Abstract
Dyspnea is a general term used to characterize a range of different descriptors; it varies in intensity, and is influenced by a wide variety of factors such as cultural expectations and the patient's experiences. Healthy subjects can experience dyspnea in different situations, e.g. at high altitude, after breath-holding, during stressful situations that cause anxiety or panic, and more commonly during strenuous exercise. Discussing the mechanisms of dyspnea we need to briefly take into account the physiological mechanisms underlying the sensation of dyspnea: the functional status of the respiratory muscles, the role of chemoreceptors and mechanoreceptors, and how the sense of respiratory motor output reaches a level of conscious awareness. We also need to take into account theories on the pathophysiological mechanisms of the sensation of dyspnea and the possibility that each pathophysiological mechanism produces a distinct quality of breathing discomfort. The terms used by subjects to identify different characteristics of breathing discomfort - dyspnea descriptors - may contribute to understanding the mechanisms of dyspnea and providing the rationale for a specific diagnosis.
Similar content being viewed by others
Dyspnea is a general term used to characterize a range of different descriptors; it varies in intensity, and is influenced by a wide variety of factors such as cultural expectations and the patient's experiences [1]. Many different clinical disorders that affect the heart, lungs and neuromuscular apparatus produce symptoms of dyspnea.
The sensation of dyspnea seems to originate with the activation of sensory systems involved in respiration. Sensory information is, in turn, relayed to higher brain centers where central processing of respiratory-related signals and contextual, cognitive and behavioral influences shape the ultimate expression of the evoked sensation. The homeostatic systems involved in the regulation of respiration provide a framework for understanding the mechanisms of dyspnea [1]. Awareness of respiratory sensation can occur in normal situations. Dyspnea is a heightened level of awareness of respiratory sensation and has a strong emotional component. The neural basis of dyspnea is therefore likely to involve activation of both the cortex and the limbic system [2]. Healthy subjects can experience dyspnea in different situations, e.g. at high altitude, after breath-holding, during stressful situations that cause anxiety or panic, and more commonly during strenous exercise.
Many factors play an important role in the mechanisms of dyspnea: functional status or respiratory muscles, mechanical and chemical afferents, central motor output.
The Physiology of Dyspnea
Respiratory muscles
Exercise is the most common setting in which healthy subjects refer a sensation of dyspnea. Given the complexity of disturbances in respiratory mechanics during exercise, it is difficult to be sure which alterations contribute most strongly to the sensation of dyspnea [3].
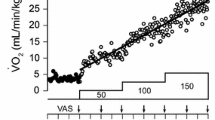
Increased sensation of respiratory effort is frequently a chosen descriptor of dyspnea both in normal subjects and in patients with COPD during exercise [3]. Studies in healthy humans have shown that the increase in effort represents the increase in motor command [4, 5]. The effort required to sustain any given power increases the longer the activity is sustained. It is noteworthy that inspiratory effort is not synonymous with inspiratory pressure. For a given pressure per breath (Pbr), the perception of effort is a function of maximal inspiratory pressure (MIP), so that the greater the Pbr/MIP ratio, the greater the perception of respiratory effort [4, 5]. During exercise, respiratory impedance can experimentally be either increased, resulting in greater pressure and lesser velocity of contraction, or decreased, resulting in a greater velocity of shortening and less pressure; both peak of pressure and velocity of inspiratory muscle shortening contribute independently and collectively to dyspnea [4]. With exercise, a greater tidal volume (Vt) increases end-inspiratory lung volume forcing the subject to breathe at higher volumes in the flat part of the pressure-volume curve, and increasing the inspiratory pressure per breath [4, 6]; moreover, the maximal pressure-generating capacity diminishes at high lung volumes and decreases with the increase in velocity of muscle shortening for any given lung volume [5]. In turn, pressure per breath to maximal pressure-generating capacity ratio increases during progressive exercise in proportion to the sense of effort. Leblanc et al. [5] emphasize the importance of the relationship between demands placed on the inspiratory muscles and their capacity to generate pressure in understanding the perception of dyspnea experienced by patients with respiratory disorders. Thus, the awareness of effort seems to be the dominant descriptor of dyspnea in most circumstances, even if it may not be possible to equate the grading of effort with dyspnea in all situations [3].
Respiratory muscle recruitment may affect the sensation of respiratory discomfort. Dyspnea may be the signal that rib cage inspiratory muscles are being recruited to assist the diaphragm [7]. Although the diaphragm is recruited progressively, i.e. its power progressively increases with exercise or chemical ventilatory stimuli, it is not recruited to the same degree as the inspiratory muscles of the rib cage [8]. An important observation is that the velocity of shortening of rib cage inspiratory muscles is also correlated with the perception of effort [9]. A large body of evidence indicates the role played by rib cage muscle activation in the sensation of effort in healthy subjects: dyspnea may be due to a central perception of an overall increase in central respiratory motor output directed preferentially to the rib cage muscles [9–11]. Thus, an increased central output to the rib cage muscles contributes importantly to exercise dyspnea [3].
Weakness and respiratory muscle fatigue may play a role in the onset of dyspnea. The intensity of dyspnea is greater in patients with cardio-respiratory disorders and weak respiratory muscles because it takes more effort to drive a weak muscle than it does to drive a strong muscle. During exercise, the greater the increase in muscle force, the greater the increase in maximal power output; for a given maximal power output the weaker the inspiratory muscles the greater the dyspnea, with a 2-fold increase in MIP resulting in about 30% decrease in dyspnea [12]. Therefore, in addition to other factors, one must also take into account the contribution of muscle weakness to the increased dyspnea perception and reduced work capacity [12].
Fatigue is defined as a loss of the capability to generate skeletal muscle force and/or velocity which is accompanied by recovery during rest [13]. The role of inspiratory muscle fatigue on dyspnea has long been investigated. Bradley et al. [14] demonstrated in healthy subjects at rest during inspiratory resistive loading that, irrespective of whether the diaphragmatic patterns of contraction were fatiguing or not, the sensation of inspiratory effort was directly related to negative intrathoracic pressure, i.e. the driving pressure for inspiration [14]. These findings are in line with the notion that the generation of intrathoracic pressure is the most important stimulus for the sensation of inspiratory effort. Fatigue, however, has no major effect on the sensation of dyspnea during exercise in healthy subjects [11]. High intensity exercise causes quadriceps fatigue [15] but not diaphragmatic fatigue [16, 17] in most patients with COPD of moderate severity. Central inhibitory fatigue of the diaphragm, i.e. a low level of activation of the muscle, does not take place in COPD while exercising to exhaustion; dynamic hyperinflation during exhaustive exercise reduces diaphragm pressure-generating capacity, while promoting a high level of diaphragm activation [18]. On the other hand, available data in humans show the influence of heavy intensity whole body exercise on diaphragm fatigue, likely due to less blood flow availability to the diaphragm in the face of high blood flow demands by locomotor muscles [7]. In turn, while data in COPD argue against inspiratory muscle fatigue contributing to dyspnea, respiratory muscle fatigue could limit exercise performance via an increased sensation of dyspnea in healthy subjects [3].
The recruitment of the expiratory muscles also plays a role in the onset of dyspnea. Previous and recent data have reported the progressive recruitment of expiratory muscles during exercise in healthy humans [9, 11, 19–22] and in patients with COPD [23–27]. Expiratory muscle recruitment is enhanced by flow limitation both in healthy humans [9, 21] and in patients with COPD [23]. Unlike the diaphragm, the expiratory muscles contribute importantly to the perception of dyspnea during incremental exercise with expiratory flow limitation [9].
In normal subjects, also different chest wall kinematics and different patterns of muscle coordination during diverse exercise tasks (leg exercise, arm exercise), may differently affect the sensation of respiratory effort and dyspnea. Romagnoli et al. [28], comparing the effects (in terms of dyspnea) of a cycloergometer incremental exercise test with unsupported arm exercise bearing 2 Kg of weight in each forearm, observed that the Borg score was significantly higher with unsupported arm exercise at the same level of ventilation (50 L·min-1). Inspiratory muscle pressure and abdominal pressure were the sole predictors of the variability in Borg score during leg exercise and arm exercise, respectively. Those data showed that (i) the Borg score was significantly higher at 50 L·min-1 of ventilation in a time when both expiratory rib cage muscles and abdominal muscle pressures, but not transdiaphragmatic pressure, were greater with arm exercise; and (ii) changes in abdominal pressure predicted a large amount of the variability in Borg score with arm exercise. Conceivably, Romagnoli et al. speculated that a shift of central motor output to the expiratory muscles would appear to be the prime candidate for generating the sensation of respiratory difficulty with arm exercise [28].
Chemoreceptors
Dyspnea is a normal phenomenon that is protective against abnormalities in gas exchange. Hypercapnia and hypoxia drive breathing and therefore must influence the perception of the motor events.
It is well known that intense dyspnea can be induced by breathing a gas mixture with high CO2 or low O2 [1]. Hypercapnic-hyperpnea induces a subjectively more intense dyspnea than that induced by voluntary hyperventilation or exercise [29]. Dyspnea induced by hypercapnia could theoretically result either directly from activation of chemoreceptors, or indirectly through the increase in respiratory afferent feedback from the resulting increase in respiratory motor output [2]. It is thought that the majority of the dyspnea that occurs is due to the latter mechanism. In fact, in curarized healthy subjects increasing PCO2 did not induce the sensation of dyspnea [30, 31]. In another study on healthy, passively ventilated subjects, dyspnea was sensed in response to increased PCO2 only after respiratory efferent activation [32], implying that it is the respiratory afferent activation that causes the dyspnea and not the elevated PCO2 per se. However, there is also evidence from several other studies suggesting that hypercapnia can induce dyspnea independently of changes in respiratory output. In particular, Banzett et al. showed the effect of increasing hypercapnia in mechanically ventilated quadriplegics [33] and in healthy subjects after complete neuromuscular block exposed to progressive elevations in inspired CO2 [34]. There is other evidence indicating that changes in CO2 can induce dyspnea independently of changes in respiratory effort [35]. For example, for the same level of ventilation, individuals breathing a hypercapnic gas mixture experience more dyspnea compared to eucapnic individuals and presumably equivalent motor output [36, 37]. Moreover, an increased intensity of dyspnea is evoked when ventilation is voluntarily decreased below the level dictated by chemical drive despite the lesser respiratory motor output [38]. That dyspnea occurs when there is a mismatch between ventilation and the demand set by the chemical drive exemplifies the importance of maintaining chemical homeostasis [2]. If ventilation is maintained at a constant level, subjects still experience an increased intensity of dyspnea when PCO2 is increased; however their subjective estimation of respiratory effort is actually decreased [39]. Thus, although respiratory afferent feedback may play a large role under some conditions, it appears that there is also a direct and independent effect of hypercapnia itself [2]. There is some evidence that increase in PCO2 activates forebrain regions and that these same regions are activated in association with dyspnea induced by other factors [2].
Data from respiratory-related evoked potential studies in humans show that brief periods of breathlessness induced by upper airway occlusion activate the somatosensory cortex [40]. Functional imaging studies with positron emission tomography (PET) and functional magnetic resonance (fMRI) imaging reveal that hypercapnia causes activation of multiple limbic regions of the brain, including the cingulate cortex, hippocampus, insula, amygdala and hypothalamus, but not forebrain regions that are activated by volitional breathing, such as the primary motor cortex, premotor area and supplementary motor area [41–43]. Functional imaging with PET and fMRI demonstrate that some regions, such as the opercolum and amygdala, are activated by dyspnea induced by other means (e.g. lung volume restriction) than hypercapnia [43, 44]. These results are consistent with the possibility that dyspnea induced by hypercapnia is due to activation of the limbic system by direct or indirect projections from chemoreceptors to limbic regions [2].
Dyspnea may be generated by hypoxia but it is a much weaker stimulus of dyspnea. Nonetheless, progressively more effort is required to generate any given muscle power as the arterial oxygen content declines (i.e. altitude or anemia). Muscles fatigue more readily, and more effort is required as the muscles fatigue [3]. Change in O2 content may affect dyspnea directly via chemoreceptors independently of change in , or indirectly, by increasing in normal subjects [45] and in COPD patients [46]. The relative importance of afferent feedback versus direct chemoreceptor input is unclear, but hypoxia is thought to be less dyspnea inducing than hypercapnia [35].
Chest wall and pulmonary vagal receptors
Afferent signals from mechanoreceptors in the joint, tendons and muscles of the chest wall to the brain appear to play a role in modulating respiratory sensations. Above all, afferents from intercostal muscles have been shown to project to the cerebral cortex and contribute to propioception and kinesthesia [47, 48]. During hypercapnia associated with the imposition of a resistive load, the effect of vibration on the chest wall produces a reduction in dyspnea at a constant level of central drive, suggesting a preeminent role for chest wall receptors [49]. However evidence also exists against the role of afferent muscle feedback in exercising healthy subjects during epidural anesthesia, in whom rate of perceived exertion during cycling exercise is either unchanged or increased [50, 51], despite a marked reduction in afferent limb muscle sensory inputs. And Marcora [52], focusing the evidence on the issue, stresses the point that perception of effort during exercise is independent of afferent feedback from skeletal muscles. However it seems prudent to consider that effort likely requires both central stimulation as well as continuous modulation by afferent information from a variety of sources [53].
There is some evidence that vagal influences, independently of any effect on the level and pattern of breathing, may also contribute to the sensation of dyspnea [1]. Relatively dated studies showed that vagal blockade or its section reduced dyspnea in cardiac patients [54]. More recent evidence has focused on the role of irritant vagal receptors on the sensation of chest constriction [55, 56]. The role of stretch receptors has been highlighted in paralyzed and ventilated subjects at constant level of PaCO2, in whom dyspnea increases with the reduction of tidal volume [57]. The role of C-fibers is not completely clarified. However, evidence exists that during exercise, dyspnea arises in patients with double lung transplantation who can estimate the magnitude of inspiratory resistive loads based on their normal sense of effort [58]. This means that pulmonary vagal receptors are not essential to the onset of dyspnea in this condition. Respiratory sensations mediated through pulmonary C-fiber activation can also be generated under certain normal physiological conditions. For example, Paintal and co-workers [59] have suggested that an increase in interstitial fluid volume resulting from elevated pulmonary arterial and capillary pressures contributes to the sensation of breathlessness after moderate and severe exercise [59]. Increases in pulmonary arterial and capillary pressures can also occur as a result of pulmonary vasoconstriction in healthy individuals exposed to the hypoxic environment at high altitude. Thus, it seems reasonable to suggest that respiratory symptoms associated with high altitude pulmonary edema are caused by activation of pulmonary C-fibers [59]. However, it should be pointed out that an increase in pulmonary interstitial volume is also a potent and consistent stimulus of rapidly adapting pulmonary stretch receptors in the lung, as documented by Kappagoda et al. [60]. Dyspnea and sensation of breathlessness are not always evoked when these afferents are activated by different types of chemical stimulants. This variability probably reflects the chemical nature of the stimulants, as well as the possibility that different subtypes of C-fibers encoded by different receptor proteins are activated [61].
Corollary discharge
There is a conscious awareness of the outgoing respiratory motor command to the ventilatory muscles. This sense of respiratory motor output is distinct from sensations directly related to changes in muscle length or tension and is attributed to a corollary discharge from brainstem respiratory neurons to the sensory cortex during automatic reflex breathing or from cortical motor centers to the sensory cortex during voluntary respiratory efforts [62].
Corollary discharges occur simultaneously with the primary respiratory discharges and convey information regarding the breathing effort to the sensory cortex to keep the cortex "aware" of the level of respiratory activity [2]. Corollary discharges are known to activate the cortex [63], midbrain [64] and thalamus [65]. These corollary discharges are thought to be important in shaping the sense of respiratory effort [1].
Pathophysiology of dyspnea
In the 1960s Campbell and Howell first introduced the theory of "length-tension appropriateness" to explain the sensation of dyspnea originating from the inappropriate response of the respiratory system to the outgoing motor command [66]. More recently this theory has been redefined and a mechanism based on a neuro-ventilatory dissociation [67–69] has been proposed. Dyspnea results from a dissociation between central respiratory drive and incoming afferent information from receptors in the airways, lungs and chest wall [38, 70]. A feedback linked to peripheral afferents (chest wall, lungs) modulates central respiratory drive and attenuates respiratory effort perception. On the contrary, the intensity of the dyspnea is heightened when the sensorial feedback linked to changes in respiratory pressure, airflow and volume, tension, and displacement is inappropriate to the outgoing motor command. This theory explains dyspnea associated with breathholding, the unpleasant sensation of air hunger experienced by patients receiving mechanical ventilation with small tidal volumes and low inspiratory flow rates, and the discomfort of subjects who voluntarily constrain the rate and depth of their breathing [37, 38, 57, 70].
The language of dyspnea
Based on the hypothesis that various qualities of respiratory discomfort result from different pathophysiological abnormalities, language could help to define one or more of the abnormalities responsible for breathing discomfort. The use of descriptors of dyspnea may contribute to the understanding of the mechanisms of dyspnea, and assist in identifying or predicting a specific diagnosis [71].
Using the descriptors of dyspnea, Simon et al. [72] demonstrated that normal volunteers could distinguish between the kinds of dyspnea induced by different stimuli, such as breathholding, carbon dioxide inhalation, exercise, resistive and elastic respiratory loads, and constrained tidal volume. Descriptors of dyspnea were also readily obtained in symptomatic patients with different cardiorespiratory diseases. Standardized descriptors were grouped in discrete clusters with high discriminating value among diseases [72]. Based on the hypothesis that various qualities of respiratory discomfort result from different pathophysiological abnormalities, language could help to define one or more of the abnormalities responsible for breathing discomfort [73]. 'Chest tightness', 'Work/effort', 'Unrewarded inspiration', 'Rapid breathing', 'Air hunger' are the clusters of dyspnea most frequently selected by patients with respiratory disorders and healthy subjects [71].
In healthy individuals Harver et al. [74], testing the hypothesis that descriptors of breathlessness represent distinct cognitive constructs and predicting that the use of descriptors of breathlessness by healthy subjects is the same as their use by patients with cardiopulmonary disease, showed that the relations among descriptors in healthy subjects support the contention that the association of different clusters with different diseases reflects distinct cognitive constructs that are not simply dependent on the presence of an underlying pathophysiological mechanism or on a specific disease [74]. Moreover, their results suggest that distinct qualities of breathlessness relate to different physiologic mechanisms underlying respiratory discomfort [74].
Conflict of Interest Statement
The author has no conflict of interest to declare in relation to the subject of this manuscript.
References
American Thoracic Society: Dyspnea. Mechanisms, assessment, and management: a consensus statement. Am J Respir Crit Care Med. 1999, 159: 321-340.
Buchanan GF, Richerson GB: Role of chemoreceptors in mediating dyspnea. Respir Physiol Neurobiol. 2009, 167: 9-19. 10.1016/j.resp.2008.12.002.
Grazzini M, Stendardi L, Gigliotti F, Scano G: Pathophysiology of exercise dyspnea in healthy subjects and in patients with chronic obstructive pulmonary disease (COPD). Respir Med. 2005, 99: 1403-1412. 10.1016/j.rmed.2005.03.005.
el-Manshawi A, Killian KJ, Summers E, Jones NL: Breathlessness during exercise with and without resistive loading. J Appl Physiol. 1986, 61: 896-905.
Leblanc P, Summers E, Inman MD, Jones NL, Campbell EJ, Killian KJ: Inspiratory muscles during exercise: a problem of supply and demand. J Appl Physiol. 1988, 64: 2482-2489.
O'Donnell DE, Bertley JC, Chau LK, Webb KA: Qualitative aspects of exertional breathlessness in chronic airflow limitation: pathophysiologic mechanisms. Am J Respir Crit Care Med. 1997, 115: 109-115.
Babcock MA, Pegelow DF, McClaran SR, Suman OE, Dempsey JA: Contribution of diaphragmatic power output to exercise-induced diaphragm fatigue. J Appl Physiol. 1995, 78: 1710-1719.
Grimby G, Goldman M, Mead J: Respiratory muscle action inferred from rib cage and abdominal V-P partitioning. J Appl Physiol. 1976, 41: 739-751.
Kayser B, Sliwiński P, Yan S, Tobiasz M, Macklem PT: Respiratory effort sensation during exercise with induced expiratory-flow limitation in healthy humans. J Appl Physiol. 1997, 83: 936-947.
Ward ME, Eidelman D, Stubbing DG, Bellemare F, Macklem PT: Respiratory sensation and pattern of respiratory muscle activation during diaphragm fatigue. J Appl Physiol. 1988, 65: 2181-2189.
Sliwiński P, Yan S, Gauthier AP, Macklem PT: Influence of global inspiratory muscle fatigue on breathing during exercise. J Appl Physiol. 1996, 80: 1270-1278.
Hamilton AL, Killian KJ, Summers E, Jones NL: Muscle strength, symptom intensity, and exercise capacity inpatients with cardiorespiratory disorders. Am J Respir Crit Care Med. 1995, 152: 2021-2031.
NHLBI Workshop summary: Respiratory muscle fatigue. Report of the Respiratory Muscle Fatigue Workshop Group. Am Rev Respir Dis. 1990, 142: 474-480.
Bradley TD, Chartrand DA, Fitting JW, Killian KJ, Grassino A: The relation of inspiratory effort sensation to fatiguing patterns of the diaphragm. Am Rev Respir Dis. 1986, 134: 1119-1124.
Mador MJ, Kufel TJ, Pineda L: Quadriceps fatigue after cycle exercise in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000, 161: 447-453.
Mador MJ, Kufel TJ, Pineda LA, Sharma GK: Diaphragmatic fatigue and high-intensity exercise in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000, 161: 118-123.
Polkey MI, Kyroussis D, Keilty SE, Hamnegard CH, Mills GH, Green M, Moxham J: Exhaustive treadmill exercise does not reduce twitch transdiaphragmatic pressure in patients with COPD. Am J Respir Crit Care Med. 1995, 152: 959-964.
Sinderby C, Spahija J, Beck J, Kaminski D, Yan S, Comtois N, Sliwinski P: Diaphragm activation during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001, 163: 1637-1641.
Aliverti A, Cala SJ, Duranti R, Ferrigno G, Kenyon CM, Pedotti A, Scano G, Sliwinski P, Macklem PT, Yan S: Human respiratory muscle actions and control during exercise. J Appl Physiol. 1997, 83: 1256-1269.
Sanna A, Bertoli F, Misuri G, Gigliotti F, Iandelli I, Mancini M, Duranti R, Ambrosino N, Scano G: Chest wall kinematics and respiratory muscle action in walking healthy humans. J Appl Physiol. 1999, 87: 938-946.
Aliverti A, Iandelli I, Duranti R, Cala SJ, Kayser B, Kelly S, Misuri G, Pedotti A, Scano G, Sliwinski P, Yan S, Macklem PT: Respiratory muscle dynamics and control during exercise with externally imposed expiratory flow limitation. J Appl Physiol. 2002, 92: 1953-1963.
Iandelli I, Aliverti A, Kayser B, Dellacà R, Cala SJ, Duranti R, Kelly S, Scano G, Sliwinski P, Yan S, Macklem PT, Pedotti A: Determinants of exercise performance in normal men with externally imposed expiratory flow limitation. J Appl Physiol. 2002, 92: 1943-1952.
Potter WA, Olafsson S, Hyatt RE: Ventilatory mechanics and expiratory flow limitation during exercise in patients with obstructive lung disease. J Clin Invest. 1971, 50: 910-919. 10.1172/JCI106563.
Martinez FJ, de Oca MM, Whyte RI, Stetz J, Gay SE, Celli BR: Lung-volume reduction improves dyspnea, dynamic hyperinflation, and respiratory muscle function. Am J Respir Crit Care Med. 1997, 155: 1984-1990.
Dodd DS, Brancatisano T, Engel LA: Chest wall mechanics during exercise in patients with severe chronic air-flow obstruction. Am Rev Respir Dis. 1984, 129: 33-38.
Grimby G, Elgefors B, Oxhoj H: Ventilatory levels and chest wall mechanics during exercise in obstructive lung disease. Scand J Respir Dis. 1973, 54: 45-52.
Montes de Oca M, Rassulo J, Celli BR: Respiratory muscle and cardiopulmonary function during exercise in very severe COPD. Am J Respir Crit Care Med. 1996, 154: 284-289.
Romagnoli I, Gorini M, Gigliotti F, Bianchi R, Lanini B, Grazzini M, Stendardi L, Scano G: Chest wall kinematics, respiratory muscle action and dyspnoea during arm vs. leg exercise in humans. Acta Physiol (Oxf). 2006, 188: 63-73. 10.1111/j.1748-1716.2006.01607.x.
Chonan T, Mulholland MB, Leitner J, Altose MD, Cherniack NS: Sensation of dyspnea during hypercapnia, exercise, and voluntary hyperventilation. J Appl Physiol. 1990, 68: 2100-2106. 10.1063/1.346564.
Campbell EJ, Freedman S, Clark TJ, Robson JG, Norman J: The effect of muscular paralysis induced by tubocurarine on the duration and sensation of breath-holding. Clin Sci. 1967, 32: 425-432.
Campbell EJ, Godfrey S, Clark TJ, Freedman S, Norman J: The effect of muscular paralysis induced by tubocurarine on the duration and sensation of breath-holding during hypercapnia. Clin Sci. 1969, 36: 323-328.
Castele RJ, Connors AF, Altose MD: Effects of changes in CO2 partial pressure on the sensation of respiratory drive. J Appl Physiol. 1985, 59: 1747-1751.
Banzett RB, Lansing RW, Reid MB, Adams L, Brown R: 'Air hunger' arising from increased PCO2 in mechanically ventilated quadriplegics. Respir Physiol. 1989, 76: 53-68. 10.1016/0034-5687(89)90017-0.
Banzett RB, Lansing RW, Brown R, Topulos GP, Yager D, Steele SM, Londoño B, Loring SH, Reid MB, Adams L, Nations CS: "Air hunger" from increased PCO2 persists after complete neuromuscular block in humans. Respir Physiol. 1990, 81: 1-17. 10.1016/0034-5687(90)90065-7.
Manning HL, Schwartzstein RM: Pathophysiology of dyspnea. N Engl J Med. 1995, 333: 1547-1553. 10.1056/NEJM199512073332307.
Adams L, Lane R, Shea SA, Cockcroft A, Guz A: Breathlessness during different forms of ventilatory stimulation: a study of mechanisms in normal subjects and respiratory patients. Clin Sci. 1985, 69: 663-672.
Chonan T, Mulholland MB, Cherniack NS, Altose MD: Effects of voluntary constraining of thoracic displacement during hypercapnia. J Appl Physiol. 1987, 63: 1822-1828.
Schwartzstein RM, Simon PM, Weiss JW, Fencl V, Weinberger SE: Breathlessness induced by dissociation between ventilation and chemical drive. Am Rev Respir Dis. 1989, 139: 1231-1237.
Demediuk BH, Manning H, Lilly J, Fencl V, Weinberger SE, Weiss JW, Schwartzstein RM: Dissociation between dyspnea and respiratory effort. Am Rev Respir Dis. 1992, 146: 1222-1225.
Davenport PW, Friedman WA, Thompson FJ, Franzen O: Respiratory-related cortical potentials evoked by inspiratory occlusion in humans. J Appl Physiol. 1986, 60: 1843-1848.
Liotti M, Brannan S, Egan G, Shade R, Madden L, Abplanalp B, Robillard R, Lancaster J, Zamarripa FE, Fox PT, Denton D: Brain responses associated with consciousness of breathlessness (air hunger). Proc Natl Acad Sci USA. 2001, 98: 2035-2040. 10.1073/pnas.98.4.2035.
Brannan S, Liotti M, Egan G, Shade R, Madden L, Robillard R, Abplanalp B, Stofer K, Denton D, Fox PT: Neuroimaging of cerebral activations and deactivations associated with hypercapnia and hunger for air. Proc Natl Acad Sci USA. 2001, 98: 2029-2034. 10.1073/pnas.98.4.2029.
von Leupoldt A, Dahme B: Cortical substrates for the perception of dyspnea. Chest. 2005, 128: 345-354. 10.1378/chest.128.1.345.
Evans KC, Banzett RB, Adams L, McKay L, Frackowiak RS, Corfield DR: BOLD fMRI identifies limbic, paralimbic, and cerebellar activation during air hunger. J Neurophysiol. 2002, 88: 1500-1511.
Chronos N, Adams L, Guz A: Effect of hyperoxia and hypoxia on exercise-induced breathlessness in normal subjects. Clin Sci. 1988, 74: 531-537.
Lane R, Cockcroft A, Adams L, Guz A: Arterial oxygen saturation and breathlessness in patients with chronic obstructive airways disease. Clin Sci. 1987, 72: 693-698.
Gandevia SC, Macefield G: Projection of low threshold afferents from human intercostal muscles to the cerebral cortex. Respir Physiol. 1989, 77: 203-214. 10.1016/0034-5687(89)90007-8.
Homma I, Kanamaru A, Sibuya M: Proprioceptive chest wall afferents and the effect on respiratory sensation. Respiratory Psychophysiology. Edited by: von Euler C, Katz-Salamon M. 1988, New York:Stockton Press, 161-166.
Edo H, Kimura H, Niijima M, Sakabe H, Shibuya M, Kanamaru A, Homma I, Kuriyama T: Effects of chest wall vibration on breathlessness during hypercapnic ventilatory response. J Appl Physiol. 1998, 84: 1487-1491.
Kjaer M, Hanel B, Worm L, Perko G, Lewis SF, Sahlin K, Galbo H, Secher NH: Cardiovascular and neuroendocrine responses to exercise in hypoxia during impaired neural feedback from muscle. Am J Physiol. 1999, 277: R76-R85.
Smith SA, Querry RG, Fadel PJ, Gallagher KM, Stromstad M, Ide K, Raven PB, Secher NH: Partial blockade of skeletal muscle somatosensory afferents attenuates baroreflex resetting during exercise in humans. J Physiol. 2003, 551: 1013-1021. 10.1113/jphysiol.2003.044925.
Marcora S: Perception of effort during exercise is independent of afferent feedback from skeletal muscles, heart, and lungs. J Appl Physiol. 2009, 106: 2060-2062. 10.1152/japplphysiol.90378.2008.
Scano GL: Commentaries on viewpoint: perception of effort during exercise is independent of afferent feedback from skeletal muscles, heart, and lungs. J Appl Physiol. 2009, 106: 2064-
Guz A, Noble MIN, Eisele JH, Trenchard D: Experimental results of vagal block in cardiopulmonary disease. Breathing: Hering-Breuer Centenary Symposium. Edited by: Porter R. 1971, London: Churchill Livingstone, 315-329.
Taguchi O, Kikuchi Y, Hida W, Iwase N, Satoh N, Chonan T, Takishma T: Effects of bronchoconstriction and external resisting loading on the sensation of dyspnea. J Appl Physiol. 1991, 71: 2183-2190.
Permutt S, Fessler HE, Brower RG, Kosnik E: Breathlessness in acute asthma. Breathlessness The Campbell Symposium. Edited by: Jones, Killian. 1992, Hamilton, ON: CME, 60-65.
Manning HL, Shea SA, Schwartzstein RM, Lansing RW, Brown R, Banzett RB: Reduced tidal volume increases 'air hunger' at fixed PCO2 in ventilated quadriplegics. Respir Physiol. 1992, 90: 19-30. 10.1016/0034-5687(92)90131-F.
Zhao W, Martin AD, Davenport PW: Magnitude estimation of inspiratory resistive loads by double-lung transplant recipients. J Appl Physiol. 2003, 94: 576-582.
Paintal AS: Sensation from J receptors. News Physiol Sci. 1995, 10: 238-243.
Kappagoda CT, Man GC, Teo KK: Behaviour of canine pulmonary vagal afferent receptors during sustained acute pulmonary venous pressure elevation. J Physiol. 1987, 394: 249-265.
Lee LY: Respiratory sensations evoked by activation of bronchopulmonary C-fibers. Respir Physiol Neurobiol. 2009, 167: 26-35. 10.1016/j.resp.2008.05.006.
Killian KJ, Gandevia SC, Summers E, Campbell EJ: Effect of increased lung volume on perception of breathlessness, effort, and tension. J Appl Physiol. 1984, 57: 686-691.
Shea SA, Andres LP, Shannon DC, Guz A, Banzett RB: Respiratory sensations in subjects who lack a ventilatory response to CO2. Respir Physiol. 1993, 93: 203-219. 10.1016/0034-5687(93)90006-V.
Chen Z, Eldridge FL, Wagner PG: Respiratory-associated rhythmic firing of midbrain neurones in cats: relation to level of respiratory drive. J Physiol. 1991, 437: 305-325.
Chen Z, Eldridge FL, Wagner PG: Respiratory-associated thalamic activity is related to level of respiratory drive. Respir Physiol. 1992, 90: 99-113. 10.1016/0034-5687(92)90137-L.
Campbell EJ, Howell JB: The sensation of breathlessness. Br Med Bull. 1963, 19: 36-40.
Gandevia SC: Neural mechanisms underlying the sensation of breathlessness: kinesthetic parallels between respiratory and limb muscles. Aust N Z J Med. 1988, 18: 83-91. 10.1111/j.1445-5994.1988.tb02252.x.
Zechman FJ, Wiley RL: Afferent inputs of breathing: respiratory sensation. Handbook of Physiology: the respiratory system. American Physiology Society. Edited by: Fishman AP. 1986, Bethesda, 2: 449-474.
O'Donnell DE: Breathlessness in patients with chronic airflow limitation. Mechanisms and management. Chest. 1994, 106: 904-912. 10.1378/chest.106.3.904.
Manning HL, Molinary EJ, Leiter JC: Effect of inspiratory flow rate on respiratory sensation and pattern of breathing. Am J Respir Crit Care Med. 1995, 151: 751-757.
Scano G, Stendardi L, Grazzini M: Understanding dyspnoea by its language. Eur Respir J. 2005, 25: 380-385. 10.1183/09031936.05.00059404.
Simon PM, Schwartzstein RM, Weiss JW, Fencl V, Teghtsoonian M, Weinberger SE: Distinguishable types of dyspnea in patients with shortness of breath. Am Rev Respir Dis. 1990, 142: 1009-1014.
Elliott MW, Adams L, Cockcroft A, MacRae KD, Murphy K, Guz A: The language of breathlessness. Use of verbal descriptors by patients with cardiopulmonary disease. Am Rev Respir Dis. 1991, 144: 826-832. 10.1164/ajrccm/144.4.826.
Harver A, Mahler DA, Schwartzstein RM, Baird JC: Descriptors of breathlessness in healthy individuals: distinct and separable constructs. Chest. 2000, 118: 679-690. 10.1378/chest.118.3.679.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Gigliotti, F. Mechanisms of dyspnea in healthy subjects. Multidiscip Respir Med 5, 195 (2010). https://doi.org/10.1186/2049-6958-5-3-195
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2049-6958-5-3-195