analyzed alone might be ethnic difference, with a different polymorphism associated with SoJRA and a different disease frequency. Although both cohorts consisted of Caucasians, there might still have been ethnic differences between them. Therefore, it could be that the association of TPSN allele 260Arg with SoJRA in the US population is due to LD, with different SoJRA susceptibility alleles located on chromosome 6 being due to differing recombination processes between the US and UK Caucasian populations.
Because weak associations between SoJRA and HLA-DR alleles [5–7] have previously been noted, we compared the available class II allele frequencies, including HLA-DR, HLA-DP and HLA-DQ, in SoJRA patients from the US cohort (n = 69) with healthy control individuals (n = 66). No statistically significant differences were found (data not shown). However, it is worth noting that we detected a small trend toward a lower HLA-DPB*0401 frequency in SoJRA patients (28%) as compared with healthy control individuals (35%), which is consistent with a previous report [6] that suggested a possible protective role for this particular HLA allele in SoJRA. Furthermore, we applied a test for LD (using the EH program) to assess LD between TPSN alleles and the HLA alleles in SoJRA patients. We included 34 SoJRA-affected children from the US cohort and 38 healthy individuals for whom HLA typing data were available. There was no evidence for LD between the TPSN and any of the HLA alleles with the SoJRA-affected individuals or the healthy individuals. Because HLA typing was not available for all patients in the US and UK SoJRA patient groups, these calculations were done using very small sample sizes, and so the possibility of LD between the TPSN and HLA loci in these groups cannot be completely eliminated.
The landmark cytokines that contribute directly to the clinical features or autoimmune process of SoJRA, namely IL-6, tumor necrosis factor (TNF)-α, and IL-1, are also known to be important regulators of apoptosis. SoJRA's characteristic clinical and laboratory features, such as fever, skin rash, hypergammaglobulinemia, hypoalbuminemia, elevated erythrocyte sedimentation rate, and fibrinogen levels, may all be explained by cytokine-activated inflammatory and/or immune responses. Elevated blood level of IL-6 in SoJRA is known to correlate with fever episodes [22, 23]. Some of these cytokines were evaluated for their associations with SoJRA. The non-MHC cytokine gene polymorphisms that have been associated with SoJRA are the IL-6 5' flanking polymorphism [24], the TNF-α 5' flanking polymorphism [25], and the macrophage migration inhibition factor polymorphism [26]. Recent cytotoxicity studies also implicate natural killer cell dysfunction in this process [27].
Functional differences between the tapasin proteins encoded by the two alleles (Arg versus Thr at 260) have not, to our knowledge, been described. Given what is known about the function of tapasin, it is conceivable that polymorphisms might affect the quality or quantity of peptides presented by class I molecules, thereby influencing the immune response. It is also worth noting that the TPSN gene is separated from Daxx, an effector of Fas ligand and transforming growth factor-β mediated apoptosis [28, 29] by only a single gene (BING2). Apoptosis plays a key role in regulating the immune response in part by balancing excess cellular proliferation, and several of the key cytokines that have been implicated in the pathogenesis of SoJRA, such as TNF-β, IL-6, and IL-1, are known to influence apoptotic pathways. Thus, it is perhaps more tempting to speculate that the TPSN 01 polymorphism (TPSN 260Arg) associated with SoJRA might be in LD with another susceptibility allele in a gene such as Daxx (or other genes in the region that play roles in apoptosis). Furthermore, the TPSN 260Arg allele might be part of a haplotype in the HLA region that contributes to susceptibility to SoJRA. It will be important to examine additional SoJRA populations to determine whether TPSN is associated with disease. If so then further genetic studies of this region, including LD testing and exploration of candidate gene alleles in the region, may be of considerable interest.
Conclusion
In conclusion, our studies support the existence of a weak association, possibly due to a linked gene in the region, between the TPSN 01 allele and susceptibility to SoJRA.
Abbreviations
- df:
-
degrees of freedom
- IL:
-
interleukin
- JRA:
-
juvenile rheumatoid arthritis
- LD:
-
linkage disequilibrium
- MHC:
-
major histocompatibility complex
- PDT:
-
pedigree disequilibrium test
- SoJRA:
-
systemic onset juvenile rheumatoid arthritis
- TDT:
-
transmission disequilibrium test
- TNF:
-
tumor necrosis factor.
References
Glass DN, Giannini EH: Juvenile rheumatoid arthritis as a complex genetic trait. Arthritis Rheum. 1999, 42: 2261-2268. 10.1002/1529-0131(199911)42:11<2261::AID-ANR1>3.0.CO;2-P.
Murray K, Moroldo MB, Donnelly P, Prahalad S, Passo MH, Giannini EH, Glass DN: Age-specific effects of juvenile rheumatoid arthritis-associated HLA alleles. Arthritis Rheum. 1999, 42: 1843-1853. 10.1002/1529-0131(199909)42:9<1843::AID-ANR8>3.0.CO;2-M.
Miller ML, Aaron S, Jackson J, Frazer P, Cairns L, Hoch S, Borel Y, Larson M, Glass DN: HLA gene frequencies in children and adults with systemic onset juvenile rheumatoid arthritis. Arthritis Rheum. 1985, 28: 146-150.
Glass DN, Litvin DA: Heterogeneity of HLA associations in systemic onset juvenile onset rheumatoid arthritis. Arthritis Rheum. 1980, 23: 796-799.
Bedford PA, Ansell BM, Hall PJ, Woo P: Increased frequency of DR4 in systemic onset juvenile chronic arthritis. Clin Exp Rheumatol. 1992, 10: 189-193.
Paul C, Yao Z, Nevinny-Stickel C, Keller E, Schoenwald U, Truckenbrodth H, Hoza J, Suschke J, Albert ED: Immunogenetics of juvenile rheumatoid arthritis. Immunity. 1995, 45: 280-283.
Date Y, Seki N, Higuchi T, Hirata T, Miyata K, Ohkuni M, Tatsuzawa O, Kimura A, Itoh K, Kato H: Identification of a genetic risk factor for systemic juvenile rheumatoid arthritis in the 5'-flanking region of the TNF-α genes and HLA genes. Arthritis Rheum. 1999, 42: 2577-2582. 10.1002/1529-0131(199912)42:12<2577::AID-ANR10>3.0.CO;2-O.
Pamer E, Cresswell P: Mechanisms of MHC class I-restricted antigen processing. Annu Rev Immunol. 1998, 16: 323-358. 10.1146/annurev.immunol.16.1.323.
Herberg JA, Sgouros J, Jones T, Copeman J, Humphray SJ, Sheer D, Cresswell P, Beck S, Trowsdale J: Genomic analysis of the tapasin gene, located close to TAP loci in the MHC. Eur J Immunol. 1998, 28: 459-467. 10.1002/(SICI)1521-4141(199802)28:02<459::AID-IMMU459>3.3.CO;2-Q.
Herberg JA, Beck S: Tapasin, DAXX, RGL2, HKE2, and four new genes (BING 1, 3 to 5) form a dense cluster at the centromeric end of the MHC. J Mol Biol. 1998, 277: 839-857. 10.1006/jmbi.1998.1637.
Williams AP, Bevan S, Bunce M, Houlston R, Welsh KI, Elliott T: Identification of novel Tapasin polymorphisms and linkage disequilibrium to MHC class I alleles. Immunogenetics. 2000, 52: 9-11. 10.1007/s002510000244.
Ahmad T, Neville M, Marshall SE, Armuzzi A, Mulcahy-Hawes K, Walton R, Bunce M, Jewell DP, Welsh KI: Haplotype specific linkage disequilibrium patterns define the genetic topography of the human MHC. Hum Mol Genet. 2003, 12: 647-656. 10.1093/hmg/12.6.647.
Spielman RS, Ewens WJ: The TDT and other family-based tests for linkage disequilibrium and association. Am J Hum Genet. 1996, 59: 983-989.
Spielman RS, McGinnis RE, Ewens WJ: Transmission test for linkage disequilibrium: the insulin gene region and insulin-dependent diabetes mellitus (IDDM). Am J Hum Genet. 1993, 52: 506-516.
Clayton D: A generalization of the transmission/disequilibrium test for uncertain haplotype transmission. Am J Hum Genet. 1999, 65: 1170-1177. 10.1086/302577.
Xie X, Ott J: Testing linkage disequilibrium between a disease gene and marker loci. Am J Hum Genet. 1993, 53: 1107-
Ott J: Statistical properties of the haplotype relative risk. Genet Epidemiol. 1989, 6: 127-130.
Martin ER, Monks SA, Warren LL, Kaplan NL: A test for linkage and association in general pedigrees: the pedigree disequilibrium test. Am J Hum Genet. 2000, 67: 146-154. 10.1086/302957.
Martin ER, Bass MP, Hauser ER, Kaplan NL: Accounting for linkage in family-based tests of association with missing parental genotypes. Am J Hum Genet. 2003, 73: 1016-1026. 10.1086/378779.
Martin ER, Bass MP, Gilbert JR, Pericak-Vance MA, Hauser ER: Genotype-based association test for general pedigrees: the genotype-PDT. Genet Epidemiol. 2003, 25: 203-213. 10.1002/gepi.10258.
Fisher R: Statistical Methods and Scientific Interference. 1973, New York: Macmillan, 3rd
Rooney M, David J, Symons J, Di Giovine F, Varsani H, Woo P: Inflammatory cytokine responses in juvenile chronic arthritis. Br J Rheumatol. 1995, 34: 454-460.
Prieur AM, Roux-Lombard P, Dayer JM: Dynamics of fever and cytokine network in systemic onset juvenile rheumatoid arthritis. Rev Rhum Engl Ed. 1996, 63: 163-170.
Fishman D, Faulds G, Jeffery R, Mohamed-Ali V, Yudkin JS, Humpries S, Woo P: The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J Clin Invest. 1998, 102: 1369-1376.
Date Y, Seki N, Kamizono S, Higuchi T, Hirata T, Miyata K, Ohkuni M, Tatsuzawa O, Yokota S, Joo K, et al: Identification of a genetic risk factor for systemic juvenile rheumatoid arthritis in the 5'-flanking region of the TNFα gene and HLA genes. Arthritis Rheum. 1999, 42: 2577-2582. 10.1002/1529-0131(199912)42:12<2577::AID-ANR10>3.0.CO;2-O.
Donn RP, Barrett J, Farhan A, Stopford A, Pepper L, Shelley E, Davies N, Ollier WER, Thompson W, at BPS Group: Cytokine gene polymorphisms and susceptibility to juvenile idiopathic arthritis. Arthritis Rheum. 2001, 44: 802-810. 10.1002/1529-0131(200104)44:4<802::AID-ANR136>3.0.CO;2-G.
Grom AA, Villanueva J, Lee S, Goldmuntz EA, Passo M, Filipovich A: Natural killer cell dysfunction in patients with systemic-onset juvenile rheumatoid arthritis and macrophage activation syndrome. J Pediatr. 2003, 142: 292-296. 10.1067/mpd.2003.110.
Yang X, Krhosrsravi-Far R, Chang HY, Baltimore D: DAXX, a novel Fas-binding protein that activates JNK and apoptosis. Cell. 1997, 89: 1067-1076. 10.1016/S0092-8674(00)80294-9.
Perlman R, Schiemann WP, Brooks WW, Lodish HF, Weinberg RA: TGF-beta induced apoptosis is mediated by the adapter protein DAXX that facilitates JNK activation. Nat Cell Biol. 2001, 3: 708-714. 10.1038/35087019.
Acknowledgements
We acknowledge the British Paediatric Rheumatology Study Group for their contributions to this study. Hulya Bukulmez, MD, is supported in part by NRSA/NHLBI, T32HL07567 and NRSA, NIAMS, T32AR07594. Jane Olson is supported in part by USPHS grants HG01577 from the NCHGR and RR03655 from the NCRR. Robert Elston is supported in part by grants GM28356 from NIGMS and RR 03655 from NCRR. Monica Tsoras, Susan Thompson, David Glass and Robert Colbert are supported by NIH/NIAMS N01AR42218, P60AR47784, P30AR47363, and AR41677. The work conducted in the UK was funded by the Arthritis Research Campaign (AR47363-02).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
HB carried out the molecular genetic study in US, genotyped the US cohort, did the statistical analysis of both US and UK cohorts, and drafted the manuscript. MF carried out the molecular study in UK and participated in drafting the manuscript. MT confirmed the genotypes of US SoJRA patients. SDT participated in the coordination of the study and drafting the manuscript. NAT genotyped the UK SoJRA cohort. PW coordinated the UK study and participated in drafting the manuscript for the UK cohort.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Bukulmez, H., Fife, M., Tsoras, M. et al. Tapasin gene polymorphism in systemic onset juvenile rheumatoid arthritis: a family-based case–control study. Arthritis Res Ther 7, R285 (2005). https://doi.org/10.1186/ar1480
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar1480