Abstract
Background
Obstructive sleep apnea-hypopnea syndrome (OSAHS) is characterized by repeated breathing pauses during sleep and is closely associated with obesity. Body fat is known to be a predictive factor for OSAHS and its severity.
Aim
To study the correlation between the severity of OSAHS and body composition measurements.
Methods
30 patients with OSAHS (21 men, 9 women, mean age 45.1 years, mean apnea-hypopnea index = 29.6/hour) were included in the study after full polysomnography. They were divided into 3 groups according to the apnea-hypopnea index (AHI): mild OSAHS (mean AHI 10.9/h), moderate OSAHS (mean AHI 23.9/h) and severe OSAHS (mean AHI 53.9/h). Body composition (body fat, body water and dry lean mass) was assessed using bioelectric impedance assay (BIA). Other measurements included neck and abdominal circumferences and body mass index (BMI). Pearson's coefficient (r) was used to express correlations between AHI and the following parameters: BMI, neck and abdominal circumferences, body fat, dry lean mass, and body water. Wilcoxon Sum-of-Ranks (Mann-Whitney) test for comparing unmatched samples was used to compare anthropometric and body composition measurements between groups.
Results
The correlation between AHI and BMI was weak (r = 0.38). AHI correlated moderately with neck circumference (r = 0.54), with neck circumference corrected by height (r = 0.60), and more strongly with body fat (r = 0.67), with body water (r = 0.69) and with abdominal circumference (r = 0.75). There was a strong negative correlation between AHI and dry lean mass (r = - 0.92). There were significant differences in body fat, body water, neck circumference corrected by height and abdominal circumference (Wilcoxon Sum-of-Ranks, p < 0.01), between mild and severe OSASH groups, but not in BMI (Wilcoxon Sumof-Ranks, W = 86.5; p = 0.17).
Conclusions
In our study, the severity of OSAHS correlated with body fat and with body water more strongly than with general and cervical obesity. Abdominal adiposity may predict OSAHS severity better than neck circumference.
Raissunto
Premesse
La sindrome dell’apnea ostruttiva del sonno (OSAHS) è caratterizzata da pause respiratorie ripetute durante il sonno ed è strettamente associata con l’obesità. È stato dimostrato che il grasso corporeo rappresenta un fattore indicativo per la presenza di OSAHS e per la relativa gravità. Scopo: Studio della correlazione tra la gravità della OSAHS ed i valori della composizione corporea
La sindrome dell’apnea ostruttiva del sonno (OSAHS) è caratterizzata da pause respiratorie ripetute durante il sonno ed è strettamente associata con l’obesità. È stato dimostrato che il grasso corporeo rappresenta un fattore indicativo per la presenza di OSAHS e per la relativa gravità. Scopo: Studio della correlazione tra la gravità della OSAHS ed i valori della composizione corporea
Risultati
Sono stati inclusi nello studio, dopo un completo esame polisonnografico, 27 pazienti affetti da OSAHS (21 uomini e 9 donne) con età media di 45,1 anni e con un indice di apnea ipopnea (AHI) di 29,6/ora. Sono stati divisi in tre gruppi in funzione dell’AHI: con OSAHS lieve (AHI medio di 10.9/ora), con OSAHS moderato (AHI medio di 23,9/ora) e con OSAHS grave (AHI medio 53,9/ora). La composizione corporeaè stata determinata usando l’analisi di impedenza bioelettrica. Altre misurazioni realizzate sono state: la circonferenza del collo e addominale, l’indice di massa corporea (BMI). Il coefficiente di Pearson (r) è stato utilizzato per esprimere le correlazioni tra AHI ed i seguenti parametri: BMI, circonferenza del collo e addominale, grasso corporeo, massa asciutta magra e acqua corporea. Il test Wilcoxon Sum-of-Ranks (Mann-Whitney) è stato usato per comparare tra i gruppi i valori di composizione corporea ed antropometrici
Metodi
Sono stati inclusi nello studio, dopo un completo esame polisonnografico, 27 pazienti affetti da OSAHS (21 uomini e 9 donne) con età media di 45,1 anni e con un indice di apnea ipopnea (AHI) di 29,6/ora. Sono stati divisi in tre gruppi in funzione dell’AHI: con OSAHS lieve (AHI medio di 10.9/ora), con OSAHS moderato (AHI medio di 23,9/ora) e con OSAHS grave (AHI medio 53,9/ora). La composizione corporea è stata determinata usando l’analisi di impedenza bioelettrica. Altre misurazioni realizzate sono state: la circonferenza del collo e addominale, l’indice di massa corporea (BMI). Il coefficiente di Pearson (r) è stato utilizzato per esprimere le correlazioni tra AHI ed i seguenti parametri: BMI, circonferenza del collo e addominale, grasso corporeo, massa asciutta magra eacqua corporea. Il test Wilcoxon Sum-of-Ranks (Mann-Whitney) è stato usato per comparare tra i gruppi i valori di composizione corporea ed antropometrici
Conclusioni
Nel nostro studio la gravità dell’OSAHS è correlata con il grasso e l’acqua corporea maggiormente che non con l’o Nel nostro studio la gravità dell’OSAHS è correlatacon il grasso e l’acqua corporea maggiormente che non con l’obesità generale e cervicale. L’adiposità addominale può costituire un indice della gravità dell’OSAHS migliore di quello della circonferenza del collo
Similar content being viewed by others
Introduction
Obstructive sleep apnea-hypopnea syndrome (OSAHS) is a common chronic condition characterized by repeated episodes of upper airway obstruction during sleep, associated with intermittent sleep hypoxemia, sleep fragmentation and potentially fatal cardio-metabolic consequences [1]. The classic risk factors for OSAHS include obesity, age, masculine sex and cervical fat deposition (neck circumference above 41 cm in women and 43 cm in men). The gold standard for the diagnosis of OSAHS is polysomnography, a complex investigation including the concomitant recording of several neurologic, respiratory and cardiovascular parameters during sleep. OSAHS is defined by an apnea-hypopnea index (AHI) of 5 or more obstructive episodes per hour associated with typical symptoms such as daytime somnolence, loud snoring, witnessed breathing pauses, or awakenings due to gasping. The diagnosis of OSAHS may be ruled at 15 or more obstructive respiratory events per hour of sleep even in the absence of sleep related symptoms, given the importance of this cutoff point in predicting complications such as increased cardiovascular risk.
OSAHS is considered mild for an AHI between 5 and 15/h, moderate for an AHI between 15 and 30 and severe for an AHI above 30/h [1, 2].
Obesity is the main risk factor for OSAHS, although sleep apnea may also be found in lean subjects. Cervical adiposity affects upper airway anatomy because of fat deposition [1, 2]. Excessive abdominal fat is the major determinant of obesity-induced hypoventilation, but it also contributes to obstructive apneas by increasing upper airway collapsibility in recumbent position because of the loss in "tracheal tug" (the normal caudal traction of the upper airways) [3]. In addition to these mechanical effects of fat deposition, the metabolic activity of the adipose tissue plays an important pathogenic role in OSAHS. Inflammatory cytokines, insulin resistance, visceral fat, atherogenic dyslipidemia and arterial hypertension are common features linking OSAHS and the metabolic syndrome, a complex condition which is associated with many cardiovascular risk factors [4].
The body mass index (BMI) is the most simple assessment tool for nutritional status and is defined as the individual's body weight divided by the square of his height. A value under 18.5 indicates under weight, a value between 18.5 and 25 is considered optimal; a value between 25 and 30 indicates that the person is overweight, while a number above 30 represents obesity. BMI alone does not reflect accurately a person's adiposity [5].
Fat mass represents 25% of the body mass. Lean mass (75%) is three quarters water and one quarter the minerals and proteins in the body (dry lean mass or cellular mass, representing 18.75% of the body mass) [6]. Body composition may be estimated using several techniques. Anthropometric methods use skinfolds or circumferences, combined in statistical models to predict body density, from which body fat may be deduced using equations. Hydrostatic (underwater) weighing is a method based on Archimedes' principle, which measures body density, with the subsequent deduction of body fat. A large number of errors may occur while using these methods [6].
The most accurate methods for body composition assessment are the isotopic methods, such as deuterium isotope dilution measurements, and total body potassium estimation using a whole body scintillation counter which detects natural body radiation produced by 40K, a marker of the cellular mass; the use of isotopic methods is limited by their accessibility [7]. Dual energy X-ray absorptiometry, or DXA (formerly DEXA), commonly cited as the current gold standard for body composition testing, uses two different types of X-ray, with the computed subtraction of fat mass [7].
Bioelectrical impedance assay (BIA) is a less accurate, but more affordable method which estimates body fat percentage: a small electrical current is sent through conductors attached to the skin and the resistance between the conductors provides a measure of body fat, body water and dry lean mass [6]. Visceral fat can be estimated by measuring the CT cross-sectional area of abdominal visceral fat [7].
Aims
The aim of this study was to correlate body composition compartments and traditional anthropometric markers of regional and general obesity with the severity of OSAHS expressed by the AHI.
Materials and methods
We selected 30 patients with OSAHS (21 men, 9 women, mean age 45.1 years) who all underwent complete overnight supervised video-polysomnography including electroencephalogram (2 channels), electrocardiogram (1 channel), electrooculogram, chin and leg electromyogram, nasal flow, thoracic and abdominal movements, snoring, body position, pulse-oximetry, and audio-video recording (SomnoLab-version 5, Weinmann, Germany). The criteria for the diagnosis of OSAHS were an apnea-hypopnea index (AHI) above 5 per hour of sleep, associated with self-reported daytime sleepiness. Only patients without clinical edema were selected for the study. The mean AHI for the whole group was 29.6/hour. Patients were divided into 3 groups according to the AHI: mild OSAHS (n = 10, mean AHI 10.9/h), moderate OSAHS (n = 10, mean AHI 23.9/h), and severe OSAHS (n = 10, mean AHI 53.9/h). Body composition (body fat, body water and dry lean mass) was assessed by bioelectric impedance assay (BIA), using a medical hand-held, battery operated bio-impedance analyzer with two main cable leads, working at a fixed frequency of 50 kHz (Bodystat 1500 - Medical 2004, Bodystat Ltd, Isle of Man). Written consent was obtained for all measurements and for data use. The results were expressed in percent of the total body mass. Other measurements included neck and abdominal circumferences and body mass index (BMI = weight in kg/height in m2). Pearson's coefficient (r) was used to express correlations between AHI and the following parameters: BMI, neck and abdominal circumferences, body fat, dry lean mass, and body water. We compared anthropometric and body composition measurements between the 3 groups (mild, moderate and severe) using the Wilcoxon Sum-of-Ranks (Mann-Whitney) test for comparing relatively small unmatched samples, with a significance threshold of p = 0.05.
Results
Patient characteristics of the overall group and of patients divided according to OSAHS severity can be found in Table 1. Mean BMI and mean age were higher in the severe OSAHS group compared to the mild and the moderate OSAHS group, but the differences were not statistically significant (p > 0.05). Body fat percentage, body water percentage, abdominal circumference, and neck circumference were significantly higher and dry lean mass was significantly lower in the severe OSAHS group compared to the mild OSAHS group (p < 0.01). Abdominal circumference and body composition compartments were also different between severe and moderate OSAHS groups (p < 0.05). Neck circumference and dry lean mass were significantly different between the mild and the moderate OSAHS groups (p < 0.05). The results of the comparison between mild, moderate and severe OSAHS using the Wilcoxon Sum-of-Ranks (Mann-Whitney) test for comparing two unmatched samples are shown in Table 2.
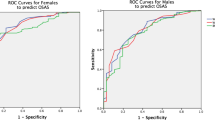
The correlation between AHI and age was weak (r = 0.34). The correlation between AHI and BMI was also weaker than expected (r = 0.38) (Figure 1). AHI correlated moderately with neck circumference (r = 0.54) (Figure 2), with neck circumference corrected for height (r = 0.60), and stronger with body fat percentage (r = 0.67), with body water percentage (r = 0.69) and with abdominal circumference (r = 0.75) (Figure 3). There was a strong negative correlation between AHI and dry lean mass percentage (r = - 0.92) (Figure 4).
Body composition compartments in the 3 groups are represented in Figure 5.
Discussion
In our study, the severity of OSAHS expressed by the apnea-hypopnea index showed a stronger correlation with body fat and with abdominal circumference than with regional and cervical obesity, which suggests that abdominal adiposity may predict OSAHS severity better than neck circumference and general body mass index.
Most of the existing evidence shows a good correlation between body fat percentage (estimated by anthropometric measurements and bio-impedance) and the severity of OSAHS [7, 8]. In one of the studies, body fat percentage estimated by bio-impedance predicted the risk for OSAHS, contributing to the pre-test probability [7]. Visceral fat determined by computed tomography seems to predict the risk for OSAHS more accurately than BMI or body fat percentage [7]. All these data are in agreement with our results, confirming the superiority of body fat percentage and visceral fat deposition over cervical and general obesity as markers for the risk and the severity of OSAHS. The role of abdominal adiposity in OSAHS severity is well known (both the mechanical and the metabolic role), but body water has been less studied.
This is the first study on body water in OSAHS and its correlation with the severity of the disease. Body water distribution is altered in OSAHS. Nocturnal pulmonary hypertension, increased atrial natriuretic peptide release, altered renin-angiotensinaldosterone activity, and high levels of endothelin could be the mechanisms of the altered fluid distribution in OSAHS, causing nocturnal polyuria, peripheral edema and hemoconcentration [10].
We selected patients without any clinical edema, in order to ensure a higher accuracy of body water assessment using BIA. The significant difference in body water between mild and severe OSAHS and the strong positive correlation between body water and AHI suggest a degree of subclinical edema in the severe OSAHS patients.
Fluid retention and altered fluid distribution are not only consequences of sleep apnea, but they may contribute to the pathogenesis and the severity of upper airway resistance. It has been demonstrated that overnight rostral fluid displacement, both spontaneous (related to prolonged diurnal sitting) and induced by lower body positive pressure, may play a role (previously unrecognized) in the pathogenesis of obstructive sleep apnea in nonobese men, independently of body weight. The mechanism is increased upper airway resistance caused by upper airway edema consecutive to fluid migration from the legs to the neck [11, 12]. Our data are in agreement with these findings and add to the current knowledge the fact that fluid retention correlates with the severity of OSAHS. It remains however unclear to what extent the increased body water percentage is the consequence or the cause of sleep apnea severity.
Another unclear aspect is the role of gender in the relationship between body composition and the severity of OSAHS. In our study, a comparison between men and women regarding the body composition in relationship with the severity of OSAHS was not possible, because of the small number of female patients ([9] females vs. 21 males).
The very strong negative correlation between dry lean mass and AHI suggests a possible role played by muscle depletion in upper airway collapsibility. Unfortunately, our study could not discriminate the role of body fat as a confounder on body water and on dry lean mass, because the small size of our case series made multiple regression analysis unfeasible.
Conclusions
We conclude that the severity of OSAHS correlates with body fat and with body water more strongly than with general and cervical obesity and that abdominal adiposity may predict OSAHS severity better than neck circumference.
Future studies carried out on larger groups should focus on the role of body composition compartments as independent predictors of OSAHS and its severity.
Conflict of interests statement
Neither author has any conflict of interest to declare in relation to the subject matter of this manuscript
References
American Academy of Sleep Medicine. International classification of sleep disorders. Diagnostic and coding manual. 2005, Westchester, IL: American Academy of Sleep Medicine, 2
Phillipson EA, Sleep disorders: Textbook of respiratory medicine. Edited by: Murray JF, Nadel JA. 1988, Philadelphia, PA: WB Saunders, 1841-1860.
Van de Graaff WB: Thoracic influence on upper airway patency. J Appl Physiol. 1988, 65: 2124-2131.
Vgontzas AN, Bixler EO, Chrousos GP: Sleep apnea is a manifestation of the metabolic syndrome. Sleep Med Rev. 2005, 9: 211-224. 10.1016/j.smrv.2005.01.006.
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F: Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes. 2008, 32: 959-966. 10.1038/ijo.2008.11.
Siri SE: Body composition from fluid spaces and density: analysis of methods. Techniques for measuring body composition. Edited by: Brozek J, Henschel A. 1961, Washington, DC: National Academy of Sciences, National Research Council, 223-234.
Lee SY, Gallagher D: Assessment methods in human body composition. Curr Opin Clin Nutr Metab Care. 2008, 11: 566-572. 10.1097/MCO.0b013e32830b5f23.
Oğretmenoğlu O, Süslü AE, Yücel OT, Onerci TM, Sahin A: Body fat composition: a predictive factor for obstructive sleep apnea. Laryngoscope. 2005, 115: 1493-1498. 10.1097/01.mlg.0000172204.82314.c3.
Mercanti LB, Bezerra ML, Fernandes Filho J, Struchiner CJ: Dermatoglyphics and body composition in obstructive sleep apnea. Arq Neuropsiquiatr. 2004, 62: 858-864. 10.1590/S0004-282X2004000500022.
O'Hearn DJ, Gold AR, Gold MS, Diggs P, Scharf SM: Lower extremity edema and pulmonary hypertension in morbidly obese patients with obstructive sleep apnea. Sleep Breath. 2009, 13: 25-34. 10.1007/s11325-008-0200-z.
Redolfi S, Yumino D, Ruttanaumpawan P, Yau B, Su MC, Lam J, Bradley TD: Relationship between overnight rostral fluid shift and obstructive sleep apnea in nonobese men. Am J Respir Crit Care Med. 2009, 179: 241-246.
Chiu KL, Ryan CM, Shiota S, Ruttanaumpawan P, Arzt M, Haight JS, Chan CT, Floras JS, Bradley TD: Fluid shift by lower body positive pressure increases pharyngeal resistance in healthy subjects. Am J Respir Crit Care Med. 2006, 174: 1378-1383. 10.1164/rccm.200607-927OC.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lovin, S., Bercea, R., Cojocaru, C. et al. Body composition in obstructive sleep apneahypopnea syndrome bio-impedance reflects the severity of sleep apnea. Multidiscip Respir Med 5, 44 (2010). https://doi.org/10.1186/2049-6958-5-1-44
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2049-6958-5-1-44