Abstract
Synovial tissue is readily accessible by closed needle or arthroscopic biopsy. These techniques provide adequate tissue for most diagnostic requirements. Examination of synovial tissue can assist in the diagnosis of some joint infections, and in several atypical or rare synovial disorders. Histological confirmation is not normally required for diagnosis of the common forms of inflammatory arthritis, including rheumatoid arthritis (RA). In patients with either established or early RA, immunohistological measures of inflammation in synovial tissue are associated with clinical measures of disease activity, may predict the clinical outcome, and change in response to treatment. Surrogate markers of disease activity and outcome that have been identified in synovial tissue include components of the cellular infiltrate, and several mediators of inflammation and matrix degradation. There is evidence that the very early introduction of disease-modifying therapy inhibits progressive structural damage maximally. Clinicians exploiting this 'window of opportunity' therefore require very early indicators of the diagnosis and outcome in patients who present with an undifferentiated inflammatory arthritis. Some immunohistological features have been described that distinguish patients who are likely to develop progressive RA and who might benefit most from early aggressive therapeutic intervention. In this regard, the inclusion of pharmacogenomic and proteomic techniques in the analysis of synovial tissue presents some exciting possibilities for future research.
Similar content being viewed by others
History of synovial biopsy in the diagnosis of arthritis
Early histopathological studies of rheumatoid arthritis (RA) were based on tissue samples obtained at surgery or at postmortem examination. In 1932 a technique for obtaining non-surgical synovial tissue for diagnostic purposes, using a dental nerve extractor that was introduced into the joint through a large-calibre needle, was first proposed [1]. The introduction of this technique to clinical practice was never described. About 20 years later, early experiences with needle biopsy of the synovium were published [2, 3]. It was suggested that the procedure was safe and practical for use in both hospital wards and outpatient clinics. However, because of their wide bore and the need for an incision, these prototype biopsy needles tended to cause significant trauma to the penetrated tissues. In 1963, Parker and Pearson described a simplified 14-gauge needle that did not require a skin incision [4]. They published their experience of 125 procedures, almost all from the suprapatellar pouch of the knee joint, with a very high yield of adequate tissue for analysis. No serious complications were encountered. For about 30 years, the Parker–Pearson needle, or a modification of it [5, 6], remained the instrument of choice when acquiring synovial tissue for diagnostic or research purposes.
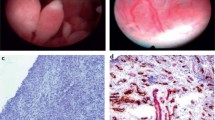
Arthroscopic techniques, which enable the selection of synovial tissue under direct vision, were also developed primarily to assist in the diagnosis of arthritis [7]. Early studies by rheumatologists suggested a lack of association between the arthroscopic findings and clinical, laboratory and radiological features of arthritis [8, 9]. More recently there has been an upsurge in the use of arthroscopic techniques by rheumatologists, particularly those interested in the pathogenesis of arthritis and the effects of new therapeutic strategies [10]. Initially, arthroscopy required hospitalisation and a general anaesthetic. The production of high-definition, small-bore arthroscopes (1–2.7 mm), and the development of local and regional anaesthesia protocols [11, 12], have permitted day-case arthroscopy to move from the operating theatre to procedure rooms, and even to the outpatient clinic [13].
Synovial biopsy in routine clinical practice
Synovial biopsy is not normally required for routine diagnostic or therapeutic purposes in patients with established arthritis. However, examination of synovial tissue can assist in the diagnosis of some joint infections [14]. In acute bacterial arthritis, the synovial membrane contains clusters or sheets of polymorphonuclear leukocytes. Bacteria can be demonstrated in synovial tissue by Gram's stain. Sometimes, cultures of synovial tissue may be positive even when blood and synovial fluid cultures have been negative. In chronic infections, such as tuberculosis and fungal diseases, characteristic synovial lesions may be focal, and multiple biopsies are advised. Mycobacterial granulomas in the synovium do not always demonstrate caseation. With appropriate staining, acid-fast organisms, fungi and spirochetes (Lyme disease and secondary syphilis) can be demonstrated. The presence of bacterial DNA in synovial biopsy samples can provide important information in the diagnosis of infectious arthritis [15].
Occasionally, the diagnosis of chronic sarcoidosis is established after synovial biopsy [16]. The characteristic histological feature is a well-defined granuloma. The central area of the granuloma is occupied by lymphocytes, which are predominantly CD4+, and by mononuclear phagocytes and their progeny, including epithelioid cells and multinucleated giant cells. Caseation is absent, but a small area of fibrinoid necrosis may be present. The outer zone of the granuloma is formed by CD4+ and CD8+ lymphocytes, fibroblasts, mast cells and other immunoregulatory cells.
Both gout and pseudogout can demonstrate tophus-like deposits in synovial tissue [14]. When handling tissues, special care is required to preserve the crystalline structures. Amyloid may be deposited in synovium in patients with primary amyloidosis, Waldenstrom's macroglobulinemin, multiple myeloma and adult cystic fibrosis [17]. Arthropathy associated with ochronosis and haemachromatosis demonstrate characteristic histological features. Pigmented villonodular synovitis, multicentric reticulohistiocytosis and rare tumours of the synovial membrane require a biopsy for diagnosis.
Synovial biopsy can have a major role in the diagnosis of monarticular arthritis. A closed needle biopsy of the knee joint might provide sufficient tissue for histological, immunohistological and microbiological analysis. An open biopsy or needle arthroscopic biopsy is the procedure of choice when other joints are involved, and should be undertaken in the knee joint if closed needle biopsy fails to yield a diagnosis.
Synovial biopsy in rheumatoid arthritis
Established rheumatoid arthritis
General comments
The diagnosis of RA after the chronic polyarticular manifestations have become established is usually based on characteristic clinical, radiological and serological manifestations. Histological confirmation is not required. The gross changes that are characteristic of RA result from chronic synovial inflammation. Typically, the surface of the synovium becomes hypertrophic and oedematous, with an intricate system of prominent villous fronds that extend into the joint cavity. Microscopic evaluation of synovial tissue inflammation in RA confirms marked cellular hyperplasia in the lining layer. T cells, plasma cells, macrophages, B cells, neutrophils, mast cells, natural killer cells and dendritic cells accumulate in the synovial sublining layer (reviewed in [18]). The appearances are not specific for RA. The dominant cell populations in the lining layer are fibroblast-like synoviocytes and macrophages, which release an array of proinflammatory cytokines and their inhibitors, promoting further intra-articular perturbations. There is abundant production of matrix metalloproteinases (MMPs), cysteine proteases and other tissue-degrading mediators, which accumulate in the synovial fluid and augment joint damage by interacting directly with exposed cartilage matrix. These features are present very early in the disease course. T cells and plasma cells are prominent in the synovial sublining layer. Perivascular T cell aggregates are observed in 50–60% of patients with RA. These aggregates can be surrounded by plasma cells. There are two basic patterns of T cell infiltration. First, perivascular lymphocyte aggregates can be found, which consist predominantly of CD4+ cells in association with B cells, few CD8+ cells, and dendritic cells. The second pattern of T cell infiltration is the diffuse infiltrate of T cells scattered throughout the synovium. A subset of the CD4+ T cells in synovial tissue is activated. A possible biological effect of activated perivascular T cells in the synovium is the stimulation of migrating macrophage populations through direct cell contact. This mechanism is known to stimulate macrophage production of cytokines and MMPs in vitro. Many of the synovial tissue T cells are, however, in a state of hyporesponsiveness. Interdigitating dendritic cells, which are potent antigen-presenting cells, are located in proximity to CD4+ T cells in the lymphocyte aggregates and near the intimal lining layer. In addition, macrophages and lymphocytes infiltrate the areas between the lymphocyte aggregates. The macrophages often constitute the majority of inflammatory cells in the synovial sublining layer. B cells constitute a small proportion of the total number of lymphocytes in the synovial sublining layer. However, numerous plasma cells may be present throughout the synovium, sometimes exceeding the number of infiltrating T cells.
An issue that frequently arises in the context of possible associations between synovial tissue immunohistology and progressive structural damage relates to the acquisition of tissue samples from a knee joint and the evaluation of radiographic images, usually of the hands and feet. Such studies make the assumption that the immunohistological appearances in a knee joint are representative of pathophysiological events occurring at other sites. Evidence to support this hypothesis comes from a study of patients with RA who underwent biopsy of a knee joint and a small upper-limb joint on the same day [19]. Another important issue that requires consideration is the question of selection bias. This issue has been evaluated extensively, confirming that despite the degree of histological variation within a joint, representative measures of inflammation can be obtained by examining a limited area of tissue [20–23].
The intensity of the cellular infiltrate, the levels of activation and the amount of secreted products vary greatly between individual patients with RA and other arthropathies [20, 24, 25]. Many studies of synovial tissue have been reported that indicate associations between immunohistological features of inflammation and clinical measures of disease activity [20, 26, 27], as well as with local measures of synovitis [28]. The immunohistological measures of synovitis observed in the knee joint are reflected in other joints from the same patient biopsied at the same time [19]. Clinically uninvolved joints in patients with RA demonstrate similar immunohistological changes, although less intensely than in the affected joints [29, 30]. Serial synovial biopsies in open therapeutic studies and in randomised clinical trials showed that the immunohistological features of RA and other arthropathies change after treatment with disease-modifying anti-rheumatic drugs (DMARDs) [26, 31–37], oral corticosteroids [38] and targeted biological agents [39–42]. The mediators of inflammation that have been shown to change in therapeutic studies include mononuclear cell populations [26, 31, 32, 35, 36, 39, 40, 42], adhesion molecule expression [35, 36, 38–40, 42], levels of cytokine production [31, 33, 35, 36, 41] and MMPs [34, 36, 37]. Thus, synovial tissue analysis in patients with RA has revealed several surrogate markers of disease activity and response to treatment.
The value of synovial biopsy
In contrast to the studies of disease status and response to treatment in patients with established arthritis, limited attention has been given to the study of the immunohistological appearances and associations with disease outcome. One cross-sectional analysis demonstrated significant correlations between the number of lining layer and sublining layer macrophages, but not other mononuclear cell populations, and joint damage scores in RA [27]. A longitudinal study highlighted the association between the number of synovial tissue macrophages at baseline and increases in the joint damage scores over 1 year [43]. Other investigators showed that the predominant change in the synovial tissue of patients in remission after treatment with DMARDs was a striking decrease in the number of macrophages [44]. These observations are consistent with the hypothesis that chronic RA is a macrophage-mediated disorder and that a decrease in synovial macrophage content should be a primary aim of successful treatment.
Preliminary studies have evaluated possible associations between the known mediators of inflammation in synovial tissue, including cytokines, and outcome in established RA (Table 1). The effect of blockade of tumour necrosis factor-α (TNF-α) on TNF-α production in synovial tissue was evaluated in patients treated with infliximab [41]. All patients in the study met the American College of Rheumatology 20% improvement response criteria (ACR20), and half of the patients met the ACR50. Patients meeting the ACR50 criteria were those with the highest baseline levels of TNF-α synthesis. There was a significant correlation between baseline levels of TNF-α expression and change in tissue TNF-α levels in response to therapy. The authors concluded that high levels of synovial tissue TNF-α production before treatment might predict responsiveness to anti-TNF-α therapy.
Interleukin-10 (IL-10) is a chondroprotective cytokine and functions in part by inhibiting the production of TNF-α, IL-1 and MMPs (reviewed in [45]). Treatment of experimental models of arthritis with recombinant IL-10 inhibited both the incidence and the severity of disease. In a cross-sectional biopsy study, IL-10 mRNA levels were measured in synovial tissue from patients with erosive RA and compared with those in patients with chronic non-erosive arthritis [46]. The patients with erosive RA were positive for IgM-rheumatoid factor (IgM-RF+) and had a mean disease duration of 16.8 years. The patients with non-erosive arthritis had a mean disease duration of 7 years, and most were seronegative. Synovial tissue IL-10 mRNA levels were significantly lower in the patients with erosive RA (P < 0.03). This observation from a cross-sectional analysis of patients with established RA was extended in a longitudinal study of IL-10 polymorphisms in 291 consecutive patients with early RA. During the first 6 years of follow-up, the increase in radiographic damage scores in the patients who were homozygous for the genotype -1082AA was significantly less than the increase in patients with the genotype -1082GG. The smaller number of erosions in patients with RA who had the -1082AA genotype could not be explained by other determinants of progressive joint damage, such as an increased concentration of IgM-RF, the presence of the shared epitope, or the baseline radiographic damage score. Taken together, these observations suggested that increased expression of IL-10 mRNA in synovial tissue might be required for protection against progressive erosive disease, and that patients with RA who have different IL-10 genotypes have a different disease course. Future research is necessary to confirm whether or not there is a baseline threshold of tissue IL-10 mRNA expression that will identify individual patients with early RA who are more likely to demonstrate an aggressive disease course.
Synovial angiogenesis, a mechanism that is central to synovial proliferation and pannus formation, is largely dependent on vascular endothelial growth factor (VEGF) [47]. In a small study of patients with RA, synovial tissue samples were evaluated for the presence of VEGF at the time of joint replacement surgery and, on average, 10 years later [48]. An association between the amount of VEGF production in endothelial cells and the rate of progressive joint damage was suggested. Further studies of proinflammatory cytokines, tissue-degrading enzymes, angiogenic factors and other mediators of inflammation and damage in the synovium, at the level of either gene expression or protein production, might reveal characteristics associated with a favourable or unfavourable outcome.
Early rheumatoid arthritis
General comments
The approach to treating patients with early RA has changed substantially in recent years. In most centres, early arthritis refers to patients who present within 1 year of the onset of symptoms. This change has occurred for several reasons. First, there has been a growing recognition that irreversible structural damage can occur very early in the course of inflammatory arthritis [49]. Second, the establishment of dedicated early arthritis clinics facilitates the early referral of patients with inflammatory arthritis [50]. Third, there is a wider recognition of reliable diagnostic factors [51]. Fourth, rheumatologists have access to effective therapeutic modalities that greatly reduce the rate of progressive joint damage [52–54]. Last, it has been established that DMARD therapy reduces the rate of progressive joint damage more effectively when introduced within 6 months of the onset of symptoms [55]. It is therefore now standard practice to introduce conventional DMARDs, such as methotrexate, and even targeted biological therapies, as first-line treatments in patients with RA [56].
The presence of some autoantibodies, including IgM-RF and anti-citrulline-containing peptide (anti-CCP) antibody, facilitates an early diagnosis of RA [57]. In addition, several clinical and laboratory factors at baseline reliably predict outcome. These include higher baseline joint counts, a high titre of IgM-RF, an elevated acute-phase response, the number of baseline erosions and the shared epitope [58]. However, these factors were identified in large cohorts and do not always apply to individual patients. Some clinical investigators have developed algorithms that incorporate selected prognostic factors to predict outcome [59, 60].
The value of synovial biopsy
Studies of synovial tissue to identify indicators of outcome in RA, and changes after treatment, have been necessarily limited in size in comparison with similar studies that evaluated clinical and serum factors. Synovial biopsy is an invasive procedure and, when performed at arthroscopy, is technically complicated and expensive. Quantification of changes with digital image analysis is also costly and requires considerable expertise. However, the pathophysiological events occurring in tissue are more likely than dispersed serum factors to reflect the clinical status and outcome in individual patients.
Although there is no diagnostic role in early RA, synovial biopsy and tissue analysis may provide important prognostic information. A few biopsy studies have been reported that examined mediators of synovial tissue inflammation and joint damage that were found to be associated with unfavourable clinical and radiological outcomes (Table 2). In a limited longitudinal study of patients with early inflammatory arthritis, and a mean disease duration of 9.6 months (range 2 weeks to 18 months), the number of synovial lining layer macrophages at baseline was correlated with the number of new erosions on radiographs of the hands and feet 1 year later (P = 0.002) [25]. Most patients had RA. In all patients who developed new joint erosions it was observed that more than 60% of the infiltrating lining layer cells were macrophages, suggesting that a immunohistological analysis of synovial tissue at baseline might identify individual patients who were at increased risk of developing a more aggressive disease course. This observation is similar to the findings in patients with established RA [27, 43]. Macrophages are the primary source of the proinflammatory cytokines IL-1 and TNF-α, which induce the production of MMPs by fibroblast-like synoviocytes. Employing in situ hybridisation techniques, it was observed that the number of MMP-1-producing cells in the synovial lining layer, in contrast to cells producing cathepsin B and cathepsin L, seemed to be strongly correlated with the number of new erosions that developed during the first year of follow-up (P = 0.0007) [25].
In a similar early synovitis cohort, the expression of MMP-2, MMP-9, MMP-14 and TIMP-2 (tissue inhibitor of metalloproteinases-2) was quantified in synovial tissue biopsies obtained at baseline [61]. Radiographs of the hands and feet were repeated after 1 year. The synovial tissue samples from patients who developed joint erosions had significantly higher levels of MMP-2 than those from the patients who did not develop erosions (P = 0.04). There seemed to be considerable overlap between the groups, and the authors did not distinguish between MMP-2 expression in the lining and sublining layers. Nevertheless, the observation suggested that baseline tissue MMP-2 levels might be a marker for more aggressive synovial inflammation.
Early undifferentiated arthritis
General comments
With the emergence of convincing scientific evidence that very early introduction of disease-modifying therapies inhibits progressive structural damage more effectively [55], it is inevitable that some patients who receive treatment will not meet the ACR criteria for RA and will have a self-limiting, non-progressive arthritis. Thus, clinicians will seek a balance between exploiting the early 'window of opportunity' in some patients, and delaying effective treatment until the appearance of sufficient diagnostic criteria in others. About 30% of patients have an undifferentiated inflammatory arthritis at the time of their first presentation to an early arthritis clinic [50]. Similarly, a diagnosis of RA can be established in about 30% of patients. During the period of follow-up, many of the patients with undifferentiated arthritis will develop features that enable a diagnosis of RA, or other categories of arthritis. Several factors have been identified that distinguish groups of patients with undifferentiated arthritis who acquire a diagnosis of RA. Thus, the presence in the serum of anti-perinuclear factor [62], anti-RA33 [63], anti-Sa [64], anti-keratin [65], antifilaggrin [66] and anti-CCP antibodies [51] has been associated with the diagnosis or outcome of RA. In addition, high-titre antibody against serum amyloid A in patients attending an early arthritis clinic with undifferentiated arthritis was associated with a subsequent diagnosis of RA [67].
The value of synovial biopsy
Some studies employing synovial tissue analysis to identify early diagnostic markers in patients with undifferentiated arthritis have been reported (Table 3). In one study, a synovial biopsy was obtained from 95 patients who presented with unclassified arthritis for less than 12 months [68]. The objective was to determine which immunohistological markers could best distinguish RA from other categories of arthritis. Using regression analytic approaches, it was observed that high scores for CD38+ plasma cells and CD22+ B cells were the best discriminating markers when comparing RA with non-RA categories. The authors concluded that immunohistochemical analysis of synovial tissue samples could be used to distinguish patients with RA from other diagnostic categories.
In another study, immunohistological differences between RA and other categories of arthritis were also observed in 71 patients, including 16 who had had RA for less than 12 months [69]. The intensity of infiltration by both T and B cells, and differential expression of α V integrin, seemed to distinguish patients with RA from those with spondylarthritis and those with osteoarthritis. The disease duration of RA did not influence the findings. However, the immunohistological features highlighted in both of these studies seem insufficiently disease-specific for routine use as diagnostic markers.
The demonstration of intracellular citrullinated proteins in synovial tissue samples from 18 of 36 patients with RA, and in none of 52 patients with spondylarthritis, osteoarthritis and other categories of arthritis, suggested a useful method of discriminating RA from other inflammatory joint diseases [70]. This observation was the first description of a specific histological marker for RA in synovial tissue. The specificity of intracellular citrullinated proteins to RA is the subject of continuing investigation, and it is clear that further biochemical characterisation of the citrullinated proteins present in the synovium of patients with RA, and other inflammatory joint diseases, is required [71, 72]. Nevertheless, the possibility that demonstrating intracellular citrullinated protein in synovial tissue might be a new tool for the early diagnosis of undifferentiated arthritis is an important prospect.
Future challenges
There is increasing emphasis on the need to recognise potentially erosive disease in patients presenting with early undifferentiated arthritis, before sufficient criteria for RA have evolved. It is likely that pathophysiological pathways that directly or indirectly result in bone and cartilage degradation are preferentially activated in articular tissues from the earliest phases of the disease. The recognition of enhanced proinflammatory or degradative pathways, or the downregulation of inhibitory factors, that participate in the progression or prevention of arthritis, is most likely to emerge from studies of articular tissues. The preliminary studies of synovial tissues reported here support this hypothesis. The inclusion of pharmacogenomic and proteomic techniques in the analysis of synovial tissue from patients with different categories and stages of arthritis presents some exciting possibilities for future research.
Abbreviations
- ACR:
-
American College of Rheumatology
- CCP:
-
citrulline-containing peptide
- DMARDs:
-
disease-modifying anti-rheumatic drugs
- IL:
-
interleukin
- MMP:
-
matrix metalloproteinase
- RA:
-
rheumatoid arthritis
- RF:
-
rheumatoid factor
- TNF-α:
-
tumour necrosis factor-α
- VEGF:
-
vascular endothelial growth factor.
References
Forestier J: Instrumentation pour biopsie médicale. C R Séances Soc Biol Filiales. 1932, 110: 388-402.
Polley HF, Bickle WH, Dockerty MB: Experience with an instrument for punch biopsy of synovial membrane. Mayo Clin Proc. 1951, 26: 273-281.
Zeveley HA, French AJ, Mikkelsen WM, Duff IF: Synovial specimens obtained by knee joint punch biopsy. Histologic study in joint diseases. Am J Med. 1956, 20: 510-519. 10.1016/0002-9343(56)90135-8.
Parker HR, Pearson CM: A simplified synovial biopsy needle. Arthritis Rheum. 1963, 6: 172-176.
Williamson N, Holt LP: A synovial biopsy needle. Lancet. 1966, 9: 799-10.1016/S0140-6736(66)91871-X.
Moon MS, Kim JM: Synovial biopsy by Franklin–Silverman needle. Clin Orthop. 1980, 150: 224-228.
Jayson M, Dixon A: Arthroscopy of the knee in rheumatic diseases. Ann Rheum Dis. 1968, 27: 503-511.
Yates DB, Scott JT: Rheumatoid synovitis and joint disease. Relationship between arthroscopic and histological features. Ann Rheum Dis. 1975, 34: 1-6.
Henderson D, Jayson M, Tribe C: Lack of correlation of synovial histology with joint damage in rheumatoid arthritis. Ann Rheum Dis. 1975, 34: 7-11.
Kane D, Veale DJ, FitzGerald O, Reece R: Survey of arthroscopy performed by rheumatologists. Rheumatology. 2002, 41: 210-215. 10.1093/rheumatology/41.2.210.
Wallace DA, Carr AJ, Loach AB, Wilson-McDonald J: Day case arthroscopy under local anaesthesia. Ann R Coll Surg Engl. 1994, 76: 330-331.
Smith MD, Chandran G, Youssef PP, Darby T, Ahern MJ: Day case knee arthroscopy under regional anaesthesia performed by rheumatologists. Aust NZ J Med. 1996, 26: 108-109.
Reece R, Emery P: Needle arthroscopy. Br J Rheumatol. 1995, 34: 1102-1104.
Schumacher HR: Synovial fluid analysis and synovial biopsy. In Textbook of Rheumatology. Edited by: Kelley WN, Harris ED, Ruddy S, Sledge CB. 1993, Philadelphia: WB Saunders Company, 562-578.
Gerard HC, Wang Z, Wang GF, El-Gabalawy H, Goldbach-Mansky R, Li Y, Majeed W, Zhang H, Ngai N, Hudson AP, Schumacher HR: Chromosomal DNA from a variety of bacterial species is present in synovial tissue from various forms of arthritis. Arthritis Rheum. 2001, 44: 1689-1697. 10.1002/1529-0131(200107)44:7<1689::AID-ART293>3.0.CO;2-K.
Newman L, Rose C, Maier L: Sacroidosis. N Engl J Med. 1997, 336: 1224-1234. 10.1056/NEJM199704243361706.
Noone PG, Bresnihan B: Rheumatic disease in cystic fibrosis. In Cystic Fibrosis in Adults. Edited by: Yankaskas JR, Knowles MR. 1999, Philadelphia: Lippincott-Raven, 439-448.
Tak PP, Bresnihan B: The pathogenesis and prevention of joint damage in rheumatoid arthritis. Arthritis Rheum. 2000, 43: 2619-2633. 10.1002/1529-0131(200012)43:12<2619::AID-ANR1>3.0.CO;2-V.
Kraan MC, Reece RJ, Smeets TJM, Veale DJ, Emery P, Tak PP: Comparison of synovial tissues from the knee joints and the small joints rheumatoid arthritis patients. Implications for pathogenesis and evaluation of treatment. Arthritis Rheum. 2002, 46: 2034-2038. 10.1002/art.10556.
Rooney M, Condell D, Quinlan W, Daly L, Whelan A, Feighery C, Bresnihan B: Analysis of the histologic variation of synovitis in rheumatoid arthritis. Arthritis Rheum. 1988, 31: 956-963.
Bresnihan B, Cunnane G, Youssef P, Yanni G, FitzGerald O, Mulherin D: Rheumatoid arthritis: proposals for the evaluation of tissue samples by quantitative analysis. Br J Rheumatol. 1998, 37: 636-642. 10.1093/rheumatology/37.6.636.
Dolhain RJ, Ter Haar NT, De Kuiper R, Nieuwenhuis IG, Zwinderman AH, Breedveld FC, Miltenburg AM: Distribution of T cells and signs of T-cell activation in the rheumatoid joint: implications for semiquantitative comparative histology. Br J Rheumatol. 1998, 37: 324-330. 10.1093/rheumatology/37.3.324.
Kirkham B, Portek I, Lee CS, Stavros B, Lenarczyk A, Lassere M, Edmonds J: Intraarticular variability of synovial membrane histology, immunohistology, and cytokine mRNA expression in patients with rheumatoid arthritis. J Rheumatol. 1999, 26: 777-784.
Ulfgren A-K, Lindblad S, Klareskog L, Andersson J, Andersson U: Detection of cytokine producing cells in the synovial membrane from patients with rheumatoid arthritis. Ann Rheum Dis. 1995, 54: 654-661.
Cunnane G, FitzGerald O, Beeton C, Cawston TE, Bresnihan B: Early joint erosions and serum levels of matrix metalloproteinase 1, matrix metalloproteinase 3 and tissue inhibitor of metalloproteinases 1 in rheumatoid arthritis. Arthritis Rheum. 2001, 44: 2263-2274. 10.1002/1529-0131(200110)44:10<2263::AID-ART389>3.3.CO;2-T.
Rooney M, Whelan A, Feighery C, Bresnihan B: Changes in lymphocyte infiltration of the synovial membrane and the clinical course of rheumatoid arthritis. Arthritis Rheum. 1989, 32: 361-369.
Mulherin D, FitzGerald O, Bresnihan B: Synovial tissue macrophage populations and articular damage in rheumatoid arthritis. Arthritis Rheum. 1996, 39: 115-124.
Tak PP, Smeets TJM, Daha MR, Kluin PM, Meijers KAE, Brand R: Analysis of the synovial cell infiltrate in early rheumatoid synovial tissue in relation to local disease activity. Arthritis Rheum. 1997, 40: 217-225.
Soden M, Rooney M, Cullen A, Whelan A, Feighery C, Bresnihan B: Imunohistological features in the synovium obtained from clinically uninvolved knee joints of patients with rheumatoid arthritis. Br J Rheumatol. 1989, 28: 287-292.
Kraan MC, Versendaal H, Jonker M, Bresnihan B, Post WJ, 't Hart BA, Breedveld FC, Tak PP: Asymptomatic synovitis preceded clinically manifest arthritis. Arthritis Rheum. 1998, 41: 1481-1488. 10.1002/1529-0131(199808)41:8<1481::AID-ART19>3.0.CO;2-O.
Walters MT, Smith JL, Moore K, Evans PR, Cawley MI: An investigation of the action of disease modifying antirheumatic drugs on the rheumatoid synovial membrane: reduction in T lymphocyte subpopulations and HLA-DP and DQ antigen expression after gold or penicillamine therapy. Ann Rheum Dis. 1987, 46: 7-16.
Yanni G, Farahat MNMR, Poston RN, Panayi GS: Intramuscular gold decreases cytokine expression and macrophage numbers in the rheumatoid synovial membrane. Ann Rheum Dis. 1994, 53: 315-322.
Kirkham BW, Navarri FJ, Corkill MM, Panayi GS: In vivo analysis of disease modifying drug therapy activity in rheumatoid arthritis by sequential immunohistological analysis of synovial membrane interlukin 1β. J Rheumatol. 1994, 21: 1615-1619.
Firestein GS, Paine MM: Stromelysin and tissue inhibitor of metalloproteinase gene expression in rheumatoid arthritis synovium. Am J Pathol. 1992, 140: 1309-1314.
Dolhain RJEM, Tak PP, Dijkmans BAC, de Kuiper P, Breedveld FC, Miltenburg AMM: Methotrexate treatement reduces inflammatory cell numbers, expression of monokines and of adhesion molecules in synovial tissue of patients with rheumatoid arthritis. Br J Rheumatol. 1998, 37: 502-508. 10.1093/rheumatology/37.5.502.
Kraan MC, Reece RJ, Barg EC, Smeets TJ, Farnell J, Rosenburg R, Veale DJ, Breedveld FC, Emery P, Tak PP: Modulation of inflammation and metalloproteinase expression in synovial tissue by leflunomide and methotrexate in patients with active rheumatoid arthritis. Findings in a prospective, randomized, double-blind, parallel-design clinical trial in thirty-nine patients at two centers. Arthritis Rheum. 2000, 43: 1820-1830. 10.1002/1529-0131(200008)43:8<1820::AID-ANR18>3.0.CO;2-D.
Littman BH, Schumacher HR, Boyle DL, Weisman MH, Firestein GS: Effect of tenidap on metalloproteinase gene expression in rheumatoid arthritis: a synovial biopsy study. J Clin Rheumatol. 1997, 3: 194-202.
Youssef PP, Haynes DR, Triantafillou S, Parker A, Gamble JR, Roberts-Thomson PJ, Ahern MJ, Smith MD: Effects of pulse methylprednisolone on inflammatory mediators in peripheral blood, synovial fluid, and synovial membrane in rheumatoid arthritis. Arthritis Rheum. 1997, 40: 1400-1408.
Tak PP, Van der Lubbe PA, Cauli A, Daha MR, Smeets TJM, Kluin PM, Meinders AE, Yanni G, Panayi GS, Breedveld FC: Reduction of synovial inflammation after anti-CD4 monoclonal antibody treatment in early rheumatoid arthritis. Arthritis Rheum. 1995, 38: 1457-1465.
Tak PP, Taylor PC, Breedveld FC, Smeets TJ, Daha MR, Kluin PM, Meinders AE, Maini RN: Decrease in cellularity and expression of adhesion molecules by anti-tumor necrosis factor alpha monoclonal antibody treatment in patients with rheumatoid arthritis. Arthritis Rheum. 1996, 39: 1077-1081.
Ulfgren AK, Andersson U, Engstrom M, Klareskog L, Maini RN, Taylor PC: Systemic anti-tumor necrosis factor alpha therapy in rheumatoid arthritis down-regulates synovial tumor necrosis factor alpha synthesis. Arthritis Rheum. 2000, 43: 2391-2396. 10.1002/1529-0131(200011)43:11<2391::AID-ANR3>3.0.CO;2-F.
Cunnane G, Madigan A, Murphy E, FitzGerald O, Bresnihan B: The effects of treatment with interleukin-1 receptor antagonist on inflamed synovial membrane in rheumatoid arthritis. Rheumatology. 2001, 40: 62-69. 10.1093/rheumatology/40.1.62.
Yanni G, Whelan A, Feighery C, Bresnihan B: Synovial tissue macrophages and joint erosion in rheumatoid arthritis. Ann Rheum Dis. 1994, 53: 39-44.
Smith MD, Kraan MC, Slavotinek J, Au V, Weedon H, Parker A, Coleman M, Roberts-Thomson PJ, Ahern MJ: Treatment-induced remission in rheumatoid arthritis patients is characterized by a reduction in macrophage content of synovial biopsies. Rheumatology. 2001, 40: 367-374. 10.1093/rheumatology/40.4.367.
Brennan FM: Interleukin 10 and arthritis. Rheumatology. 1999, 38: 293-297. 10.1093/rheumatology/38.4.293.
Huizinga TWJ, Keijsers V, Yanni G, Hall M, Ramage W, Lanchbury J, Pitzalis C, Drossaers-Bakker WK, Westendorp RGJ, Breedveld FC, Panayi G, Verweij CL: Are differences in interleukin 10 production associated with joint damage?. Rheumatology. 2000, 39: 1180-1188. 10.1093/rheumatology/39.11.1180.
Koch AE: Angiogenesis: implications for rheumatoid arthritis. Arthritis Rheum. 1998, 41: 951-962. 10.1002/1529-0131(199806)41:6<951::AID-ART2>3.0.CO;2-D.
Latour F, Zabraniecki L, Dromer C, Brouchet A, Durroux R, Fourni B: Does vascular endothelial growth factor in the rheumatoid synovium predict joint damage? A clinical, radiological, and pathological study in 12 patients monitored for 10 years. Joint Bone Spine. 2001, 68: 493-498. 10.1016/S1297-319X(01)00313-X.
van der Heijde DM, van Leeuwen MA, van Riel PL, van de Putte LB: Radiographic progression on radiographs of hands and feet during the first 3 years of rheumatoid arthritis measured according to Sharp's method (van der Heijde modification). J Rheumatol. 1995, 22: 1792-1796.
van der Horst-Bruinsma IE, Speyer I, Visser H, Breedveld FC, Hazes JMW: Diagnosis and course of early-onset arthritis: results of a special early arthritis clinic compared to routine patient care. Br J Rheumatol. 1998, 37: 1084-1088. 10.1093/rheumatology/37.10.1084.
Schellekens GA, Visser H, de Jong BA, van den Hoogen FH, Hazes JM, Breedveld FC, van Venrooij WJ: The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Arthritis Rheum. 2000, 43: 155-163. 10.1002/1529-0131(200001)43:1<155::AID-ANR20>3.0.CO;2-3.
Bresnihan B, Alvaro-Gracia JM, Cobby M, Doherty M, Domljan Z, Emery P, Nuki G, Pavelka K, Rau R, Rozman B, Watt I, Williams B, Aitchison R, McCabe D, Musikic P: Treatment of rheumatoid arthritis with recombinant human interleukin-1 receptor antagonist. Arthritis Rheum. 1998, 41: 2196-2204. 10.1002/1529-0131(199812)41:12<2196::AID-ART15>3.3.CO;2-U.
Lipsky P, van der Heijde DMFM, St Clair EW, Furst DE, Breedveld FC, Kalden JR, Smolen JS, Weisman M, Emery P, Feldmann M, Harriman GR, Maini RN: Infliximab and methotrexate in the treatment of rheumatoid arthritis. N Engl J Med. 2000, 343: 1594-1602. 10.1056/NEJM200011303432202.
Bathon JM, Martin RW, Fleischmann RM, Tesser JR, Schiff MH, Keystone EC, Genovese MC, Wasko MC, Moreland LW, Weaver AL, Markenson J, Finck BK: A comparison of etanercept and methotrexate in patients with early rheumatoid arthritis. N Engl J Med. 2000, 343: 1586-1593. 10.1056/NEJM200011303432201.
Bukhari MAS, Wiles NJ, Lunt M, Harrison BJ, Scott DGI, Symmons DPM, Silman AJ: Influence of disease-modifying therapy on radiographic outcome in inflammatory polyarthritis at five years. Results from a large observational inception study. Arthritis Rheum. 2003, 48: 46-53. 10.1002/art.10727.
Bresnihan B: Rheumatoid arthritis: principles of early treatment. J Rheumatol. 2002, 29 (Suppl 64): 9-12.
Meyer O, Labarre C, Dougados M, Goupille P, Cantagre A, Dubois A, Nicaise-Roland P, Sibilia J, Combe B: Anticitrullinated protein/peptide antibody assays in early rheumatoid arthritis for predicting five year radiographic damage. Ann Rheum Dis. 2003, 62: 120-126. 10.1136/ard.62.2.120.
Combe B, Dougados M, Goupille P, Cantagrel A, Eliaou JF, Sibilia J, Meyer O, Sany J, Daures JP, Dubois A: Prognostic factors for radiographic damage in early rheumatoid arthritis: a multiparameter prospective study. Arthritis Rheum. 2001, 44: 1736-1743. 10.1002/1529-0131(200108)44:8<1736::AID-ART308>3.0.CO;2-I.
Drossaers-Bakker KW, Zwinderman AH, Vlieland TP, Van Zeben D, Vos K, Breedveld FC, Hazes JM: Long-term outcome in rheumatoid arthritis: a simple algorithm of baseline parameters can predict radiographic damage, disability, and disease course at 12-year followup. Arthritis Rheum. 2002, 15: 383-390. 10.1002/art.10513.
Visser H, le Cessie S, Vos K, Breedveld FC, Hazes JMW: How to diagnose rheumatoid arthritis early: a prediction model for persistent (erosive) arthritis. Arthritis Rheum. 2002, 46: 357-365. 10.1002/art.10117.
Goldbach-Mansky R, Lee J, McCoy A, Hoxworth J, Yarboro C, Smolen JS, Steiner G, Rosen A, Zhang C, Menard HA, Zhou ZJ, Palosuo T, Van Venrooij WJ, Wilder RL, Klippel JH, Schumacher HR, El-Gabalawy HS: Active synovial matrix metalloproteinase-2 is associated with radiographic erosions in patients with early rheumatoid arthritis. Arthritis Res. 2000, 2: 145-153. 10.1186/ar79.
Aho K, von Essen R, Kurki P, Palosuo T, Heliovaara M: Antikeratin antibody and antiperinuclear factor as markers for subclinical rheumatoid disease process. J Rheumatol. 1993, 20: 1278-1281.
Hassfeld W, Steiner G, Graninger W, Witzmann G, Schweitzer H, Smolen JS: Autoantibody to the nuclear antigen RA33: a marker for early rheumatoid arthritis. Br J Rheumatol. 1993, 32: 199-203.
Menard HA, Lapointe E, Rochdi MD, Zhou ZJ: Insights into rheumatoid arthritis derived from the Sa immune system. Arthritis Res. 2000, 2: 429-432. 10.1186/ar122.
Young BJJ, Mallya RK, Leslie RDG, Clark CJM, Hamblin TJ: Antikeratin antibodies in rheumatoid arthritis. Br Med J. 1979, ii: 97-99.
Forslin K, Vincent C, Serre G, Svensson B: Anti-filaggrin antibodies in early rheumatoid arthritis may predict radiological progression. Scand J Rheumatol. 2001, 30: 221-224. 10.1080/030097401316909567.
Cunnane G, Grehan S, Geoghegan S, Shields D, McCormack C, Whitehead A, Bresnihan B, FitzGerald O: Serum amyloid A in the assessment of early inflammatory arthritis. J Rheumatol. 2000, 27: 58-63.
Kraan MC, Haringman JJ, Post WJ, Versendaal J, Breedveld FC, Tak PP: Immunohistological analysis of synovial tissue for differential diagnosis in early arthritis. Rheumatology. 1999, 38: 1074-1080. 10.1093/rheumatology/38.11.1074.
Baeten D, Demetter P, Cuvelier C, Van den Bosch F, Kruithof E, Van Damme N, Verbruggen G, Mielants H, Veys EM, De Keyser F: Comparative study of the synovial histology in rheumatoid arthritis, spondyloarthropathy, and osteoarthritis: influence of disease duration and activity. Ann Rheum Dis. 2000, 59: 945-953. 10.1136/ard.59.12.945.
Baeten D, Peene I, Union A, Meheus L, Sebbag M, Serre G, Veys EM, De Keyser F: Specific presence of intracellular citrullinated proteins in rheumatoid arthritis synovium: relevance to antifilaggrin autoantibodies. Arthritis Rheum. 2001, 44: 2255-2262. 10.1002/1529-0131(200110)44:10<2255::AID-ART388>3.0.CO;2-#.
Masson-Bessiere C, Sebbag M, Girbal-Neuhauser E, Nogueira L, Vincent C, Senshu T, Serre G: The major synovial targets of the rheumatoid arthritis-specific antifilaggrin autoantibodies are deiminated forms of the alpha- and beta-chains of fibrin. J Immunol. 2001, 166: 4177-4184.
Smeets TJM, Vossenaar EM, van Venrooij WJ, Tak PP: Is expression of intracellular citrullinated proteins in synovial tissue specific for rheumatoid arthritis?. Arthritis Rheum. 2002, 46: 2824-2826. 10.1002/art.10473.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Rights and permissions
About this article
Cite this article
Bresnihan, B. Are synovial biopsies of diagnostic value?. Arthritis Res Ther 5, 271 (2003). https://doi.org/10.1186/ar1003
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar1003