Abstract
Background
Mental burden due to the SARS-CoV-2 pandemic has been widely reported for the general public and specific risk groups like healthcare workers and different patient populations. We aimed to assess its impact on mental health during the early phase by comparing pandemic with prepandemic data and to identify potential risk and protective factors.
Methods
For this systematic review and meta-analyses, we systematically searched PubMed, PsycINFO, and Web of Science from January 1, 2019 to May 29, 2020, and screened reference lists of included studies. In addition, we searched PubMed and PsycINFO for prepandemic comparative data. Survey studies assessing mental burden by the SARS-CoV-2 pandemic in the general population, healthcare workers, or any patients (eg, COVID-19 patients), with a broad range of eligible mental health outcomes, and matching studies evaluating prepandemic comparative data in the same population (if available) were included. We used multilevel meta-analyses for main, subgroup, and sensitivity analyses, focusing on (perceived) stress, symptoms of anxiety and depression, and sleep-related symptoms as primary outcomes.
Results
Of 2429 records retrieved, 104 were included in the review (n = 208,261 participants), 43 in the meta-analysis (n = 71,613 participants). While symptoms of anxiety (standardized mean difference [SMD] 0.40; 95% CI 0.15–0.65) and depression (SMD 0.67; 95% CI 0.07–1.27) were increased in the general population during the early phase of the pandemic compared with prepandemic conditions, mental burden was not increased in patients as well as healthcare workers, irrespective of COVID-19 patient contact. Specific outcome measures (eg, Patient Health Questionnaire) and older comparative data (published ≥5 years ago) were associated with increased mental burden. Across the three population groups, existing mental disorders, female sex, and concerns about getting infected were repeatedly reported as risk factors, while older age, a good economic situation, and education were protective.
Conclusions
This meta-analysis paints a more differentiated picture of the mental health consequences in pandemic situations than previous reviews. High-quality, representative surveys, high granular longitudinal studies, and more research on protective factors are required to better understand the psychological impacts of the SARS-CoV-2 pandemic and to help design effective preventive measures and interventions that are tailored to the needs of specific population groups.
Similar content being viewed by others
Introduction
The emergence of novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was described for the first time in Wuhan, China [1, 2] and declared a public health emergency of international concern on 30 January 2020 [3]. The virus spread rapidly and, as of January 14, 2021, led to 90,759,370 confirmed infections and 1,963,169 deaths worldwide [4].
During the early phase of the pandemic, many countries adopted drastic measures, including testing, tracing, self-isolation, and quarantine measures as well as broader population measures ranging from travel bans, school closures, assembly restrictions, curfews, to full lockdowns [5,6,7]. Besides substantial stressors for individuals and the general public (eg, social isolation, reduced income, restructuring of school, university, and work life) and healthcare systems (eg, disruption of essential health services) [8, 9], the SARS-CoV-2 pandemic has had major socio-economic consequences for the affected countries (eg, global supply chain disruptions) [10, 11]. By drastically changing our way of social interaction (eg, social distancing), it continues to affect many areas of daily life and in line with this social life and participation.
The disease-related threats, containment measures, and associated stressors may have a negative psychological impact on the community at large and potentially even more so on specific risk groups [12,13,14,15,16,17]. Given the work-related stressors in the context of disease outbreaks (eg, high workload, risk of infection, triage decisions), healthcare workers may suffer from a particularly high burden [18]Footnote 1,Footnote 2 [20,21,22]. Patients with pre-existing physical or mental conditions (eg, chronically ill individuals, psychiatric patients, geriatric patients), people with confirmed COVID-19 diagnosis, those recovering from the infection, or suffering from long COVID-19, and subgroups with special risk exposure (eg, caregivers) may also be at risk of developing stress-related mental symptoms [15, 22,23,24,25,26,27,28].
Various systematic reviews have synthesized the evidence on psychiatric symptoms associated with previous highly contagious infectious disease outbreaks (eg, Ebola, SARS-CoV) and the SARS-CoV-2 pandemic [20, 24, 29,30,31,32,33,34,35], some of them also narratively summarizing risk and protective factors for mental health [20, 30, 31, 33, 34]. Several meta-analyses have been conducted, either calculating the pooled prevalence of mental symptoms or odds ratios for the risk of mental burden attributable to the SARS-CoV-2 pandemic [20, 24, 29, 32, 33, 36]. Potential moderators of the negative mental health impact were also partly investigated [32]. International evidence indicates an elevated level of mental symptoms in the general public, including symptoms of anxiety, depression, and stress [30,31,32,33, 36]. Confirming the risk status of healthcare workers, several reviews also found an increased prevalence of mental symptoms in this group [18]1,2 [20, 29, 31, 32]. Finally, a few studies in patient populations (eg, COVID-19 patients, patients with pre-existing mental or physical conditions) show increased mental burden [24, 31,32,33].
There are several shortcomings of reviews published to date. Most either focus on the general population, healthcare workers, or patients, with only few publications examining the level of mental burden across all three specified, most relevant population groups [31,32,33]. Further limitations included a limited search strategy [31], language restrictions [24, 30, 31, 33], or a missing preregistration [20, 24, 29,30,31, 33, 36]. Most importantly, all but one systematic review failed to compare the mental burden during an ongoing pandemic with the burden before the pandemic [31]. Such comparisons, however, are necessary to quantify the mental burden specifically attributable to the current pandemic. We therefore aimed to assess the mental health impact of the SARS-CoV-2 pandemic by comparing data from the early phase of the current pandemic with prepandemic data in the general population, healthcare workers, and patients. We aimed to identify population-specific risk and protective factors for mental health.
Methods
Review registration
This systematic review [37] was preregistered with PROSPERO (registration no. CRD42020193249) with the title ‘Psychological distress, protective factors and resilience during the SARS-CoV-2 pandemic: a systematic review and meta-analysis with comparison to standard data’. Details of the methods are presented in the Additional file 1. The MOOSE Checklist for Meta-analyses of Observational Studies and differences between the protocol and the final review are presented in eTables 1 and 2.
Search strategy and selection criteria
We searched three bibliographic databases from January 1, 2019 to May 29, 2020 (PubMed, PsycINFO, and Web of Science) and inspected the reference lists of included studies. The search strategy comprised terms associated with mental health, pandemics, and the populations of interest (see eMethods 1 in Additional file 1). There were no restrictions concerning language, publication date, or publication format. We did not consider preprint articles. If not reported within a study, we systematically searched for prepandemic comparative data in the same or a similar population (PubMed, PsycINFO; see eMethods 2).
The populations of interest comprised the general population, healthcare workers, and any patients (eg, COVID-19 patients, those with pre-existing physical or mental conditions; eTable 3). Participants were included irrespective of age, health, or employment status. We did not consider infectious disease outbreaks other than due to SARS-CoV-2. To be eligible for the review, studies had to assess at least one mental health outcome, with a broad range of eligible outcomes (ie, anxiety and worrying, depression, posttraumatic stress, sleep, stress, general psychological distress). These outcomes were also considered for a descriptive synthesis of the prevalence (see data analysis). We included original research articles reporting on cross-sectional and longitudinal surveys.
All pandemic studies meeting these criteria were included but were only taken forward to pairwise meta-analyses if using a validated outcome measure and if prepandemic comparative data were available (eTables 4, 5). These were defined as data collected before the exposure to the current pandemic, and in the absence of other disease outbreaks or macro-stressors (eg, disasters), in the same country and population group (if available) and using the same outcome measure. In contrast to the review, we only focused on the four most frequently reported mental health outcomes (primary outcomes), including symptoms related to stress, anxiety, depression, or sleep. Posttraumatic stress, although reported more often than sleep, was not considered for pairwise meta-analyses. As this outcome is usually measured in the aftermath of macro-stressors, we were not able to identify adequate comparative data as mentioned above. Comparative data were selected stepwise using four levels to ensure best available comparability between SARS-CoV-2 exposure (‘pandemic’) studies and prepandemic (‘comparative’) studies. If representative studies in the same country and population (level 1) were not available, we used prepandemic studies in the same (level 2) or an alternative population (level 3; eg, healthcare workers compared with the general population), before resorting to the best available data in a similar country (level 4).
Study selection, data extraction, and quality assessment
The study selection process for the pandemic studies at the level of titles/abstracts and full-texts was performed in duplicate by two reviewers independently (NR, LG). Any disagreements were resolved by discussion or by consulting a third reviewer (KL). At both title/abstract (κ = 0.90) and full-text level (κ = 0.97), excellent inter-rater reliability was achieved.
Relevant information for each included study was extracted in duplicate by two reviewers (NR, LG), working independently, using a customized spreadsheet (eTable 6), which was shortened for the extraction of comparative data. Discrepancies were resolved through discussion or by a third reviewer (KL).
Three independent reviewers (NR, JSW, LG) assessed the quality of included studies using the modified National Institutes of Health (NIH) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [38] (eTable 7), with disagreements being resolved by discussion or a third reviewer (KL). The level of comparability between pandemic and comparative data was assessed using a self-developed tool with four levels based on the previously mentioned levels for the stepwise selection of comparative data (eTable 8).
Data analysis
The included studies were synthesized in narrative and tabular form, with a descriptive analysis of prevalence rates for mental health symptoms (ie, proportion of participants beyond a cut-off score reported in the included study) and of risk and protective factors. If adequate comparative data for any of the primary outcomes were available, pairwise meta-analyses were performed for the general population, healthcare workers, and patients, respectively (eMethods 3). Given the multiple uses of comparative studies, we used multilevel meta-analyses [39] for the general population and healthcare workers, with pandemic studies being clustered according to prepandemic comparators. For patients, the multilevel model reduces to the classic random-effects model as different comparative studies were available. Prediction intervals were calculated in meta-analyses with at least four studies to take the large between-study heterogeneity into account [40].
Two sensitivity analyses referred to the quality of pandemic studies and the level of comparability (see Search strategy and selection criteria), by limiting the analyses to very comparable pandemic and prepandemic studies (ie, level 1 and 2 mentioned above).
Subgroup analyses for each of the three groups were performed for the surveyed populations (eg, age), characteristics of the pandemic studies (eg, survey start) and of comparative data (eg, publication year), and the relationship of sample sizes in pandemic versus comparative studies, in order to identify potential sources of heterogeneity of the psychological impact of the SARS-CoV-2 pandemic.
Results
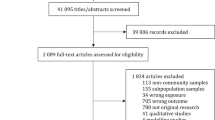
Details of the results are presented in the Additional file 2. The systematic search for studies performed during the SARS-CoV-2 pandemic identified 2429 records from database searches and 17 additional records from reference lists, of which 104 studies were included in the review and 43 studies in the meta-analyses (Fig. 1). Of the 104 eligible studies, most studies were performed in the general population (50 studies), followed by 30 studies in healthcare workers, and seven studies in various patient populations. Seventeen studies included mixed samples. Across the three population groups, a total of 208,261 participants ranging from 51 to 52,730 participants [41, 42]1 from the pandemic studies were included in the review, the number of participants considered in the meta-analyses, in total 71,613, ranged from 127 to 60,213 participants (eTable 9).
The study characteristics of the 104 included pandemic studies (early phase) are presented in Table 1.
Although we imposed no restrictions on the age limits, we identified no studies conducted in children but did find some studies in the general population that included participants below the age of 18 years [47, 58]1. Thus, the mean age of participants in the pandemic studies ranged from 20 (SD not reported) to 56.9 (SD 7.6) years [49, 99]1. The studies covered Asia (67 studies [26, 41,42,43, 49, 50, 54, 57, 58, 60, 62, 64, 71, 74, 76, 80, 81, 85, 86, 88,89,90,91, 93, 98, 101, 102, 104, 109, 111,112,113,114,115,116, 118,119,120,121,122,123, 126, 124, 128, 131,132,133, 136, 137, 140, 141, 143, 145]1 [18, 48, 59, 73, 84, 87, 92, 100, 105, 106, 108, 117, 134, 138, 139, 142, 144]1,2 [127]1,Footnote 3) thereof from China [42, 49, 50, 57, 58, 60, 62, 64, 71, 80, 81, 85, 86, 88,89,90,91, 93, 101, 104, 109, 115, 116, 118,119,120, 122,123,124, 126, 128, 131,132,133, 136, 140, 141, 143, 145]1 [18, 48, 59, 84, 87, 92, 100, 105, 106, 108, 117, 134, 138, 139, 142, 144]1,2 [127]1,3, Europe (24 studies) [47, 99, 44,45,46, 51,52,53, 55, 61, 63, 65, 66, 68, 70, 110, 77, 78, 82, 83, 94, 97, 130, 103, 135]1, North America (six studies) [56, 67, 79, 107, 146, 147]1, or different continents (seven studies) [69, 72, 75, 95, 96, 125, 129]1. For 13 studies investigating more than one population, several samples were considered [130,131,132,133, 135, 140, 141, 143, 145]1 [134, 138, 139, 144]1,2. We identified 47 matching prepandemic comparative studies (eTable 10), including one pandemic study reporting adequate comparative data [127]1,3 [148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193]3.
Prevalence rates of the six mental health symptoms, that were considered for the review, were available for a varying number of included pandemic studies (Table 2). The proportion of participants beyond a cut-off value in the included studies varied considerably (eg, anxiety in general population: 0.7–64.0%). Based on cut-off values reported in the primary studies (eTable 11), we found increased levels of mental burden during the SARS-CoV-2 pandemic in the general population, healthcare workers, and patients regarding each of the symptoms observed during the current pandemic, that is, without considering the prepandemic situation.
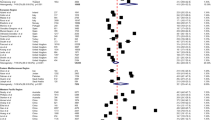
In pairwise meta-analyses comparing pandemic (early phase) with prepandemic data for the four primary outcomes, however, we found only evidence for a small increase of anxiety (standardized mean difference [SMD] 0.40; 95% CI 0.15–0.65; p = .002) and a moderate increase of depressive symptoms (SMD 0.67; 95% CI 0.07–1.27; p = .03) in the general population. No evidence for a change in stress or sleep-related symptoms was identified (Table 3). For healthcare workers compared with healthcare staff before the pandemic, the meta-analyses showed no evidence of any effect on the primary outcomes (Table 3). The same was found for patients (Table 3); however, prepandemic data in patients were only available for four samples. Forest plots are presented in Figs. 2, 3, and eResults 1 in the Additional file 2.
Of the 104 studies, 38 studies were judged to be of fair quality and 57 studies of poor quality, with main concerns regarding selection bias, the validity of outcome measures, and the description of the sample and the survey period (eTable 12). From nine high-quality studies, four were representative surveys [44, 47, 77, 88]1. From the 85 pairwise comparisons relevant for meta-analyses, 52 comparisons were of level-1 and 33 of level-2 quality (eTable 13). When excluding low-quality pandemic studies (Table 3), the effects on anxiety and depressive symptoms in the general population increased. The effect on anxiety in the general population was stable in the sensitivity analysis when only best comparable data sets (ie, level-1 and level-2 comparability) were included, while there was no longer evidence for an effect on depressive symptoms (Table 3 and eResults 2 in Additional file 2).
Heterogeneity was considerable in main and sensitivity analyses, with I2 scores mostly ranging from 90 to 100% and wide prediction intervals (Table 3). We therefore performed subgroup analyses with at least k = 5 studies in the main analyses in attempts to explain this heterogeneity (Table 4; eResults 3 in Additional file 2).
Regarding population characteristics (pandemic studies), age was no consistent risk or protective factor. Within the general population, we identified no evidence for a subgroup difference according to stressor exposure except for elevated sleep symptoms in isolated individuals [62]1. In healthcare workers, there was no evidence for a moderating effect of COVID-19 patient contact on mental health. In different groups of patients, we identified no evidence of differences in anxiety or depression. Compared with COVID-19 patients [131]1, psychiatric patients reported more stress, with the caveat of few studies [42, 132, 135]1.
Among general characteristics of the pandemic studies, we found no (consistent) evidence of differences depending on when the surveys started, whether they were conducted in China, or the sample size. We found evidence of an elevated level of depressive symptoms in the general population and patients depending on the specific outcome measure employed (eg, Patient Health Questionnaire [PHQ], Zung Self-Rating Depression Scale [SDS]).
In subgroup analyses for comparative study characteristics, there was no evidence of a consistent moderation of comparison sample sizes.
Across the three populations, we identified a higher level of anxiety and depressive symptoms if included studies were compared to prepandemic data published five or more years before versus a smaller burden in comparison to prepandemic data of less than 2 years ago.
The relationship of sample sizes explained the heterogeneity of the psychological impact of the SARS-CoV-2 pandemic in the general population and patients, with evidence for elevated symptoms of anxiety if similar sample sizes were compared.
The risk and protective factors narratively identified for each population are presented in Table 5 and eTables 14 and 15, with most of them being investigated in the general population, and few studies investigating protective factors at all. Most frequently named risk factors across the populations were pre-existing mental disorders, female sex, and concerns about COVID-19 infection, whereas most frequently reported protective factors were older age, good economic situation, and higher education.
Discussion
To our knowledge, this is the first systematic review and meta-analysis to assess the mental health impact of the SARS-CoV-2 pandemic in the general population, healthcare workers, and patients, by contrasting data from the early phase of the current pandemic with prepandemic data. We identified 104 independent studies, mainly in the general population, that suggest an increased prevalence of mental burden due to the SARS-CoV-2 pandemic. This finding is in line with previous reviews and meta-analyses that merely pooled the prevalence of or calculated the risk for mental burden in either one or several of these groups [20, 24, 29, 32, 33, 36].
On the other hand, the pairwise meta-analyses for 43 studies across the four primary outcomes revealed different results. Compared with prepandemic data, we only found an elevated level of some mental symptoms (anxiety, depression) due to the SARS-CoV-2 pandemic in the general population, but not of stress or sleeping problems.
Although healthcare workers were found to be a group at risk for mental health problems during the SARS-CoV-2 pandemic [18]1,2 [20, 29, 31, 32], we identified no evidence for an increased mental burden during the early phase when comparing them with healthcare staff prior to the pandemic. Because of a (chronic) work-related risk exposure in daily life [194], as a kind of ‘stress inoculation’, healthcare professionals might have learned effective strategies (eg, self-efficacy) helping them to cope more professionally with crises than other groups. In contrast to previous findings [20, 195], the level of COVID-19 patient contact did not affect the mental health impact.
Overall, the results of this review paint a more nuanced picture of the mental health consequences of the SARS-CoV-2 pandemic than previous reviews – an observation in line with stress resilience research that identified different trajectories of psychological adaptation after potentially traumatic events, ranging from no mental burden to severe mental illness [196, 197]. Indeed, a recent analysis of 523 healthy subjects from the German LORA study showed a decrease of perceived stress and stressor load while mental health improved during the eight-week measurement after lockdown, indicating that the pandemic and pandemic response may also have positive effects [198]. The number of studies reporting on protective factors in this review was rather limited, especially in healthcare workers and patients. However, these factors might also partly explain the heterogeneity of findings regarding mental health consequences. This is in line with positive aspects (eg, improved social relationships with close social contacts such as families) that were likewise reported for previous infectious disease outbreaks. The importance of taking a ‘resilience perspective’ in SARS-CoV-2 mental health research and investigating resilience factors has been pointed out previously [19, 22, 197, 199].
Several aspects must be considered when interpreting the results. First, the absence of evidence of effects in healthcare workers and patients in this review does not necessarily mean that there is evidence for the absence of effects of the SARS-CoV-2 pandemic on mental health in these groups. Second, for healthcare workers, the mental burden on individuals probably depends on the location of survey (eg, country, region) and how heavily the respective healthcare systems were burdened in the pandemic timeline (eg, number of hospitalized COVID-19 patients). Among the 13 included studies in meta-analyses for healthcare staff, we could only include a few studies from heavily burdened countries (eg, Italy: k = 2; Spain: k = 0; USA: k = 0). However, nine studies in these meta-analyses had been conducted in China, which, compared internationally, was less affected by the SARS-CoV-2 pandemic [4]. In the subgroup analysis regarding the level of COVID-19 patient contact, we assigned studies to the subgroup ‘high level of contact’ if at least 50% of the sample had close contact to COVID-19 patients (ie, ‘frontline healthcare workers’). However, the nature of contact was insufficiently described in the included studies.
Strengths of this review compared with previous publications include the systematic search for comparative prepandemic data for inclusion in pairwise meta-analyses, the stepwise selection of prepandemic studies to ensure best available comparability, and the population-specific analysis of risk and protective factors. One limitation refers to the search methods for pandemic studies (eg, no preprints; no reference lists of reviews) and comparative data (eg, subgroups in general population only partially searched). We had no restrictions regarding the publication format except for the exclusion of preprints which might be viewed as limitation. This restriction might have affected the evidence found in this review compared to others (eg, Cochrane reviews) where preprint articles are included.
The large between-study heterogeneity, a problem shared by previous meta-analyses [20, 24, 32, 33], could not be fully explained by subgroup analyses. This heterogeneity probably resulted from differences between the pandemic studies (eg, countries, sociocultural differences in the perception of mental burden, pandemic outbreak severity, subpopulations, outcome measures) and variability between the comparative studies (eg, study design, outcome measures), respectively. Among the pandemic studies, especially the specific outcome measures used were an important source of heterogeneity. Furthermore, the pandemic and comparative data were heterogeneous (eg, country, population), which could be partially captured by our self-developed tool for the level of comparability and was controlled for by the corresponding sensitivity analysis. We cannot preclude that moderators of effects are present that we, though our best efforts, did not identify and therefore could not control for. Besides, comparative studies with larger sample sizes were preferred, leading to small 95% CIs and a lack of CI overlap with pandemic study findings. Despite the comprehensiveness of this review compared to previous publications, the small number of studies in certain subgroups potentially limited the statistical power (eg, surveys including students).
Apart from specific outcome measures, less recent comparative data, and homogenous sample sizes, the subgroup analyses indicated no consistent determinants of heterogeneity. An elevated level of depression based on the assessment with the PHQ and SDS might – at least for the PHQ-9 – be explained by the high sensitivity to change of this instrument and its usefulness to monitor treatment outcomes [200, 201]. Given the increased mental burden if pandemic studies were compared to older prepandemic data, cohort effects cannot be excluded.
Discrepancies between subgroup analyses and the narrative synthesis of risk and protective factors (eg, COVID-19 patient contact) might be due to methodological differences. Because of the primary use of screening but not diagnostic tools to determine mental burden in the included pandemic studies, this review does not allow any conclusions concerning a putative increase of diagnoses of mental disorders during the early phase of the SARS-CoV-2 pandemic. Consistent with the synthesis of risk factors, the meta-analyses partly showed an increased level of mental symptoms in young and middle-aged groups, in line with previous studies [12]. However, more studies including elderly would be needed to clearly investigate age differences, and whether the pandemic works as a ‘burning lens’ for the already increased mental burden in young people [202]. Finally, given the pandemic timeline, the evidence is substantially based on Chinese studies thus potentially limiting the transferability of findings to other contexts.
Further research in other countries (eg, USA), that started later on during the pandemic, could change the findings. The latter is also supported by the wide prediction intervals identified in this review, which indicate uncertainty in our conclusions about whether the pandemic and related stressors do affect mental health [203].
The review has several implications for research and practice. There is an urgent need for representative surveys, in order to allow fair comparisons between the mental burden caused by SARS-CoV-2 in different countries and to examine other risk and protective factors (eg, cultural context). Representative surveys in the general population might also serve to identify specific subgroups at risk for which further studies would be needed. From a public mental health perspective, a stronger focus on (psychosocial) protective factors for mental health would be desirable to derive appropriate contents for preventive measures (eg, pandemic preparedness plans) or health-promoting interventions (eg, resilience training) prior to, during, and after a pandemic [199]. By further investigating the mental health impact of specific stressors – in line with Brooks and colleagues [13] – researchers and practitioners might gain further knowledge about when (eg, in pandemic timeline) and for whom (eg, after exposure to which stressors) interventions should be implemented to buffer negative mental health effects of SARS-CoV-2.
Conclusions
In conclusion, compared with prepandemic data, this review shows different adverse mental health consequences of the early phase of the SARS-CoV-2 pandemic in the examined population groups in contrast to previous research, with healthcare workers being more resilient than expected. The quality of studies varies. High-quality, representative surveys in the general population and specific subpopulations, longitudinal studies, and further research efforts on protective factors are needed to better understand the psychological impacts of the SARS-CoV-2 pandemic and to help design effective preventive measures and interventions that are tailored to the needs of specific population groups.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files. Additional data (eg, detailed extracted data) are available from the corresponding author on request.
Notes
included pandemic studies.
studies already considered in previous systematic review (Gilan, Röthke and colleagues) [19].
prepandemic comparative studies.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- LORA:
-
Longitudinal Resilience Assessment
- MOOSE:
-
Meta-analyses Of Observational Studies in Epidemiology
- NIH:
-
National Institutes of Health
- PHQ:
-
Patient Health Questionnaire
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- SARS-CoV(− 2):
-
Severe Acute Respiratory Syndrome Coronavirus (− 2)
- SD:
-
Standard deviation
- SDS:
-
Zung Self-Rating Depression Scale
- SMD:
-
Standardized mean difference
References
Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–74.
World Health Organization. Disease outbreak news. Novel coronavirus – China. 2020. https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/. Accessed 30 June 2020.
Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–6.
World Health Organization. Coronavirus (COVID-19) Dashboard. 2020. https://who.sprinklr.com/. Accessed 28 Sept 2020.
BBC. Coronavirus: the world in lockdown in maps and charts. 2020. https://www.bbc.com/news/world-52103747. Accessed 30 June 2020.
The Guardian. China's coronavirus lockdown strategy: brutal but effective. 2020. https://www.theguardian.com/world/2020/mar/19/chinas-coronavirus-lockdown-strategy-brutal-but-effective. Accessed 7 May 2020.
White House. The President’s coronavirus guidelines for America. 2020. Accessed 30 June 2020.
World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report. 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1. Accessed 4 Nov 2020.
Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8(5):506–17.
Pak A, Adegboye OA, Adekunle AI, Rahman KM, McBryde ES, Eisen DP. Economic consequences of the COVID-19 outbreak: the need for epidemic preparedness. Front Public Health. 2020;8:241.
Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–93.
Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–92.
Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20.
Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–2.
Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–60.
Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020;14(5):779–88.
Inter-Agency Standing Committee (IASC). Interim briefing note addressing mental health and psycosocial aspects of COVID-19 outbreak (developed by the IASC’s Reference Group on Mental Health and Psychosocial Support). 2020. https://interagencystandingcommittee.org/iasc-reference-group-mental-health-and-psychosocial-support-emergency-settings/interim-briefing. Accessed 2 Oct 2020.
Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease. JAMA Netw Open. 2020;3:e203976.
Gilan D, Röthke N, Blessin M, et al. Psychomorbidity, resilience, and exacerbating and protective factors during the SARS-CoV-2-pandemic. A systematic literature review and results from the German COSMO-PANEL. Dtsch Arztebl Int. 2020;117(38):625–32.
Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642.
Robertson E, Hershenfield K, Grace SL, Stewart DE. The psychosocial effects of being quarantined following exposure to SARS: a qualitative study of Toronto health care workers. Can J Psychiatr. 2004;49(6):403–7.
Vinkers CH, van Amelsvoort T, Bisson JI, et al. Stress resilience during the coronavirus pandemic. Eur Neuropsychopharmacol. 2020;35:12–6.
Yao H, Chen J-H, Xu Y-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):E21.
Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611–27.
Chan E, Gobat N, Kim JH, et al. Informal home care providers: the forgotten health-care workers during the COVID-19 pandemic. Lancet. 2020;395(10242):1957–9.
Wang H, Li T, Barbarino P, et al. Dementia care during COVID-19. Lancet. 2020;395(10231):1190–1.
National Health Service. After-care needs of inpatients recovering from COVID-19. 2020. https://search3.openobjects.com/mediamanager/nottinghamshire/fsd/files/c0388-after-care-needs-of-inpatients-recovering-from-covid-19-5-june-2020.pdf. Accessed 2 Oct 2020.
Eckardt JP. Caregivers of people with severe mental illness in the COVID-19 pandemic. Lancet Psychiatry. 2020;7(8):e53.
da Silva FCT, Neto MLR. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry. 2020;104:110062.
Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64.
Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;S0889–1591(20):30954–5.
Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293:113382.
Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. 2020;291:113190.
Preti E, Di Mattei V, Perego G, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Reports. 2020;22(8):43.
Cénat JM, Felix N, Blais-Rochette C, et al. Prevalence of mental health problems in populations affected by the Ebola virus disease: a systematic review and meta-analysis. Psychiatry Res. 2020;289:113033.
Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1):57.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
National Heart, Lung, and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies 2014. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 2 Oct 2020.
Van den Noortgate W, López-López JA, Marín-Martínez F, Sánchez-Meca J. Three-level meta-analysis of dependent effect sizes. Behav Res. 2013;45(2):576–94.
Higgins JPT, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A (Statistics in Society). 2009;172(1):137–59.
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213.
Liu X, Lin H, Jiang H, et al. Clinical characteristics of hospitalised patients with schizophrenia who were suspected to have coronavirus disease (COVID-19) in Hubei Province, China. Gen Psychiatr. 2020;33(2):e100222.
Ahmad AR, Murad HR. The impact of social media on panic during the COVID-19 pandemic in Iraqi Kurdistan: online questionnaire study. J Med Internet Res. 2020;22(5):e19556.
Bacon AM, Corr PJ. Coronavirus (COVID-19) in the United Kingdom: a personality-based perspective on concerns and intention to self-isolate. Br J Health Psychol. 2020;25(4):839–48.
Bäuerle A, Teufel M, Musche V, et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health (Oxf). 2020;42(4):672–78.
Teufel M, Schweda A, Dörrie N, et al. Not all world leaders use twitter in response to the COVID-19 pandemic: impact of the way of Angela Merkel on psychological distress, behaviour and risk perception. J Public Health. 2020;42(3):644–6.
Buzzi C, Tucci M, Ciprandi R, et al. The psycho-social effects of COVID-19 on Italian adolescents' attitudes and behaviors. Ital J Pediatr. 2020;46(1):69.
Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934.
Chang J, Yuan Y, Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao. 2020;40(2):171–6.
Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4):e0231924.
Germani A, Buratta L, Delvecchio E, Mazzeschi C. Emerging adults and COVID-19: the role of individualism-collectivism on perceived risks and psychological maladjustment. Int J Environ Res Public Health. 2020;17(10):3497.
González-Sanguino C, Ausín B, Castellanos MÁ, et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172–6.
Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic [published online ahead of print, 2020 Apr 27]. Int J Ment Heal Addict. 2020:1–14. https://doi.org/10.1007/s11469-020-00281-5.
Jahanshahi AA, Dinani MM, Madavani AN, Li J, Zhang SX. The distress of Iranian adults during the Covid-19 pandemic - more distressed than the Chinese and with different predictors. Brain Behav Immun. 2020;87:124–5.
Lauri Korajlija A. Jokic-Begic N. COVID-19: Concerns and behaviours in Croatia [published online ahead of print, 2020 May 16]. Br J Health Psychol. 2020. https://doi.org/10.1111/bjhp.12425.
Lee SA, Mathis AA, Jobe MC, Pappalardo EA. Clinically significant fear and anxiety of COVID-19: a psychometric examination of the coronavirus anxiety scale. Psychiatry Res. 2020;290:113112.
Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med Sci Monit. 2020;26:e924609.
Li Y, Wang Y, Jiang J, et al. Psychological distress among health professional students during the COVID-19 outbreak [published online ahead of print, 2020 May 11]. Psychol Med. 2020:1–3. https://doi.org/10.1017/S0033291720001555.
Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020;287:112921.
Liu S, Liu Y, Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatry Res. 2020;289:113070.
López J, Perez-Rojo G, Noriega C, et al. Psychological well-being among older adults during the COVID-19 outbreak: a comparative study of the young-old and the old-old adults. Int Psychogeriatr. 2020;32(11):1365–70.
Ma K, Zhang Y, Hou T, Wu M, Cai W, Wen T. Investigation of physical and mental health in isolated people during the outbreak of novel coronavirus pneumonia. Chin J Clin Med. 2020;27(1):36–40.
Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among Italian Ppople during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020;17(9):3165.
McKay D, Yang H, Elhai J, Asmundson GJG. Anxiety regarding contracting COVID-19 related to interoceptive anxiety sensations: the moderating role of disgust propensity and sensitivity. J Anxiety Disord. 2020;73:102233.
Moccia L, Janiri D, Pepe M, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun. 2020;87:75–9.
Odriozola-González P, Planchuelo-Gómez Á, Irurtia MJ, de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020;290:113108.
Sanchez TH, Zlotorzynska M, Rai M, Baral SD. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS Behav. 2020;24(7):2024–32.
Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Niveles de estrés, ansiedad y depresión en la primera fase del brote del COVID-19 en una muestra recogida en el norte de España [stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain]. Cad Saude Publica. 2020;36(4):e00054020.
Özdin S, Bayrak ÖŞ. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Soc Psychiatry. 2020;66(5):504–11.
Pérez-Fuentes MDC, Molero Jurado MDM, Oropesa Ruiz NF, et al. Questionnaire on perception of threat from COVID-19. J Clin Med. 2020;9(4):1196.
Ren Y, Zhou Y, Qian W, et al. Letter to the editor "a longitudinal study on the mental health of general population during the COVID-19 epidemic in China". Brain Behav Immun. 2020;87:132–3.
Reznik A, Gritsenko V, Konstantinov V, Khamenka N, Isralowitz R. COVID-19 fear in Eastern Europe: validation of the fear of COVID-19 scale [published online ahead of print, 2020 May 12]. Int J Ment Health Addict. 2020:1–6. https://doi.org/10.1007/s11469-020-00283-3.
Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083.
Sakib N, Bhuiyan AKMI, Hossain S, et al. Psychometric validation of the Bangla fear of COVID-19 scale: confirmatory factor analysis and Rasch analysis [published online ahead of print, 2020 May 11]. Int J Ment Heal Addict. 2020:1–12. https://doi.org/10.1007/s11469-020-00289-x.
Satici B, Gocet-Tekin E, Deniz ME, Satici SA. Adaptation of the fear of COVID-19 scale: its association with psychological distress and life satisfaction in Turkey [published online ahead of print, 2020 May 8]. Int J Ment Heal Addict. 2020:1–9. https://doi.org/10.1007/s11469-020-00294-0.
Shammi M, Bodrud-Doza M, Towfiqul Islam ARM, Rahman MM. COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: a case from Bangladesh. Heliyon. 2020;6(5):e04063.
Shevlin M, Nolan E, Owczarek M, et al. COVID-19-related anxiety predicts somatic symptoms in the UK population. Br J Health Psychol. 2020;25(4):875–82.
Soraci P, Ferrari A, Abbiati FA, et al. Validation and psychometric evaluation of the Italian version of the fear of COVID-19 scale [published online ahead of print, 2020 May 4]. Int J Ment Health Addiction. 2020:1–10. https://doi.org/10.1007/s11469-020-00277-1.
Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, Gratz KL. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289:113098.
Tan W, Hao F, McIntyre RS, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92.
Tian F, Li H, Tian S, Yang J, Shao J, Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020;288:112992.
Tsipropoulou V, Nikopoulou VA, Holeva V, et al. Psychometric properties of the Greek version of FCV-19S [published online ahead of print, 2020 May 26]. Int J Ment Heal Addict. 2020:1–10. https://doi.org/10.1007/s11469-020-00319-8.
Voitsidis P, Gliatas I, Bairachtari V, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020;289:113076.
Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729.
Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–8.
Wang H, Xia Q, Xiong Z, et al. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: a web-based survey. PLoS One. 2020;15(5):e0233410.
Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2021;26(1):13–22.
Yang H, Ma J. How an epidemic outbreak impacts happiness: factors that worsen (vs. protect) emotional well-being during the coronavirus pandemic. Psychiatry Res. 2020;289:113045.
Yuan R, Xu Q-H, Xia C-C, et al. Psychological status of parents of hospitalized children during the COVID-19 epidemic in China. Psychiatry Res. 2020;288:112953.
Zhang SX, Huang H, Wei F. Geographical distance to the epicenter of Covid-19 predicts the burnout of the working population: ripple effect or typhoon eye effect? Psychiatry Res. 2020;288:112998.
Zhang SX, Wang Y, Rauch A, Wei F. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288:112958.
Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int J Environ Res Public Health. 2020;17(7):2381.
Zhou SJ, Zhang LG, Wang LL, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020;29(6):749–58.
Abdessater M, Rouprêt M, Misrai V, et al. COVID19 pandemic impacts on anxiety of French urologist in training: outcomes from a national survey. Prog Urol. 2020;30(8–9):448–55.
Ahmed MA, Jouhar R, Ahmed N, et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int J Environ Res Public Health. 2020;17(8):2821.
Alhaj AK, Al-Saadi T, Mohammad F, Alabri S. Neurosurgery residents' perspective on COVID-19: knowledge, readiness, and impact of this pandemic. World Neurosurg. 2020;139:e848–58.
Amerio A, Bianchi D, Santi F, et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Biomed. 2020;91(2):83–8.
Badahdah AM, Khamis F, Mahyijari NA. The psychological well-being of physicians during COVID-19 outbreak in Oman. Psychiatry Res. 2020;289:113053.
Bohlken J, Schömig F, Seehagen T, et al. Erfahrungen und Belastungserleben niedergelassener Neurologen und Psychiater während der COVID-19-Pandemie [experience of practice-based psychiatrists and neurologists during the COVID-19 pandemic]. Psychiatr Prax. 2020;47(4):214–7.
Cai H, Tu B, Ma J, et al. Psychological impact and coping strategies of frontline medical staff in hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monit. 2020;26:e924171.
Cai W, Lian B, Song X, Hou T, Deng G, Li H. A cross-sectional study on mental health among health care workers during the outbreak of Corona virus disease 2019. Asian J Psychiatr. 2020;51:102111.
Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–65.
Consolo U, Bellini P, Bencivenni D, Iani C, Checchi V. Epidemiological aspects and psychological reactions to COVID-19 of dental practitioners in the northern Italy districts of Modena and Reggio Emilia. Int J Environ Res Public Health. 2020;17(10):3459.
Gan X, Shi Z, Chair SY, Cao X, Wang Q. Willingness of Chinese nurses to practice in Hubei combating the coronavirus disease 2019 epidemic: a cross-sectional study. J Adv Nurs. 2020;76(8):2137–50.
Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38(3):192–5.
Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–7.
Khusid JA, Weinstein CS, Becerra AZ, et al. Well-being and education of urology residents during the COVID-19 pandemic: results of an American National Survey. Int J Clin Pract. 2020;74(9):e13559.
Mo Y, Deng L, Zhang L, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. 2020;28(5):1002–9.
Pu J, Li G, Cao L, Wu Y, Xu L. Investigation and analysis of the psychological status of the clinical nurses in a class. A hospital facing the novel coronavirus pneumonia. Chongqing Med. 2020;36:E015.
Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. 2020;3(5):e2010185.
Sahu D, Agrawal T, Rathod V, Bagaria V. Impact of COVID 19 lockdown on orthopaedic surgeons in India: a survey. J Clin Orthop Trauma. 2020;11(Suppl 3):S283–90.
Shacham M, Hamama-Raz Y, Kolerman R, Mijiritsky O, Ben-Ezra M, Mijiritsky E. COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. Int J Environ Res Public Health. 2020;17(8):2900.
Suleiman A, Bsisu I, Guzu H, et al. Preparedness of frontline doctors in Jordan healthcare facilities to COVID-19 outbreak. Int J Environ Res Public Health. 2020;17(9):3181.
Tan BYQ, Chew NWS, Lee GKH, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(4):317–20.
Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med. 2020;70(5):364–9.
Wu K, Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. 2020;26:e924085.
Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549.
Xu J, Xu Q-H, Wang C-M, Wang J. Psychological status of surgical staff during the COVID-19 outbreak. Psychiatry Res. 2020;288:112955.
Yin Q, Sun Z, Liu T, et al. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin Psychol Psychother. 2020;27(3):384–95.
Zhang C, Yang L, Liu S, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11:306.
Zhang SX, Liu J, Afshar Jahanshahi A, et al. At the height of the storm: healthcare staff's health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav Immun. 2020;87:144–6.
Zhu J, Sun L, Zhang L, et al. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front Psychiatry. 2020;11:386.
Cai X, Hu X, Ekumi IO, et al. Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. Am J Geriatr Psychiatry. 2020;28(10):1030–9.
Yuan B, Li W, Liu H, et al. Correlation between immune response and self-reported depression during convalescence from COVID-19. Brain Behav Immun. 2020;88:39–43.
Durankuş F, Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study [published online ahead of print, 2020 May 18]. J Matern Fetal Neonatal Med. 2020:1–7. https://doi.org/10.1080/14767058.2020.1763946.
Li X, Dai T, Wang H, et al. Clinical analysis of suspected COVID-19 patients with anxiety and depression. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;49(2):203–8.
Wu Y, Zhang C, Liu H, et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol. 2020;223(2):240.e1–9.
Xu H, Yang K, Yang G, et al. Explore the optimal resolvent of medical needs and mental health for patients with lung cancer during epidemic novel coronavirus pneumonia. Zhongguo Fei Ai Za Zhi. 2020;23(4):247–54.
Yassa M, Birol P, Yirmibes C, et al. Near-term pregnant women's attitude toward, concern about and knowledge of the COVID-19 pandemic. J Matern Fetal Neonatal Med. 2020;33(22):3827–34.
Büntzel J, Klein M, Keinki C, Walter S, Büntzel J, Hübner J. Oncology services in corona times: a flash interview among German cancer patients and their physicians. J Cancer Res Clin Oncol. 2020;146(10):2713–5.
Guo Q, Zheng Y, Shi J, et al. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav Immun. 2020;88:17–27.
Hao F, Tan W, Jiang L, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–6.
Hao X, Zhou D, Li Z, et al. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in Southwest China. Epilepsia. 2020;61(6):11661173.
Huang Y, Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? [retracted in: Psychol Health Med. 2020 Oct 23;:1]. Psychol Health Med. 2021;26(1):23–34.
Iasevoli F, Fornaro M, D'Urso G, et al. Psychological distress in patients with serious mental illness during the COVID-19 outbreak and one-month mass quarantine in Italy [published online ahead of print, 2020 May 19]. Psychol Med. 2020;1-3. https://doi.org/10.1017/S0033291720001841.
Jin YH, Huang Q, Wang YY, et al. Perceived infection transmission routes, infection control practices, psychosocial changes, and management of COVID-19 infected healthcare workers in a tertiary acute care hospital in Wuhan: a cross-sectional survey. Mil Med Res. 2020;7(1):24.
Ko N-Y, Lu W-H, Chen Y-L, et al. COVID-19-related information sources and psychological well-being: an online survey study in Taiwan. Brain Behav Immun. 2020;87:153–4.
Li Z, Ge J, Yang M, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020;88:916–9.
Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936.
Ni MY, Yang L, Leung CMC, et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Mental Health. 2020;7(5):e19009.
Wu W, Zhang Y, Wang P, et al. Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. J Med Virol. 2020;92(10):1962–70. https://doi.org/10.1002/jmv.25914.
Yuan S, Liao Z, Huang H, et al. Comparison of the indicators of psychological stress in the population of Hubei province and non-endemic provinces in China during two weeks during the coronavirus disease 2019 (COVID-19) outbreak in February 2020. Med Sci Monit. 2020;26:e923767.
Zhang J, Lu H, Zeng H, et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. 2020;87:49–50.
Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):242–50.
Zhu S, Wu Y, Zhu C-Y, et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav Immun. 2020;87:56–8.
Olagoke AA, Olagoke OO, Hughes AM. Exposure to coronavirus news on mainstream media: the role of risk perceptions and depression. Br J Health Psychol. 2020;25(4):865–74.
Sutin AR, Robinson E, Daly M, et al. BMI, Weight discrimination, and psychological, behavioral, and interpersonal responses to the coronavirus pandemic. Obesity (Silver Spring, Md). 2020;28(9):1590–4.
Alosaimi FD, Alawad HS, Alamri AK, et al. Patterns and determinants of stress among consultant physicians working in Saudi Arabia. Adv Med Educ Pract. 2018;9:165–74.
Balestrieri M, Isola M, Quartaroli M, Roncolato M, Bellantuono C. Assessing mixed anxiety-depressive disorder. A national primary care survey. Psychiatry Res. 2010;176(2–3):197–201.
Basta M, Karakonstantis S, Koutra K, et al. NEET status among young Greeks: association with mental health and substance use. J Affect Disord. 2019;253:210–7.
Bilgel N, Bayram N. Turkish version of the depression anxiety stress scale (DASS-42): psychometric properties. Nöropsikiyatri Arşivi. 2010;47(2):118–26.
Bonfiglio NS, Renati R, Hjemdal O, Friborg O. The resilience scale for adults in Italy: a validation study comparing clinical substance abusers with a nonclinical sample. Psychol Addict Behav. 2016;30(4):509–15.
Bottesi G, Ghisi M, Altoè G, Conforti E, Melli G, Sica C. The Italian version of the Depression Anxiety Stress Scales-21: Factor structure and psychometric properties on community and clinical samples. Compr Psychiatry. 2015;60:170–81.
Cai S, Lin H, Hu X, Cai YX, Chen K, Cai WZ. High fatigue and its associations with health and work related factors among female medical personnel at 54 hospitals in Zhuhai, China. Psychol Health Med. 2017;23(3):304–16.
Carlucci L, Watkins MW, Sergi MR, Cataldi F, Saggino A, Balsamo M. Dimensions of anxiety, age, and gender: assessing dimensionality and measurement invariance of the State-Trait for Cognitive and Somatic Anxiety (STICSA) in an Italian sample. Front Psychol. 2018;9:2345.
Carta MG, Angermeyer MC, Matschinger H, Holzinger A, Floris F, Moro MF. Perception of depressive symptoms by the Sardinian public: results of a population study. BMC Psychiatry. 2013;13:57.
Choueiry N, Salamoun T, Jabbour H, El Osta N, Hajj A, Rabbaa Khabbaz L. Insomnia and relationship with anxiety in university students: a cross-sectional designed study. PLoS One. 2016;11(2):e0149643.
Chung KF, Tso KC. Relationship between insomnia and pain in major depressive disorder: a sleep diary and actigraphy study. Sleep Med. 2010;11(8):752–8.
Dadfar M, Salabifard S, Dadfar T, Roudbari M, Safarabad NM. Validation of the Patient Health Questionnaire-2 with Iranian students. Ment Health Relig Cult. 2019;22(10):1048–56.
Dong H, Zhang Q, Sun Z, Sang F, Xu Y, et al. BMC Psychiatry. 2017;17(1):241.
Ertekin Pinar S, Duran Aksoy O, Daglar G, Yurtsal ZB, Cesur B. Effect of stress management training on depression, stress and coping strategies in pregnant women: a randomised controlled trial. J Psychosom Obstet Gynaecol. 2017;39(3):203–10.
Fleishman JA, Zuvekas SH. Global self-rated mental health: associations with other mental health measures and with role functioning. Med Care. 2007;45(7):602–9.
García-Campayo J, Zamorano E, Ruiz MA, Pérez-Páramo M, López-Gómez V, Rejas J. The assessment of generalized anxiety disorder: psychometric validation of the Spanish version of the self-administered GAD-2 scale in daily medical practice. Health Qual Life Outcomes. 2012;10:114.
Ho RT, Fong TC, Wan AH, et al. A randomized controlled trial on the psychophysiological effects of physical exercise and tai-chi in patients with chronic schizophrenia. Schizophr Res. 2016;171(1–3):42–9.
Hossain S, Anjum A, Uddin ME, Rahman MA, Hossain MF. Impacts of socio-cultural environment and lifestyle factors on the psychological health of university students in Bangladesh: a longitudinal study. J Affect Disord. 2019;256:393–403.
Huang F, Wang H, Wang Z, et al. Psychometric properties of the perceived stress scale in a community sample of Chinese. BMC Psychiatry. 2020;20(1):130.
Ivziku D, Clari M, Piredda M, De Marinis MG, Matarese M. Anxiety, depression and quality of life in chronic obstructive pulmonary disease patients and caregivers: an actor-partner interdependence model analysis. Qual Life Res. 2018;28(2):461–72.
Jeyagurunathan A, Sagayadevan V, Abdin E, et al. Psychological status and quality of life among primary caregivers of individuals with mental illness: a hospital based study. Health Qual Life Outcomes. 2017;15(1):106.
Jin H, Wu W, Zhang M. Preliminary analysis of SCL-90 assessment results of Chinese normal people. Chinese J Nerv Ment Dis. 1986;12:260–3.
Lee KS, Yoo TK, Liao L, et al. Association of lower urinary tract symptoms and OAB severity with quality of life and mental health in China, Taiwan and South Korea: results from a cross-sectional, population-based study. BMC Urol. 2017;17(1):108.
Lin R-M, Xie S-S, Yan W-J, Yan Y-W. Factor structure and psychometric properties of the insomnia severity index in mainland China. Soc Behav Personal Int J. 2018;46(2):209–18.
Liu H, Zhang H, Xiao W, et al. Scales for evaluating depressive symptoms in Chinese patients with schizophrenia. J Nerv Ment Dis. 2009;197(2):140–2.
Liu RQ, Qian Z, Trevathan E, et al. Poor sleep quality associated with high risk of hypertension and elevated blood pressure in China: results from a large population-based study. Hypertens Res. 2016;39(1):54–9.
Liu X, Wang XQ, Zhang WN, Bo QY, Zhu SY. Study on the relationship between quality of nursing professional life and depression tendency of nursing staff. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38(5):365–8.
Löwe B, Decker O, Müller S, et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. 2008;46(3):266–74.
Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the patient health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1–2):86–95.
Lu S, Hu S, Guan Y, et al. Measurement invariance of the Depression Anxiety Stress Scales-21 across gender in a sample of Chinese university students. Front Psychol. 2018;9:2064.
Lu W, Bian Q, Wang W, Wu X, Wang Z, Zhao M. Chinese version of the Perceived Stress Scale-10: a psychometric study in Chinese university students. PLoS One. 2017;12(12):e0189543.
Paparrigopoulos T, Tzavara C, Theleritis C, Psarros C, Soldatos C, Tountas Y. Insomnia and its correlates in a representative sample of the Greek population. BMC Public Health. 2010;10:531.
Pereira-Lima K, Loureiro SR. Burnout, anxiety, depression, and social skills in medical residents. Psychol Health Med. 2014;20(3):353–62.
Ramón-Arbués E, Martínez Abadía B, Granada López JM, et al. Conducta alimentaria y su relación con el estrés, la ansiedad, la depresión y el insomnio en estudiantes universitarios [Eating behavior and relationships with stress, anxiety, depression and insomnia in university students.]. Nutr Hosp. 2019;36(6):1339–45.
Sasaki N, Imamura K, Thuy TTT, et al. Validation of the Job Content Questionnaire among hospital nurses in Vietnam. J Occup Health. 2019;62(1):e12086.
Schmidt RE, Cullati S, Mostofsky E, et al. Healthcare-related regret among nurses and physicians is associated with self-rated insomnia severity: a cross-sectional study. PLoS One. 2015;10(10):e0139770.
Sinclair SJ, Siefert CJ, Slavin-Mulford JM, Stein MB, Renna M, Blais MA. Psychometric evaluation and normative data for the depression, anxiety, and stress scales-21 (DASS-21) in a nonclinical sample of U.S. adults. Eval Health Prof. 2012;35(3):259–79.
Wang K, Shi HS, Geng FL, et al. Cross-cultural validation of the depression anxiety stress Scale-21 in China. Psychol Assess. 2016;28(5):e88–100.
Wang W, Bian Q, Zhao Y, et al. Reliability and validity of the Chinese version of the patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36(5):539–44.
Wang WL, Zhou YQ, Chai NN, Li GH, et al. Sleep disturbance and quality of life in clinically stable inpatients with schizophrenia in rural China. Qual Life Res. 2020;29(10):2759–68.
Wang X, Wang X, Ma H. Handbook of Mental Health Assessment Scale. Chin Ment Health J. 1999;13(1):31–5.
Wang Y, Yang X, Song X, et al. Co-treatment of buspirone with atypical antipsychotic drugs (AAPDs) improved neurocognitive function in chronic schizophrenia. Schizophr Res. 2019;209:135–40.
Yang X, Zhang P, Zhao J, et al. Confucian culture still matters: the benefits of Zhongyong thinking (doctrine of the mean) for mental health. J Cross-Cult Psychol. 2016;47(8):1097–113.
Yıldırım A, Boysan M, Kefeli MC. Psychometric properties of the Turkish version of the depression anxiety stress Scale-21 (DASS-21). Br J Guid Couns. 2018;46(5):582–95.
Yu B, Gu Y, Bao X, et al. Distinct associations of computer/mobile devices use and TV watching with depressive symptoms in adults: a large population study in China. Depress Anxiety. 2019;36(9):879–86.
Zhou J, Yang Y, Qiu X, et al. Relationship between anxiety and burnout among Chinese physicians: a moderated mediation model. PLoS One. 2016;11(8):e0157013.
Kunzler AM, Helmreich I, Chmitorz A, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst Rev. 2020;7:CD012527.
Salazar de Pablo G, Vaquerizo-Serrano J, Catalan A, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J Affect Disord. 2020;275:48–57.
Bonanno GA, Mancini AD. Beyond resilience and PTSD: mapping the heterogeneity of responses to potential trauma. Psychol Trauma Theory Res Pract Policy. 2012;4:74–83.
Mancini AD. Heterogeneous mental health consequences of COVID-19: costs and benefits. Psychol Trauma Theory Res Pract Policy. 2020;12(S1):S15–6.
Ahrens KF, Neumann RJ, Kollmann B, et al. Differential impact of COVID-related lockdown on mental health in Germany. World Psychiatry. 2021;20:1.
Veer IM, Riepenhausen A, Zerban M, et al. Psycho-social factors associated with mental resilience in the Corona lockdown. 2020. https://psyarxiv.com/4z62t/. Accessed 4 Nov 2020.
Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the patient health questionnaire (PHQ-9). J Affect Disord. 2004;81(1):61–6.
Duffy FF, Chung H, Trivedi M, Rae DS, Regier DA, Katzelnick DJ. Systematic use of patient-rated depression severity monitoring: is it helpful and feasible in clinical psychiatry? Psychiatr Serv. 2008;59(10):1148–54.
Erskine HE, Moffitt TE, Copeland WE, et al. A heavy burden on young minds: the global burden of mental and substance use disorders in children and youth. Psychol Med. 2015;45(7):1551–63.
IntHout J, Ioannidis JPA, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6(7):e010247.
Acknowledgements
We appreciate the contributions of Prof Raffael Kalisch PhD to the discussion of the findings of our review.
Funding
The CEOsys and the egePan project are funded under a scheme issued by the Network of University Medicine (Nationales Forschungsnetzwerk der Universitätsmedizin (NUM)) by the Federal Ministry of Education and Research of Germany (Bundesministerium für Bildung und Forschung (BMBF); Grant number 01KX2021). The Project RESPOND is funded by the EU RIA-call H2020-SC1-PHE-CORONAVIRUS-2020-2-RTD (Grant number 101016127). The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
AMK, NR, JSW, and KL designed the study. NR and LG, respectively, assessed study eligibility; KL was consulted in case of any disagreements. NR and LG extracted and analyzed data for Table 1, with KL being consulted in case of any disagreements. AMK, NR, and GS designed the statistical analyses. AMK and NR analyzed data for Tables 2, 3, 4 and 5 based on pairwise meta-analyses (including subgroup and sensitivity analyses) and the narrative synthesis of risk/protective factors. GS and HB reviewed the statistical analyses. KL monitored the review process. All authors contributed to the interpretation of the results, with special expertise provided in the field of resilience research (AMK, OT, KL), public health (MC, ER), and evidence-based medicine (CS, JJM). AMK wrote the first draft of the manuscript with input and subsequent edits by all authors. KL is the guarantor. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
LG, JSW, and GS have no conflicts of interest to disclose. AMK, NR, OT, MC, ER, HB, CS, JJM, and KL report grants from the Federal Ministry of Education and Research (BMBF), Germany, during the conduct of the study. JJM reports grants from the Federal Ministry of Health (BMG), Germany, outside of the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Methods of the systematic review with meta-analyses. eTable 1. MOOSE Checklist. eTable 2. Differences between protocol and review. eMethods 1. Search strategies for SARS-CoV-2 (‘pandemic’) studies. eMethods 2. Search strategy for prepandemic comparative studies. eTable 3. Eligibility criteria for SARS-CoV-2 pandemic studies. eTable 4. Eligibility criteria for prepandemic comparative studies. eTable 5. Eligibility criteria for pairwise meta-analyses. eTable 6. Customized data extraction sheet. eTable 7. Modified quality assessment tool. eTable 8. Rating of comparability between pandemic and prepandemic comparative studies. eMethods 3. Further methodological details of this systematic review and meta-analyses.
Additional file 2:
Results of the systematic review with meta-analyses. eTable 9. Details on number of included (pandemic and comparative) studies. eTable 10. Study characteristics of the prepandemic comparative studies. eTable 11. Cut-off values reported in included pandemic studies. eResults 1. Forest plots of main analyses. eTable 12. Quality assessment of included pandemic studies. eTable 13. Assessment of level of comparability between pandemic and prepandemic comparative studies. eResults 2. Forest plots of sensitivity analyses. eResults 3. Detailed results of subgroup analyses. eTable 14. Risk factors in the general population, healthcare workers, and patients. eTable 15. Protective factors in the general population, healthcare workers, and patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kunzler, A.M., Röthke, N., Günthner, L. et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health 17, 34 (2021). https://doi.org/10.1186/s12992-021-00670-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12992-021-00670-y