Abstract
Background
Sex disparities in blood pressure and anthropometry may account for differences in cardiovascular (CV) risk burden with advancing age; modulated by ethnic variability. We explored trajectories of blood pressures (BPs) and anthropometric indices with age on the basis of sex in an urban Nigerian population.
Methods
We conducted a secondary analysis on data from 5135 participants (aged 16–92 years; 2671(52%) females) from our population-based cross-sectional study of BP profiles. We utilized the WHO STEPS and standardized methods for documenting BPs, body mass index (BMI) and waist circumference (WC). Data was analyzed using Analysis of variance (ANOVA), Spearman correlation analysis and mean difference in variables (with 95% confidence interval). We explored the influence of age and sex on BP profiles and specific anthropometric indices using generalized regression analysis.
Results
In those aged 15–44 years, males had significantly higher systolic BP (SBP) and pulse pressure (PP). However, mean SBP and PP rose more steeply in females from 25 to 34 years, intersected with that of males from 45 to 54 years and remained consistently higher. Difference in mean BPs (95% Confidence Interval) (comparing < and > 45 years) was higher in females compared to males for SBP (17.4 (15.8 to 19.0) v. 9.2 (7.7 to 10.7), DBP (9.0 (7.9 to 10.1) v. 7.8 (6.7 to 8.9)), and PP (8.4 (7.3 to 9.5) v. 1.4 (0.3 to 2.5)). Females had significantly higher BMI and WC across all age groups (p < 0.001). Age more significantly correlated with BPs, BMI and WC in females. Interaction models revealed that SBP was significantly predicted by age category in females from (15–54 years), while DBP was only significantly predicted by age in the 15–34-year category (p < 0.01). BMI and WC were significantly predicted by age only in the 25–34-year category in females, (p < 0.01).
Conclusions
Our population demonstrates sex disparity in trajectories of SBP, PP, BMI and WC with age; with steeper rise in females. There is a need to focus on CV risk reduction in females, starting before, or during early adulthood.
Similar content being viewed by others
Introduction
Blood pressure and body adiposity are broadly recognized determinants of cardiovascular disease (CVD) risk [1, 2]. Reported variations in cardiovascular outcomes in men versus women have previously been attributed to sex-specific disparities in body adiposity and blood pressure trajectories, and are exemplified by differences in incidence, prevalence, disease patterns and profiles, and mortality [3,4,5,6]. As examples, high SBP has a higher global attributable disability-adjusted life years (DALYs) for females compared to males and pulse pressure (which is also associated with subclinical CVD) is modulated by sex [8]. Beyond the physiological and hormonal import of sex differences on vascular function, intersecting social factors such as disparate health-seeking behavior, access to healthcare, environmental and lifestyle dissimilarities may be contributory [9,10,11].
Any sex disparity in CV risk and outcomes deserves recognition due to the implications for risk management, surveillance and development of sex-specific guidelines guided by evidence [3,4,5, 12,13,14]. Although sex specific blood pressure trajectories and the implied CVD related risks have been reported, these are subject to wide racial, ethnic, geographic and cultural differences which are critical in planning interventions to reduce CVD-related adverse outcomes [8, 15,16,17]. The steeper rise in blood pressure reported to occur among women has shown variations in age of onset across populations [4, 8, 18, 19]. Furthermore, although measures of body adiposity (BMI and WC) have been independently associated with CVD risk; age, sex and ethnic variability have also been reported with these measures [20,21,22,23,24].
There is increasing incidence and prevalence of CV diseases in sub-Saharan Africa (SSA) with lower age of onset, different clinical profile and worse outcomes, which makes it imperative to investigate the pattern of involvement of known modifiable and non-modifiable risk factors in local contexts. This data is useful for informing policy and directing health system planning especially as it regards to women’s health. Data on BP trajectory as well as sex dissimilarities in the trajectory of CV risk factors in sub-Saharan Africa is limited [25,26,27,28,29].
We thus set out to conduct a sex-based comparison of the correlation and association between age and blood pressures as well as specific anthropometric indices (waist circumference and BMI) from early adulthood.
Methods
We conducted a secondary analysis of the data from a cross-sectional, community-based hypertension prevalence study in Nigerians aged 16 years and above, residing in an urban area of Lagos state, Nigeria and whose methodology has previously been described [30]. To summarize, between May and December 2017 after obtaining ethics approval from the Lagos University Teaching Hospital Health Research and Ethics Committee, we carried out a cross-sectional prevalence study of blood pressure profiles: using a stratified multistage random sampling approach we carried out a door-to-door survey of 200 households randomly selected from 8 of 16 mixed income densely populated local government areas of the state [30]. As previously described, we utilized the World Health Organizations STEPwise approach to chronic disease risk factor surveillance (WHO STEPS) [30, 31]. Written informed consent was also obtained from the head of household and/or legal guardian, and from each participating individual. The study protocol was carried out in accordance with the Declaration of Helsinki.
Blood pressure was measured using an appropriately calibrated Omron® sphygmomanometer, with the average of the last two (of three) readings taken while seated utilized for the study [30]. Anthropometric indices i.e., weight, height, waist circumference, hip circumference and waist–hip ratio were all measured according to standard protocol and this has been previously documented [32,33,34] Data for 5135 community-dwelling participants were included in this secondary analysis and the variables of interest include age (years), sex, systolic BP (mmHg), diastolic BP (mmHg), BMI (kg/m2) and waist circumference (cm). Pulse pressure (mmHg) was derived as the difference between systolic BP and diastolic BP (systolic BP minus diastolic BP).
Data analysis
Data was analyzed using IBM ® SPSS ® version 24. Continuous variables are presented as mean ± standard deviation (SD) and inter-group comparisons were explored using Analysis of Variance (ANOVA). Correlation analysis (Spearman’s) was conducted to explore the association between age and systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse pressure (PP), body mass index (BMI), and waist circumference (WC) in males compared with females. Based on the age at which the male and female SBP and PP intercepted each other (45 years), the mean difference in variables between those aged < and ≥ 45 years was computed using Medcalc® open-source software, and presented as mean difference (95% confidence interval) [35].
Generalized linear regression was used to analyze the influence of age (as age categories) and sex (female as reference category) as factors on SBP, DBP, PP (with BMI and WC added as co-variates). This was carried out as individual main effects as well as interaction term (age category*sex). Generalized linear regression was also used to analyze the influence of age (as age categories) and sex (female as reference category) on WC and BMI (also analyzing main effects and interaction of age category*sex). The regression models out-performed the null hypothesis as the omnibus test was significant for all (p = 0.000) and the models were all a good fit to the data as deviance (goodness-of-fit test) was < 2.5 for all models (0.02–1.58). Statistical significance was set at the level of p < 0.05.
Results
There were 5135 urban community-dwelling adults (age range 16 to 92 years) comprising 2671 (52.0%) females and 2464 (48.0%) males. Table 1 shows the characteristics of the study population, including a comparison of blood pressure and anthropometric indices. We dichotomized age at 45 years based on the observation that the sex-based intercept for SBP trajectory with age was in that age stratum, (Fig. 1). There was no sex difference in the mean ages of the population, nor of the proportion of adults < or ≥ 45 years based on gender (p = 0.24). Males had significantly higher SBP and PP compared to females only below 45 years (p < 0.001). All the mean BP measures (SBP, DBP, and PP) were higher in women aged ≥ 45 years although the difference did not reach statistical significance. Diastolic blood pressure was comparable irrespective of sex in the age strata. BMI and WC were significantly higher in females overall and in the age categories < 45 and ≥ 45 years (p < 0.001). The mean differences in the measured variables between age categories < 45 and ≥ 45 years in both sexes are also shown in Table 1, and indicate that females compared to males, had consistently greater positive differences from age categories < 45 to ≥ 45 years for all the variables.
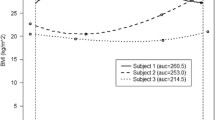
The blood pressures and anthropometric indices trajectories with age in males and females are illustrated in Table 2 and Fig. 1. As shown in Table 3, in correlation analysis, all SBP, DBP, BMI and WC exhibited significant positive correlation with age in both sexes (p < 0.001), whereas PP correlated significantly with age only in females. There was a stronger correlation with age for all the parameters in females compared to males.
Trajectory of blood pressure with age based on sex
Table 2 and Fig. 1 show the trends in mean SBP and DBP by age category for both sexes. From the age group 25 to 34 years, SBP demonstrated a steeper rise in in females, intercepting and becoming higher than in men from the age category 45 to 54 years upwards. From age 65 years there was a decline in the SBP, albeit more obvious in males. The upward trajectory in DBP was parallel in both sexes, with nearly overlapping mean values (p < 0.05). Pulse pressure had a similar course with SBP (Table 2).
Trajectory of BMI and WC with age group based on sex
The trend of association between anthropometric indices and age in males and females are displayed in Table 2 and Fig. 2. In both sexes there was a steady rise in anthropometric indices with age, with decline in mean BMI and waist circumference observed from age categories 45 to 54 years and 65 to 74 years respectively. The decline in BMI with age was steeper in males than in females.
Trajectory of association between anthropometric indices (BMI and WC) and age based on sex. Line graphs depicting the trend of association between anthropometric indices and age in females (red) and males (blue): A – BMI; B – waist circumference (WC). Both BMI and WC were higher in females compared to males across all age categories, with significant differences across all age groups except ≤ 24 and ≥ 75 (p > 0.05)
Predictors of BP and anthropometric profiles and their interactive effects
Generalized linear regression results are displayed in Additional file 1: Table 1. For models involving BP profiles (SBP, DBP and PP), the ≥ 75-year category was redundant. All variables in the model had significant Type III effects (sex, age category, BMI and WC). The interaction model (interaction term age category* sex) revealed that SBP was significantly predicted by age category in females from ages 15–54 years while DBP was only significantly predicted by age category in females in the 15–34-year range (p < 0.01). BMI and WC were significantly predicted by age category in females, only in the 25–34-year category (p < 0.01). (Additional file 1: Table 1).
Discussion
The impetus for this study was the reported sex disparity in attributable risk for adverse cardiovascular outcomes (with a higher burden in females) from other populations. Our objective was to gain insight into the trajectories of blood pressure and anthropometric indices with increasing age based on gender in our black African population.
With respect to blood pressures, we observed that, compared to males, SBP was initially lower in females at adolescence, but rose steeply from age group 25–34, intersected with and became higher than males at 45–54 years, only declining in both sexes from age bracket 65–74 years (but with a more appreciable decline in men). Diastolic BP had similar course in both sexes up to age 55–64 group, when it subsequently declined in men but continued to rise in women till age 65–74 where a steep decline was observed to parallel the values for men by age ≥ 75 years. The rise in pulse pressure also occurred at an earlier age in females (25–34 v. 35–44), intersected at 45–54 years, continuing to rise in females while declining in men from age ≥ 65 years.
Our findings corroborate those from other populations indicating that SBP and DBP are lower in females in early life, subsequently exhibiting a steeper and more rapid rise in SBP with advancing age, switching to become higher at about middle age, whereas the trajectory of DBP remains largely similar in both sexes [18, 36] This pattern suggests a greater cardiovascular risk in women from middle age, coinciding with the menopausal age in many populations [1, 7, 8, 18, 19, 37, 38]. The consequent loss of the protective effect of oestrogen at menopause with resultant increased renal sodium retention, loss of endothelial dependent nitric oxide production, increase in plasma rennin and angiotensin converting enzyme activity may partially account for the observation [18]. However, we postulate that the higher risk actually precedes menopause based on our observation (and that of others), that women actually begin to exhibit a sharper and consistent rise in SBP from about the age of 25 years (at least 2 decades before typical menopausal age), and at a rate steeper than that observed from middle age [36]. This observation is important as it is well documented that each 20 mmHg increase in SBP is associated with a doubling in the risk of adverse CV events [39]. It would therefore appear that our population of black African women actually bear a greater CV risk at a much earlier age, and is consistent with previous reports that sub-Saharan Africans have a lower age of onset and different clinical profile of cardiovascular diseases [28, 29]. Existing estimates of CVD risk from most sub-Saharan African countries are premised on sparse, sometimes methodologically flawed primary studies, and probably represent an underestimation of the true burden in both sexes, with the potential for greater misrepresentation of females. This would invariably misdirect surveillance and the timing of gender specific interventions if the surge in SBP observed earlier in life in females is not taken into consideration. More so, as previously reported, the steady increase in SBP (hence the CV risk) is sustained throughout life in females [36]. However, in the European cohorts aged 19–78 years included in the MORGAM (MOnica, Risk, Genetics, Archiving, and Monograph) project, the relative superiority of SBP over DBP as a risk factor for fatal and non-fatal stroke risk which was consistent and independent of other cardiovascular risk factors, became apparent at age 47 years, and was significant from age 62 years [40]. The study also demonstrated a significant effect modification of the SBP-stroke mortality association by sex in which the positive association between SBP and stroke mortality was present in both sexes but did not reach significance in women before middle age (implying a pre-menopausal hormonal protection up to age 50 or around menopause) in that population [40, 41].
The pulse pressure trajectory reported in our study is similar to that for SBP and is in keeping with previous studies [8, 36]. Pulse pressure is independently associated with subclinical cardiovascular diseases, albeit with sex variability (increased tendency in females) in the strength of this association [8, 36]. For example, increased pulse pressure is more strongly associated with increased left ventricular mass index, increased prevalence of, and poorer outcome from heart failure with preserved ejection fraction in females [8, 36, 42].
The GBD Study 2019 reiterates the disturbing burden of metabolic risk factors including BMI as leading causes of DALYs and contributors to mortality globally, with considerable heterogeneity in the risks and trends between countries [1]. High BMI is one of three risk factors that accounted for > 1% DALYs in addition to increasing in exposure by more than 1% per annum [1]. The higher BMI and WC in black African females in this study, consistent across all age groups, corroborate reports from several other studies [43,44,45]. However, it differs from some studies conducted amongst predominantly Caucasian and Asian populations where men had higher waist circumference, and in keeping with recognized ethnic and regional variability in sex distribution of abdominal adiposity [43,44,45,46,47,48]. Black women reportedly have a greater shift in waist circumference with age and an increased tendency to truncal obesity compared to other ethnicities and men [45]. Both increasing BMI and WC are independently associated with increased risk of hypertension and cardiovascular diseases and may contribute to the steady rise in blood pressure with age observed in this and other studies [21, 22, 49,50,51]. Sexual dimorphism in the pathogenesis of obesity-related hypertension has been associated with increased atherogenic lipid profile and induction of metabolic disorders in women but not in men [52]. This may further widen the gender divide culminating in the tendency towards a worse CV risk profile and potential for worse CV outcomes in women, even starting at an earlier age.
We acknowledge the limitations of our study in being largely descriptive and cross-sectional data for which only one set of measures (blood pressure and anthropometry) were obtained, and did not include any longitudinal outcome data to test the impact of our observation. In deriving conclusions regarding the implications of our findings, we have relied on existing literature that indicate the strength of association between high systolic blood pressure and anthropometric indices (e.g. BMI) and adverse CV outcome, such as that from the GBD 2019 study. The smaller numbers of participants at the highest extremes of age in this study (≥ 75 years) may also have introduced some bias into the data in that subgroup for both sexes. The numbers in this study represent the small proportion of the general population in the country (2.74%) aged ≥ 65 years according to estimates from the United Nations Population Divisions’ World Population prospects (2019 revision) [53]. Otherwise, the robust sample size and the population source of our data with adequate representation of other age strata may however attenuate this limitation, although we suggest longitudinally studying a larger and nationally representative sample of the population as well as the older elderly in the future, given improvements in life expectancy that are expanding the population representation of that age group. Our primary data collection did not include laboratory-based assessments and, although we appreciate the import of exploring other metabolic variables that can further substantiate cardiovascular risk; this consideration was precluded by funding and logistic limitations.
Conclusions
The trajectory of SBP, PP, and anthropometric indices of obesity and abdominal adiposity documented in our study, and taken together with existing literature are persuasive indicators of the need to focus on women’s cardiovascular risk modification, starting in early adolescence through to the postmenopausal period. We join previous researchers to advocate for sex specific intervention strategies to modify the trend [3,4,5, 12,13,14]. In black African females in our population, we propose population-level primordial prevention policies and projects aimed at increasing awareness on the specific risk of women, improving access to information regarding healthy lifestyle choices from early life, and enabling implementation of evidence-based measures such as dietary choices and exercise. In addition, primary prevention through policies and programs that improve access to documenting and tracking women’s cardiovascular health indices and outcomes across the lifespan, integrated into existing women’s health or female-predominant user programs (such as maternity and childhood immunization) would be beneficial.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- BP:
-
Blood pressure
- BMI:
-
Body mass index
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- DALYs:
-
Disability-adjusted life years
- GBD:
-
Global burden of diseases
- IBM:
-
International business machine corporations
- LUTH-HREC:
-
Ethics approval was obtained from the Lagos university teaching hospital health research ethics committee.
- PP:
-
Pulse pressure
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- SPSS:
-
Statistical package for social sciences
- SSA:
-
Sub-Saharan Africa
- WC:
-
Waist circumference
- WHO STEPS:
-
World Health Organizations STEPwise approach to chronic disease risk factor surveillance
References
Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1223–49.
Cercato C, Fonseca FA. Cardiovascular risk and obesity. Diabetol Metab Syndr. 2019;11(1):74.
Eaton CB, Pettinger M, Rossouw J, Martin LW, Foraker R, Quddus A, et al. Risk factors for incident hospitalized heart failure with preserved versus reduced ejection fraction in a multiracial cohort of postmenopausal women. Circ Hear Fail. 2016;9(10): e002883.
Dean J, Dela Cruz S, Mehta PK, Merz CNB. Coronary microvascular dysfunction: sex-specific risk, diagnosis, and therapy. Nat Rev Cardiol. 2015;12(7):406–14.
Beale AL, Meyer P, Marwick TH, Lam CSP, Kaye DM. Sex differences in cardiovascular pathophysiology. Circulation. 2018;138(2):198–205.
Song J-J, Ma Z, Wang J, Chen L-X, Zhong J-C. Gender differences in hypertension. J Cardiovasc Transl Res. 2020;13(1):47–54.
Strandberg TE, Pitkala K. What is the most important component of blood pressure: systolic, diastolic or pulse pressure? Curr Opin Nephrol Hypertens. 2003;12(3):293–7.
Winston GJ, Palmas W, Lima J, Polak JF, Bertoni AG, Burke G, et al. Pulse pressure and subclinical cardiovascular disease in the multi-ethnic study of atherosclerosis. Am J Hypertens. 2013;26(5):636–42.
Magodoro IM, Feng M, North CM, Vořechovská D, Kraemer JD, Kakuhikire B, et al. Female sex and cardiovascular disease risk in rural Uganda: a cross-sectional, population-based study. BMC Cardiovasc Disord. 2019;19(1):96.
O’Neil A, Scovelle AJ, Milner AJ, Kavanagh A. Gender/sex as a social determinant of cardiovascular risk. Circulation. 2018;137(8):854–64.
Goossens GH, Jocken JWE, Blaak EE. Sexual dimorphism in cardiometabolic health: the role of adipose tissue, muscle and liver. Nat Rev Endocrinol. 2021;17(1):47–66.
Regitz-Zagrosek V. Therapeutic implications of the gender-specific aspects of cardiovascular disease. Nat Rev Drug Discov. 2006;5(5):425–39.
Cifkova R, Pitha J, Krajcoviechova A, Kralikova E. Is the impact of conventional risk factors the same in men and women? Plea for a more gender-specific approach. Int J Cardiol. 2019;286:214–9.
Calabrò P, Niccoli G, Gragnano F, Grove EL, Vergallo R, Mikhailidis DP, et al. Are we ready for a gender-specific approach in interventional cardiology? Int J Cardiol. 2019;286:226–33.
Lackland DT. Racial differences in hypertension: implications for high blood pressure management. Am J Med Sci. 2014;348(2):135–8.
Higginbottom GMA. “Pressure of life”: ethnicity as a mediating factor in mid-life and older peoples’ experience of high blood pressure. Sociol Heal Illn. 2006;28(5):583–610.
Wang X, Poole JC, Treiber FA, Harshfield GA, Hanevold CD, Snieder H. Ethnic and gender differences in ambulatory blood pressure trajectories. Circulation. 2006;114(25):2780–7.
Oparil S, Miller AP. Gender and blood pressure. J Clin Hypertens. 2005;7(5):300–9.
de Kat AC, Dam V, Onland-Moret NC, Eijkemans MJC, Broekmans FJM, van der Schouw YT. Unraveling the associations of age and menopause with cardiovascular risk factors in a large population-based study. BMC Med. 2017;15(1):2.
Dua S, Bhuker M, Sharma P, Dhall M, Kapoor S. Body mass index relates to blood pressure among adults. N Am J Med Sci. 2014;6(2):89–95.
Drøyvold WB, Midthjell K, Nilsen TIL, Holmen J. Change in body mass index and its impact on blood pressure: a prospective population study. Int J Obes. 2005;29(6):650–5.
Islam MT, Möller J, Zhou X, Liang Y. Life-course trajectories of body mass index and subsequent cardiovascular risk among Chinese population. Ikeda N, editor. PLoS One. 2019;14(10):e0223778.
Reas DL, Nygård JF, Svensson E, Sørensen T, Sandanger I. Changes in body mass index by age, gender, and socio-economic status among a cohort of Norwegian men and women (1990–2001). BMC Public Health. 2007;7:269.
Albrecht SS, Gordon-Larsen P. Ethnic differences in body mass index trajectories from adolescence to adulthood: a focus on Hispanic and Asian subgroups in the United States. Votruba SB, editor. PLoS One. 2013;8(9):e72983.
Price AJ, Crampin AC, Amberbir A, Kayuni-Chihana N, Musicha C, Tafatatha T, et al. Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-Saharan Africa: a cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes Endocrinol. 2018;6(3):208–22.
Agyemang C, Boatemaa S, Frempong GA, de-Graft Aikins A. Obesity in Sub-Saharan Africa. In: Ahema R, editor. Metabolic Syndrome. Cham: Springer International Publishing; 2015. p. 1–13.
Chukwuonye II, Chuku A, John C, Ohagwu KA, Imoh ME, Isa SE, et al. Prevalence of overweight and obesity in adult Nigerians - a systematic review. Diabetes Metab Syndr Obes. 2013;6:43–7.
Cappuccio FP, Miller MA. Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Intern Emerg Med. 2016;11(3):299–305.
Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, Laurence C, Adebamowo C, Ajayi I, et al. The burden of hypertension in sub-Saharan Africa: a four-country cross sectional study. BMC Public Health. 2015;15(1):1211.
Okubadejo NU, Ozoh OB, Ojo OO, Akinkugbe AO, Odeniyi IA, Adegoke O, et al. Prevalence of hypertension and blood pressure profile amongst urban-dwelling adults in Nigeria: a comparative analysis based on recent guideline recommendations. Clin Hypertens. 2019;25(1):7.
World Health Organization. STEPwise approach to chronic disease risk factor surveillance, World Health Organization 2009. http://www.who.int/chp/ steps/ reports/en/index.html. Accessed 18 June 2018.
World Health Organisation (WHO). WHO|waist circumference and waist–hip ratio. Report of a WHO Expert Consultation. Geneva, 8–11 December 2008. 2008;8.
Garrow JS, Webster J. Quetelet’s index (W/H2) as a measure of fatness. Int J Obes. 1985;9(1):147.
Adegoke O, Ozoh OB, Odeniyi IA, Bello BT, Akinkugbe AO, Ojo OO, et al. Prevalence of obesity and an interrogation of the correlation between anthropometric indices and blood pressures in urban Lagos, Nigeria. Sci Rep. 2021;11(1):3522.
Medcalc® open source software. http://www.medcalc.org/calc/comparison_of_means.php. Assessed 11 June 2021.
Ji H, Kim A, Ebinger JE, Niiranen TJ, Claggett BL, Bairey Merz CN, et al. Sex differences in blood pressure trajectories over the life course. JAMA Cardiol. 2020;5(3):255.
Anolue FC, Dike E, Adogu P, Ebirim C. Women’s experience of menopause in rural communities in Orlu. Eastern Nigeria Int J Gynecol Obstet. 2012;118(1):31–3.
OlaOlorun F, Lawoyin T. Age at menopause and factors associated with attainment of menopause in an urban community in Ibadan. Nigeria Climacteric. 2009;12(4):352–63.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–52.
Vishram JKK, Borglykke A, Andreasen AH, Jeppesen J, Ibsen H, Jørgensen T, et al. Impact of age on the importance of systolic and diastolic blood pressures for stroke risk. Hypertension. 2012;60(5):1117–23.
Vishram JKK, Borglykke A, Andreasen AH, Jeppesen J, Ibsen H, Jørgensen T, et al. Do other cardiovascular risk factors influence the impact of age on the association between blood pressure and mortality? The MORGAM Project J Hypertens. 2014;32(5):1025–33.
Beale AL, Nanayakkara S, Kaye DM. Impact of sex on ventricular-vascular stiffness and long term outcomes in heart failure with preserved ejection fraction: TOPCAT trial substudy. J Am Heart Assoc. 2019. https://doi.org/10.1161/JAHA.119.012190.
Ramsay M, Crowther NJ, Agongo G, Ali SA, Asiki G, Boua RP, et al. Regional and sex-specific variation in BMI distribution in four sub-Saharan African countries: the H3Africa AWI-Gen study. Glob Health Action. 2018;11(Suppl 2):1556561.
Stevens J, Katz EG, Huxley RR. Associations between gender, age and waist circumference. Eur J Clin Nutr. 2010;64(1):6–15.
Beydoun MA, Wang Y. Gender-ethnic disparity in BMI and waist circumference distribution shifts in US adults. Obesity. 2009;17(1):169–76.
Lahti-Koski M, Harald K, Männistö S, Laatikainen T, Jousilahti P. Fifteen-year changes in body mass index and waist circumference in Finnish adults. Eur J Cardiovasc Prev Rehabil. 2007;14(3):398–404.
Johnson W, Norris T, Hamer M. Secular changes in mid-adulthood body mass index, waist circumference, and low HDL cholesterol between 1990, 2003, and 2018 in Great Britain. Eur J Clin Nutr. 2021;75(3):539–45.
Zhai Y, Fang HY, Yu WT, Yu DM, Zhao LY, Feng LX, et al. Changes in waist circumference and abdominal obesity among Chinese adults over a ten-year period. Biomed Env Sci. 2017;30(5):315–22.
Yang Y, Dugué P-A, Lynch BM, Hodge AM, Karahalios A, MacInnis RJ, et al. Trajectories of body mass index in adulthood and all-cause and cause-specific mortality in the Melbourne collaborative cohort study. BMJ Open. 2019;9(8): e030078.
Wang L, Lee Y, Wu Y, Zhang X, Jin C, Huang Z, et al. A prospective study of waist circumference trajectories and incident cardiovascular disease in China: the Kailuan Cohort Study. Am J Clin Nutr. 2021;113(2):338–47.
Emiloju OC, Chinedu SN, Onuoha MC, Iheagwam FN. Association between gender, age, body weight and hypertension in Nigeria. FASEB J. 2017;31:1011–20.
Kaneva AM, Bojko ER. Sex differences in the association between obesity and hypertension. Arch Physiol Biochem. 2021. https://doi.org/10.1080/13813455.2020.1861027.
World Bank. Population ages 65 and above (% of total population) – Nigeria. https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?view=chart&locations=NG. Accessed 30 November 2019.
Acknowledgements
Not applicable
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
O.A., O.O.O., O.B.O. and N.U.O. contributed to the conceptualization, design, data analysis and initial draft of the manuscript. O.A. O.O.O. and N.U.O. analyzed and interpreted the data and prepared the manuscript. A.O.A., I.A.O., B.T.B. and O.P.A. contributed to the conceptualization, design, data gathering and data management. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Lagos University Teaching Hospital Health, Research Ethics Committee (LUTH -HREC). We obtained written informed consent from head of household and/ or legal guardian, as well as from each participating individual. The study protocol was carried out in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
Generalized linear regression models using age and sex to predict trend in blood pressure profiles and anthropometric indices.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Adegoke, O., Ojo, O.O., Ozoh, O.B. et al. The impact of sex on blood pressure and anthropometry trajectories from early adulthood in a Nigerian population: insights into women’s cardiovascular disease risk across the lifespan. BMC Women's Health 22, 303 (2022). https://doi.org/10.1186/s12905-022-01888-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-01888-7