Abstract
Aims
Serum N-terminal pro-B-type natriuretic peptide (NT-proBNP) was lower in the general population with metabolic syndrome (MetS). The aim of this study was to evaluate the relationship between MetS and fasting serum NT-proBNP concentration in elderly persons.
Methods
Fasting blood samples were obtained from 84 elderly volunteers aged 65 years or older. MetS and its components were defined using diagnostic criteria from the International Diabetes Federation.
Results
Thirty-eight elderly persons (45.2%) had MetS. Fasting NT-proBNP level was negatively correlated with MetS among elderly patients (p = 0.001). Univariate linear regression analysis showed that age (r = 0.338; p = 0.002) was positively correlated with fasting serum log-NT-proBNP levels, while height (r = -0.253; p = 0.020), body weight (r = -0.238; p = 0.029), waist circumference (r = -0.270; p = 0.013), body fat mass (r = -0.356; p = 0.002) and triglyceride (r = -0.291; p = 0.007) were negatively correlated with fasting serum log-NT-proBNP levels among the elderly persons. Multivariate forward stepwise linear regression analysis of the significant variables showed that age (R2 change = 0.114, p = 0.011), triglyceride (R2 change = 0.118, p < 0.001), body fat mass (R2 change = 0.084, p < 0.001), and height (R2 change = 0.101, p < 0.001) were the independent predictor of fasting serum log-NT-proBNP levels in elderly persons.
Conclusions
NT-proBNP level is significantly reduced in elderly persons affected by MetS, and is significantly positively related to age, while negatively related to triglyceride, body fat mass, height in these subjects.
Similar content being viewed by others
Introduction
The heart secretes two natriuretic peptides, atrial natriuretic peptides (ANP) and B-type natriuretic peptides (BNP). They are widely known as body homeostasis regulators that oppose volume expansion [1]. BNP and its N-terminal counterpart, N-terminal pro-B-type natriuretic peptide (NT-proBNP), are cardiac biomarkers that have been established for the assessment of congestive heart failure [2, 3]. Recent studies also suggested natriuretic peptides are potent lipolytic agents that act in adipose tissue [4, 5]. Low levels of NT-proBNP might lead to reduced lipolysis and excessive weight gain, which may be one of the biological alterations that contribute to the development of metabolic syndrome in the general population (MetS) [6, 7].
In old age, fat is redistributed from subcutaneous to intra-abdominal visceral depots as well as other ectopic sites, including bone marrow, muscle and the liver. These changes are associated with increased risk of MetS [8]. MetS increased all-cause and cardiovascular disease mortality in a cohort study of Chinese aged 50 years or older [9]. There is no study about the association between serum NT-proBNP levels and MetS in elderly persons. The aim of this study was to investigate the relationship between the fasting serum NT-proBNP level and MetS among elderly persons.
Materials and methods
Participants
Between October 2009 and May 2010, one hundred elderly volunteers aged 65 years or older at a medical center in Hualien, eastern Taiwan were enrolled into this study. The Protection of the Human Subjects Institutional Review Board of Tzu-Chi University and Hospital approved this study. Patients were excluded if they had any acute infection (n = 2), acute myocardial infarction (n = 1), heart failure (n = 5), serum creatinine ≥ 1.2 mg/dl at the time of blood sampling (n = 7) or if they refused to provide informed consent for the study (n = 1). Heart failure defined by the American College of Cardiology Foundation and the American Heart Association 2005 Guidelines. Heart failure is a complex clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood [10]. Total about eighty-four elderly volunteers (28 males and 56 females) were included in this study.
Anthropometric analysis
Body weight was measured to the nearest half-kilogram with patients wearing light clothing and without shoes. Height was measured to the nearest 0.5 cm. Waist circumference was measured by tape around patient’s waist from the point between patient’s lowest ribs and patient’s hip bones by placing patient’s hands on patient’s hips. The body mass index (BMI) was calculated as weight (kilograms) divided by height squared (meters). Bioimpedance measurements of fat mass were performed at the bedside according to the standard tetrapolar whole body (hand-foot) technique, using a single-frequency (50-kHz) analyzer (Biodynamic-450, Biodynamics Corporation, Seattle, USA). Measurements were carried out by the same operator. Fat mass was collected and analyzed by specific formulae supplied by the manufacturer. [11, 12].
2D echocardiographic examination
The 2D echocardiographic recordings were obtained in all patients using commercially available machines. Ejection fraction was calculated by a modification of the method of Quinones et al. [13]. The left ventricular (LV) mass index was calculated as a ratio of LV mass to body surface area. Transmitral flow velocity curves were recorded to measure peak early diastolic (E) and late diastolic (A) velocities. There are three components of the tissue Doppler profile that are routinely measured: the systolic myocardial velocity (S’); the early diastolic myocardial velocity (E’); and the late diastolic myocardial velocity (A’) as previously described [14].
Biochemical investigations
Fasting blood samples of approximately 5 ml for measuring complete blood count (Sysmex K-1000, Bohemia, NY, USA) and other factors were immediately centrifuged at 3000 g for 10 min. Serum levels of blood urea nitrogen (BUN), creatinine (Cre), fasting glucose, total cholesterol (TCH), triglyceride (TG), high-density lipoprotein cholesterol (HDL-cholesterol), and low-density lipoprotein cholesterol (LDL-cholesterol) were measured using an autoanalyzer (COBAS Integra 800, Roche Diagnostics, Basel, Switzerland). Blood samples were assayed for NT-proBNP by electrochemiluminescence immunoassay on the Elecsys 2010 Immunoanalyzer (Roche Diagnostics, Indianapolis, IN, USA).
Metabolic syndrome and its components
The prevalence of MetS was defined using the International Diabetes Federation definition [15]. People were classified as having MetS if they had central (abdominal) obesity with a waist circumference ≥ 90 cm (men) or ≥ 80 cm (women) (Chinese criteria), and matched two or more of the following criteria: fasting serum glucose of 110 mg/dl or more, triglycerides of 150 mg/dl or higher, HDL-cholesterol level less than 40 mg/dl in men or less than 50 mg/dl in women, or blood pressure of 130/85 mmHg or higher. The use of antihypertensive medication was considered as indicative of high blood pressure in this analysis. Type 2 diabetes was determined according to World Health Organization criteria [16]. A person was regarded as diabetic if the fasting plasma glucose was either 126 mg/dl or more, or if the 2 h glucose during an oral glucose tolerance test was 200 mg/dl or more, or if he/she was using diabetes medication (oral or insulin).
Statistical analysis
Data are expressed as means ± standard deviation (SD) and were tested for normal distribution by Kolmogorov-Smirnov test. Categorical variables were analyzed by the Chi-square test. Comparisons between patients were performed using the Student’s independent t test (two-tailed) for normally distributed data or the Mann–Whitney U test for parameters that presented with non-normal distribution (NT-proBNP). Because the NT-proBNP was non-normal distribution, we used log-NT-proBNP (logarithm of NT-proBNP to base 10) and noted log-NT-proBNP was normal distribution. The significance of differences of NT-proBNP between numbers of metabolic syndrome criteria was analyzed by the Kruskal-Wallis analysis of variance (AVONA) test. Clinical variables that correlated with serum log-NT-proBNP levels in elderly persons were evaluated by univariate linear regression analyses. Variables that were significantly associated with log-NT-proBNP in elderly persons were tested for independency in multivariate forward stepwise regression analysis. Data were analyzed using SPSS for Windows (version 13.0; SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Results
The clinical, echocardiographic recordings and laboratory characteristics of the elderly persons are presented in Table 1 and Table 2. Medical histories included: diabetes (n = 30; 35.7%), and hypertension (n = 68; 80.9%). The use of drugs included: angiotensin receptor blocker (ARB; n = 40; 47.4%), angiotensin-converting enzyme inhibitor (ACEI; n = 16; 19.1%), calcium channel blocker (CCB; n = 46; 54.8%), β-blocker (n = 38; 45.2%), statin (n = 20; 23.8%), fibrate (n = 10; 11.9%), sulfonylurea (n = 8; 9.5%), and metformin (n = 18; 21.4%). Thirty-eight patients (45.2%) had MetS, whereas 46 patients (54.8%) did not. Elderly persons who had MetS had lower serum fasting NT-proBNP levels than those without MetS (p = 0.001). NT-proBNP levels did not differ statistically by gender distribution, diabetes, hypertension, ARB, ACEI, CCB, β-blocker, statin, fibrate, sulfonylurea, or metformin drugs used.
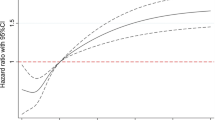
Fasting serum NT-proBNP levels in different metabolic syndrome diagnostic criteria are presented in Figure 1. There was a tendency for decreased fasting NT-proBNP levels as the number of diagnostic criteria for metabolic syndrome in patients increased. A statistically significant difference between the number of metabolic syndrome criteria and serum NT-proBNP levels in elderly persons (p = 0.030) was established.
The univariate linear analysis of fasting serum log-NT-proBNP levels in elderly persons is presented in Table 3. Ages (r = 0.338; p = 0.002) was positively correlated with fasting serum log-NT-proBNP levels, while height (r = -0.253; p = 0.020), body weight (r = -0.238; p = 0.029), waist circumference (r = -0.270; p = 0.013), body fat mass (r = -0.356; p = 0.002) and triglyceride (r = -0.291; p = 0.007) were negatively correlated with fasting serum log-NT-proBNP levels among the elderly persons (Table 3).
Multivariate forward stepwise linear regression analysis of the variables that were significantly associated with fasting serum log-NT-proBNP levels among elderly persons showed that age (β = 0.242, R2 change = 0.114, p = 0.011), triglyceride (β = -0.392, R2 change = 0.118, p < 0.001), body fat mass (β = -0.398, R2 change = 0.084, p < 0.001), and height (β = -0.362, R2 change = 0.101, p < 0.001) were the independent predictor of fasting serum log-NT-pro-BNP levels (Table 4).
Discussion
The results of our study showed that the fasting NT-proBNP level was negatively associated with MetS in elderly persons, and that age, triglyceride, body fat mass and height were independent predictors of fasting serum NT-proBNP levels.
In elderly people disorders occur that are closely related to the ageing process. They include symptoms from the cardiovascular system, such as elevated systolic blood pressure, pulse pressure, increased mass of the left ventricle and more frequent ischemic heart disease, as well as cardiac arrhythmias, and particularly atrial fibrillation [17]. As compared to normal volunteers echocardiographic data at Aizawa et al. [14] our study noted the E/A ratio and E’ were lower, and the LV mass index was higher in elderly persns.
MetS is a constellation of cardiovascular risk factors that has been associated with increased risk of cardiovascular disease, diabetes, and mortality as well as other adverse health outcomes [15]. Aging is characterized by body fat redistribution with increased visceral fat and relative loss of subcutaneous fat, especially in the periphery. The impaired capacity of fat tissue to store lipids associated with aging may be responsible for increased systemic free fatty acid exposure, leading to ectopic fat deposition, lipotoxicity and metabolic disease [8]. Anthropometric changes with an increase in fat mass with a parallel decline in fat free mass, environmental changes such as dietary habit changes and reduced physical activity, neurohormonal variations which may have an opposing effect on insulin, and an increase in oxidative stress in the elderly induce insulin resistance and are associated with impaired glucose handling, mainly through the decline of insulin action in the elderly [18]. The MetS is associated with the incidence of diabetes, and the synergy between MetS and diabetes is an important risk factor for all-cause mortality in elderly subjects [19]. MetS in an elderly population is a proven risk factor for all-cause and cardiovascular disease mortality [9]. The prevalence of MetS in the United States is 43.5% and 42.0% for participants aged 60 through 69 years and aged at least 70 years, respectively [20]. Our study noted the overall prevalence of MetS is 45.2% in the elderly and the prevalence of MetS was 42.9% (12/28) in men and 46.4% (26/56) in women.
The renin-angiotensin-aldosterone system is activated in obese patients and angiotensin II acting as a ‘growth factor’ for adipose tissue growth and development [4]. BNP binds its common receptor, guanylyl cyclase-A (GC-A), which leads to biological actions through a cyclic guanosine monophosphate (cGMP)-dependent pathway and has an inhibition effect of the renin–angiotensin–aldosterone axis [2]. So, low levels of natriuretic peptide may activate the renin-angiotensin-aldosterone system, which may contribute to the development of obesity. In normal subjects, natriuretic peptide may affect the homoeostasis of glucose and lipid metabolism, partly through the reduction in adipogenesis, as well as the increased release and more efficient consumption of non-esterified fatty acids by peripheral tissues [21]. It can be speculated that low levels of natriuretic peptide may lead to reduced lipolysis and excessive weight gain, which may be one of the biological alterations that contribute to the development of obesity [5]. BNP through a cGMP-dependent pathway can promote muscle mitochondrial biogenesis and fat oxidation, as to prevent obesity and glucose intolerance in mice [22]. Some studies did not find an association between serum NT-proBNP concentrations and MetS [23, 24]. However, other studies noted serum NT-proBNP was lower in the general population with MetS [6, 7]. Recent study on elderly population from Poland noted obese patients had significantly more frequently NT-proBNP values < 400 pg/ml (73.0%) and less frequently NT-proBNP values > 2000 pg/ml (2.8%) [25]. Our study also noted that elderly persons with MetS had lower fasting serum NT-proBNP levels. Moreover, our study also noted a tendency for decreasing fasting serum NT-proBNP levels as the number of diagnostic criteria for metabolic syndrome in elderly persons increased.
NT-proBNP values were substantially higher in women compared to men at every age, and levels increased with increasing age for both genders in healthy individuals from the Framingham Heart Study Generation 3 cohort study [26]. This study also noted upper reference limit for NT-proBNP implied is more than 2-fold higher in women than men [26]. Our result also showed that age was positively correlated with fasting serum log-NT-proBNP levels and nearly 2-fold higher in women than men among the elderly persons. Although gender differences in circulating natriuretic peptides have been previously reported, the underlying mechanisms remain unclear [27]. In symptomatic left ventricular systolic heart failure patients a higher BMI is associated with decreased NT-proBNP levels [28]. Our study noted that height and body weight were negatively correlated with fasting serum log-NT-proBNP levels in elder persons, but did not differ statistically by BMI in this study. Plasma NT-proBNP was inversely associated with visceral adipose tissue volumes measured by multidetector computed tomography in a study of 1,873 community-based individuals [29]. However, another study noted NT-proBNP was inversely associated with hematocrit and hepatic steatosis, while no association was found with waist circumference and skinfold fat measurement in the elderly [30]. Serum NT-proBNP was inversely related to triglyceride [6, 24]. Our study also showed that waist circumference, body fat mass, and triglyceride were negatively correlated with fasting serum log-NT-proBNP levels among the elderly persons. Multivariate forward stepwise linear regression analysis of significant variables showed that age, triglyceride, body fat mass, and height were waist circumference was the independent predictor of fasting serum log-NT-proBNP levels in our study.
Pharmacological interventions have been shown to influence serum NT-proBNP in humans. The use of valsartan reduces plasma concentrations of NT-proBNP in post–myocardial infarction and congestive heart failure patients [31]. After 8 weeks of treatment with losartan a significant decrease was noted in the levels of NT-proBNP in patients after acute myocardial infarction [32]. NT-proBNP was significantly reduced after six months of treatment with enalapril or carvedilol combined with enalapril treatment in stable systolic heart failure patients. In contrast, no change was observed in the carvedilol group [33]. Atorvastatin treatment reduced NT-proBNP levels in heart failure patients [34]. Our results did not show a relationship between statins or other drugs (angiotensin receptor blocker, angiotensin-converting enzyme inhibitor, calcium channel blocker, or β-blocker) and serum NT-proBNP among elderly persons. Further studies are required to elucidate the relationship between medication and NT-proBNP in elderly persons.
Our study has some limitations. First, the number of patients enrolled was small and there was weak statistical power in terms of the small number of patients. Secondly, this study had a cross-sectional design. NT-proBNP, have been shown a high prognostic value in total mortality, cardiovascular mortality in the elderly population and is independent predictor of all-cause mortality in patients with acute heart failure at 30 days and 1 year after emergency department in elderly persons [35, 36]. Therefore, our findings should be investigated in long-term prospective studies before a causal relationship between serum NT-proBNP and MetS in elderly persons can be established. It should also be noted that BNP can enhance adiponectin production by human adipocytes in vitro and even in patients with heart failure [37]. Serum adiponectin values were found to correlate inversely with the presence of MetS [38]. Adiponectin is independently associated with NT-proBNP in the general population [39] and in elderly coronary artery disease patients [40]. Additional studies are required to ascertain whether the serum concentration of adiponectin is associated with NT-proBNP in elderly persons.
Conclusion
Low levels of NT-proBNP might lead to reduced lipolysis and excessive weight gain, which may be one of the biological alterations that contribute to the development of MetS. The present study shows a negative association between circulating fasting NT-proBNP and MetS among elderly persons. Age, triglyceride, body fat mass and height were independent predictor of the serum log-NT-proBNP level among elderly persons.
Abbreviations
- ANP:
-
Atrial natriuretic peptides
- BNP:
-
B-type natriuretic peptides
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- MetS:
-
Metabolic syndrome
- BMI:
-
Body mass index
- BUN:
-
Blood urea nitrogen
- Cre:
-
Creatinine
- HDL-C:
-
High-density lipoprotein-cholesterol
- LDL-C:
-
Low-density lipoprotein-cholesterol
- TCH:
-
Total cholesterol
- TG:
-
Triglyceride
- GC-A:
-
Guanylyl cyclase-A
- cGMP:
-
Cyclic guanosine monophosphate.
References
Potter LR: Natriuretic peptide metabolism, clearance and degradation. FEBS J. 2011, 278: 1808-1817. 10.1111/j.1742-4658.2011.08082.x.
Clerico A, Recchia FA, Passino C, Emdin M: Cardiac endocrine function is an essential component of the homeostatic regulation network: physiological and clinical implications. Am J Physiol Heart Circ Physiol. 2006, 290: H17-H29.
Gopal DJ, Iqbal MN, Maisel A: Updating the role of natriuretic peptide levels in cardiovascular disease. Postgrad Med. 2011, 123: 102-113. 10.3810/pgm.2011.11.2500.
Sarzani R, Salvi F, Dessì-Fulgheri P, Rappelli A: Renin-angiotensin system, natriuretic peptides, obesity, metabolic syndrome, and hypertension: an integrated view in humans. J Hypertens. 2008, 26: 831-843. 10.1097/HJH.0b013e3282f624a0.
Beleigoli AM, Diniz MF, Ribeiro AL: Natriuretic peptides: linking heart and adipose tissue in obesity and related conditions: a systematic review. Obes Rev. 2009, 10: 617-626. 10.1111/j.1467-789X.2009.00624.x.
Olsen MH, Hansen TW, Christensen MK, Gustafsson F, Rasmussen S, Wachtell K, et al: N-terminal pro brain natriuretic peptide is inversely related to metabolic cardiovascular risk factors and the metabolic syndrome. Hypertension. 2005, 46: 660-666. 10.1161/01.HYP.0000179575.13739.72.
Bao Y, Shang X, Zhou L, Hu R, Li Y, Ding W: Relationship between N-terminal pro-B-type natriuretic peptide levels and metabolic syndrome. Arch Med Sci. 2011, 7: 247-256.
Sepe A, Tchkonia T, Thomou T, Zamboni M, Kirkland JL: Aging and regional differences in fat cell progenitors - a mini-review. Gerontology. 2011, 57: 66-75. 10.1159/000279755.
Sun DL, Wang JH, Jiang B, Li LS, Li LS, Wu L, et al: Metabolic syndrome vs. its components for prediction of cardiovascular mortality: a cohort study in Chinese elderly adults. J Geriatr Cardiol. 2012, 9: 123-129. 10.3724/SP.J.1263.2012.01172.
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, et al: 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009, 119: e391-e479.
Hsieh JC, Wang JH, Lee CJ, Chen YC, Liou HH, Hsu BG: Low serum long-acting natriuretic peptide level correlates with metabolic syndrome in hypertensive patients: a cross-sectional study. Arch Med Res. 2013, 44: 215-220. 10.1016/j.arcmed.2013.03.001.
Wang JH, Lee CJ, Hsieh JC, Chen YC, Hsu BG: Inversely association of long-acting natriuretic peptide with metabolic syndrome in congestive heart failure patients. Diabetol Metab Syndr. 2013, 5: 19-10.1186/1758-5996-5-19.
Quinones MA, Waggoner AD, Reduto LA, Nelson JG, Young JB, Winters WL, et al: A new, simplified and accurate method for determining ejection fraction with two-dimensional echocardiography. Circulation. 1981, 64: 744-753. 10.1161/01.CIR.64.4.744.
Aizawa Y, Sakata Y, Mano T, Takeda Y, Ohtani T, Tamaki S, et al: Transition from asymptomatic diastolic dysfunction to heart failure with preserved ejection fraction – roles of systolic function and ventricular distensibility. Circ J. 2011, 75: 596-602. 10.1253/circj.CJ-10-1037.
Alberti KG, Zimmet PZ, Shaw J: Metabolic syndrome - a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006, 23: 469-480. 10.1111/j.1464-5491.2006.01858.x.
Alberti KG, Zimmet PZ: Definition, diagnosis and classification of diabetes mellitus and its complications. I. Diagnosis and classification of diabetes mellitus: provisional report of a WHO consultation. Diabet Med. 1998, 15: 539-553. 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S.
Lakatta EG, Levy D: Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: part I: aging arteries: a “set up” for vascular disease. Circulation. 2003, 107: 139-146. 10.1161/01.CIR.0000048892.83521.58.
Sinclair A, Viljoen A: The metabolic syndrome in older persons. Clin Geriatr Med. 2010, 26: 261-274. 10.1016/j.cger.2010.02.011.
Noale M, Maggi S, Zanoni S, Limongi F, Zambon S, Crepaldi G, ILSA working group: The metabolic syndrome, incidence of diabetes and mortality among the elderly: the Italian Longitudinal Study of Ageing. Diabetes Metab. 2012, 38: 135-141. 10.1016/j.diabet.2011.09.005.
Ford ES, Giles WH, Dietz WH: Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002, 287: 356-359. 10.1001/jama.287.3.356.
Savoia C, Volpe M, Alonzo A, Rossi C, Rubattu S: Natriuretic peptides and cardiovascular damage in the metabolic syndrome: molecular mechanisms and clinical implications. Clin Sci. 2009, 118: 231-240. 10.1042/CS20090204.
Miyashita K, Itoh H, Tsujimoto H, Tamura N, Fukunaga Y, Sone M, et al: Natriuretic peptides/cGMP/cGMP-dependent protein kinase cascades promote muscle mitochondrial biogenesis and prevent obesity. Diabetes. 2009, 58: 2880-2892. 10.2337/db09-0393.
Sezen Y, Baş M, Demirbag R, Yildiz A, Celik H, Aksoy S: N-terminal pro-brain natriuretic peptide in cases with metabolic syndrome and its relationship with components of metabolic syndrome and left ventricular mass index. Clin Biochem. 2009, 42: 1500-1503. 10.1016/j.clinbiochem.2009.07.007.
Li WY, Chiu FC, Chien YF, Lin JW, Hwang JJ: Association of amino-terminal pro-brain natriuretic peptide with metabolic syndrome. Intern Med. 2011, 50: 1143-1147. 10.2169/internalmedicine.50.4765.
Nadrowski P, Chudek J, Grodzicki T, Mossakowska M, Skrzypek M, Wiecek A, et al: Plasma level of N-terminal pro brain natriuretic peptide (NT-proBNP) in elderly population in Poland - The PolSenior Study. Exp Gerontol. 2013, 48: 852-857. 10.1016/j.exger.2013.05.060.
Fradley MG, Larson MG, Cheng S, McCabe E, Coglianese E, Shah RV, et al: Reference limits for N-terminal-pro-B-type natriuretic peptide in healthy individuals (from the Framingham Heart Study). Am J Cardiol. 2011, 108: 1341-1345. 10.1016/j.amjcard.2011.06.057.
Wang TJ, Larson MG, Levy D, Leip EP, Benjamin EJ, Wilson PW, et al: Impact of age and sex on plasma natriuretic peptide levels in healthy adults. Am J Cardiol. 2002, 90: 254-258. 10.1016/S0002-9149(02)02464-5.
Taçoy G, Açikgöz K, Kocaman SA, Ozdemir M, Cengel A: Is there a relationship between obesity, heart rate variability and inflammatory parameters in heart failure?. J Cardiovasc Med. 2010, 11: 118-124. 10.2459/JCM.0b013e328332e730.
Cheng S, Fox CS, Larson MG, Massaro JM, McCabe EL, Khan AM, et al: Relation of visceral adiposity to circulating natriuretic peptides in ambulatory individuals. Am J Cardiol. 2011, 108: 979-984. 10.1016/j.amjcard.2011.05.033.
Muscari A, Berzigotti A, Bianchi G, Giannoni C, Ligabue A, Magalotti D, et al: Non-cardiac determinants of NT-proBNP levels in the elderly: relevance of haematocrit and hepatic steatosis. Eur J Heart Fail. 2006, 8: 468-476. 10.1016/j.ejheart.2005.10.018.
Anand IS, Fisher LD, Chiang YT, Latini R, Masson S, Maggioni AP, et al: Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (Val-HeFT). Circulation. 2003, 107: 1278-1283. 10.1161/01.CIR.0000054164.99881.00.
Marinsek M, Sinkovic A: A randomized trial comparing the effect of ramipril and losartan in survivors of ST-elevation myocardial infarction. J Int Med Res. 2009, 37: 1577-1587. 10.1177/147323000903700536.
Rosenberg J, Gustafsson F, Remme WJ, Riegger GA, Hildebrandt PR: Effect of beta-blockade and ACE inhibition on B-type natriuretic peptides in stable patients with systolic heart failure. Cardiovasc Drugs Ther. 2008, 22: 305-311. 10.1007/s10557-008-6099-6.
Stypmann J, Schubert A, Welp H, Schulte H, Assmann G, Breithardt G, et al: Atorvastatin therapy is associated with reduced levels of N-terminal prohormone brain natriuretic peptide and improved cardiac function in patients with heart failure. Clin Cardiol. 2008, 31: 478-481. 10.1002/clc.20273.
Muscari A, Bianchi G, Forti P, Giansante C, Giovagnoli M, Magalotti D, et al: A comparison of risk factors as predictors of cardiovascular and non-cardiovascular mortality in the elderly people–relevance of N-terminal pro-B-type natriuretic peptide and low systolic blood pressure. Int J Clin Pract. 2013, 67: 1182-1191. 10.1111/ijcp.12195.
Golcuk Y, Golcuk B, Velibey Y, Oray D, Atilla OD, Colak A, et al: Predictive cutoff point of admission N-terminal pro-B-type natriuretic peptide testing in the ED for prognosis of patients with acute heart failure. Am J Emerg Med. 2013, 31: 1191-1195. 10.1016/j.ajem.2013.04.038.
Tsukamoto O, Fujita M, Kato M, Yamazaki S, Asano Y, Ogai A, et al: Natriuretic peptides enhance the production of adiponectin in human adipocytes and in patients with chronic heart failure. J Am Coll Cardiol. 2009, 53: 2070-2077. 10.1016/j.jacc.2009.02.038.
Hung J, McQuillan BM, Thompson PL, Beilby JP: Circulating adiponectin levels associate with inflammatory markers, insulin resistance and metabolic syndrome independent of obesity. Int J Obes. 2008, 32: 772-779. 10.1038/sj.ijo.0803793.
Sung SH, Chuang SY, Sheu WH, Lee WJ, Chou P, Chen CH: Relation of adiponectin and high-sensitivity C-reactive protein to pulse-wave velocity and N-terminal pro-B-type natriuretic peptide in the general population. Am J Cardiol. 2009, 103: 1411-1416. 10.1016/j.amjcard.2009.01.355.
Baldasseroni S, Mannucci E, Orso F, Di Serio C, Pratesi A, Bartoli N, et al: Adiponectin in outpatients with coronary artery disease: independent predictors and relationship with heart failure. Nutr Metab Cardiovasc Dis. 2012, 22: 292-299. 10.1016/j.numecd.2011.03.012.
Acknowledgements
This study was supported by grants from Buddhist Tzu Chi Hospital (TCRD 98–32 and TCRD 100–02) in Taiwan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
All authors declare that they have no competing interests.
Authors’ contributions
LCJ researched and analyzed data. WJH and HBG designed of the study, interpretation of data and wrote the manuscript. HJC, CYC and WJH collected the data. All authors read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wang, JH., Lee, CJ., Hsieh, JC. et al. N-terminal pro-B-type natriuretic peptide level inversely associates with metabolic syndrome in elderly persons. Diabetol Metab Syndr 6, 15 (2014). https://doi.org/10.1186/1758-5996-6-15
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1758-5996-6-15