Abstract
The epidemiology of Candida infections has changed over the last two decades: The number of patients suffering from such infections has increased dramatically and the Candida species involved have become more numerous as Candida albicans is replaced as an infecting agent by various non-C. albicans species (NAC). At the same time, additional antifungal agents have become available. The different Candida species may vary in their susceptibility for these various antifungals. This draws more attention to in vitro susceptibility testing. Unfortunately, several different test methods exist that may deliver different results. Moreover, clinical breakpoints (CBP) that classify test results into susceptible, intermediate and resistant are controver- sial between CLSI and EUCAST. Therefore, clinicians should be aware that interpretations may vary with the test system being followed by the microbiological laboratory. Thus, knowledge of actual MIC values and pharmacokinetic properties of individual antifungal agents is important in delivering appropriate therapy to patients
Similar content being viewed by others
Introduction
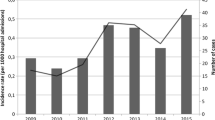
In 2001, McNeil et al. reported that (in the USA) "from 1980 through 1997, the annual number of deaths in which an invasive mycosis was listed on the death certificate (multiple-cause mortality) increased from 1557 to 6534" (Table 1, Figure 1) [1]. Augmentation of fungal infections had been published earlier i.e. by Beck-Sague and Jarvis [2] and Edmond et al. [3] for the USA and by Lamagni et al. [4] for England and Wales (Figure 2). There are several possible reasons for this change. An important one might be the increase in lifespan in the populations of the developed world and the age related loss of immune-competence. An increase of systemic fungal infections is probably also due to more intensive treatment schemes for hematological and oncological patients causing prolonged neutropenic phases. Finally, more effective antibacterial treatments allow patients with infections to survive longer without necessarily overcoming the underlying diseases and thus leaving them susceptible to other opportunistic infections. Eggimann et al. [5] summarized prior surgery, acute renal failure, previous yeast colonization, neutropenia, antibacterial therapy, parenteral nutrition, and central venous catheters as risk factors for invasive Candidia infections.
Mortality in the united states, 1980-1997, 'due to candidiasis, and other mycoses in persons infected and persons not infected with HIV [1].
Annual rates of candidosis laboratory reports, by sex (England and Wales: 1990-9) [4].
Change in Epidemiology
The increase in incidence of Candida infections barely preceded the introduction of fluconazole in 1990. This azole agent combined good activity against Candida albicans with reduced toxicity as compared to i.e. polyene anti-fungals. It is orally and parentally available and has a reliable that means linear pharmacokinetic profile [6], which makes it easy to handle. Not surprisingly, fluconazole became the agent of choice for many fungal infections as well as for prophylactic purposes, at that time often being applied in rather low doses. Although there is inconclusive evidence, many experts in the field believe that it was the selective pressure exerted by this therapeutic concept that caused changes in the epidemiology [7]. While in earlier years, C. albicans was responsible most of the invasive fungal infections (Table 2) [8], gradually more and more non-C. albicans species (NAC) were found as offending agents (Table 3) [9–16]. While the data show similar tendencies in the prevalence of various Candida ssp. worldwide, considerable differences can be observed as well. However, these do not lend themselves to further interpretation since significant differences in the demographics of the patients observed seem to be obvious. This change in prevalence of various Candida spp. is nevertheless of clinical importance, since individual species vary in their susceptibility to various antifungal agents. While national and international surveillance is important to recognize trends in epidemiology it is, however, of utmost importance to gain knowledge about the local epidemiology as this information should guide the empiric therapy of patients.
Susceptibility Testing
Some of the already cited and many other studies have also reported on the in-vitro susceptibility of Candida spp. For various reasons it is difficult to assess the various results. There are currently several test methods for performing these assays. Standardized methods have been published by the Clinical and Laboratory Standards Institute (CLSI) of the USA [17, 18] and by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [19]. The two broth dilution methods are not identical as methodological differences include glucose concentration, inoculum size, shape of microtitration wells (flat or round), and end-point reading (visual or spectrophotometric). However, it appears that they result in similar MIC levels for polyenes, azoles and echinocandins for identical isolates with a few noted exceptions [20–23]. This is especially true if isolates with defined resistance mechanisms are being tested [22, 23]. However, some "drug/bug" combinations seem to offer particular test problems i.e. caspofungin and C. glabrata [22]. Moreover, EUCAST (and for that matter Etest) results have a tendency for one to two dilution steps lower MIC values [20, 23]. There are also some commercially available test devices that have been tested in their performance. A high degree of correlation with the reference methods was found for the Etest by various authors [22, 23]. The percentage of strains classified as resistant in vitro by the EUCAST procedure and as susceptible in vitro by the VITEK 2 system was 2.6%, and as resistant by the CLSI method and as susceptible by the VITEK 2 was 1.6% (very major error) [24]. The difference observed for the Vitek 2 results and CLSI and EUCAST is driven by the fact that there are differences in clinical breakpoints (CBP) suggested by the two organizations. However these results indicate that although the CBP of EUCAST and CLSI are significantly different, currently only few strains are affected by this difference.
CBP are used to classify MIC results into susceptible (S), intermediate (I) (CLSI for some strange reason "susceptible dose dependent"; S-DD), and resistant (R), respectively. This has complicated to assess and compare studies were only percentages of S, I and R are published. The same is true for published MIC50/90 values, as very different MIC distributions might be behind these numbers. To illustrate this further, two very different fictitious distributions resulting in the same MIC50/90 values are given with Figure 3. Therefore, meaningful surveillance data should be published as MIC distributions. That allows for evaluation of the results even at a later date when i.e. CBP had been changed as has happened in the past. To circumvent the problem with differences in CBP published by various organizations, it has been suggested to use epidemiological cut -off values to distinguish between wild type (WT) organisms without any resistance mechanisms and non-wild type (N-WT) strains with higher MIC values that are thought or known to possess a resistance mechanism [22, 25]. This would put in vitro test results on the safe side as long as the particular species is a target for the antifungal agent in question. Obviously, CBP should not divide WT distributions as this will cause arbitrary test results. Monitoring the development of N-WT strains in surveillance studies allows one to analyze the spread of resistance mechanisms.
Resistance Mechanisms
A number of different resistance mechanisms have been described in Candida spp. Often, several of these mechanisms are combined to result in a stepwise development of clinically relevant resistance. Resistance to i.e. fluconazole can be caused i.e. by alterations in sterol biosynthesis, by mutations in the drug target enzyme, sterol 14α-demethylase, which lowers its affinity for fluconazole, by increased expression of the ERG11 gene encoding for this enzyme, or by overexpression of genes coding for membrane transport proteins of the ABC transporter (CDR1/CDR2) or the major facilitator (MDR1) superfamilies [26].
Similarly Candida isolates were found with reduced susceptibility to echinochandins that showed mutations in selected regions of fks1, the gene encoding the echinocandin target enzyme 1-3-b-D-glucan synthase [27]. In particular, mutations of the serine at position 645 and also, in some cases, at position 641 have been associated with decreased susceptibility to echinochandins [28].
It should be noted that there is at least for fluconazole a clear relation between MIC values, pharmacokinetics (expressed in serum AUC) and outcome (Figure 4) [29]. Since resistance development against i.e. echinocandines so far is very limited, it is obviously very difficult to establish such a correlation. This problem is further aggravated by the fact that current antifungals still leave much to be desired as they i.e. do not reach the cure rates of antibacterial agents for susceptible bacteria. Moreover, the described resistance mechanisms were at least in individual cases associated with clinical failure of the involved patients [30–35]. This has raised concern over the CBP as suggested by the CLSI. For a discussion of this subject see [36, 37].
Mortality rate stratified by tertiles and fluconazole Auc/Mic at 24 h (P = 0.09 using logistic regression controlling for time to initiation of fluconazole therapy) [29].
Resistance surveillance
Among the worldwide largest and long run surveillance systems is the ARTEMIS program. In a recent publication [9], comparative susceptibility data for fluconazole and voriconazole for more than 190,000 isolates collected from 2001 to 2007 were provided and analysis of resistance rates by year, geographic location, hospital location, and specimen type for selected species were included. The data were collected employing the CLSI disk diffusion method and are summarized in Table 4. They show that fluconazole resistance has to be expected especially in C. glabrata, krusei, guillermondii, famata, inconspicua, rugosa, norvegensis and some other rarer species. There seem to be some but no complete crossresistance with voriconazole which leaves the latter as an option in appropriate cases. A trend toward increased resistance over the most recent 3 years (2005 to 2007) was observed for voriconazole and some species with low prevalence such as C. famata (1.1% to 5.7%), C. norvegensis (0.0% to 6.9%), C. lipolytica (0.0% to 11.1%), and C. pelliculosa (14.3% to 16.7%). However, there was no trend toward increased resistance to voriconazole among the fluconazole-resistant species C. glabrata, C. krusei, C. guilliermondii, C. rugosa, and C. inconspicua.
MIC distributions for echinocandins have been published by Pfaller et al. (Table 5) [39]. The results of this study demonstrate the comparable spectrum and potency of all three available echinocandin antifungals against a large collection of clinically important Candida spp. It also highlights the fact that species such as C. parapsilosis and C. guilliermondii exhibit decreased susceptibilities to all three echinocandins. The clinical relevance of these elevated MICS currently remains doubtful.
The data collected by the SENTRY surveillance program were published as MIC50/90 values and interpreted results according to CLSI, only [39, 40]. However, this study included most important antifungals. An excerpt for C. parapsilosis is given with Table 6. German data were published in the same way [15], not offering significant differences to the SENTRY results with the exception of a high degree of flucytosine resistance in C. krusei and C. tropicalis. Finally, susceptibility data for rare Candida isolates have been collected by Diekema et al. [41] (Table 7) and chen et al. [42] that might help to guide therapy in these cases.
Conclusion
Meanwhile in vitro methods are available to assess reliably the susceptibility of fungal isolates. There are, however, considerable differences in the evaluation of the results, as CLSI and EUCAST breakpoints vary. If isolates with known resistance mechanisms that have been shown to be clinically relevant at least in individual cases shall not be categorized as susceptible, some CLSI CBP need to be reconsidered. Despite the fact that a number of new antifungals are nowadays available, clinical results of antifungal therapy leave much to be desired. Hence, optimization of empiric therapy according to the local epidemiological situation and reevaluation of the therapeutic regimen when susceptibility results become available should carefully be followed. With our expanded knowledge on pharmacokinetics of antifungal compounds, MIC data could be valuable at least when treating invasive fugal infections. More information about MICs of clinical isolates and outcome of the particular patients would be helpful to establish further and validate current CBP.
References
McNeil MichaelM, Nash StephanieL, Hajjeh RanaA, Phelan MaureenA, Conn LauraA, Plikaytis BrianD, Warnock DavidW: Trends in Mortality Due to In- vasive Mycotic Diseases in the United States, 1980–1997. Clin Infect Dis 2001,33(5):641–647. 10.1086/322606
Beck-Sague C, Jarvis WR: Secular trends in the epidemiology of nosocomial fungal infections in the United States, 1980–1990. National Nosocomial Infections Surveillance System. J Infect Dis 1993, 167: 1247–1251. 10.1093/infdis/167.5.1247
Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, Wenzel RP: Nosocomial bloodstream infections in United States hospitals: a three-year analysis. Clin Infect Dis 1999, 29: 239–244. 10.1086/520192
Lamagni TL, Evans BG, Shigematsu M, Johnson EM: Emerging trends in the epidemiology of invasive mycoses in England and Wales (1990–9). Epidemiol Infect 2001,126(3):397–414.
Eggimann P, Garbino J, Pittet D: Epidemiology of Candida species infections in critically ill non-immuno-suppressed patients. Lancet Infect Dis 2003, 3: 685–702. 10.1016/S1473-3099(03)00801-6
Washton H: Review of fluconazole: a new triazole antifungal agent. Diagn Microbiol Infect Dis 1989,12(4 Suppl):229S-233S.
Leroy Olivier, Gangneux Jean-Pierre, Montravers Philippe, Mira Jean-Paul, Gouin François, Sollet Jean-Pierre, Carlet Jean, Reynes Jacques, Rosenheim Michel, Regnier Bernard, Lortholary Olivier, for the AmarCand Study Group: Epidemiology, management, and risk factors for death of invasive Candida infections in critical care: A multicenter, prospective, observational study in France (2005–2006). Crit Care Med 2009,37(5):1612–18. 10.1097/CCM.0b013e31819efac0
Pfaller MA, Diekema DJ: Epidemiology of Invasive Candidiasis: a Persistent Public Health Problem. Clin Microbiol Rev 2007,20(1):133–163. 10.1128/CMR.00029-06
Pfaller MA, Diekema DJ, Gibbs DL, Newell VA, Ellis D, Tullio V, Rodloff A, Fu W, Ling TA, the Global Antifungal Surveillance Group: Results from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997 to 2007: a 10.5-Year Analysis of Susceptibilities of Candida Species to Fluconazole and Voriconazole as Determined by CLSI Standardized Disk Diffusion. J Clin Microbiol 2010,48(4):1366–1377. 10.1128/JCM.02117-09
Pfaller MA, Moet GJ, Messer SA, Jones RN, Castanheira M: Candida bloodstream infections: comparison of species distributions and antifungal resistance patterns in community-onset and nosocomial isolates in the SENTRY Antimicrobial Surveillance Program, 2008–2009. Antimicrob Agents Chemother 2011,55(2):561–6. 10.1128/AAC.01079-10
Horn DavidL, Dionissios Neofytos, Anaissie EliasJ, Fishman JayA, Steinbach WilliamJ, Olyaei AliJ, Marr KierenA, Pfaller MichaelA, Chi-Hsing Chang, Webster KarenM: Epidemiology and Outcomes of Candidemia in 2019 Patients: Data from the Prospective Antifungal Therapy Alliance Registry. Clin Infect Dis 2009, 48: 1695–703. 10.1086/599039
Ostrosky-Zeichner Luis, Rex JohnH, Pappas PeterG, Hamill RichardJ, Larsen RobertA, Horowitz HaroldW, Powderly WilliamG, Newton Hyslop, Kauffman CarolA, John Cleary, Mangino JulieE, Jeannette Lee: Antifungal Susceptibility Survey of 2,000 Bloodstream Candida Isolates in the United States. Antimicrob Agents Chemother 2003,47(10):3149–3154. 10.1128/AAC.47.10.3149-3154.2003
Cisterna R, Ezpeleta G, Telleria O, Guinea J, Regueiro B, Garcia-Rodriguez J, Esperalba J, The Spanish Candidemia Surveillance Group: Nationwide Sentinel Surveillance of Bloodstream Candida Infections in 40 Tertiary Care Hospitals in Spain. J Clin Microbiol 2010,48(11):4200–4206. 10.1128/JCM.00920-10
Arendrup MC, Bruun B, Christensen JJ, Fuursted K, Johansen HK, Kjaeklgaard P, Knudsen JD, Kristensen L, Moller J, Nielsen L, Rosenvinge FS, Roder B, Schønheyder HC, Thomsen MK, Truberg K: National surveillance of fungemia in Denmark (2004–2009). J Clin Microbiol 2011,49(1):325–34. 10.1128/JCM.01811-10
Fleck Ralf, Dietz Annebärbel, Hof Herbert: In vitro susceptibility of Candida species to five antifungal agents in a German university hospital assessed by the reference brothmicrodilution method and Etest. J Antimicrob Chemother 2007, 59: 767–771. 10.1093/jac/dkl555
Borg-von Zepelin M, Kunz L, Rüchel R, Reichard U, Weig M, Gross U: Epidemiology and antifungal susceptibilities of Candida spp. to six antifungal agents: results from a surveillance study on fungaemia in Germany from July 2004 to August 2005. J Antimicrob Chemother 2007,60(2):424–8. 10.1093/jac/dkm145
M27-A3, Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard - Third Edition Clinical and Laboratory Standards Institute, Wayne, USA 2008.
M44A2, Method for Antifungal Disk Diffusion Susceptibility Testing of Yeasts; Approved Guideline-Second Edition Clinical and Laboratory Standards Institute, Wayne, USA 2009.
Subcommittee on Antifungal Susceptibility Testing (AFST) of the ESCMID European Committee for Antimicrobial Susceptibility Testing (EUCAST): EUCAST Definitive Document EDef 7.1: method for the determination of broth dilution MICs of antifungal agents for fermentative yeasts. Clin Microbiol Infect 2008, 14: 398–405.
Cuenca-Estrella Manuel, Lee-Yang Wendy, Ciblak MeralA, Arthington-Skaggs Emilia Mellado BethA, Warnock DavidW, Rodriguez-Tudela JuanL: Comparative Evaluation of NCCLS M27-A and EUCAST Broth Microdilution Procedures for Antifungal Susceptibility Testing of Candida Species. Antimicrob Agents Chemother 2002,46(11):3644–3647. 10.1128/AAC.46.11.3644-3647.2002
Espinel-Ingroff A, Barchiesi F, Cuenca-Estrella M, Pfaller MA, Rinaldi M, Rodriguez-Tudela JL, Verweij PE: International and Multicenter Comparison of EUCAST and CLSI M27-A2 Broth Microdilution Methods for Testing Susceptibilities of Candida spp. to Fluconazole, Itraconazole, Posaconazole, and Voriconazole. J Clin Microbiol 2005,43(8):3884–3889. 10.1128/JCM.43.8.3884-3889.2005
Arendrup Maiken Cavling, Garcia-Effron Guillermo, Lass-Flörl Cornelia, Lopez Alicia Gomez, Rodriguez-Tudela Juan-Luis, Cuenca-Estrella Manuel, Perlin DavidS: Echinocandin Susceptibility Testing of Candida Species: Comparison of EUCAST EDef 7.1, CLSI M27- A3, Etest, Disk Diffusion, and Agar Dilution Methods with RPMI and IsoSensitest Media. Antimicrob Agents Chemother 2010,54(1):426–439. 10.1128/AAC.01256-09
Pfaller MA, Castanheira M, Diekema DJ, Messer SA, Moet GJ, Jones RN: Comparison of European Committee on Antimicrobial Susceptibility Testing (EUCAST) and Etest Methods with the CLSI Broth Microdilution Method for Echinocandin Susceptibility Testing of Candida Species. J Clin Microbiol 2010,48(5):1592–1599. 10.1128/JCM.02445-09
Cuenca-Estrella Manuel, Gomez-Lopez Alicia, Alastruey-Izquierdo Ana, Bernal-Martinez Leticia, Cuesta Isabel, Buitrago MariaJ, Rodriguez-Tudela JuanL: Comparison of the VITEK 2 Antifungal Susceptibility System with the CLSI and the EUCAST Broth Microdilution Reference Methods and with the Sensititre Yeast-One and the Etest Techniques for the Detection in Vitro of Antifungal Resistance in Yeasts. J Clin Microbiol 2010, 48: 1782–1786. 10.1128/JCM.02316-09
Arendrup Maiken Cavling, Kahlmeter Gunnar, Rodriguez-Tudela Juan Luis, J Peter Donnelly: Breakpoints for Susceptibility Testing Should Not Divide WildType Distributions of Important Target Species. Antimicrobial Agents Chemother 2009,53(4):1628–1629. 10.1128/AAC.01624-08
Morschhäuser J: The genetic basis of fluconazole resistance development in candida albicans. Biochim Biophys Acta 2002, 1587: 240–248.
Park S, Kelly R, Kahn JN, Robles J, Hsu M-J, Register E, Li W, Vyas V, Fan H, Abruzzo G, Flattery A, Gill G, Chrebet G, Parent SA, Kurtz M, Teppler H, Douglas CM, Perlin DS: Specific substitutions in the echinocandin target Fks1p account for reduced susceptibility of rare laboratory and clinical Candida sp. isolates. Antimicrob Agents Chemother 2005,49(8):3264–73. 10.1128/AAC.49.8.3264-3273.2005
Balashov SV, Park S, Perlin DS: Assessing resistance to the echinocandin antifungal drug caspofungin in candida albicans by profiling mutations in FKs1. Antimicrob Agents Chemother 2006, 50: 2058–63. 10.1128/AAC.01653-05
Pai ManjunathP, Turpin RobinS, Garey KevinW: Association of Fluconazole Area under the Concentration-Time curve/Mic and Dose/Mic Ratios with Mortality in Nonneutropenic Patients with can- didemia. Antimicrob Agents Chemother 2007,51(1):35–39. 10.1128/AAC.00474-06
Hernandez S, Lopez-Ribot JL, Najvar LK, Mccarthy DoraI, Bocanegra Rosie, Graybill JohnR: Caspofungin resistance in Candida albicans: correlating clinical outcome with laboratorysusceptibility testing of three isogenic isolates serially obtainedfrom a patient with progressive Candida esophagitis. Antimicrob Agents Chemother 2004, 48: 1382–3. 10.1128/AAC.48.4.1382-1383.2004
Katiyar S, Pfaller M, Edlind T: Candida albicans and candida glabrata clinical isolates exhibiting reduced echinocandin susceptibility. Antimicrob Agents Chemother 2006, 50: 2892–4. 10.1128/AAC.00349-06
Laverdiere M, Lalonde RG, Baril JG, Sheppard DonaldC, Park Steven, Perlin DavidS: Progressive loss of echinocandin activity following prolonged use for treatment of candida albicans oesophagitis. J Antimicrob Chemother 2006, 57: 705–8. 10.1093/jac/dkl022
Miller CD, Lomaestro BW, Park S, Perlin DavidS: Progressive esophagitis caused by candida albicans with reduced susceptibility to caspofungin. Pharmacotherapy 2006, 26: 877–80. 10.1592/phco.26.6.877
Hakki M, Staab JF, Marr KA: Emergence of a candida krusei isolate with reduced susceptibility to caspofungin during therapy. Antimicrob Agents Chemother 2006, 50: 2522–4. 10.1128/AAC.00148-06
Krogh-Madsen M, Arendrup MC, Heslet L, Knudsen Jenny Dahl: Amphotericin B and caspofungin resistance in candida glabrata isolates recovered from a critically ill patient. Clin Infect Dis 2006, 42: 938–44. 10.1086/500939
Arendrup MaikenC, Cuenca-Estrella Manuel, Donnelly J Peter, Lass-Flo"rl Cornelia, Rodriguez-Tudela JuanL: Association of Fluconazole Pharmacodynamics with Mortality in Patients with candidemia. Antimicrob Agents Chemother 2009,53(6):2704–2705. 10.1128/AAC.01411-08
Baddley JohnW, Ostrosky-Zeichner Luis, Bhavnani SujataM, Andes DavidR: Authors' Reply. Antimicrob Agents Chemother 2009,53(6):2705–2706.
Pfaller MA, Boyken L, Hollis RJ, Kroeger J, Messer SA, Tendolkar S, Diekema DJ: In Vitro susceptibility of Invasive Isolates of candida spp. To Anidulafungin, caspofungin, and Micafungin: Six Years of Global Surveillance. J Clin Microbiol 2008,46(1):150–156. 10.1128/JCM.01901-07
Messer ShawnA, Moet GaryJ, Kirby JeffreyT, Jones RonaldN: Activity of contemporary Antifungal Agents, Including the Novel Echinocandin Anidulafun- gin, Tested against candida spp., cryptococcus spp., and Aspergillus spp.: Report from the sENTRY Antimicrobial Surveillance Program (2006 to 2007). J Clin Microbiol 2009,47(6):1942–1946. 10.1128/JCM.02434-08
Messer ShawnA, Jones RonaldN, Moet GaryJ, Kirby JeffreyT, Mariana Castanheira: Potency of Anidulafungin Compared to Nine Other Antifungal Agents Tested against Candida spp., Cryptococcus spp., and Aspergillus spp.: Results from the Global SENTRY Antimicrobial surveillance Program (2008). J Clin Microbiol 2010,48(8):2984–2987. 10.1128/JCM.00328-10
Diekema DJ, Messer SA, Boyken LB, Hollis RJ, Kroeger J, Tendolkar S, Pfaller MA: In Vitro Activity of seven systemically Active Antifungal Agents against a Large Global collection of Rare candida species as Determined by cisi Broth Microdilution Methods. J Clin Microbiol 2009,47(10):3170–3177. 10.1128/JCM.00942-09
Chen SCA, Marriott D, Playford EG, Nguyen Q, Ellis D, Meyer W, Sorrell TC, Slavin M, the Australian candidaemia study: candidaemia with uncommon candida species: predisposing factors, outcome, antifungal susceptibility, and implications for management. Clin Microbiol Infect 2009, 15: 662–669. 10.1111/j.1469-0691.2009.02821.x
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rodloff, A., Koch, D. & Schaumann, R. Epidemiology and antifungal resistance in invasive candidiasis. Eur J Med Res 16, 187 (2011). https://doi.org/10.1186/2047-783X-16-4-187
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2047-783X-16-4-187