Abstract
Purpose
To evaluate the efficacy of cytokine-induced killer (CIK) cell therapy in the treatment of hepatocellular carcinoma.
Materials and methods
Randomized phase II and III trials on CIK cell-based therapy were identified by electronic searches using a combination of "hepatocellular carcinoma" and "cytokine-induced killer cells".
Results
The analysis showed significant survival benefit (one-year survival, p < 0.001; two-year survival, p < 0.001; median overall survival, p < 0.001) in favor of CIK-based therapy. Comparison of CIK group versus non-CIK group resulted in a significantly prolonged progression-free survival (PFS) (p < 0.01). A favored disease control rate (DCR) and overall response rate (ORR) were also observed in patients receiving CIK cell therapy (p < 0.01). Meanwhile, patients in the CIK group showed better quality of life (QoL), diminished HBV-DNA content and AFP level (p < 0.01). Comparing T-lymphocyte subsets in peripheral blood, the analysis showed the ratio of CD3+, CD4+, CD4+CD8+ and CD3+CD4+ T cells significantly increased in the CIK group, compared with the non-CIK group (p < 0.01).
Conclusions
CIK cell therapy demonstrated a significant superiority in prolonging the median overall survival, PFS, DCR, ORR and QoL of HCC patients. These results support further larger scale randomized controlled trials for HCC patients with or without the combination of other therapeutic methods.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is the third most common cancer globally, with a poor prognosis and limited systemic treatment options [1]. In men, it is the fifth most common cancer worldwide and the third-leading cause of cancer-related death [2]. HCC is resistant to conventional chemotherapy and is insensitive to radiotherapy. Surgery, transcatheter arterial chemoembolization (TACE) and radiofrequency ablation (RFA) are considered as the main treatments for HCC today [3]. However, the recurrence rate is still high, and long-term survival is unsatisfactory, as approximately 80% of patients die within a year of diagnosis. After curative resection or transplantation, tumor recurrence rate can be as high as 25% per year. Although some centers have reported excellent long-term results, survival after hepatic resection or transplantation is as low as 50% at 3 years and 20%-30% at 5 years [4]. Therefore, finding effective methods to strengthen treatment efficacy and prevent recurrence is an important issue in HCC therapy.
Cytokine-induced killer (CIK) cells, which are non-major histocompatibility complex (MHC)-restricted CD3+CD56+ T cells, take advantage of the body's natural ability to eliminate tumor cells by stimulating and restoring the immune system to recognize and kill tumor cells [5]. Majority of CIK cells express T cell receptors, and others express NK cell markers. CIK cells are generated by incubating mononuclear cells from peripheral blood, bone marrow or cord blood with various types of additions. Current protocols to differentiate CIK cells are based on a combination of interferon (IFN)-γ on day 1 of culture, followed by CD3 monoclonal antibody (CD3McAb), interleukin2 (IL2), interleukin1 (ILl) 24 hours later [6, 7]. CIK cells have higher proliferation rate, cytolytic activities and non-MHC-restricted killing of tumor cells in comparison with lymphokine-activated killer cells (LAK cells) which are essentially activated by natural killer (NK) cells [8, 9].
Clinical studies indicated that autologous CIK cell therapy could be used as an efficient adjuvant anticancer immunotherapy to eradicate residual cancer cells, prevent recurrence, improve progression-free survival (PFS) rates, and promote the quality of life (QoL) for cancer patients [10–14]. Therefore, we performed a systematic review and meta-analysis of randomized controlled clinical trials (RCTs) to assess the efficacy and tolerability of CIK cells in the treatment of patients with HCC.
Materials and methods
Study design, search strategy, and eligibility criteria
Trials were identified by electronic searches in the PubMed database, the Cochrane Central Registry of Controlled Trials, the Wanfang Database, the China Science and Technology Periodical Database, China Journal Net, reference lists of published trials and relevant review articles. The search strategy included the medical subject headings of "hepatocellular carcinoma", "cytokine-induced killer cells" and free text searches. No language limits were applied. Initial searches were performed in August 2011, with updates in February 2012. In addition, we contacted drug manufacturers, asked experts in the field, and performed manual searches in reference lists, conference proceedings of the American Society of Clinical Oncology (ASCO) Annual Meetings and the European Cancer Conference (ECCO). We excluded abstracts that were never subsequently published as full papers and studies on animals.
Data collection
We gathered information including authors' names, journal and year of publication, sample size per arm, performance status (PS score), regimen used, median age of patients, and information pertaining to study design (whether the trial reported the mode of randomization, allocation concealment, description of withdrawals per arm, and blinding) for the trials included in the study. Written informed consent was obtained from the patient for publication of this report and any accompanying images.
Definition of outcome measures
Overall survival (OS) and the PFS were the primary outcome measure. OS was defined as the time from the initiation of treatment until death from any cause. PFS was defined as the time from the initiation of treatment to the first observation of disease progression or death from any cause. The secondary endpoints were the overall response rate (ORR) and disease control rate (DCR). Toxicity was graded according to the NCI Common Toxicity Criteria. QoL was assessed by the Karnofsky performance status (KPS) [15].
Statistical analysis
The analysis was performed using a Review Manager Version 5.0 (Nordic Cochran Centre, Copenhagen). We defined a statistical test with a p value less than 0.05 as significant. Odds ratio (OR) and 95% confidence interval (CI) as relevant effect measures were estimated directly or indirectly from the given data. Where they were not provided, they were estimated indirectly from other summary statistics or from the data extracted from published Kaplan-Meier curves. To assess statistical heterogeneity among trials, the Cochran's chi-square test (Q test) was performed, with a predefined significance threshold of 0.05. If the Q test was statistical significant (p < 0.05), a random effects meta-analysis was performed; otherwise, a fixed effect model was used. All reported p values result from two-sided versions of the respective tests. The revision of funnel plots did not reveal any considerable publication bias.
Results
Selection of the trials
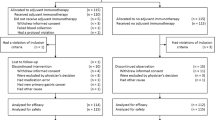
The electronic searches yielded two hundred eighty six references. After title and abstract review, 252 publications were excluded for different reasons (25 for being review articles, 119 for using animal models, 6 for being case reports, 98 for being vitro experiments, 4 for being nursing studies). The full texts of 34 articles were selected as potentially relevant and retrieved for more detailed assessment. We excluded a total of 21 studies for the following reasons: 3 trials were excluded for being phase I clinical trials, 18 trials were excluded for being non-RCTs. The selection procedure of the clinical trials is shown in Figure 1. As a result, 13 articles reporting phase II and III clinical trials of CIK cell-based therapy were selected for meta-analysis. These 13 eligible RCTs included a total of 1212 patients.
Characteristics of CIK cell-based therapy
Clinical data of these trials are listed in Table 1. CIK therapy combined with TACE in four of the trials [16–19], with TACE and RFA in other four of the trials [20–23], with surgery alone in three trials [24–26], with TACE alone or TACE and percutaneous ethanol injection (PEI) in other two trials [27, 28] were evaluated. IFN-γ, CD3McAb, IL-1a and IL-2 were used in CIK cell culture system in all of the analyzed trials.
The CIK cells for all trials were prepared from peripheral blood. The number of CIK cells transfused into patients in these studies ranged from 8.0 × 109 to 5.0 × 1010 per course. The patient information from two groups (CIK cell therapy and non-CIK cell therapy) of the trials such as gender and CIK cell dose were analysed by χ2 test. There was no statistically significant difference between groups (p > 0.05). Different article-origin of the patient information in each group did not interfere with the results of meta-analysis.
Survival
The analysis showed that significant survival benefit (OS: OR = -20.01, 95% CI: -25.72 to -15.31, p < 0.001) was observed in patients receiving CIK-based therapy. The results of the pooled analysis showed that CIK arm was associated with significantly improved one-year survival (OR = 0.25, 95% CI: 0.12 to 0.52, p < 0.001) and two-year survival (OR = 0.17, 95% CI: 0.07 to 0.43, p < 0.001). However, there was no difference in half-year survival comparing the CIK group versus non-CIK group (77% in CIK group versus 67% in the non-CIK group; OR = 0.43, 95% CI: 0.05 to 3.94, p = 0.45) (Figure 2).
Comparison of 0.5-year, 1-year, and 2-year survival between non-CIK group and CIK group. OR, odds ratio; OS, overall survival. non-CIK, non-CIK-containing therapy; CIK, CIK-containing therapy. The random effects meta-analysis model (Mantel-Haenszel method) was used in this analysis. Each trial is represented by a square, the center of which gives the odds ratio for that trial. The size of the square is proportional to the information in that trial. The ends of the horizontal bars denote a 95% CI. The black diamond gives the overall odds ratio for the combined results of all trials. The center denotes the odds ratio, and the extremities denote the 95% CI.
Concerning PFS, treatment with CIK-combined therapy was also associated with a significantly prolonged half-year PFS (OR = 0.29, 95% CI: 0.16 to 0.52, p < 0.001) and one-year PFS (OR = 0.35, 95% CI: 0.22 to 0.53, p < 0.001) (Figure 3).
Response rate
The analysis of DCR and ORR also demonstrated favorable results for the CIK cell therapy arm (OR = 0.09, 95% CI: 0.04 to 0.25, p < 0.001 and OR = 0.21, 95% CI: 0.13 to 0.35, p < 0.001) (Figure 4).
In the subgroup analysis, a significantly prolonged DCR (OR = 0.08, 95% CI: 0.02 to 0.40, p = 0.002) and ORR (OR = 0.36, 95% CI: 0.17-0.72, p = 0.004) were observed in the patients treated with CIK combined TACE therapy compared with those treated with TACE combined PEI therapy.
Toxicity, HBV-DNA content and plasma AFP
In most trials, slight fever and chills could be seen, and the body temperature varied from 37.5°C to 39.0°C within 24 hours after CIK cell transfusion. The overall OR of 0.07 (95% CI: 0.01 to 0.53) demonstrated that the incidence of fever in the CIK therapy group was significantly higher than those in the non-CIK group (p = 0.01).
We classified QoL as "improvement", "stability" or "deterioration", if KPS was higher than, equal to or lower than pretreatment, respectively. The analysis showed that TACE combined CIK therapy can improve HCC patients' QoL, showing a better QoL (OR = 0.32, 95% CI: 0.16 to 0.64, p = 0.001) when compared with non-CIK therapy. The HBV-DNA content in the analysis was based on two HCC trials [21, 22]. During one-year follow-up, no patient HBV-DNA content was more than 1 × 106 copy/ml in the CIK therapy group. Patients in the CIK group had lower HBV-DNA content than patients in the non-CIK group (OR = 27.5, 95% CI: 5.21 to 145.15, p < 0.01). (Table 2).
The AFP content in the analysis was based on three HCC trials 23,26.27. Plasma AFP decreased more significantly in the CIK group than in the non-CIK group (OR = 0.20, 95% CI: 0.14 to 0.29, p < 0.001). Plasma AFP of patients in the CIK group was more likely to drop to a normal level, compared with the non-CIK group (OR = 0.20, 95% CI: 0.11 to 0.35, p < 0.001), the TACE alone group (OR = 0.12, 95% CI: 0.05 to 0.26, p < 0.001) and the PEI group (OR = 0.34, 95% CI: 0.16 to 0.72, p = 0.005) (Figure 5).
Forest plot for AFP concentration drop to normal in different therapy group. non-CIK, non-CIK-based therapy; CIK, CIK-based therapy; TACE, transcatheter arterial chemoembolization therapy; PEI, percutaneous ethanol injection therapy. The fixed effects meta-analysis model (Mantel-Haenszel method) was used in this analysis.
Comparison of T-lymphocyte subsets in peripheral blood
The analysis showed the ratio of CD3+, CD4+, CD4+CD8+ and CD3+CD4+ T cells significantly increased in the CIK group, compared with the non-CIK group, which was reflected by a pooled OR of -0.79 for CD3+ cells (95% CI:-1.13 to -0.45, p < 0.001),-2.00 for CD4+ cells (95% CI:-2.7 to -1.3, p < 0.001), 0.04 for CD4+CD8+ cells (95% CI: 0.03 to 0.05, p < 0.001), and -2.02 for CD3+CD4+ cells (95% CI:-2.27 to -1.76, p < 0.001). Furthermore, the percentage of CD8+ and CD3+CD8+ T cells significantly decreased in the CIK group compared with the non-CIK group (95% CI: 2.43 to 3.67, p < 0.001; 95% CI:-2.1 to -1.56, p < 0.001; respectively) (Table 3).
Discussion
According to research in recent years, HCC patients have some immune dysfunctions, including those in innate and adaptive immune responses [29]. It has been reported that interferon therapy appeared to decrease recurrence rate after resection of hepatitis C virus or hepatitis B virus-related HCC in some randomized controlled trials. Tumor immunological studies show that cellular immunity of cancer patients is closely related to the occurrence and development of cancers. Cytokine immunotherapy not only has fewer side effects but also can avoid tumor dysimmunity and specific tolerance of tumor antigen. With the rapid advance of molecular biology technology, the application of immunotherapy combined with surgery or interventional therapy is thought to be promising strategy of HCC treatment.
Schmidt-Wolf et al. [5] first reported that CIK cells had a strong anti-proliferative capacity and cytotoxicity on tumor cells. Further studies have demonstrated that CIK cells, which are lymphocytes induced by many cytokines [30], have better anti-tumor effects compared with LAK cells (lymphocytes activated by IL-2 alone). Our analysis showed that CIK cell therapy was associated with significantly prolonged one-year and two-year survival, OS and PFS, but had no effect on half-year survival (p = 0.45). A favored DCR and ORR were also observed in patients receiving CIK cell therapy (p < 0.01). The mechanism of anti-tumor activity of CIK cells is still unclear. Schmidt-Wolf et al. [31] demonstrated that perforin-mediated pathways possibly play an important role in CIK cells induced tumor cell killing effect.
The study also indicated that patients receiving CIK cell therapy had improved QoL compared with patients in the non-CIK group (p < 0.01). Although CIK group was associated with more fevers (p = 0.01). However, fever after CIK cell transfusion was light in most trials and lasted only 24 hours or less. In biological treatments, moderate fever is considered to be a normal reaction of immune function and beneficial to treatment [32].
We also observed that the HBV-DNA and AFP levels decreased significantly in the CIK group (p < 0.01). Hepatitis B virus infection can lead to hepatic sclerosis and HCC. AFP is currently widely recognized as a tumor-related prognosis antigen for HCC. HCC patients with high levels of HBV-DNA and AFP have a poor prognosis [33, 34]. Concomitant infection with HBV and impairment from hepatic sclerosis in the hepatic parenchyma lead to an increase of AFP levels [35, 36]. The reduction of AFP content and HBV-DNA content contribute to preventing the short-term recurrence of HCC and prolonging patients' survival time.
Targeting of the human immune system against tumor mainly depends on cellular immunity. CD4+ T cells are considered to have a predefined role as a helper T cell within the immune system, providing help in recruiting CD8+ T cells and activating macrophages through IFN-γ production. It has been demonstrated that cytotoxicity against tumor is dependent on an appropriate CD4+ and CD8+ T cell interaction. The ratios of T lymphocyte subsets in peripheral blood are usually disordered in tumor patients [37, 38]. The analysis showed the percentage of CD3+, CD4+ and CD3+CD4+ T cells significantly increased in the CIK group, compared with the non-CIK group, but the percentage of CD8+ and CD3+CD8+ T cells significantly decreased in the CIK group, compared with non-CIK group (p < 0.001). The percentage of CD4+ T cells significantly increased, CD8+ T cells significantly decreased, and thus the ratio of CD4+/CD8+ increased. Therefore, immune suppression was attenuated, enhancing the immune system's tumor clearance ability.
In present study, CIK cells were cultured in complete medium (CM) supplemented with human blood serum in eleven trials, and other two trials used serum-free medium (SFM) to culture CIK cells. Mitomycin, cisplatin, anthracycline and lipiodol were used for TACE. Most studies showed that the culture of CIK cells amplified more and produced more IFN-γ, IL-4, or IL-5 in CM than in SFM [39, 40]. Our analysis showed that half-year PFS, one-year PFS, one-year survival in the CM were 93.6%, 85.3%, 84.2% which differ significantly from the 72.2%, 40.3%, 72.2% in CIK cells cultured in the SFM. However, half-year survival (68.5%) and two-year survival in the CM (51.5%) were lower than those in SFM group (90.3%, 72.2%).
The present meta-analysis was not based on individual patient data and was not subjected to an open external evaluation procedure. Therefore, the analysis is limited in that the use of published data may have led to an over-estimation of the treatment effects. With respect to both response and survival, we could not limit our analysis to intention-to-treat populations as the total number of patients randomized per arm was not always reported. Therefore, for consistency among studies, we elected to use the assessable patients for our analysis. Moreover, all the selected trials in present study were conducted in Asia, lacking multinational larger sample multicenter clinic research with sufficient statistical power. In order to solve this problem, a larger scale international multicenter randomized clinical trial should be conducted in the near future.
Taken together, the CIK cells were prepared after in vitro priming and were transfused into patients with HCC. These early results appear very promising, and the side effects related to CIK cell transfusion were few. It will hopefully lead to more large and controlled clinical trials in these settings.
Conclusion
CIK cell therapy demonstrated a significant superiority in prolonging the OS, PFS, DCR, ORR and QoL of HCC patients compared with non-CIK therapy. These observations support further larger scale RCTs to evaluate the efficacy of CIK cell therapy in the treatment of HCC with or without the combination of other therapeutic methods.
References
Aravalli RN, Steer CJ, Cressman EN: Molecular mechanisms of hepatocellular carcinoma. Hepatology 2008, 48: 2047–2063.
Höpfner M, Schuppan D, Scherübl H: Growth factor receptors and related signalling pathways as targets for novel treatment strategies of hepatocellular cancer. World J Gastroenterol 2008, 14: 1–14.
Avila MA, Berasain C, Sangro B, Prieto J: New therapies for hepatocellular carcinoma. Oncogene 2006, 25: 3866–3884.
Poon RT, Fan ST, Ng IO, et al.: Singnificance of resection margin in hepatectomy for hepatocellular carcinoma:a critical reappraisal. Ann Surg 2000, 231: 544–551.
Schmidt-Wolf IG, Negrin RS, Kiem HP, et al.: Use of a SCID mouse/human lymphoma model to evaluate cytokine-induced killer cells with potent antitumor cell activity. J Exp Med 1991, 174: 139–149.
Introna M, Borleri G, Conti E, et al.: Repeated infusions of donor-derived cytokine-induced killer cells in patients relapsing after allogeneic stem cell transplantation: a phase I study. Haematologica 2007, 92: 952–959.
Li Q, Chang AE: Adoptive T-cell immunotherapy of cancer. Cytokines Cell Mol Ther 1999,5(2):105–117.
Schmidt-Wolf IG, Lefterova P, Mehta BA, et al.: Phenotypic characterization and identification of effector cells involved in tumor cell recognition of cytokine-induced killer cells. J Exp Hematol 1993,21(13):1673–1679.
Linn YC, Hui KM: Cytokine-induced NK-like T cells: from bench to bedside. J Biomed Biotechnol 2010, 2010: 1–8.
Hontscha C, Borck Y, Zhou H, et al.: Clinical trials on CIK cells: first report of the international registry on CIK cells (IRCC). J Cancer Res Clin Oncol 2010, 137: 305–310.
Bonanno G, Iudicone P, Mariotti A, et al.: Thymoglobulin, interferon-γ and interleukin-2 efficiently expand cytokine-induced killer (CIK) cells in clinical-grade cultures. J Transl Med 2010,7(8):129–143.
Introna M, Pievani A, Borleri G, et al.: Feasibility and safety of adoptive immunotherapy with CIK cells after cord blood transplantation. Biol Blood Marrow Transplant 2010,16(11):1603–1607.
Wei G, Ni W, Chiao J-W, et al.: A meta-analysis of CAG (cytarabine, aclarubicin, G-CSF) regimen for the treatment of 1029 patients with acute myeloid leukemia and myelodysplastic syndrome. J Hematol Oncol 2011, 4: 46.
Tan J, Cang S, Ma Y, et al.: Novel histone deacetylase inhibitors in clinical trials as anti-cancer agents. J Hematol Oncol 2010, 3: 5.
Yates JW, Chalmer B, McKegney FP: Evaluation of patients with advanced cancer using the Karnofsky performance status. Cancer 1980, 45: 2220–2224.
Zhang K, Zuo Q, Luo R-C, et al.: The CIK cells adoptive immunotherapy on immune function in patients with liver cancer after TACE effect. J Guangdong Med 2007,28(9):1487–1488.
Guo P, Lu H, Dong S-X, et al.: The clinical reserach of CIK cells combined interventional therapy for advanced liver cancer. Chin Hosp Pharm J 2007,27(11):1565–1567.
Hao M-Z, Cheng Q, Ye Y-B, et al.: Transcatheter arterial chemoembolization combined with cytokine induced killers in treatment of hepatocellular carcinoma. Chin J Cancer Biother 2006,13(4):303–305.
Hao MZ, Lin HL, Chen Q, et al.: Efficacy of transcatheter arterial chemoembolization combined with cytokine-induced killer cell therapy on hepatocellular carcinoma: a comparative study. Chin J Cancer 2010, 29: 172–177.
Weng DS, Zhou J, Zhou QM, et al.: Minimally invasive treatment combined with cytokine-induced killer cells therapy lower the short-term recurrence rates of hepatocellular carcinomas. J Immunother 2008, 31: 63–71.
Zhao M, Wu PH, Zeng YX, et al.: Cytokine-induced killer cell fusion to lower recurrence of hepatocellular carcinoma after transcatheter arterial chemoembolization sequentially combined with radiofrequency ablation: a randomized trial. Zhonghua Yi Xue Za Zhi 2006, 86: 1823–1828.
Pan CC, Huang ZL, Li W, et al.: Serum alpha-fetoprotein measurement in predicting clinical outcome related to autologous cytokine-induced killer cells in patients with hepatocellular carcinoma undergone minimally invasive therapy. Chin J Cancer 2010, 29: 596–602.
Wan C, Luo RC, Cui F, et al.: Transcatheter arterial chemoembolization plus sequential radiofrequency ablation combined with cytokine-induced killer cell therapy for hepatocellular carcinoma. J Pract Med 2008,24(8):1321–1323.
Hui D, Qiang L, Jian W, et al.: A randomized, controlled trial of postoperative adjuvant cytokine-induced killer cells immunotherapy after radical resection of hepatocellular carcinoma. J Dig Liver Dis 2009, 41: 36–41.
Lu B, Li DY, Zhang X: The observation of CIK cells on the survival rate of liver cancer patients. J Med Forum 2008,29(24):69–70.
Yu WC, Ye YB, Zhou D, et al.: Effect of postoperative transcatheter arteial chemoembolization combined with cytokine-induced killer immunotherapy of recurrence and suvival rate of hepatocellular carcinoma patients. J Minim Invasive Med 2009,4(5):459–461.
Zhang ZN, Xu YM, Xu FX, et al.: Clinical study on the treatment of advanced hepatocellular carcinoma by CIK cell. J Southeast Natl Defense Med 2006,8(2):84–87.
Shi Y, Gao CJ, Dong SL, et al.: Cytokine-induced killer cell for interventionla chemotherapy of hepatocellular carcinoma. J Intervent Radiol 2007,16(4):235–239.
Sun K, Wang L, Zhang YY: Dendritic Cell as Therapeutic Vaccines against Tumors and Its Role in Therapy for Hepatocellular Carcinoma. Cell Mol Immunol 2006,3(3):197–203.
Verneris MR, Karami M, Baker J, et al.: Role of NKG2D signaling in the cytotoxicity of activated and expanded CD8+ T cells. Blood 2004, 103: 3065–3072.
Schmidt-Wolf GD, Negrin RS, Schmidt-Wolf IG: Activated T cells and cytokine-induced CD3 + CD56+ killer cells. Ann Hematol 1997,74(2):51–56.
Hada H, Arima T, Nagashima H, et al.: Hepatitis B virus DNA in human hepatocellular carcinoma: is the integration of hepatitis B virus DNA really carcinogenic? Gastroenterol Japan 1986,21(6):594–600.
Wei GQ, Ni WM, Chiao JW, et al.: Targeting insulin-like growth factor axis in hepatocellular carcinoma. J Hematol Oncol 2011, 4: 30.
Cedrone A, Covino M, Caturelli E, et al.: Utility of alpha - fetoprotein (AFP) in the screening of patients with virus - related chronic liver disease: does different viral etiology influence AFP levels in HCC? A study in 350 western patients. Hepatogastroenterology 2000,47(36):1654–1658.
Soresi M, Magliarisi C, Campagna P, et al.: Usefulness of alpha- fetoprotein in the diagnosis of hepatocellular carcinoma. Anticancer Res 2003,23(2):1747–1753.
Johnson PJ: The role of serum alpha - fetoprotein estimation in the diagnosis and management of hepatocellular carcinoma. Clin Liver Dis 2001,5(1):145–159.
Kastelan Z, Lukac J, Derezic D, et al.: Lymphocyte subsets, lymphocyte reactivity to mitogens, NK cell activity and neutrphil and monocyte phagocytic functions in patients with bladder carcinoma. Anticancer Res 2003, 23: 5185–5189.
Attallah AM, Tabll AA, El-Sadny M, et al.: Dysregulation of blood lymphocyte subsets and natural killer cells in schistosomal liver cirrhosis and hepatocellular carcinoma. Clin Exp Med 2003, 3: 181–185.
Cao JP, Jiang ZM, Zhang XC, et al.: The proliferation, phenotype change and anti-tumor activity of cytokine induced killer cell. J Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 2005,21(5):583–586.
Kambe N, Kambe M, Chang HW, et al.: An improved proved procedure for the development of human mast cells from dispersed fetal liver cells in serum-free culture medium. J Immounol Methods 2000,240(1–2):101–110.
Acknowledgements
This study was supported by Shanghai Municipal Natural Science Foundation (Project Number: 09ZR1417900), Leading academic discipline project of Shanghai Municipal Education Committee (Project Number: J50208), Shanghai Pujiang Program (Project Number: 11PJ1406500), and the National Natural Science Funds (Project Number: 81102015).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
LT and YCX performed the computerized search of the trials, contacted experts and participated in the trial selection. YM and ZZ participated in the trial selection and performed the statistical analysis. HXW and JW conceived of the study. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ma, Y., Xu, YC., Tang, L. et al. Cytokine-induced killer (CIK) cell therapy for patients with hepatocellular carcinoma: efficacy and safety. Exp Hematol Oncol 1, 11 (2012). https://doi.org/10.1186/2162-3619-1-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2162-3619-1-11