Abstract
Introduction
In utero and/or childhood environmental tobacco smoke exposure is well known to adversely affect lung function and to depreciate child's health in many ways. Fewer studies have assessed the long-term effects on COPD development and disease severity in later adulthood.
Methods
COPD patients were interviewed using a structured questionnaire regarding their personal as well as the smoking habits of their parents. Data were compared with the disease history, e.g. COPD exacerbation rate, and their lung function data.
Results
Between 2003 and 2004 COPD patients were recruited a) in a private practice specialized in pulmonary medicine (n = 133) and b) in a hospital (n = 158). 75% of their fathers and only 15.4 of all mothers smoked regularly. COPD patients from smoking mothers had lower FEV1 predicted than those raised in household without maternal smoking exposure: 39.4 ± 9.5% vs. 51.9 ± 6.0% (P = 0.037). Fathers had no effect on FEV1 regardless if they are smokers or non-smokers. Rate of severe exacerbations requiring hospitalization remained unaffected by parental second hand smoke exposure.
Conclusion
Maternal smoking negatively affects lung function of their offspring even in late adulthood when they develop COPD. It even aggravates the cumulative effect of active cigarette consumption. Clinical course of the COPD remained unaffected.
Similar content being viewed by others
Introduction
Second hand smoking is well known for its deteriorating effects in man. It increases significantly recurrent colds, cough and phlegm, throat problems, and the presence of respiratory symptoms by roughly a factor of 2 [1, 2]. It even has been linked to increase the risk for lung cancer by the factor of 1.3, particularly when the exposure occurs before the age of 25 [3]. Cigarette smoking is still quite common in many parts of the world. In parallel, exposure to second-hand smoke continues to be widespread despite declines in smoking in developed countries and despite evidence of serious health effects in infants and children. In addition to whatever effects direct and postnatal second-hand tobacco smoke exposure have on the occurrence of asthma, bronchitis, cardio-vascular diseases and impaired levels and growth of lung function in adolescents, there is an underlying alteration in the prenatal and early postnatal development of the structural and mechanical characteristics of the lung that contribute substantially to these deficits. These developmental effects are important contributors to the future risks for impaired pulmonary function in adolescence [4, 5].
While the detrimental effect of parental smoking exposure on the respiratory health of children is well known since years [6], information on the long-lasting consequence on human health, particularly regarding the development of diseases like chronic obstructive pulmonary disease (COPD) is sparse [7, 8]. Consequently, the purpose of this study was to assess the risk of environmental smoke exposure at home during childhood a) for COPD severity, b) for disease instability defined as higher exacerbation rate in later adulthood, and c) whether it might have an add-on effect to yearlong active smoke exposure.
Patients and Methods
This study has been approved by the ethics committee of the Saxonian Physician Association, Dresden/Germany (Code No.: EK-AMG-89/2003). Patients who refuse to participate or who were unable to understand the written informed consent form were excluded.
A structured 11 pages questionnaire was used to question prospectively COPD patients for their family and social history, previous occupation and possible occupational exposure status, parental and personal smoking habits. Diseases during childhood and adolescence were recorded as well as the year of COPD diagnosis and frequency of exacerbations, defined as those that required hospitalization and treatment with antibiotics and/or systemic corticosteroids [9]. At the time of the interview, following parameter were gathered from the patient: anthropometric data, dyspnoea using MRC-scale, lung function, blood gas analysis, and a current medication. To exclude concurrent diseases as defined below, patients were examined using EKG, echocardiography, X-ray of the chest.
Inclusion criteria were: COPD according to the GOLD (Global obstructive Lung Disease [10]) definition of all stages, age ≥ 30 years, negative reversibility testing (FEV1 < 12% and < 200 ml, 30 minutes after inhalation with salbutamol 400 μg). Patients were regarded non-eligible, when the following applied: severe concomitant co-morbidities in an acute deterioration or in chronic disease stage such as heart failure (NYHA ≥ 3), myocardial infarction ≤ 6 months, pneumonia and other acute infectious disease, asthma as defined by GINA (Global Initiative for Asthma [11]), interstitial and other lung disease except COPD, chronic kidney disease requiring dialysis, sleep apnoea syndrome, any malignant diseases, occupational disease of the lung (e.g. silicosis, asbestosis). For this bicentre trial COPD patients were recruited a) when admitted to the in-patient or out-patient unit of our centre (Robert-Koch-Hospital), an academic teaching hospital specialized in the management of acute and chronic pulmonary diseases including lung cancer, and b) in a private practice of a pulmonologist.
Statistical Evaluation
On the basis of earlier studies - whereas we choose paediatric studies due lack of comparable investigations with COPD patients - we calculated a sample size of 250 patients [12–14]. The software SPSS Version 11.5 was used for all statistical calculations. Unless otherwise stated data were compared using a t-test, and Mann Witney-U and the Chi2 tests. All efficacy analysis used the intent-to-treat population, defined as all included patients. The study was designed to show the influence of parental (father or mother) second hand exposure on the development of COPD. Within the predefined error probability, a significant influence was accepted at P ≤ 0.05.
Results
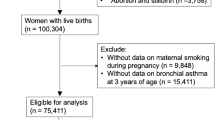
In 2003 and 2004 we included 133 COPD patients from the practice and another 158 from the Robert-Koch-Hospital. Patients were admitted because of routine check-up or due to an acute exacerbation. We interviewed and tested the latter shortly before dismissal after their clinical improvement in order to avoid that the acute worsening biased data quality. To proof that clinical instability, defined as frequent exacerbations, is caused by parental smoking, the COPD cohort was divided in a group lacking any severe exacerbation (see definition above) within the last 24 years (1980-2004) and in a group having at least 1 severe exacerbation. The 24 -year cut-off resulted from the length of the archival patient records. Both groups were similar regarding mean age, gender distributions begin of chronic cigarette smoking and frequency of pulmonary diseases during childhood (Table 1).
In contrast to never-exacerbaters (NE), patients with ≥ 1 exacerbation (1E) reported that they had to be hospitalized about 3-times (mean) within the last 24 years because of severe deterioration of their disease. At the time of interview 58% of all patients were exsmokers (= non-smoking ≥ 1 year), 22% smoked actively and 19.2% claimed to be live long non-smoker.
The fathers smoked longer and more cigarettes than the mothers (Table 2). Paternal smoking habits had no influence on FEV1 of our COPD patients. In contrast, patients who's mothers smoked, exhibit significantly (P = 0.037) lower FEV1 values than those raised without maternal smoke exposure (Figure 1). Hospitalization rate due to COPD exacerbations remained unaffected through smoking parents: Difference due to smoking vs. non-smoking fathers P = 0.999, and smoking vs. non-smoking mothers P = 0.547. No significant differences between HE and 1E were found (data not shown).
Discussion
Ca.10% of adult smokers demonstrate an increased decline of lung function with age [15, 16]. The effects of passive smoke exposure vary with genetic factors, gender, race and exposure to other pollutants [7, 8]. Exposure to environmental tobacco smoke during childhood and subsequent active smoking in later adulthood both further aggravate symptoms and have a negative effect on lung function, among others [17, 18].
This paper focuses on the effects of second-hand smoke in addition of direct exposure on the respiratory health of the lung function and frequency of exacerbations in COPD patients. Once birth cohort studies on this subject are unrealistic due to necessary long observation time, we choose an interview based approach in which COPD patients comment on their active cigarette smoking habits and second hand exposure during their childhood at home. Interestingly, maternal smoking resulted in further lung function decline in our patients, and thus has an additional effect to active smoking in later life. Although fathers smoked much more than theirs wives, paternal smoking was no contributor to the future risk for impaired pulmonary function. Based on earlier observations [19], we may speculate: Because mostly mothers but not their fathers raise children, the exposure to maternal cigarette smoke are much more intense than from paternal second hand smoke. Our patients could not know whether their mothers also smoked during pregnancy from obvious reasons. Assuming that this was the case in most instances, intra-uterine and inhalant second hand exposure may have contributed to lung function reduction as observed in our cohort [20]. Jurado et al [21] and others reported that maternal smoking increased the risk of wheezing with colds, cough with phlegm and asthma in the offspring up to 3-fold. The detrimental effect depended on the intensity of smoke exposure and if it occurs only prenatal, postnatal or both. Smoking fathers did not exert this effect or their influence was significantly smaller which was confirmed by our data [22–24].
Our results are very well in concurrence with published data indicating that direct and postnatal secondhand tobacco smoke exposure promotes the incidence of asthma and bronchitis, and impairs the growth of the lung [20, 25]. Tobacco smoke alters very early in life prenatal and early postnatal development of the structural and mechanical characteristics of the lung that contribute substantially to these deficits. These developmental effects are therefore important contributors to the future risks for impaired pulmonary function and COPD [26, 27].
Lower FEV1 in the cohort with smoking mothers did not correlate with increased rate of severe exacerbations requiring hospitalization. This amazes considering, that patients with FEV1 < 50% predicted has an 2.6-fold higher risk to become again hospitalized due to an COPD exacerbation [28]. Inversely reduces a FEV1 increase of 10% the exacerbation rate by 28% [29]. FEV1 values are by and large poor predictors for future exacerbations rates, because many patients with low FEV1 may be stable and patients with lower disease stages may frequently exacerbate [30, 31]. Good therapeutic management as demonstrated in studies using tiotropium bromide and inhaled corticosteroids or smoking cessation may help reduce exacerbations [9, 32–34]. All these factors could have diminished in our study a possible influence of environmental tobacco smoke exposure in childhood.
Our study has various disadvantages. Although the data were collected prospectively, we relayed predominantly on individual mental capacity for incidents dating back decades in the past. Objective methods to verify patient's strength to remember this kind of information is, to our knowledge, not on hand. We omitted therefore intelligence tests and related assessments. The study design did not allow the differentiation between in utero and post-natal smoke exposure. We only can assume that smoking mothers smoke also during pregnancy and not just after the delivery of their child. According to previous reports, about one third of smoking mothers stopped during pregnancy [35]. But after successful smoking cession during pregnancy approximately 10 - 60% of all women relapse to smoking during the next 6 months. 34% of all children are exposed to maternal smoking [35, 36]. Considering these data, one can reckon that over 70% of our patients reporting second hand smoke exposure during childhood were also exposed in utero.
We hereby demonstrate the reliability of data collection from COPD patients even if the event date back many decades, and we confirmed for the first time with this approach that maternal smoke exposure effects COPD severity, which even adds up to active smoking.
Conflicts of interest
The study was supported by Boehringer Ingelheim Pharma KG, Germany.
References
Ho SY, Lam TH, Chung SF, Lam TP: Cross-sectional and prospective associations between passive smoking and respiratory symptoms at the workplace. Ann Epidemiol 2007, 17: 126–31. 10.1016/j.annepidem.2006.06.010
Ho LM, Hedley AJ, Adab P, Fielding R, McGhee SM, Leung GM, Abaronson-Daniel L: Secondhand smoke and respiratory ill health in current smokers. Tob Control 2005, 14: 307–14. 10.1136/tc.2005.011775
Asomaning K, Miller DP, Liu G, Wain JC, Lynch TJ, Su L, Christiani DC: Second hand smoke, age of exposure and lung cancer risk. Lung Cancer 2008, 61: 13–20. 10.1016/j.lungcan.2007.11.013
Tager IB: The effects of second-hand and direct exposure to tobacco smoke on asthma and lung function in adolescence. Paediatr Resp Rev 2008, 9: 29–37. 10.1016/j.prrv.2007.11.006
Eisner MD, Wang Y, Haight TJ, Balmes J, Hammond SK, Tager IB: Secondhand smoke exposure, pulmonary function, and cardiovascular mortality. Ann Epidemiol 2007, 17: 364–73. 10.1016/j.annepidem.2006.10.008
Cook DG, Strachan DP: Summary of effects of parental smoking on the respiratory health of children and implications for research. Thorax 1999, 54: 357–66. 10.1136/thx.54.4.357
Radon K, Nowak D: Passivrauchen - aktueller Stand des Wissens. Dtsch Med Wschr 2004, 129: 157–62.
Radon K, Büsching K, Heinrich J, Wichmann H-E, Jörres R, Magnussen H, Nowak D: Passive smoking exposure: a risk factor for chronic bronchitis and asthma in adults? Chest 2002, 122: 1086–90. 10.1378/chest.122.3.1086
Wedzicha JA, Calverley PMA, Seemungal TAR, Hagan G, Ansan Z, Stockley RA: The prevention of COPD exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med 2008, 177: 19–26.
GOLD Executive Committee: Global initiative for chronic obstructive lung disease. 2007.
Bateman ED, GINA Executive and Science Committee, Global Initiative for Asthma (GINA): Global strategy for asthma management and prevention. Bethesda, USA; 2008.
Horstman D, Kotesovec F, Vitnerova N: Pulmonary functions of school children in highly polluted Northern Bohemia. Arch Environ Health 1997, 52: 56–62. 10.1080/00039899709603801
Corbo GM, Agabiti N, Forastiere F: Lung function in children and adolescents with occasional exposure to environmental tobacco smoke. Am J Respir Crit Care Med 1996, 154: 695–700.
Cook DG, Strachan DP, Carey IM: Health effects of passive smoking. 9. Parental smoking and spirometric indices in children. Thorax 1998, 53: 884–93. 10.1136/thx.53.10.884
Anthonisen NR, Lindgren PG, Tashkin DP, Kanner RE, Scanlon PD, Connett JE: Bronchodilator response in the lung health study over 11 years. Eur Respir J 2005, 26: 45–51. 10.1183/09031936.05.00102604
The Lung Health Study Group: Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary disease. N Engl J Med 2000, 343: 1902–9.
Landau L: Tobacco smoke exposure and tracking of lung function into adult life. Paediatr Resp Rev 2008, 9: 39–43. 10.1016/j.prrv.2007.11.002
Stein RT, Holberg CJ, Sherrill D, Wright AL, Morgan WJ, Taussig L, Martinez FD: Influence of parental smoking on respiratory symptoms during the first decade of life. The Tucson Children's Respiratory Study. Am J Epidemiol 1999, 149: 1030–7. 10.1093/oxfordjournals.aje.a009748
David GL, Koh W-P, Lee H-P, Yu MC, London SJ: Childhood exposure to environmental tobacco smoke and chronic respiratory symptoms in non-smoking adults: The Singapore Chinese Health Study. Thorax 2005, 60: 1052–8. 10.1136/thx.2005.042960
Edwards CA, Osman LM, Godden DJ, Campbell DM, Douglas JG: Relationship, between birth weight and adult lung function: controlling for maternal factors. Thorax 2003, 58: 1061–5. 10.1136/thorax.58.12.1061
Jurado D, Munoz C, Luna Jde D, Munoz-Hoyos A: Maternal smoking more determinant than paternal smoking on the respiratory symptoms of young children? Respir Med 2005, 99: 1138–44. 10.1016/j.rmed.2005.02.014
Mannino DM, Homa DM, Redd SC: Involuntary smoking and asthma severity in children. Date from the third national health and nutrition examination survey. Chest 2002, 122: 409–15. 10.1378/chest.122.2.409
Li Y-F, Gilliland FD, Berhane K, McConnell R, Gauderman WJ, Rappaport EB, Peters JM: Effects of in utero and environmental tobacco smoke exposure on lung function in boys and girls with and without asthma. Am J Respir Crit Care Med 2009, 162: 2097–104.
Leuenberger P, Schartz J, Ackermann-Liebrich U, Blaser K, Bolognini G, Bongard JP, Brandli O, Braun P, Bron C, Brutsche M: Passive smoking exposure in adults and chronic respiratory symptoms (SAPALDIA Study). Am J Respir Crit Care Med 1994, 150: 1222–8.
Gilliland FD, Berhane K, McConnell R, Gauderman WJ, Vora H, Rapaport EB, Avol E, Peters JM: Maternal smoking during pregnancy, environmental tobacco smoke exposure and childhood lung function. Thorax 2000, 55: 271–6. 10.1136/thorax.55.4.271
Gold DR, Wang X, Wypij D, Speizer FE, Ware JH, Dockery DW: Effects of cigarette smoking on lung function in adolescent boys and girls. N Engl J Med 1996, 335: 931–7. 10.1056/NEJM199609263351304
Wang X, Wypij D, Speizer FE, Ware JH, Ferris BG, Dockery DW: A longitudinal study of the effects of parental smoking on pulmonary function n children 6–18 years. Am J Respir Crit Care Med 1994, 149: 1420–5.
Cao Z, Ong KC, Eng P, Tan WC, Ng TP: Frequent hospital readmissions for acute exacerbation of COPD and their associated factors. Respirology 2006, 11: 188–95. 10.1111/j.1440-1843.2006.00819.x
Miravitlles M, Guerrero T, Mayordomo T, Sanchez-Agudo C, Nicolau L, Segu JL: Factors associated with increased risk of exacerbation and hospital admission in a cohort of ambulatory COPD patients: a multiple logistic regression analysis. The EOLO study group. Respiration 2000, 67: 495–501. 10.1159/000067462
Soler-Cataluna JJ, Martinez-Garcia MA, Roman Sanchez P, Salcedo E, Navarro M, Ochando R: Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005, 60: 925–31. 10.1136/thx.2005.040527
Celli BR, Thomas NE, Anderson JA, Ferguson GT, Jenkins C, Jones PW, Vestbo J, Knobil K, Yates J, Calverley PMA: Effect of pharmacotherapy on rate of decline of lung function in COPD: results from the TORCH study. Am J Respir Crit Care Med 2008, 178: 332–8. 10.1164/rccm.200712-1869OC
Anzueto A, Sethi S, Martinez FD: Exacerbations of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2007, 4: 554–64. 10.1513/pats.200701-003FM
Powrie DJ, Wilkinson TM, Donaldson GC, Jones PW, Scrine K, Viel K, Kesten S, Wedzicha JA: Effect of tiotropium on sputum and serum inflammatory markers and exacerbations in COPD. Eur Respir J 2007, 30: 472–8. 10.1183/09031936.00023907
Foreman MG, DeMeo DL, Hersh CP, Reilly JJ, Silverman EK: Clinical determinants of exacerbations in severe, early-onset COPD. Eur Respir J 2007, 30: 1124–30. 10.1183/09031936.00009307
Lelong N, Kaminski M, Saurel-Cubizolles MJ, Bouvier-Colle MH: Postpartum return to smoking among usual smokers who quit during pregnancy. Eur J Public Health 2001, 11: 334–9. 10.1093/eurpub/11.3.334
Röske K, Hannöver W, Thyrian JR, Grempel J, Rumpf H-J, John U, Hapke U: Warum Frauen nach der Geburt ihres Kindes wieder mit dem Rauchen anfangen (Why women postpartum resume smoking). Gesundheitswesen 2006, 68: 171–5. 10.1055/s-2006-926639
World Health Organization: WHO report of an expert committee: Definition and diagnosis of pulmonary disease with special reference to chronic bronchitis and emphysema. WHO Techn Rep Ser 1961, 213: 14–9.
Burge S, Wedzicha JA: COPD exacerbations: definition and classifications. Eur Respir J 2003, 41: 46s-53s.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beyer, D., Mitfessel, H. & Gillissen, A. Maternal smoking promotes chronic obstructive lung disease in the offspring as adults. Eur J Med Res 14 (Suppl 4), 27 (2009). https://doi.org/10.1186/2047-783X-14-S4-27
Published:
DOI: https://doi.org/10.1186/2047-783X-14-S4-27