Abstract
The Swedish Family-Cancer Database has been used for some 10 years in the study of familial risks at all common sites. In the present paper we describe some of the main features of version VII of this Database, assembled in year 2006. This update included all residents in Sweden born or immigrated in 1932 and later (offspring) with their biological parents, a total of 11.5 million individuals. Cancer cases were retrieved from the Swedish Cancer Registry from years 1958 to 2004, including over 1.2 million first and multiple primary cancers and in situ tumours. We show one application of the Database in the study of familial risks in prostate cancer, with special reference to the modification of familial risk at the time of about 50% increase in incidence due to prostate specific antigen (PSA) screening. The familial risks for prostate cancer were 1.92 for sons of affected fathers, 3.03 for brothers and 5.44 for men with an affected father and an affected brother. Familial risk for prostate cancer according to the time since the first family member was diagnosed showed significant increases for two family members being diagnosed in the same year compared to 5+ years apart. Increased surveillance and the availability of PSA screening are the likely reasons for the overestimated familial relative risk shortly after the first diagnosis. This lead time bias should be considered in clinical counselling.
Similar content being viewed by others
Introduction
The family history is the prime anamnestic piece of information in the clinical genetic counselling of many diseases, including breast, prostate and colorectal cancers [1, 2]. A confirmed family history of a disease has been the initial clue about its heritable causation and a starting point for gene identification of most hereditary diseases. Public awareness of familial risks and the demand for counselling have increased. In the USA, increasing numbers of National Cancer Institute-designated cancer centres offer clinical genetic counselling, not only to patients and their families but to any concerned individuals [3]. Awareness of familial risks and concern after diagnosis of a family member may lead to an early diagnosis of the same disease, if screening methods are available, as shown for melanoma and in situ breast and cervical cancers [4]. The usefulness of the family history is critically dependent on its accuracy. A recommendation for mutation testing for a disease gene is usually based on the family history, and the result may turn out to be negative simply because the family history has been wrong. Unfortunately patients tend often to be unaware of the medical histories of their relatives. Recently, data on the accuracy of family histories have been accumulated by comparing reported histories to those with medical documentation. Murff et al. collected literature on the accuracy of family history data for cancer [5]. The positive predictive value (positives of true positives) of the reported family history compared to medical diagnosis in a first-degree relative was 93% for breast, 85% for prostate, 81% for colon, 69% for ovarian and 37% for endometrial cancers when reported by cancer patients. When the family histories were reported by healthy controls, the positive predictive values were about 20 percent units lower; the worst were ovarian (25%) and endometrial cancers (17%). The percentages were lower for the second-degree relatives than for the first-degree relatives. Many of the findings were similar in a Swedish study, which suggested that reporting is worse for rare cancers; somewhat surprisingly, the accuracy of reporting cancer in siblings was worse than that in parents [6]. These data are worrisome as they are, but they may be even worse for many other diseases, for which the diagnostics have not been as uniform as they have been for cancer during the past half century.
Familial clustering of cancer can be identified through a number of approaches. The clinical identification of probands and construction of pedigrees has been the classical approach to heritable diseases. A unique population screening program for familial cancer has been carried out among the 1.5 million inhabitants of the West Pomeranian Region around Szczecin in Poland [7, 8]. As a further alternative, population-based datasets on familial cancer have been used in Utah, Iceland, UK, Denmark, Finland and Sweden [9–13]. The largest dataset on familial cancer is the Swedish Family-Cancer Database, which has been updated periodically, and in the present article we report the seventh update, covering cancers up to year 2004, abbreviated FCD2004. We show an application of the Database to prostate cancer, with special reference to the familial risks during a period of increasing incidence.
The Family-Cancer Database of year 2004
Statistics Sweden created a family database, the "Second Generation Register", in 1995 [14]. After a few expansions, it covered offspring born after 1931 with their parents, renamed as the "Multigeneration Register" to indicate that the number of generations was more than two. We have linked this Register to the Swedish Cancer Registry (1958-2004) to make the Family-Cancer Database (MigMed2) in year 2006 for the seventh time, called here FCD2004 [15, 16]. For the first time, FCD2004 contains data on all immigrants, whereas the previous versions only included those who had children in Sweden. In FCD all data are organized in child-mother-father triplets; the parents have been registered at the time of birth of the child, allowing tracking of "biological" parents in spite of divorce and remarriage.
FCD2004 identified a total of 11.5 million persons, divided into parental and offspring generations. An overwhelming proportion (97.9%) of offspring born in Sweden have information on parents, but the proportion is much smaller for offspring born outside Sweden, for obvious reasons (Table 1). Even for those born in Sweden, the parental links are more numerous for living than for deceased individuals; 10.9% of offspring with cancer lack parental links. FCD2004 contains 1.2 million tumour notifications, compared to 1.1 million in FCD2002 (Table 2); among tumours in FCD2004, 796,000 are first primary cancers, 85,000 are multiple primaries and 237,000 are in situ cancers, dominated by cervical in situ cancers. The annual accumulation of cancer cases to the parental and offspring generation in FCD2004 and FCD2002 is shown in Fig. 1. The offspring generation had initially far fewer cases than the parental one but now in FCD2004 the number of cases among the offspring & parent group (i.e. those who were first offspring and then became parents) exceeded the case numbers of the parental generation. The parental cases are decreasing in the course of time because the parental generation was born before year 1932 and it is dying away. The 'All' curve is the sum of the three other mutually exclusive curves.

Figure 1
An application of the Database: prostate cancer
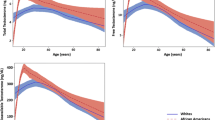
According to the Cancer Incidence in Five Continents, the difference in incidence of prostate cancer between the highest (202/100,000 for Detroit African Americans) and the lowest (1.1 for Qidong, China) rates is larger than for any major cancer [17]. The reasons for the difference are not understood but one is the ever rising incidence in the affluent countries. The increase in incidence, 3.4-fold in Sweden, is shown in Fig. 2 for the period 1960-2004, based on the Swedish Cancer Registry. There seem to be two different patterns in the age-incidence relationships. The first one prevailed until about year 1995, and it was characterized by a preferential increase in incidence in those older than 70 years [18]. This increase coincided with a more common and intense application of prostatic biopsies and transurethral resection techniques [19]. In the second phase, after year 1997, the 50% increase extended preferentially to younger age groups and it coincided with a wide application of opportunistic prostate specific antigen (PSA) testing [20, 21]. The widespread use of PSA testing was the probable cause of the upward shift in incidence between years 1998 and 2004.
The familial risks for prostate cancer are shown in Table 3 based on FCD2004 (oldest age for offspring 72 years) and FCD2002 (oldest age for offspring 70 years). The methods, based on standardized incidence ratio (SIR) and 95% confidence intervals (CIs), have been described elsewhere [15, 16]. The number of affected father-son pairs has increased from 1501 to 2546 and that of affected brother pairs from 361 to 898; for three affected individuals/family the number has increased from 118 to 259. The increases in familial cases show the reason why the biannual updating of FCD are considered worthwhile. All the familial risks have decreased slightly because of the aging population; in FCD2004 they were 1.92 for sons of affected fathers, 3.03 for brothers and 5.44 for men with an affected father and an affected brother (Table 3).
With increasing incidence and access, changes in familial risks are expected; some evidence has been seen for prostate and some other cancers earlier [4, 18, 22]. The methods, based on Poisson regression analysis, have been described elsewhere [4]; relative risk (RR), its 95%CIs and a two-sided p-value were calculated. We assessed familial risk for prostate cancer in father-son pairs using FCD2004 and FCD2002 according to the time since the first family member was diagnosed (Fig. 3). The risk was highest for sons to be diagnosed with prostate cancer in the year of the father's diagnosis, and higher in FCD2004 (RR 3.37, N = 31, 95%CI 2.34-4.86) than in FCD2002 (2.72). In FCD2004 the difference between the same year and the reference, 5+ years (RR 2.10, N = 2504, 95%CIs 2.01-2.19), was significant, p = 0.011. The similar analysis for brothers showed a somewhat different result, as the RRs were systematically lower for FCD2004 than FCD2002 (Fig. 4); however, the difference between the same and 5+ years remained. In FCD2004 the RR for diagnosis of both brothers in the same year was 5.06 (N = 101, 95%CIs 3.86-6.64) compared to 3.30 (N = 134, 95%CIs 2.60-4.18) in 5+ years, p = 0.019.
Conclusions
The median age at diagnosis of cancer at all sites is about 70 years in Sweden [23]. Thus the offspring population aged up to 72 years in FCD2004 has passed the median age. If familial cancers indeed are diagnosed at a younger age than sporadic cancers, as they are for known hereditary cancer syndromes, then we can expect to have captured a large proportion of familial cancers, particularly for relatively early onsets cancers, such as breast cancer. However, for relatively late onset cancers, exemplified by prostate cancer here, larger numbers of familial cases are obtained by extending the data to older individuals. Data from the Utah population database suggest that familial cancers can be detected even at old ages [10]. Even hereditary cancers can be found at late age; when mutation screening for hereditary nonpolyposis colorectal cancer (HNPCC) was extended to older patients, mutation-positive individuals were detected with a median age of 61 years, compared to the long-held median age of 44 years [24]. Whether familial cancers tend to be of early onset is yet to be seen and the future updates of FCD will resolve the issue.
The successes in early diagnosis and management of heritable cancers have shown that inherited cancers are no longer inevitable. Although genetic testing has become an important method for at-risk families of certain cancers, it covers a small proportion of all familial cancers. Empirical risk estimates from epidemiological studies have proven to be useful for familial breast and prostate cancers, and it is recommended that reliable risk estimates for other cancers also be seriously considered for routine clinical recommendations [25]. A familial low-penetrant risk in a common cancer may result in more cases in a given population than a high risk of a rare cancer. Furthermore, familial risks are higher for some relatively rare neoplasms, causing hardship in the affected families. Epidemiological results on familial risk are sometimes dismissed because 'they cannot be translated into individual risks'. However, there are many examples on everyday use of epidemiological data in clinical risk estimation [16, 25]. In the absence of known genes, reliable individual risk estimates need to be generated among populations.
Increased surveillance and the availability of screening methods may result in overestimated familial relative risks shortly after the first diagnosis. We show here increased risks for prostate cancer both for father-son pairs and for brothers in the year of the first family member's diagnosis. The findings are consistent with data from FCD2002 [4, 18, 22]. However, even though the overall effect of this bias on familial risks is small, it calls for consideration in clinical counselling of individuals from families in which synchronous cancers were diagnosed. The lead time bias should not misguide the doctor, who should instead explain the possibility of bias to the patients and their family members in order to comfort their anxiety.
References
American Society of Clinical Oncology: American Society of Clinical Oncology policy statement update: genetic testing for cancer susceptibility. J Clin Oncol 2003, 21: 2397–2406. 10.1200/JCO.2003.03.189
Hampel H, Sweet K, Westman JA, Offit K, Eng C: Referral for cancer genetics consultation: a review and compilation of risk assessment criteria. J Med Genet 2004, 41: 81–91. 10.1136/jmg.2003.010918
Epplein M, Koon KP, Ramsey SD, Potter JD: Genetic services for familial cancer patients: a follow-up survey of National Cancer Institute Cancer Centers. J Clin Oncol 2005, 23: 4713–4718. 10.1200/JCO.2005.00.133
Bermejo JL, Hemminki K: Familial risk of cancer shortly after diagnosis of the first familial tumor. J Natl Cancer Inst 2005, 97: 1575–1579.
Murff HJ, Spigel DR, Syngal S: Does this patient have a family history of cancer? An evidence-based analysis of the accuracy of family cancer history. Jama 2004, 292: 1480–1489. 10.1001/jama.292.12.1480
Chang E, Smedby KE, Hjalgrim H, Glimelius B, Adami HO: Reliability of self-reported family history of cancer in a large case-control study of lymphoma. J Natl Cancer Inst 2006, 98: 61–68.
Cybulski C, Gorski B, Huzarski T, Masojc B, Mierzejewski M, Debniak T, Teodorczyk U, Byrski T, Gronwald J, Matyjasik J, Zlowocka E, Lenner M, Grabowska E, Nej K, Castaneda J, Medrek K, Szymanska A, Szymanska J, Kurzawski G, Suchy J, Oszurek O, Witek A, Narod SA, Lubinski J: CHEK2 is a multiorgan cancer susceptibility gene. Am J Hum Genet 2004, 75: 1131–1135. 10.1086/426403
Gorski B, Cybulski C, Huzarski T, Byrski T, Gronwald J, Jakubowska A, Stawicka M, Gozdecka-Grodecka S, Szwiec M, Urbanski K, Mitus J, Marczyk E, Dziuba J, Wandzel P, Surdyka D, Haus O, Janiszewska H, Debniak T, Toloczko-Grabarek A, Medrek K, Masojc B, Mierzejewski M, Kowalska E, Narod SA, Lubinski J: Breast cancer predisposing alleles in Poland. Breast Cancer Res Treat 2005, 92: 19–24. 10.1007/s10549-005-1409-1
Amundadottir LT, Thorvaldsson S, Gudbjartsson DF, Sulem P, Kristjansson K, Arnason S, Gulcher JR, Bjornsson J, Kong A, Thorsteinsdottir U, Stefansson K: Cancer as a complex phenotype: pattern of cancer distribution within and beyond the nuclear family. PLoS Med 2004, 1: e65. 10.1371/journal.pmed.0010065
Kerber RA, O'Brien E: A cohort study of cancer risk in relation to family histories of cancer in the Utah population database. Cancer 2005, 103: 1906–1915. 10.1002/cncr.20989
Peto J, Easton DF, Matthews FE, Ford D, Swerdlow A: Cancer mortality in relatives of women with breast cancer: the OPCS Study. Int J Cancer 1996, 65: 275–283. 10.1002/(SICI)1097-0215(19960126)65:3<275::AID-IJC1>3.0.CO;2-X
Landgren O, Engels EA, Caporaso NE, Gridley G, Mellemkjaer L, Hemminki K, Linet MS, Goldin LR: Patterns of autoimmunity and subsequent chronic lymphocytic leukemia in Nordic countries. Blood 2006, 108: 292–296. 10.1182/blood-2005-11-4620
Matikaine N, Pukkala E, Schleutker J, Tammela TL, Koivisto P, Sankila R, Kallioniemi OP: Relatives of prostate cancer patients have an increased risk of prostate and stomach cancers: a population-based, cancer registry study in Finland. Cancer Causes Control 2001, 12: 223–230. 10.1023/A:1011283123610
Hemminki K, Vaittinen P: Familial cancer in Sweden: population-based study. Int J Oncol 1997, 11: 273–280.
Hemminki K, Li X, Plna K, Granstrom C, Vaittinen P: The nationwide Swedish family-cancer database-updated structure and familial rates. Acta Oncol 2001, 40: 772–777. 10.1080/02841860152619214
Hemminki K, Granstrom C, Chen B: The Swedish Family-Cancer Database: Update, Application to Colorectal Cancer and Cinical Relevance. Heredit Cancer in Clin Pract 2005, 3: 7–18.
IARC, (ed.): Cancer Incidence in Five Continents. IARC, Lyon; 2002.
Hemminki K, Rawal R, Bermejo JL: Prostate cancer screening, changing age-specific incidence trends and implications on familial risk. Int J Cancer 2005, 113: 312–315. 10.1002/ijc.20568
Gronberg H: Prostate cancer epidemiology. Lancet 2003, 361: 859–864. 10.1016/S0140-6736(03)12713-4
Pilebro B, Johansson R, Damber L, Damber JE, Stattin P: Population-based study of prostate-specific antigen testing and prostate cancer detection in clinical practice in northern Sweden. Scand J Urol Nephrol 2003, 37: 210–212. 10.1080/00365590310008064
Stattin P, Johansson R, Damber JE, Hellstrom M, Hugosson J, Lundgren R, Varenhorst E, Johansson JE: Non-systematic screening for prostate cancer in Sweden-survey from the National Prostate Cancer Registry. Scand J Urol Nephrol 2003, 37: 461–465. 10.1080/00365590310015778
Hemminki K, Bermejo JL: Effects of screening for breast cancer on its age-incidence relationships and familial risk. Int J Cancer 2005, 117: 145–149. 10.1002/ijc.21149
Center for Epidemiology: Cancer Incidence in Sweden 2002. Stockholm: The National Board of Health and Welfare; 2004.
Hampel H, Stephens JA, Pukkala E, Sankila R, Aaltonen LA, Mecklin JP, de la Chapelle A: Cancer risk in hereditary nonpolyposis colorectal cancer syndrome: later age of onset. Gastroenterology 2005, 129: 415–421.
Hemminki K, Eng C: Clinical genetic counselling for familial cancers requires reliable data on familial cancer risks and general action plans. J Med Genet 2004, 41: 801–807. 10.1136/jmg.2004.022731
Acknowledgements
Supported by Deutsche Krebshilfe, the Swedish Cancer Society, The Swedish Council for Working Life and Social Research and the EU, LSHC-CT-2004-503465. The Family-Cancer Database was created by linking registers maintained at Statistics Sweden and the Swedish Cancer Registry.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hemminki, K., Granström, C., Sundquist, J. et al. The updated Swedish family-cancer database used to assess familial risks of prostate cancer during rapidly increasing incidence. Hered Cancer Clin Pract 4, 186 (2006). https://doi.org/10.1186/1897-4287-4-4-186
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1897-4287-4-4-186