Abstract
Background
Lynch syndrome (LS) is associated with a high risk for colorectal cancer (CRC) and extracolonic malignancies, such as endometrial carcinoma (EC). The risk is dependent of the affected mismatch repair gene. The aim of the present study was to calculate the cumulative risk of LS related cancers in proven MLH1, MSH2 and MSH6 mutation carriers.
Methods
The studypopulation consisted out of 67 proven LS families. Clinical information including mutation status and tumour diagnosis was collected. Cumulative risks were calculated and compared using Kaplan Meier survival analysis.
Results
MSH6 mutation carriers, both males and females had the lowest risk for developing CRC at age 70 years, 54% and 30% respectively and the age of onset was delayed by 3-5 years in males. With respect to endometrial carcinoma, female MSH6 mutation carriers had the highest risk at age 70 years (61%) compared to MLH1 (25%) and MSH2 (49%). Also, the age of EC onset was delayed by 5-10 years in comparison with MLH1 and MSH2.
Conclusions
Although the cumulative lifetime risk of LS related cancer is similar, MLH1, MSH2 and MSH6 mutations seem to cause distinguishable cancer risk profiles. Female MSH6 mutation carriers have a lower CRC risk and a higher risk for developing endometrial carcinoma. As a consequence, surveillance colonoscopy starting at age 30 years instead of 20-25 years is more suitable. Also, prophylactic hysterectomy may be more indicated in female MSH6 mutation carriers compared to MLH1 and MSH2 mutation carriers.
Similar content being viewed by others
Background
Lynch syndrome (LS), also known as hereditary non-polyposis colorectal cancer, is the most common hereditary colorectal cancer (CRC) syndrome and accounts for 2-5% of all colorectal cancer cases [1]. Germline mutations in any of the four mismatch repair (MMR) genes, MLH1[2], MSH2[3], MSH6[4] and PMS2[5], are the underlying cause of LS. Subjects carrying a mutation in one of the MMR genes have a higher risk for developing colorectal cancer, but also for endometrial carcinoma and malignancies of the stomach, small bowel, ovaries, upper uroepithelial tract, biliary tract, skin and brain [6–9].
The colorectal cancer risk in LS is dependent on sex and the MMR gene involved. The reported lifetime risk for colorectal cancer in the literature varies from 28-100% in males and 25-83% in females [7, 10–18]. The risk of developing endometrial carcinoma ranges from 30-71% and the risk of other LS-associated cancers is less than 10-15% [9]. Furthermore, some studies have suggested that extracolonic cancers are more often observed in MSH2 mutation families compared to MLH1 mutation families [13, 19]. MSH6 mutation families probably have a milder clinical phenotype with a later onset of both CRC and EC and clustering of endometrial carcinoma [17]. The risks in PMS2 mutation families are largely unknown. One study reported that PMS2 mutation families have a milder phenotype compared to MLH1 and MSH2 families [20].
Unfortunately, the precise lifetime risk for CRC and endometrial carcinoma may be biased because the families selected in previous studies were mainly selected on basis of clustering of CRC or fulfilment of clinical criteria (Amsterdam II criteria). Furthermore, it was not always clear whether the affected subjects were proven mutation carriers. In addition, most studies have only evaluated lifetime risks for MLH1 and MSH2 mutations, while studies evaluating MSH6 mutation families are sparse. The most efficient way to calculate the lifetime risks of CRC and EC in Lynch syndrome would be to calculate these risks based on a cohort of proven mutation carriers. Therefore, the aim of the present study was to calculate the cumulative lifetime risks for CRC and EC in Lynch syndrome using a cohort of proven MLH1, MSH2 and MSH6 mutation carriers.
Methods
Study population
During the period 1994-2007, an MMR gene mutation was detected in 67 families who were counselled at the Department of Clinical Genetics of the Erasmus MC University Medical Center, because of a clinical suspicion for Lynch syndrome. Clinical data of family members including sex, age, mutation status, age at diagnosis of both LS-associated and other cancers were collected. LS-associated cancer included colorectal, endometrial, stomach, ovaries, upper uroepithelial tract, biliary tract, skin and brain cancer. Also, the site of the tumour, age at death and cause of death were collected. With consent of the patients or (in case the patient was deceased) of a close relative the cancer diagnosis was confirmed by pathology and/or medical reports. All pathology and medical reports were reviewed by the first author (DR) in order to confirm the diagnosis. If a subject reported the occurrence of cancer in the family and no pathology or medical report was available, the cancer was excluded from analysis. In addition, data regarding colonoscopic surveillance of affected and unaffected family members were collected.
Only subjects with a proven MMR gene mutation were included in this study.
Mutation analysis
Mutation analysis was performed by denaturing gradient gel electrophoresis, sequencing and multiplex ligation-dependent probe amplification (MRC-Holland kits P003 and P008). Mutation nomenclature was used according to international guidelines http://www.hgvs.org. A variant was considered a mutation when leading to a predicted truncated protein or based on previously published data. Silent or missense variants which were previously unreported or of unclear status were labelled unclassified variants (UV) and not considered as an MMR gene mutation.
Statistical analysis
Data were submitted for statistical testing using the Statistical Package for the Social Sciences (SPSS Inc, Chicago, IL), version 12.0.1. Data are given as median and range or as mean with standard deviation when appropriate. The chi square test, Student's t test and log rank test were used to compare differences between MLH1, MSH2 and MSH6 mutation carriers. Penetrance for age was calculated using the Kaplan Meier survival analysis method and included the 67 index cases. In case of multiple or recurrent colorectal carcinoma or endometrial adenocarcinoma, only the first diagnosis of either cancer was included in the analysis. The observation time for the different cancers was from birth until the date of first cancer diagnosis, death, date of hysterectomy (only for the observation time of endometrial carcinoma) or the end of the study (31 December 2007). A p value below .05 was considered statistically significant.
Results
Study population
In the 67 families with an MMR gene mutation, 26 (39%) were detected with an MLH1 mutation, 20 (30%) with an MSH2 mutation and 21 (31%) with an MSH6 mutation. Of the 67 families, 46 (69%) met the Amsterdam II criteria. Mutation analysis was performed in 725 subjects (296 men and 429 women) and a mutation was identified in 246 subjects (92 men, 154 women) (Table 1). At the time of mutation analysis the mean age of the 246 mutation carriers was 49 (± 16) years. Of the 246 mutation carriers, 115 (47%) were diagnosed with a Lynch syndrome associated tumour. One hundred and four (42%) mutation carriers already had been diagnosed with a Lynch syndrome associated tumour before mutation analysis was performed. Colorectal cancer was diagnosed in 83 (34%) mutation carriers, including 17 (7%) mutation carriers who developed 2 or more CRCs during their lifetime. Endometrial carcinoma was diagnosed in 37 (24%) of the 154 female mutation carriers, including 13 mutation carriers who also developed CRC during their life. Of the six families with a strong family history of endometrial carcinoma (two or more cases within the family), five (83%) were diagnosed with an MSH6 mutation. With respect to the other LS-associated cancers, 19 (8%) mutation carriers developed another LS-associated cancer during their life (Table 1). Seven of these nineteen mutation carriers were also diagnosed with CRC, one mutation carrier also with endometrial carcinoma and four mutation carriers with both CRC and EC. In total, 194 mutation carriers were under colonoscopic surveillance, including 69 subjects who had already been diagnosed with colorectal cancer before mutational testing was performed.
One of the 69 mutation carriers had previously been diagnosed with EC and developed CRC while being under colonoscopic surveillance. The other 68 mutation carriers were included in a colonoscopic surveillance program after being diagnosed with colorectal cancer. These 68 subjects were treated surgically (partial colectomy) for colorectal cancer and colonoscopic surveillance of the remaining colon was performed. Of the remaining 125 mutation carriers none developed colorectal cancer and in 23 (18%) adenomatous polyps had been detected and removed. The person-years of follow up was 1414 years and the mean follow up time of the subjects under colonoscopic surveillance was 7 ± 4 years.
Lifetime risks
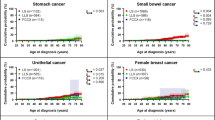
The respective lifetime risks curves are shown in figure 1, figure 2, figure 3 and figure 4. For all LS-associated tumours, the cumulative risks in both male and female mutation carriers at 70 years was 71% for MLH1, 77% for MSH2 and 75% for MSH6 mutation carriers (Figure 1). Although the cumulative risks at age 70 years were similar for the three different MMR genes, the log rank test showed a significant difference for developing any Lynch syndrome associated cancer between MSH6, MLH1 and MSH2 mutation carriers (p = 0.01). This was due to the fact that before the age of 70 years the risk of developing any Lynch syndrome associated cancer in MSH6 carriers was lower compared to MLH1 or MSH2 mutation carriers (Figure 1).
In Figure 2, the age related cumulative risk for CRC is shown for male MLH1, MSH2 and MSH6 mutation carriers. At age 70 years, the cumulative risk was the highest for MLH1 mutation carriers, 78%, while the cumulative risks for MSH2 and MSH6 mutation carriers were 57% and 54% respectively. There was no significant difference in age related cumulative risk between MSH6 mutation carriers (p = 0.05) compared to MLH1 and MSH2 mutation carriers. However, the highest increase in risk in male MLH1 and MSH2 mutation carriers was observed between the ages of 40 to 50 years, while the risk in male MSH6 mutation carriers mostly increased between the ages of 50 to 60 years. Although the age related risks were not significant different between the three different MMR genes, there was a trend in male MLH1 and MSH2 mutation carriers to develop CRC at an earlier age than male MSH6 mutation carriers. The cumulative risks for CRC in females were lower compared to males, 57% for MLH1, 52% for MSH2 and 30% for MSH6 mutation carriers (Figure 3), with a significantly lower age related cumulative risk in MSH6 mutation carriers (p = 0.001) compared to MLH1 and MSH2 mutation carriers.
For endometrial carcinoma, the highest cumulative risk was observed in the MSH6 mutation carriers (61%), while the cumulative risks for MLH1 and MSH2 mutation carriers were 25% and 49% respectively. However, the log rank test showed no significant difference in age related cumulative risk (p = 0.58) between MSH6 mutation carriers compared to MLH1 and MSH2 mutation carriers.
Median age of onset
The median age of CRC onset in males was significantly higher in MSH6 mutation carriers (48 years; range 32-84 years) compared to MSH2 mutation carriers (43 years; range 20-51 years, p = 0.03), but not significantly higher compared to MLH1 mutation carriers (45 years; range 33-63 years, p = 0.07) (Table 2). For female mutation carriers, no significant differences in the median age of CRC onset were found when comparing MSH6 (53 years; range 34-61 years) with MLH1 (50 years; range 25-79 years, p = 0.88) and MSH2 (44 years; range 29-82 years, p = 0.28). The median age of EC onset was significant higher in MSH6 mutation carriers (56 years; 47-67 years) compared to MLH1 mutation carriers (51 years; 46-54 years, p = 0.02) and MSH2 mutation carriers (46 years; 36-55 years, p = 0.001). There were no significant differences in the age of onset of other LS-associated cancers between MLH1 (53 years; range 52-54 years), MSH2 (42 years; range 23-59 years) and MSH6 (50 years; range: 35-76) mutation carriers (MLH1 vs. MSH2, p = 0.41; MLH1 vs. MSH6, p = 0.76 and MSH2 vs. MSH6, p = 0.41).
Discussion
In this study, we evaluated 246 individuals from 67 families with a proven mismatch repair gene mutation to determine the cumulative lifetime risk of developing cancer. Previous studies have shown different lifetime risks for developing CRC in Lynch patients.
One of the first studies evaluating the lifetime risk reported a lifetime risk for CRC at age 75 years of 92% in males and 83% in females [10]. Most later studies reported somewhat similar risks for CRC ranging from 65-100% in males and 30-63% risk in females [7, 11–13]. A more recently published study reported the lowest lifetime risk for CRC so far, 27% for males and 22% for females at age 70 years [15]. All these studies only evaluated the risks associated with MLH1 and MSH2 mutations. Thirty one percent of the families included in our study carried an MSH6 mutation. This frequency is higher than previously reported [4, 21–23]. Studies evaluating the lifetime risks of cancer amongst MLH1, MSH2 and MSH6 families are sparse. A study evaluating the risk in 20 MSH6 families showed that colorectal cancer was less frequent and developed 10 years later in MSH6 compared to MLH1 and MSH2. In addition a significant higher lifetime risk of endometrial carcinoma of 71% in MSH6 mutation carriers with a later age of onset (54 years vs. 48 and 49 years for MLH1 and MSH2) was reported [17]. A German study comparing 27 MSH6 mutation families with 156 MLH1 and MSH2 mutation families confirmed the lower risk and later age of onset of CRC in MSH6 families [24]. These results were also confirmed by a recently published British study, but this study only included 11 proven MSH6 mutation carriers [18].
Our study indicates that, however the cumulative risks of cancer at age 70 years in MLH1, MSH2 and MSH6 mutation carriers is similar, each mutated gene has a distinguishable cancer risk profile. In MSH6 mutation carriers the risk at age 70 years for developing CRC was the lowest in both male (54%) and female (30%) when compared to carriers of MLH1 and MSH2 mutations.
Between male MSH6 and MSH2 mutation carriers also a significant difference in the age of CRC onset (48 vs. 43 years, p = 0.03) was found and there was a trend in higher age of CRC onset between male MSH6 and MLH1 mutation carriers. For female mutation carriers, no significant differences were found in the mean age of onset of CRC. This can be explained by the fact that female MLH1 and MSH2 mutation carriers still developed CRC at an older age. The lower risk of CRC onset in female MSH6 mutation carriers under the age of 50 years raises the question whether colonoscopic surveillance guidelines in these subjects can be changed. Current guidelines advise to start with biennial colonoscopy surveillance from the age of 20-25 years [25]. In our study population, the youngest affected female MSH6 mutation carrier with CRC was 34 years. Our data and the data from previous studies support that colonoscopic surveillance can be started at an age of 30 years in female MSH6 mutation carriers [17].
However our numbers are too small to draw definite conclusions, CRC seems to be the predominant cancer in MLH1 mutation carriers. In MSH2 and MSH6 mutation carriers extracolonic cancers appear to contribute more to the similar cumulative lifetime risk of cancer in MLH1, MSH2 and MSH6 mutation carriers. A higher risk of extracolonic-LS-associated cancer was previously reported in MSH2 mutation carriers compared to MLH1 mutation carriers [13, 19]. Unfortunately, the number of extracolonic-LS associated cancer (excluding endometrial carcinoma) in our study population was too low to calculate accurate risk estimates for these cancers. In concordance with other studies [17, 26] our study indicates that MSH6 carriers have the highest endometrial cancer risk followed by MSH2 and MLH1 mutation carriers. Also, this risk increases sharply after the age of 50 years. In view of the disputable effect of endometrial carcinoma surveillance [27, 28], in female MSH6 carriers aged 45 years or above prophylactic hysterectomy may be suggested in order to decrease the risk for developing endometrial carcinoma [29]. In MSH2 and MLH1 female mutation carriers this option may be more questionable. In MSH2 mutation carriers the risk of other extracolonic and extraendometrial cancers may reduce faith in and benefit of risk reducing surgery. In MLH1 mutation carriers the risk of endometrial cancer may not outweigh the disadvantages of surgery. In case of surgery for another cause, additional hysterectomy should be considered also in MLH1 en MSH2 mutation carriers.
A strength of the present study was that the age related risks where calculated using proven mutation carriers. However, the age related risks might be somewhat lower since not all the unaffected individuals from proven mutation families opted for genetic testing and thus the total number of unaffected mutation carriers in the mutation families may be underestimated. In addition, individuals with a higher risk for mutation carriership, i.e. with an affected first degree relative, more often opt for genetic testing [30]. This may also have introduced some bias with respect to the age related risks. Also, we included the index cases in our study population. Index cases give rise to the suspicion of Lynch syndrome and they always have cancer. This may also have resulted in a slightly higher age related risk. On the other hand, the majority (77%) of not affected mutation carriers was under colonoscopy surveillance, which likely has influenced the age related risks for developing invasive CRC, since colonoscopy surveillance in Lynch syndrome patients is effective in reducing the incidence and mortality of CRC [31]. A limitation of our study was that our study population was not very large (n = 246), and the number of male carriers was 92. This could explain why we did not find a significant difference in both the mean age of CRC onset and the age related risk between male MLH1, MSH2 and MSH6 mutation carriers.
In conclusion, the present study indicates that, although the cumulative risks at age 70 years of LS related cancer in MLH1, MSH2 and MSH6 mutation carriers are similar, each mutated gene has a distinguishable cancer risk profile. It underlines that female MSH6 mutation carriers have a distinct clinical phenotype with a lower CRC risk and a higher risk for developing endometrial carcinoma. Starting with biennial colonoscopic surveillance at an age of 30 years instead of an age of 20-25 years in female MSH6 mutation carriers is more suitable. Moreover, in female MSH6 mutation carriers prophylactic hysterectomy may be considered from an age of 45 years.
Conclusions
The present study indicates that each mutated MMR gene has a distinguishable cancer risk profile. Female MSH6 mutation carriers have a lower CRC risk and a higher risk for developing endometrial carcinoma. Starting with biennial colonoscopic surveillance at an age of 30 years in female MSH6 mutation carriers is more suitable and prophylactic hysterectomy may be considered from an age of 45 years.
Abbreviations
- CRC:
-
colorectal cancer
- EC:
-
endometrial cancer
- LS:
-
Lynch syndrome
- MMR:
-
mismatch repair
- UV:
-
unclassified variant.
References
Aaltonen LA, Salovaara R, Kristo P, Canzian F, Hemminki A, Peltomaki P, Chadwick RB, Kaariainen H, Eskelinen M, Jarvinen H, Mecklin JP, de la CA: Incidence of hereditary nonpolyposis colorectal cancer and the feasibility of molecular screening for the disease. N Engl J Med 1998, 338: 1481–7. 10.1056/NEJM199805213382101
Bronner CE, Baker SM, Morrison PT, Warren G, Smith LG, Lescoe MK, Kane M, Earabino C, Lipford J, Lindblom A: Mutation in the DNA mismatch repair gene homologue hMLH1 is associated with hereditary non-polyposis colon cancer. Nature 1994, 368: 258–61. 10.1038/368258a0
Fishel R, Lescoe MK, Rao MR, Copeland NG, Jenkins NA, Garber J, Kane M, Kolodner R: The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer. Cell 1993, 75: 1027–38. 10.1016/0092-8674(93)90546-3
Miyaki M, Konishi M, Tanaka K, Kikuchi-Yanoshita R, Muraoka M, Yasuno M, Igari T, Koike M, Chiba M, Mori T: Germline mutation of MSH6 as the cause of hereditary nonpolyposis colorectal cancer. Nat Genet 1997, 17: 271–2. 10.1038/ng1197-271
Nicolaides NC, Papadopoulos N, Liu B, Wei YF, Carter KC, Ruben SM, Rosen CA, Haseltine WA, Fleischmann RD, Fraser CM: Mutations of two PMS homologues in hereditary nonpolyposis colon cancer. Nature 1994, 371: 75–80. 10.1038/371075a0
Rodriguez-Bigas MA, Vasen HF, Lynch HT, Watson P, Myrhoj T, Jarvinen HJ, Mecklin JP, Macrae F, St John DJ, Bertario L, Fidalgo P, Madlensky L, Rozen P: Characteristics of small bowel carcinoma in hereditary nonpolyposis colorectal carcinoma. International Collaborative Group on HNPCC. Cancer 1998, 83: 240–4. 10.1002/(SICI)1097-0142(19980715)83:2<240::AID-CNCR6>3.0.CO;2-U
Aarnio M, Sankila R, Pukkala E, Salovaara R, Aaltonen LA, de la Chapelle A, Peltomaki P, Mecklin JP, Jarvinen HJ: Cancer risk in mutation carriers of DNA-mismatch-repair genes. Int J Cancer 1999, 81: 214–8. 10.1002/(SICI)1097-0215(19990412)81:2<214::AID-IJC8>3.0.CO;2-L
Park YJ, Shin KH, Park JG: Risk of gastric cancer in hereditary nonpolyposis colorectal cancer in Korea. Clin Cancer Res 2000, 6: 2994–8.
Watson P, Vasen HF, Mecklin JP, Bernstein I, Aarnio M, Jarvinen HJ, Myrhoj T, Sunde L, Wijnen JT, Lynch HT: The risk of extra-colonic, extra-endometrial cancer in the Lynch syndrome. Int J Cancer 2008, 123: 444–9. 10.1002/ijc.23508
Vasen HF, Wijnen JT, Menko FH, Kleibeuker JH, Taal BG, Griffioen G, Nagengast FM, Meijers-Heijboer EH, Bertario L, Varesco L, Bisgaard ML, Mohr J, Fodde R, Khan PM: Cancer risk in families with hereditary nonpolyposis colorectal cancer diagnosed by mutation analysis. Gastroenterology 1996, 110: 1020–7. 10.1053/gast.1996.v110.pm8612988
Dunlop MG, Farrington SM, Carothers AD, Wyllie AH, Sharp L, Burn J, Liu B, Kinzler KW, Vogelstein B: Cancer risk associated with germline DNA mismatch repair gene mutations. Hum Mol Genet 1997, 6: 105–10. 10.1093/hmg/6.1.105
Lin KM, Shashidharan M, Thorson AG, Ternent CA, Blatchford GJ, Christensen MA, Watson P, Lemon SJ, Franklin B, Karr B, Lynch J, Lynch HT: Cumulative incidence of colorectal and extracolonic cancers in MLH1 and MSH2 mutation carriers of hereditary nonpolyposis colorectal cancer. J Gastrointest Surg 1998, 2: 67–71. 10.1016/S1091-255X(98)80105-4
Vasen HF, Stormorken A, Menko FH, Nagengast FM, Kleibeuker JH, Griffioen G, Taal BG, Moller P, Wijnen JT: MSH2 mutation carriers are at higher risk of cancer than MLH1 mutation carriers: a study of hereditary nonpolyposis colorectal cancer families. J Clin Oncol 2001, 19: 4074–80.
Wagner A, Hendriks Y, Meijers-Heijboer EJ, de Leeuw WJ, Morreau H, Hofstra R, Tops C, Bik E, Brocker-Vriends AH, van der Meer C, Lindhout D, Vasen HF, Breuning MH, Cornelisse CJ, van Krimpen C, Niermeijer MF, Zwinderman AH, Wijnen J, Fodde R: Atypical HNPCC owing to MSH6 germline mutations: analysis of a large Dutch pedigree. J Med Genet 2001, 38: 318–22. 10.1136/jmg.38.5.318
Quehenberger F, Vasen HF, van Houwelingen HC: Risk of colorectal and endometrial cancer for carriers of mutations of the hMLH1 and hMSH2 gene: correction for ascertainment. J Med Genet 2005, 42: 491–6. 10.1136/jmg.2004.024299
Hampel H, Stephens JA, Pukkala E, Sankila R, Aaltonen LA, Mecklin JP, de la Chapelle A: Cancer risk in hereditary nonpolyposis colorectal cancer syndrome: later age of onset. Gastroenterology 2005, 129: 415–21.
Hendriks YM, Wagner A, Morreau H, Menko F, Stormorken A, Quehenberger F, Sandkuijl L, Moller P, Genuardi M, Van Houwelingen H, Tops C, Van Puijenbroek M, Verkuijlen P, Kenter G, Van Mil A, Meijers-Heijboer H, Tan GB, Breuning MH, Fodde R, Wijnen JT, Brocker-Vriends AH, Vasen H: Cancer risk in hereditary nonpolyposis colorectal cancer due to MSH6 mutations: impact on counseling and surveillance. Gastroenterology 2004, 127: 17–25. 10.1053/j.gastro.2004.03.068
Barrow E, Alduaij W, Robinson L, Shenton A, Clancy T, Lalloo F, Hill J, Evans DG: Colorectal cancer in HNPCC: cumulative lifetime incidence, survival and tumour distribution. A report of 121 families with proven mutations. Clin Genet 2008, 74: 233–42. 10.1111/j.1399-0004.2008.01035.x
Lin KM, Shashidharan M, Ternent CA, Thorson AG, Blatchford GJ, Christensen MA, Lanspa SJ, Lemon SJ, Watson P, Lynch HT: Colorectal and extracolonic cancer variations in MLH1/MSH2 hereditary nonpolyposis colorectal cancer kindreds and the general population. Dis Colon Rectum 1998, 41: 428–33. 10.1007/BF02235755
Hendriks YM, Jagmohan-Changur S, van der Klift HM, Morreau H, Van Puijenbroek M, Tops C, van Os T, Wagner A, Ausems MG, Gomez E, Breuning MH, Brocker-Vriends AH, Vasen HF, Wijnen JT: Heterozygous mutations in PMS2 cause hereditary nonpolyposis colorectal carcinoma (Lynch syndrome). Gastroenterology 2006, 130: 312–22. 10.1053/j.gastro.2005.10.052
Peltomaki P, Vasen H: Mutations associated with HNPCC predisposition -- Update of ICG-HNPCC/INSiGHT mutation database. Dis Markers 2004, 20: 269–76.
Peterlongo P, Nafa K, Lerman GS, Glogowski E, Shia J, Ye TZ, Markowitz AJ, Guillem JG, Kolachana P, Boyd JA, Offit K, Ellis NA: MSH6 germline mutations are rare in colorectal cancer families. Int J Cancer 2003, 107: 571–9. 10.1002/ijc.11415
Kolodner RD, Tytell JD, Schmeits JL, Kane MF, Gupta RD, Weger J, Wahlberg S, Fox EA, Peel D, Ziogas A, Garber JE, Syngal S, nton-Culver H, Li FP: Germ-line msh6 mutations in colorectal cancer families. Cancer Res 1999, 59: 5068–74.
Plaschke J, Engel C, Kruger S, Holinski-Feder E, Pagenstecher C, Mangold E, Moeslein G, Schulmann K, Gebert J, von Knebel DM, Ruschoff J, Loeffler M, Schackert HK: Lower incidence of colorectal cancer and later age of disease onset in 27 families with pathogenic MSH6 germline mutations compared with families with MLH1 or MSH2 mutations: the German Hereditary Nonpolyposis Colorectal Cancer Consortium. J Clin Oncol 2004, 22: 4486–94. 10.1200/JCO.2004.02.033
Vasen HF, Moslein G, Alonso A, Bernstein I, Bertario L, Blanco I, Burn J, Capella G, Engel C, Frayling I, Friedl W, Hes FJ, Hodgson S, Mecklin JP, Moller P, Nagengast F, Parc Y, Renkonen-Sinisalo L, Sampson JR, Stormorken A, Wijnen J: Guidelines for the clinical management of Lynch syndrome (hereditary non-polyposis cancer). J Med Genet 2007, 44: 353–62. 10.1136/jmg.2007.048991
Barrow E, Robinson L, Alduaij W, Shenton A, Clancy T, Lalloo F, Hill J, Evans DG: Cumulative lifetime incidence of extracolonic cancers in Lynch syndrome: a report of 121 families with proven mutations. Clin Genet 2009, 75: 141–9. 10.1111/j.1399-0004.2008.01125.x
Dove-Edwin I, Boks D, Goff S, Kenter GG, Carpenter R, Vasen HF, Thomas HJ: The outcome of endometrial carcinoma surveillance by ultrasound scan in women at risk of hereditary nonpolyposis colorectal carcinoma and familial colorectal carcinoma. Cancer 2002, 94: 1708–12. 10.1002/cncr.10380
Renkonen-Sinisalo L, Butzow R, Leminen A, Lehtovirta P, Mecklin JP, Jarvinen HJ: Surveillance for endometrial cancer in hereditary nonpolyposis colorectal cancer syndrome. Int J Cancer 2007, 120: 821–4. 10.1002/ijc.22446
Schmeler KM, Lynch HT, Chen LM, Munsell MF, Soliman PT, Clark MB, Daniels MS, White KG, Boyd-Rogers SG, Conrad PG, Yang KY, Rubin MM, Sun CC, Slomovitz BM, Gershenson DM, Lu KH: Prophylactic surgery to reduce the risk of gynecologic cancers in the Lynch syndrome. N Engl J Med 2006, 354: 261–9. 10.1056/NEJMoa052627
Ramsoekh D, van Leerdam ME, Tops CM, Dooijes D, Steyerberg EW, Kuipers EJ, Wagner A: The use of genetic testing in hereditary colorectal cancer syndromes: genetic testing in HNPCC, (A)FAP and MAP. Clin Genet 2007, 72: 562–7. 10.1111/j.1399-0004.2007.00912.x
de Jong AE, Hendriks YM, Kleibeuker JH, de Boer SY, Cats A, Griffioen G, Nagengast FM, Nelis FG, Rookus MA, Vasen HF: Decrease in mortality in Lynch syndrome families because of surveillance. Gastroenterology 2006, 130: 665–71. 10.1053/j.gastro.2005.11.032
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
DR participated in the data collection, performed the statistical analyses and helped to draft the manuscript. AW conceived of the study and participated in the data collection. ML helped to draft the manuscript. DD participated in the data collection. CT participated in the data collection. ES participated in the design of the study and assisted in the statistical analysis. EK helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ramsoekh, D., Wagner, A., van Leerdam, M.E. et al. Cancer risk in MLH1, MSH2 and MSH6 mutation carriers; different risk profiles may influence clinical management. Hered Cancer Clin Pract 7, 17 (2009). https://doi.org/10.1186/1897-4287-7-17
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1897-4287-7-17