Abstract
Bioinformatics is the application of omics science, information technology, mathematics and statistics in the field of biomarker detection. Clinical bioinformatics can be applied for identification and validation of new biomarkers to improve current methods of monitoring disease activity and identify new therapeutic targets. Acute lung injurt (ALI)/Acute respiratory distress syndrome (ARDS) affects a large number of patients with a poor prognosis. The present review mainly focused on the progress in understanding disease heterogeneity through the use of evolving biological, genomic, and genetic approaches and the role of clinical bioinformatics in the pathogenesis and treatment of ALI/ARDS. The remarkable advances in clinical bioinformatics can be a new way for understanding disease pathogenesis, diagnosis and treatment.
Similar content being viewed by others
Review
Introduction
In recent years, there is a great increase in genomics and other molecular research which produced a tremendous amount of information related to molecular biology [1–3]. Meantime, various powerful data mining and statistical bioinformatics methods have been propagated for identifying, prioritizing and classifying robust and generalizable biomarkers with high discriminatory ability [4], and some online bioinformatics data libraries, such as Enzyme, KEGG, Gene Ontology, NCBI Taxonomy, SwissProt and TrEMBL were generated for the store and management of data. Bioinformatics now entails the creation and advancement of databases, algorithms, computational and statistical techniques and theory to solve formal and practical problems arising from the management and analysis of biological data.
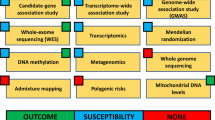
Clinical bioinformatics is a new emerging science combining clinical information, (including patients’ complaints, history, clinical symptoms and signs, physicians’ examinations, biochemical analysis, imaging profiles, pathologies), omics science, mathematics, information technology and library data together. It may play a potentially important role in the discovery of biomarkers, which will facilitate the diagnosis of disease, as well as treatment. A commonly used definition of a biomarker is “a characteristic that is objectively measured and evaluated as an indicator of normal biological process, pathogenic processes, or pharmacologic responses to a therapeutic intervention” [5]. Clinical bioinformatics is also a new way to focus on the combination of clinical symptoms and signs with human tissue-generated bioinformatics to get deep and full understand of the risk factors, pathogenesis and progress of human disease. Recent technological developments in genomics, proteomics, metabolomics, are allowing researchers to take an unbiased ‘big-picture’ approach to further elucidate the molecular pathogenesis of lung injury [6] (Figure 1). Recent years, clinical bioinformatics have been widely applied in the investigation of various kinds of diseases including acute lung injury.
The optimum pattern of clinical bioinformatics in ALI/ARDS. We get clinical information including symptoms, physical signs, medical history, lung function or images from the patients. On the other hand, we draw bioinformation from their blood, BALF or tissue. Then, the clinical information and bioinformation should be validated and complemented with each other in order to detect effective and powerful biomarkers. Only in this way, the bioinformatics technologies can be helpful.
Acute lung injury (ALI)/acute respiratory distress syndrome (ARDS) remains a major cause of high morbidity, mortality, and health care costs in critically ill patients [7]. ALI/ARDS is an acute life-threatening form of hypoxemic respiratory failure, characterized by lung tissue edema and injury, inflammatory responses, and compromised gas exchange following macrophage activation, surfactant dysfunction, and epithelial destruction. Inflammatory cells could be activated to produce a large number of mediators in the early stage of the disease, resulting in injury to both the vascular endothelium and the alveolar epithelium [8, 9]. Injury to the alveolar-capillary barrier increases permeability of the alveolar wall, increases accumulation of inflammatory cells and cytokines, and impairs alveolar fluid clearance, resulting in accumulation of protein-rich edema in the alveolar space [9].
The incidence of ALI/ARDS was reported to be 80 per 100,000 person-years with a mortality rate of 40% in United States [10]. A prospective study conducted in Chinese pediatric intensive care units indicated that the incidence of ARDS in critically ill patients was 2.7% with a mortality rate of 44.8% [11]. The reported incidence of pediatric ARDS in US was about 9.5% [12], with the overall mortality rate of 22% [13]. Over the past two decades, a variety of interventions and intensive care strategies have been used in treating patients with ALI/ARDS. However, only low tidal volume ventilation accompanied with fluid management has been shown to be beneficial in improving morbidity and mortality [14]. There is an urgent need to identify and validate disease-specific biomarkers and novel therapeutic strategies for ALI/ARDS.
Application of bioinformatics in ALI/ARDS
Genomics study in ALI is an approach to detect associated genetic variations, or gene polymorphisms, which may contribute to ALI susceptibility, severity or prognosis in a racial- and ethnic-specific manner. Examples of this approach include microarray based genome-wide expression analyses [15] and genotype detection for specific gene [16]. Although genome-wide expression profiling is an excellent method for generating long lists of candidates, it is proving to be more difficult to develop follow-on approaches to select critical genes. Then, if specific gene is supposed to be involved in the pathogenesis of ALI/ARDS, genotyping by PCR or sequencing can be applied to validate the significance of those suspected genes. Proteomics captures a comprehensive set of expressed proteins in a cell or organism to understand biological function of cells or organs [17–19]. Commonly used methods for current proteomics studies include two-dimensional gel electrophoresis (2-DE) followed by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS), liquid chromatography coupled to electrospray ionization tandem MS (LC-ESI MS/MS), surface-enhanced laser desorption/ionization coupled to TOF MS (SELDI-TOF MS), capillary electrophoresis coupled to MS, and microarrays [19]. In the pulmonary proteomic studies, bronchoalveolar lavage fluid (BALF), lung tissue, blood and alveolar cells have been used extensively.
The collection of global metabolic data and their interpretation (both spectral and biochemical) with modern spectroscopic techniques and appropriate statistical approaches is called “metabolic profiling” or “metabolomics” [20–22]. It is an emerging component of the systems biology approach for the discovery of clinically relevant biomarkers and potential therapeutic targets [23]. The most often applied technology is nuclear magnetic resonance (NMR) and mass spectrometry [24–26]. Since NMR spectrometry can identify and quantify multiple metabolites from a single liquid or solid sample and it’s cost effective and robust, it proved to be very useful in metabolomics studies.
Biomarker development in ALI/ARDS
Genomics
There are several publications reviewed the application of genomics in the study of ALI. In 2002, Marshall and his colleagues provide the first evidence of a genetic influence in ARDS, suggesting an important role for angiotensin converting enzyme (ACE) [16]. In this study, a total of 358 patients were enrolled including 96 patients fulfilling American/European Consensus Committee criteria for ARDS, 174 coronary artery bypass graft (CABG) controls and 88 non-ARDS but require mechanical ventilation patients in the intensive care unit (ICU). DNA was extracted from whole blood samples and ACE genotype was determined by three-primer polymerase chain reaction amplification. This study detected that the frequency of the DD genotype and the D allele was markedly increased in patients with ARDS compared with both the CABG and ICU comparison groups and the healthy population sample [16].
Similarly, Gong, et al demonstrated that -308GA promoter polymorphism in the TNF-a gene was associated with the mortality of ARDS [27]. SNPs of 43 Toll like receptor-related genes were identified and one of these genes was demonstrated to be associated with susceptibility to organ dysfunction and death in patients with sepsis [28]. Later, pre–B-cell colony-enhancing factor (PBEF) was found significantly increased in the expression profiling in animal models of ALI and in human ALI. In this study, multiple technologies including PCR, microarray analysis and some proteomic measurement methods were used. This combination of various technologies in bioinformatics study is important and helpful [29].
However, different from these traditional epidemiological studies in at risk populations, Marzec.et al first applied positional cloning and gene sequencing to identify candidate susceptibility genes and SNP polymorphism. They demonstrated that the -617 A SNP of Nrf2 (NF-E2 related factor 2) had a significantly higher risk for developing ALI after major trauma [30]. Then a large-scale candidate gene genotypings were carried out in a cohort of critically ill subjects with trauma to identify ALI risk variants after major trauma. Five SNPs were found to have a significant association with ALI, of which two SNPs in ANGPT2 (rs1868554 and rs2442598) replicated the significant association with ALI. And furthermore, the top associated SNPs were tested in a multicenter case-control population [31]. In a two-stage discovery/validation study, the commonly occurring FAS haplotype including FAS21541T and FAS9325A was significantly associated with ALI susceptibility and increased FAS mRNA expression in peripheral leukocytes in response to innate immune stimulation [32]. A complete summary of all published applications of genetics in the study of ALI/ARDS is far beyond the scope of this review. Table 1 provides a summary, with references, of some of the most recently or interesting applications of genetics in the diagnosis, susceptibility or prognosis of ALI/ARDS [31–37].
Among these identified genes, some of them were well demonstrated to play critical roles in the development of ALI/ARDS. NADPH oxidase contributed to the production of reactive oxygen species, which is able to induce a cell death response in oxidative stress. NADPH oxidase 1 was reported to act as an important mediator of acute lung injury mediated by oxidative stress, particularly in alveolar cells. NOX1-generated ROS are largely responsible for alveolar cell death and subsequent lung injury through JNK and ERK pathways [38]. Angiopoietin-2 (ANGPT2) has been implicated in pulmonary vascular leak syndromes including ALI and sepsis in both animal and human studies [39, 40], while recently, two ANGPT2 SNPs (rs2442598 and rs1868554) were found to be strongly associated with the development of ALI in patients with major trauma [31]. However, studies are warranted to further elucidate the characterization of ANGPT2 genetic variation and expression. Fas pathway has been investigated as a potential contributor to the inflammation and alveolar epithelial cell apoptosis observed in the lungs of patients with ALI [41, 42]. SP-B enhances the rate of phospholipid absorption to the alveolar air/water interface [43], decreases surface tension by interfering with the attractive forces acting between water molecules [44] and has anti-inflammatory properties [45]. However, the others were seldom reported and futher studies are needed to validate their functions in ALI/ARDS.
Gene expression profiles represent only a small fraction of the complexity in an organism. On the other hand, gene expression data obtained by the microarray analysis are usually moderately correlated with the expression levels of corresponding protein products due to the post-transcriptional regulation. Thus, extrapolation of protein expression on the basis of microarray-based gene expression measurements must be validated by direct measurement of the protein [15]. Then proteomics comes.
Proteomics
Proteomics captures a nearly comprehensive set of expressed proteins in a cell or organism, which determine how a cell or organism functions. Proteomics become more practical and feasible for researchers in the field of pulmonary medicine using BALF, lung tissue, and exhaled breath condensates as the source of protein analysis [46]. In 2003, Bowler et al first applied the proteomic approach in the BALF, plasma and lung edema fluid in ALI/ARDS. In this paper, the author reported that although many of the proteins were demonstrated to have increased or decreased relative intensity in the plasma and EF of ALI patients compared with normal subjects, a limitation to the 2-DE proteomics approach is that it is not easy to quantify all changes in relative protein expression among a large number of samples. The author mentioned that the proteomics approach may be complementary to microarray studies [47].
Shotgun proteomics in BALF was analyzed and 870 different proteins were identified, including surfactant, proteases, and serum proteins. However, because of the several limitations of the 2DE method to detect particular classes of proteins [48], it can only be treated as an excellent screening tool to initially characterize a sample of mostly unknown protein composition, and additional methods, including isolation of subpopulations of proteins and further refinement of the methodologies must be cooperated to identify specific proteins [49]. Then, through the combined application of SELDI-TOF, 2-DE and western blot analysis, apolipoprotein A1, and S100 calcium-binding proteins A8 and A9 were detected to increase in the inflammatory BALF [50].
Following these studies, quantitative proteomic analysis was then used to profile the changes in protein expression in the lungs at the onset and during the course of acute lung injury. Computational analysis as used to map complex protein interactions in the lung fluids and study how these interactions changed during the course of ARDS. This approach to protein network analysis identified novel mediators of acute lung injury and protein pathways were redundant and involved in multiple biological processes [51].
Table 2 provides a summary of the proteomic study in ALI/ARDS from 2009-2011 [52–58]. Caveolin-1 is involved in PMN adhesion, chemotaxis, and epithelial and endothelial cell apoptosis/senescence which accelerated lung injury in the early stage. However, cav-1 may be beneficial in the late stage through anti-fibrosis [59]. MMPs are a family of zinc-dependent proteinases which expressed by all cell types relevant to ARDS pathogenesis including alveolar epithelial cells, PMNs, macrophages, and fibroblasts. Many studies implicate MMPs in the injurious process as well ALI/ARDS, which may mainly contribute to its capability of degrading all components of the extracellular matrix [60, 61]. Vascular endothelial growth factor (VEGF) and its receptors are critical in the regulation of both vascular permeability and endothelial cell survival. However, the role of VEGF and related molecules in ALI/ARDS is controversial [62]. PAI-1 is an endogenous inhibitor of the plasminogen activators. Studies reported that elevated level of PAI-1 is an independent risk factor for mortality and adverse clinical outcomes for ALI patient [63]. RAGE is a multi-ligand-binding receptor that can bind advanced glycation end products, amyloid β-peptide, S100 proteins, and high-mobility group box-1. RAGE-ligand interaction results in intracellular signaling, which leads to activation of the proinflammatory transcription factor nuclear factor-κB (NF-κB) [64, 65]. Study indicated that RAGE may be useful as a biological marker of alveolar type I cell injury [66]. TNF-alpha and IL-8 are also well-validated inflammatory cytokines in ALI/ARDS [57]. Figure 2 integrated these factors together to show their potential roles in the pathogenesis of ALI/ARDS.
Metabolomics
Although the amplification of quantitative metabolomics in clinic bioinformaticsis in its infancy, it has been increasingly used recently. It is a unique tool of discovery because it identifies multiple endogenous markers, and it changes over time which can be predictive of clinical outcome and therapeutic response [67, 68]. The ability of magnetic resonance imaging (MRI) and metabolic NMR were investigated to detect and quantify inflammation-mediated lung injury [69]. Recently, proton nuclear magnetic resonance (1 H-NMR) based quantitative metabolomics with subsequent computational analysis was applied to investigate the plasma metabolic changes associated with sepsis-induced ALI. Several metabolites including glutathione, adenosine, phosphatidylserine, and sphingomyelin were found different between patients with ALI and healthy subjects. Additionally, computational network analysis was carried out to investigate a distinct metabolic pathway for each metabolite [24]. Moreover, there is another case-control study conducted on plasma samples from six albumin-treated and six saline-treated patients to measure the metabolic changes after albumin treatment. This study showed that blood albumin levels normalized and oxygenation improved with albumin treatment compared to saline treatment. In this study, 1 H-NMR spectroscopy was introduced to characterize systemic metabolic responses and identify patients’ unique response to pharmacologic therapy and appealed to play a potential role in the guiding treatment and reducing healthcare cost [68].
In summary, ALI/ARDS is a complex disease which can be initiated by a diverse array of precipitating factors and involving the interplay of both the environment and genetic factors. However, numerous environmental agents can induce common pathological changes, including damage to endothelial and epithelial cells, infiltration of inflammatory cells, cytokine release and so on. Those common biological pathways may be controlling generalized responses to injury and repair which cannot distinguish the type of lung injury across different models. On the other hand, susceptibility to ALI/ARDS is also different among patients with same conditions. Clinical models have identified risk factors and laboratory testing to evaluate severity, guide clinical therapy and tell prognosis. However, these strategies remain imprecise. The application of bioinformatics enables us to identify the individual expression patterns as well as the injury-specific pattern, thus may facilitate therapy and predict prognosis. Besides, in the absence of significant insights into disease pathogenesis, comprehensive bioinformatics technologies may help us to get deep understanding of such complex and life-threatening illness thus may provide novel therapeutic targets. Finally, there are several available samples that can be used in the bioinformatics study of the lung, such as exhaled breath gas, blood, lung tissue, pleural effusion and BALF, which may largely facilitate the biomarker research.
Conclusion
The genetic and proteomic approach to study ALI/ARDS in clinical setting is still in an early stage, while some important data have been generated. There is a great need of further exploratory studies to better understand the molecular mechanisms and pathophysiology of ALI/ARDS. Much effort is also needed to validate whether these biomarkers and drug targets are really useful in early detection, prediction, and so are prevention and treatment of lung diseases. The most important issue to apply clinical bioinformation for target and biomarker identification and validation should to integrate bioinformatics from genomics, proteomics and metabolomics with clinical informatics and findings. We should also think the value and role of clinical bioinformatics in clinical research and study on ALI/ARDS to benefit personalized medicine and patient prognosis.
Different from other informatics, clinical bioinformatics should focus more on clinical informatics, including patient complaints, history, therapies, clinical symptoms and signs, physician's examinations, biochemical analyses, imaging profiles, pathologies and other measurements [70]. For example, a recent study developed a digital evaluation scoring system to translate disease complexity of patient information, clinical data, standard laboratory evaluations, imaging data and symptoms into the digital [71]. This particular study tried to combine clinical informatics with protein profiles generated from antibody arrays to evaluate the disease-specific, severity-associated, duration-related biomarkers. Although the understanding of bioinformatics, clinical bioinformatics, and clinical informatics remains limited among clinicians, we believe clinical bioinformatics will have a significant impact on critical care medicine and public health. Since clinical bioinformatics is a multidisciplinary field, which combined clinical informatics, omics science, information technology, mathematics and statistics together, we suggest the cooperation of clinicians and technologists in this field. Progress in understanding of disease heterogeneity through the use of evolving biological, genomic, and genetic approaches should provide major new insights into the pathogenesis and treatment of ALI. Any effective and novel intervention generated from clinical bioinformatics may prevent or improve the high mortality and morbidity of ALI/ARDS.
References
Sarah JS, Damian AB, Joseph OD, Jeffrey DB, Issam EN: Bioinformatics Methods for Learning Radiation-Induced Lung Inflammation from Heterogeneous Retrospective and Prospective Data. J Biomed Biotechnol 2009. 10.1155/2009/892863
Lau A, Chiu JF: Biomarkers of Lung-Related Diseases: Current Knowledge by Proteomic Approaches. J Cell Physiol 2009, 221: 535–543. 10.1002/jcp.21893
Hogewega P, Hespera B: Interactive instruction on population interactions. Comput biol med 1978, 8: 319–327. 10.1016/0010-4825(78)90032-X
Baumgartner C, Osl M, Netzer M, Baumgartner D: Bioinformatic-driven search for metabolic biomarkers in disease. J Clin Bioinforma 2011, 1: 1–10. 10.1186/2043-9113-1-1
De Gruttola VG, Clax P, DeMets DL, Downing GJ, Ellenberg SS, Friedman L, Gail MH, Prentice R, Wittes J, Zeger SL: Considerations in the evaluation of surrogate endpoints in clinical trials. summary of a National Institutes of Health workshop. Control Clin Trials 2001, 22(5):485–502. 10.1016/S0197-2456(01)00153-2
Lam E, dos Santos CC: Advances in molecular acute lung injury/acute respiratory distress syndrome and ventilator-induced lung injury: the role of genomics, proteomics, bioinformatics and translational biology. Curr Opin Crit Care 2008, 14: 3–10. 10.1097/MCC.0b013e3282f42211
Rubenfeld GD, Herridge MS: Epidemiology and outcomes of acute lung injury. Chest 2007, 131: 554–562. 10.1378/chest.06-1976
Ware LB, Matthay MA: Medical progress - The acute respiratory distress syndrome. New Engl J Med 2000, 342: 1334–1349. 10.1056/NEJM200005043421806
Tomashefski JF: Pulmonary pathology of acute respiratory distress syndrome. Clin Chest Med 2000, 21: 435. 10.1016/S0272-5231(05)70158-1
Goss CH, Brower RG, Hudson LD, Rubenfeld GD: Incidence of acute lung injury in the United States. Crit Care Med 2003, 31: 1607–1611. 10.1097/01.CCM.0000063475.65751.1D
Hu X, Qian S, Xu F, Huang B, Zhou D, Wang Y, Li C, Fan X, Lu Z, Sun B: Incidence, management and mortality of acute hypoxemic respiratory failure and acute respiratory distress syndrome from a prospective study of Chinese paediatric intensive care network. Acta Paediatr 2010, 99: 715–721.
Zimmerman JJ, Akhtar SR, Caldwell E, Rubenfeld GD: Incidence and outcomes of pediatric acute lung injury. Pediatrics 2009, 124: 87–95. 10.1542/peds.2007-2462
Flori HR, Glidden DV, Rutherford GW, Matthay MA: Pediatric acute lung injury: prospective evaluation of risk factors associated with mortality. Am J Respir Crit Care Med 2005, 171: 995–1001. 10.1164/rccm.200404-544OC
Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome New Engl J Med 2000, 342: 1301–1308.
Schena M, Shalon D, Davis RW, Brown PO: Quantitative monitoring of gene expression patterns with a complementary DNA microarray. Science 1995, 270: 467–470. 10.1126/science.270.5235.467
Marshall RP, Webb S, Bellingan GJ, Montgomery HE, Chaudhari B, McAnulty RJ, Humphries SE, Hill MR, Laurent GJ: Angiotensin converting enzyme insertion /deletion polymorphism is associated with susceptibility and outcome in acute respiratory distress syndrome. Am Respir Crit Care Med 2002, 166: 646–650. 10.1164/rccm.2108086
Phizicky E, Bastiaens PIH, Zhu H, Snyder M, Fields S: Protein analysis on a proteomic scale. Nature 2003, 422: 208–215. 10.1038/nature01512
Hanash S: Disease proteomics. Nature 2003, 422: 226–232. 10.1038/nature01514
Karvunidis T, Mares J, Thongboonkerd V, Matejovic M: Recent progress of proteomics in critical illness. Shock 2009, 31: 545–552. 10.1097/SHK.0b013e3181986eab
Serkova NJ, Niemann CU: Pattern recognition and biomarker validation using quantitative 1 H-NMR-based metabolomics. Expert Rev Mol Diagn 2006, 6: 717–731. 10.1586/14737159.6.5.717
Nicholson JK, Lindon JC, Holmes E: “Metabonomics”: understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic data. Xenobiotica 1999, 29: 1181–1189. 10.1080/004982599238047
Griffin JL, Shockcor JP: Metabolic profiles of cancer cells. Nat Rev Cancer 2004, 4: 551–561. 10.1038/nrc1390
Wishart DS: Quantitative metabolomics using NMR. Trends Analytical Chem 2008, 27: 228–236. 10.1016/j.trac.2007.12.001
Stringer KA, Serkova NJ, Karnovsky A, Guire K, Paine R, Standiford TJ: Metabolic consequences of sepsis-induced acute lung injury revealed by plasma H-1-nuclear magnetic resonance quantitative metabolomics and computational analysis. Am J Physiol Lung Cell Mol Physiol 2011, 300: 4–11. 10.1152/ajplung.00231.2010
Otvos JF, Jeyarajah EJ, Bennett DW: Quantification of plasma-lipoproteins by proton nuclear-magnetic-resonance spectroscopy. Clin Chem 1991, 37: 377–386.
Frenzel J, Gessner C, Sandvoss T, Hammerschmidt S, Schellenberger W, Sack U, Eschrich K, Wirtz H: Outcome prediction in pneumonia induced ALI/ARDS by clinical features and peptide patterns of BALF determined by mass spectrometry. PLoS One 2011, 6: e25544. 10.1371/journal.pone.0025544
Gong MN, Zhou W, Williams PL, Thompson BT, Pothier L, Boyce P, Christiani DC: 308GA and TNFB polymorphisms in acute respiratory distress syndrome. Eur Respir J 2005, 26: 382–389. 10.1183/09031936.05.00000505
Wurfel MM, Gordon AC, Holden TD, Radella F, Strout J, Kajikawa O, Ruzinski JT, Rona G, Black RA, Stratton S, Jarvik GP, Hajjar AM, Nickerson DA, Rieder M, Sevransky J, Maloney JP, Moss M, Martin G, Shanholtz C, Garcia JG, Gao L, Brower R, Barnes KC, Walley KR, Russell JA, Martin TR: Toll-like Receptor 1 Polymorphisms Affect Innate Immune Responses and Outcomes in Sepsis. Am J Respir Crit Care Med 2008, 178: 710–720. 10.1164/rccm.200803-462OC
Ye SQ, Simon BA, Maloney JP, Zambelli-Weiner A, Grant A, Easley RB, Mcverry BJ, Tuder RM, Standiford T, Brower RG, Barnes KC, Garcia JGN: Pre-B-cell colony-enhancing factor as a potential novel biomarker in acute lung injury. Am J Respir Crit Care Med 2005, 171: 361–370. 10.1164/rccm.200404-563OC
Marzec JM, Christie JD, Reddy SP, Jedlicka AE, Vuong H, Lanken PN, Aplenc R, Yamamoto T, Yamamoto M, Cho HY, Kleeberger SR: Functional polymorphisms in the transcription factor NRF2 in humans increase the risk of acute lung injury. FASEB J 2007, 21: 2237–2246. 10.1096/fj.06-7759com
Nuala JM, Li MY, Feng R, Bradfield Jn, Gallop R, Bellamy S, Fuchs BD, Lanken PN, Albelda SM, Rushefski M, Aplenc R, Abramova H, Atochina-Vasserman EN, Beers MF, Carolyn SC, Mitchell JC, Jean-Francois Pittet, David CC, O’Keefe Grant E, Lorraine BW, Addison KM, Mark MW, Hakon H, Jason DC: ANGPT2 Genetic Variant Is Associated with Trauma-associated Acute Lung Injury and Altered Plasma Angiopoietin-2 Isoform Ratio. Am J Respir Crit Care Med 2011, 183: 1344–1353. 10.1164/rccm.201005-0701OC
Glavan Bradford J, Holden Tarah D, Goss Christopher H, Anthony Black R, Neff Margaret J, Nathens Avery B, Martin Thomas R, Wurfel Mark M, ARDSnet Investigators: Genetic Variation in the FAS Gene and Associations with Acute Lung Injury. Am J Respir Crit Care Med 2011, 183: 356–363. 10.1164/rccm.201003-0351OC
Zhang WJ, Wei H, Tien YT, Frei B: Genetic ablation of phagocytic NADPH oxidase in mice limits TNF alpha-induced inflammation in the lungs but not other tissues. Free Radical Bio Med. 2011, 50: 1517–1525. 10.1016/j.freeradbiomed.2011.02.027
Dahmer MK, O'Cain P, Patwari PP, Simpson P, Li SH, Halligan N, Quasney MW: The influence of genetic variation in surfactant protein B on severe lung injury in African American children. Crit Care Med 2011, 39: 1138–1144. 10.1097/CCM.0b013e31820a9416
Leikauf GD, Concel VJ, Liu PY, Bein K, Berndt A, Ganguly K, Jang AS, Brant KA, Dietsch M, Pope-Varsalona H, Dopico RA, Di YPP, Li Q, Vuga LJ, Medvedovic M, Kaminski N, You M, Prows DR: Haplotype Association Mapping of Acute Lung Injury in Mice Implicates Activin A Receptor, Type 1. Am J Respir Crit Care Med 2011, 183: 1499–1509. 10.1164/rccm.201006-0912OC
Pino-Yanes M, Ma SF, Sun X, Tejera P, Corrales A, Blanco J, Pérez-Méndez L, Espinosa E, Muriel A, Blanch L, Garcia JG, Villar J, Flores C: Interleukin-1 Receptor-associated Kinase 3 Gene Associates with Susceptibility to Acute Lung Injury. Am J Respir Cell Mol Biol 2011, 45: 740–745. 10.1165/rcmb.2010-0292OC
Mirzapoiazova T, Moitra J, Moreno-Vinasco L, Sammani S, Turner JR, Chiang ET, Evenoski C, Wang T, Singleton PA, Huang Y, Lussier YA, Watterson DM, Dudek SM, Garcia JG: Non-muscle myosin light chain kinase isoform is a viable molecular target in acute inflammatory lung injury. Am J Respir Cell Mol Biol 2011, 44: 40–52. 10.1165/rcmb.2009-0197OC
Carnesecchi S, Deffert C, Pagano A, Garrido-Urbani S, Métrailler-Ruchonnet I, Schäppi M, Donati Y, Matthay MA, Krause KH, Barazzone Argiroffo C: NADPH oxidase-1 plays a crucial role in hyperoxia-induced acute lung injury in mice. Am J Respir Crit Care Med. 2009, 180(10):972–981. 10.1164/rccm.200902-0296OC
Parikh SM, Mammoto T, Schultz A, Yuan HT, Christiani D, Karumanchi SA, Sukhatme VP: Excess circulating angiopoietin-2 may contribute to pulmonary vascular leak in sepsis in humans. PLoS Med 2006, 3: e46. 10.1371/journal.pmed.0030046
Bhandari V, Choo-Wing R, Lee CG, Zhu Z, Nedrelow JH, Chupp GL, Zhang X, Matthay MA, Ware LB, Homer RJ, et al.: Hyperoxia causes angiopoietin 2-mediated acute lung injury and necrotic cell death. Nat Med 2006, 12: 1286–1293. 10.1038/nm1494
Matute-Bello G, Lee JS, Liles WC, Frevert CW, Mongovin S, Wong V, Ballman K, Sutlief S, Martin TR: Fas-mediated acute lung injury requires fas expression on nonmyeloid cells of the lung. J Immunol 2005, 175: 4069–4075.
Altemeier WA, Zhu X, Berrington WR, Harlan JM, Liles WC: Fas (CD95) induces macrophage proinflammatory chemokine production via a myd88-dependent, caspase-independent pathway. J Leukoc Biol 2007, 82: 721–728. 10.1189/jlb.1006652
Hawgood S: Surfactant protein B: structure and function. Biol Neonate. 2004, 85(4):285–289. 10.1159/000078169
Kurutz JW, Lee KY: NMR structure of lung surfactant peptide SP-B(11–25). Biochemistry. 2002, 41(30):9627–9636. 10.1021/bi016077x
Schmidt R, Meier U, Yabut-Perez M, Walmrath D, Grimminger F, Seeger W, Gunther A: Alteration of fatty acid profiles in different pulmonary surfactant phospholipids in acute respiratory distress syndrome and severe pneumonia. Am J Respir Crit Care Med. 2001, 163(1):95–100.
Bowler RP, Ellison MC, Reisdorph N: Proteomics in pulmonary medicine. Chest 2006, 130: 567–574. 10.1378/chest.130.2.567
Bowler RP, Duda B, Chan ED, Enghild JJ, Ware LB, Matthay MA, Duncan MW: Proteomic analysis of pulmonary edema fluid and plasma in patients with acute lung injury. Am J Physiol-Lung C 2004, 286: L1095-L1104. 10.1152/ajplung.00304.2003
Gygi SP, Corthals GL, Zhang Y, Rochon Y, Aebersold R: Evaluation of two-dimensional gel electrophoresis-based proteome analysis technology. Proc Natl Acad Sci USA 2000, 97: 9390–9395. 10.1073/pnas.160270797
Schnapp LM, Donohoe S, Chen JZ, Sunde DA, Kelly PM, Ruzinski J, Martin T, Goodlett DR: Mining the acute respiratory distress syndrome proteome: Identification of the insulin-like growth factor (IGF)/IGF-binding protein-3 pathway in acute lung injury. Am J Pathol 2006, 169: 86–95. 10.2353/ajpath.2006.050612
De Torre C, Ying SX, Munson PJ, Meduri GU, Suffredini AF: Proteomic analysis of inflammatory biomarkers in bronchoalveolar lavage. Proteomics 2006, 6: 3949–3957. 10.1002/pmic.200500693
Chang DW, Hayashi S, Gharib SA, Vaisar T, King ST, Tsuchiya M, Ruzinski JT, Park DR, Matute-Bello G, Wurfel MM, Bumgarner R, Heinecke JW, Martin TR: Proteomic and computational analysis of bronchoalveolar proteins during the course of the acute respiratory distress syndrome. Am Respir Crit Care Med 2008, 178: 701–709. 10.1164/rccm.200712-1895OC
Singleton PA, Mirzapoiazova T, Guo YR, Sammani S, Mambetsariev N, Lennon FE, Moreno-Vinasco L, Garcia JGN: High-molecular-weight hyaluronan is a novel inhibitor of pulmonary vascular leakiness. Am J Physiol-Lung C 2010, 299: 639–651. 10.1152/ajplung.00405.2009
Doroszko A, Hurst TS, Polewicz D, Sawicka J, Fert-Bober J, Johnson DH, Sawicki G: Effects of MMP-9 inhibition by doxycycline on proteome of lungs in high tidal volume mechanical ventilation-induced acute lung injury. Proteo Sci 2010, 8: 3. 10.1186/1477-5956-8-3
Vento G, Tirone C, Lulli P, Capoluongo E, Ameglio F, Lozzi S, Cota F, Mosca F, Romagnoli C, Messana I, Castagnola M, Inzitari R: Bronchoalveolar lavage fluid peptidomics suggests a possible matrix metalloproteinase-3 role in bronchopulmonary dysplasia. Intensiv Care Med 2009, 35: 2115–2124. 10.1007/s00134-009-1646-6
Medford ARL, Ibrahim NBN, Millar AB: Vascular endothelial growth factor receptor and coreceptor expression in human acute respiratory distress syndrome. J Crit Care 2009, 24: 236–242. 10.1016/j.jcrc.2008.04.003
Sapru A, Curley MAQ, Brady S, Matthay MA, Flori H: Elevated PAI-1 is associated with poor clinical outcomes in pediatric patients with acute lung injury. Intensiv Care Med 2010, 36: 157–163. 10.1007/s00134-009-1690-2
Fremont RD, Koyama T, Calfee CS, Wu W, Dossett LA, Bossert FR, Mitchell D, Wickersham N, Bernard GR, Matthay MA, May AK, Ware LB: Acute Lung Injury in Patients With Traumatic Injuries: Utility of a Panel of Biomarkers for Diagnosis and Pathogenesis. J Traum-Injury Infect Crit Care 2010, 68: 1121–1127. 10.1097/TA.0b013e3181c40728
Akram A, Han B, Masoom H, Peng C, Lam E, Litvack ML, Bai X, Shan Y, Hai T, Batt J, Slutsky AS, Zhang H, Kuebler WM, Haitsma JJ, Liu M, dos Santos CC: Activating transcription factor 3 confers protection against ventilator-induced lung injury. Am J Respir Crit Care Med 2010, 182: 489–500. 10.1164/rccm.200906-0925OC
Jin Y, Lee SJ, Minshall RD, Choi AM: Caveolin-1: a critical regulator of lung injury. Am J Physiol Lung Cell Mol Physiol. 2011, 300(2):L151-L160. 10.1152/ajplung.00170.2010
Davey A, McAuley DF, O'Kane CM: Matrix metalloproteinases in acute lung injury: mediators of injury and drivers of repair. Eur Respir J. 2011, 38(4):959–970. 10.1183/09031936.00032111
Hergrueter AH, Nguyen K, Owen CA: Matrix metalloproteinases: all the RAGE in the acute respiratory distress syndrome. Am J Physiol Lung Cell Mol Physiol. 2011, 300(4):L512-L515. 10.1152/ajplung.00023.2011
Mura M, Han B, Andrade CF, Seth R, Hwang D, Waddell TK, Keshavjee S, Liu M: The early responses of VEGF and its receptors during acute lung injury: implication of VEGF in alveolar epithelial cell survival. Crit Care. 2006, 10(5):R130. 10.1186/cc5042
Ware LB, Matthay MA, Parsons PE, Thompson BT, Januzzi JL, Eisner MD: National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Clinical Trials Network. Pathogenetic and prognostic significance of altered coagulation and fibrinolysis in acute lung injury/acute respiratory distress syndrome. Crit Care Med. 2007, 35(8):1821–1828. 10.1097/01.CCM.0000221922.08878.49
Chavakis T, Bierhaus A, Nawroth PP: RAGE (receptor for advanced glycation end products): a central player in the inflammatory response. Microbes Infect 2004, 6: 1219–1225. 10.1016/j.micinf.2004.08.004
Wu DJ, Rice CM, Wang XD: Cancer bioinformatics: A new approach to systems clinical medicine. BMC Bioinformatics 2012, 13: 71. 10.1186/1471-2105-13-71
Uchida T, Shirasawa M, Ware LB, Kojima K, Hata Y, Makita K, Mednick G, Matthay ZA, Matthay MA: Receptor for advanced glycation end-products is a marker of type I cell injury in acute lung injury. Am J Respir Crit Care Med. 2006, 173(9):1008–1015. 10.1164/rccm.200509-1477OC
Roessner U, Bowne J: What is metabolomics all about? Biotechniques 2009, 46: 363–365. 10.2144/000113133
Park Y, Jones DP, Ziegler TR, Lee K, Kotha K, Yu T, Martin GS: Metabolic effects of albumin therapy in acute lung injury measured by proton nuclear magnetic resonance spectroscopy of plasma: a pilot study. Crit Care Med 2011, 39: 2308–2813. 10.1097/CCM.0b013e31822571ce
Serkova NJ, Van Rheen Z, Tobias M, Pitzer JE, Wilkinson JE, Stringer KA: Utility of magnetic resonance imaging and nuclear magnetic resonance-based metabolomics for quantification of inflammatory lung injury. Am J Physiol-Lung C 2008, 295: 152–161. 10.1152/ajplung.00515.2007
Wang XD, Liotta L: Clinical bioinformatics: A new emerging science. J Clin Bioinforma 2011, 1: 1. 10.1186/2043-9113-1-1
Cooke CR, Shah CV, Gallop R, Bellamy S, Ancukiewicz M, Eisner MD, Lanken PN, Localio AR, Christie JD: A simple clinical predictive index for objective estimates of mortality in acute lung injury. Crit Care Med 2009, 37: 1913–1920. 10.1097/CCM.0b013e3181a009b4
Acknowledgements
The work was supported by Shanghai Leading Academic Discipline Project (Project Number:B115), Fudan University (Distinguished Professor Grant), and Shanghai Science & Technology Committee (08PJ1402900, 9540702600, 08DZ2293104).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
XF contribute to collection of information, analysis and interpretation of data and writing of the manuscript. CB: contribute to revision of the manuscript. XW: contribute to the critical revision of the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Fang, X., Bai, C. & Wang, X. Bioinformatics insights into acute lung injury/acute respiratory distress syndrome. Clin Trans Med 1, 9 (2012). https://doi.org/10.1186/2001-1326-1-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2001-1326-1-9