Abstract
For persons living with HIV, hepatitis C is a major public health problem that must be controlled and could be eliminated. The challenge arises because the hepatitis C virus (HCV) is prevalent among HIV-infected persons in most parts of the world, because HIV worsens all HCV outcomes, and because HCV may add additional individual economic and psychosocial complications to HIV disease. Despite the major benefits of antiretroviral therapy on HIV outcomes, antiretroviral therapy is not sufficient to halt the complications of HCV. Nonetheless, HCV can be controlled at all stages, including prevention of infection and cure. Thus, HCV is an eradicable disease. There are significant inequalities worldwide in HCV control that could markedly constrain the impact of these measures.
Similar content being viewed by others
Review
Public health importance
HCV coinfection is common
Many persons living with HIV (PLHIV) are coinfected with the hepatitis C virus (HCV). In Europe, the United States and Australia, approximately one-quarter of PLHIV are coinfected with HCV. But these averages mask marked differences in HCV prevalence based on the route through which HIV was acquired. By far, HCV coinfection rates are highest among persons who have acquired HIV from injection drug use (Figure 1).
Rockstroh and coworkers reported in the large EuroSIDA cohort that 1519 (92%) of HIV-infected persons with a history of injecting drug use were also HCV exposed [1]. In one study from Russia, 91% of HIV-infected injecting drug users (IDUs) had HCV antibodies [2]. Similarly high HIV/HCV coinfection prevalence rates have been reported from the USA and Australia [3, 4].
In Asia also, nearly all HIV-infected IDUs also has HCV. For example, in IDUs from Chennai, India, the prevalence of coinfection with anti-HCV was 86% [5]. Among IDUs in northern Vietnam, almost all (98.5%) HIV-infected IDUs were also co-infected with HCV [6]. Likewise, HCV infection has been reported in more than 90% of IDUs in some regions in southern China [7, 8]. Given the linkage with illicit drug use, HCV is also a special problem for PLHIV in prisons [9]. In addition to risk-prone illicit drug use, unsafe tattooing contributes to HCV infection in prisons [10].
In contrast to IDUs, HCV coinfection occurs in less than 15% of persons who acquired HIV from sexual intercourse [1, 11]. One important caveat is the recent series of HCV outbreaks among HIV-infected men who have sex with men (MSM) [12, 13]. For example, Danta and coworkers described 111 acute HCV infections among MSM in England that were associated with high-risk sexual practices, as well as non-injection use of illicit drugs [12]. It is now clear that this is a widespread international trend [14].
Basis for HIV/HCV coinfection
There are biologic, sociologic and historic reasons that HCV coinfection is common in HIV-infected IDUs. Studies following a single needlestick exposure show that HCV is approximately a log10 more transmissible than HIV (1/100 versus <1/1000) [15]. With transfusion of large blood volumes, such as occurred in haemophilia populations in the early 1980s, these differences in transmissibility were inconsequential. Nearly all who were exposed by transfusion became infected [16].
However, transmission of infectious diseases by drug use typically involves inocula that are 4-5 log10 smaller. The average HIV plasma viral load is approximately a log10 less than HCV [17, 18]. Thus, with the very small inocula that are typically involved in injection drug use, it is likely that the number of infectious virions in blood is a major factor in the greater transmission of HCV compared with HIV. It is also possible that each HIV virion is less transmissible or less environmentally stable than HCV. Ultimately, the net percutaneous transmissibility of small blood inocula is lower for HIV than for HCV and a major reason for the greater HCV incidence and prevalence among IDUs (Figure 2).
Incidence of HIV and HCV among Baltimore IDUs. Adapted from Villano et al [46].
Less is known about the basis for the sometimes contradictory evidence regarding sexual transmission of HCV. For example, there are higher than expected HCV prevalence rates in populations with high-risk sexual practices, including MSM, but there is very low HCV incidence between discordant couples and in some MSM populations. It is possible that, like HIV, HCV is more transmissible just after acute infection, before formation of neutralizing antibodies and when viral titers are higher.
However, while this feature might explain low/no sexual transmission from persons with chronic hepatitis C and relatively more transmission in settings where multiple exposures to acute infections occur, there is no evidence to support the conjecture. One explanation for the recent rise in transmission among MSM is that antiretroviral therapy has reduced the fear of HIV, resulting in higher risk sexual practices than when HIV was uniformly fatal. Increased use of illicit drugs by injection or non-injection routes may also contribute. In addition, it is also possible that there is simply a greater reservoir of HCV infection among MSM than in prior years, increasing the likelihood of exposure.
Historically, the population reservoir of HCV also antedated HIV. HCV prevalence markedly expanded during the mid1900s and is strongly correlated with stepped-up production of syringes and their worldwide use both for conventional and illicit drugs [19–21]. This trend allowed HCV to spread throughout the world and explains the five- to 20-fold increased HCV prevalence rates in certain regions where unsafe injections were widespread, and among IDUs [21]. There is a tendency of older IDUs to initiate new users by inoculating themselves first. Since older IDUs are often HCV infected, this practice contributes to rapid acquisition of HCV among IDUs [22]. HIV infection has overspread IDU populations more recently than HCV which was distributed decades earlier.
In Baltimore, the HIV prevalence in various risk groups was extremely low in 1980 and rose sharply in the early 1990s [23, 24]. Consequently, most HIV/HCV-coinfected IDUs acquired HCV years before HIV, and for every one HIV/HCV-coinfected IDU, there are usually two others infected with HCV but not HIV. In Asia, HIV incidence and prevalence rates first rose in the mid and late 1980s, especially among IDUs. While there are certainly individual instances in which HIV infection occurred first, in most populations in which injection drug use antedated the introduction of HIV, IDUs were already infected with HCV. Since HIV infects activated T cells, the immunologic control of an infectious disease like HCV may differ if it first occurs after a person is HIV infected, and that consideration may explain differences in HCV natural history and seroreversion rates in various studies.
HIV infection complicates the course of hepatitis C
Although the mechanism is really not well understood, HCV infection has a well-characterized course that is adversely affected at every stage by HIV (Figure 3). Although 30% to 40% of persons spontaneously clear HCV infection, the chances of spontaneous resolution are at least two-fold lower in HIV/HCV-coinfected persons [25]. Those who do develop chronic hepatitis C have higher HCV viral loads if they are coinfected with HIV than those with just HCV [26].
Likewise, persons chronically infected with the same HCV genotype are about half as likely to respond to the same dose and duration of peginterferon and ribavirin therapy if they are HIV coinfected compared with those with just HCV [27, 28]. HIV/HCV-coinfected persons are also twice as likely to develop cirrhosis over a shorter period of time [29]. Clinical manifestations of liver failure, such as ascites, encephalopathy and esophageal varices, all occur more often in HIV/HCV-coinfected persons [30].
Antiretroviral therapy is not sufficient to negate the effects of HIV on the course of hepatitis C
Antiretroviral therapy is probably the most important biomedical breakthrough in the past two decades. Rates of HIV-related opportunistic infection and related mortality have sharply dropped since adoption of antiretroviral therapy in the mid 1990s. Antiretroviral therapy also worked in sub-Saharan Africa and wherever there was a public health system to deliver it. Transmission of HIV to infants is also dramatically reduced in settings where antiretroviral therapy is given. Even the relatively hard-to-tolerate first-generation antiretroviral therapy reduced mortality.
The enormous effectiveness of antiretroviral therapy and the observation that HIV makes liver disease worse raises the question of whether antiretroviral therapy eliminates or at least attenuates the effect. This is an intense area of investigation with too much data on both sides of the question to review here. What is clear is that antiretroviral therapy is not sufficient to prevent complications of HCV, antiretroviral therapy does not affect the rate of HCV persistence, and it does not diminish the HCV viral load (in some persons, antiretroviral therapy actually increases the HCV-RNA level by a small amount) [31].
Antiretroviral therapy might improve the response to interferon and ribavirin, but this hypothesis has never been appropriately tested, and, since the majority of published data on peginterferon/ribavirin response in HIV/HCV-coinfected persons are on persons taking fully suppressive antiretroviral therapy, it is clear that "normal" responses are not restored. Likewise, rapid progression of liver fibrosis has been described even in persons taking fully suppressive antiretroviral therapy, making it clear that antiretroviral therapy is not sufficient to control HCV infection in PLHIV.
While the lifespan of HIV-infected persons taking antiretroviral therapy has been prolonged, the lives of those coinfected with HCV remain much shorter. In one study from Denmark, mortality rates from the age of 25 years were compared in 3990 HIV-infected persons with the general population, and survival curves were fitted [32]. Mortality dropped from a high of 124/1000 person years (PYs) in the pre-antiretroviral therapy period to 38/1000 PYs in 1997-1999 to 25/1000 PYs in 2000-2005. However, the impact was markedly different by HCV coinfection status, with mortality rates in 2000-2005 of 57/1000 PYs among the HCV coinfected compared with 19/1000 among those without known HCV infection (Figure 4).
Markedly lower survival for HIV/HCV-coinfected persons in Denmark: 2000-2005. Reproduced from Lohse et al [32].
By removing the HCV-coinfected persons, survival of HIV-infected persons on antiretroviral therapy was expected to approach that of the general population, 38.9 versus 51.1 years. Some of this is caused by other health problems, like overdose or accidents. However, liver disease is now the second leading cause of death among persons with HIV taking antiretroviral therapy [33, 34]. Given the systematic underreporting of liver disease, the true impact is likely greater.
Beyond statistics
There are consequences of HCV infection that are often not appreciated by physicians and public health officials. Since HCV often comes from injecting drug use, ongoing infection can be an indelible scar of a difficult phase of life. Having overcome dependency and other related challenges and having achieved an undetectable HIV-RNA on antiretroviral therapy, HCV can represent a major residual concern for PLHIV.
There may also be stigma associated with being HCV infected [35]. In some societies, this can be extremely severe. For those who have been undergoing HIV treatment, or have been in search of appropriate HIV drug combinations, the addition of an HCV regimen can be discouraging. Often already having undergone a battle with the HIV medications, coinfected persons may not emotionally or psychologically embrace the addition of highly toxic drugs to already complex treatment plans [36]. Patients have various levels of tolerance, which together with the different side-effect experiences, may produce an array of responses from little perceivable impact on daily functions to major suffering and outright non-compliance. The majority of patients, of course, fall somewhere in between, and none enjoy HCV treatment.
Once diagnosed with HCV, IDUs who historically associate needle use with illicit drug use, now must inject themselves with a compound that often exacerbates depression [27]. For newly recovering addicts, this process, along with the HCV diagnosis, can be detrimental to their efforts to maintain abstinence from mood-altering drugs, and, therefore, they may even refuse to participate, become non-compliant, or return to illicit drug use. For some of the co-infected persons, especially young HIV-positive persons, not responding to treatment constitutes a failure of modern medicine to meet their health needs. This realization may produce all types of psychological responses, like self-blame, severe depression or misplaced rage.
Control of HCV infection
Proof-of-principle studies have demonstrated that all phases of control are possible, from prevention to treatment. At the same time, most research suggests that HCV control will create huge disparities in outcomes.
HCV transmission can be prevented
HCV transmission can clearly be prevented. Transfusion transmission of HCV has virtually been eliminated in any setting where donations are screened for HCV antibodies and RNA [37]. Likewise, nosocomial transmission has been reduced by observance of blood-borne precautions.
Prevention of HCV transmission among IDUs can be achieved but is more difficult than HIV
Harm-reduction efforts, such as needle exchange, have been associated with reductions in HIV and HCV incidences in some settings. In Baltimore, HIV incidence rates among IDUs have dropped markedly from ~5 per 100 person years in 1990 to nearly zero since 2000. In the same Baltimore cohort, HCV incidence dropped from 22 to eight per 100 person years over the same time span (Mehta S, personal communication).
Given the greater transmissibility of HCV and the greater reservoir of IDUs already infected (as we have discussed), it is not surprising that even stronger harm-reduction measures will be needed to eliminate new HCV infections. If HCV is a log10 more transmissible than HIV, public health interventions may need to be an order of magnitude stronger to control HCV.
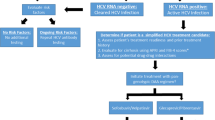
Control of chronic hepatitis C
HCV infection can also be controlled even after it occurs. The first step in controlling chronic hepatitis C is detecting infection by screening and testing. Nearly all guidelines indicate that HIV-infected persons and all IDUs be tested for HCV [38–40]. However, the effectiveness of such guidelines and the associated practices varies markedly.
In the USA, rates of testing and awareness are lower. Some have estimated that 70% of all those with chronic hepatitis C in the USA are unaware of their infection. Data from The TREAT Asia (Therapeutic Research, Education and AIDS Training in Asia) HIV Observational Database, a collaborative observational cohort study involving 15 participating sites in 12 cities in the Asia and Pacific region, indicate that hepatitis testing data are available in nearly half of the TAHOD patients, with prevalence of HBV and HCV coinfection each at approximately 10% [41]. Lack of access to HCV testing and counseling is a major problem throughout eastern and central Europe and in Asia. The cost of the test is a major barrier.
Stigmatization of illicit drug use and HCV infection itself are obstacles to screening programmes. However, these issues have been addressed for HIV and can be overcome by a variety of measures that are likely to differ in various cultures.
Opting for HCV testing
The prevalence of HCV infection is sufficiently high to justify testing of any IDU and the stigma of acknowledging illicit drug use is sufficiently high that routing testing may be preferable to screening for specific HCV risk factors (and then testing those with risk). HCV testing should include counseling and, ideally, opportunities for disease management, which sometimes will involve treatment.
Given the small proportions of HCV-infected persons who are currently aware of their infections, greater effort also should be given to development and implementation of rapid HCV tests. For example, tests that can be used at any venue and provide results that can be interpreted at the same visit are highly desirable, as with HIV [42]. Counseling to reduce transmission to others and to reduce the harm of alcohol use is essential. Vaccination should be provided to susceptible persons to prevent hepatitis A virus and hepatitis B virus infections [39, 40].
Treatment is the most potent form of controlling chronic hepatitis C
HCV infection can be cured. Even in persons with HIV, suppression of replication during treatment and for six months after treatment (called a sustained virologic response, or SVR) is considered a cure because more than 98% will remain free of HCV viremia off medication for five or more years [43]. In addition, end-stage liver disease, liver cancer and other complications of HCV infection are reduced [44].
The global standard of care is peginterferon alfa and ribavirin, a combination that is expensive, toxic and effective approximately 50% of the time. Thus, guidelines currently recommend that treatment be used only for persons most likely to benefit (high disease stage, low risk of adverse events). However, treatment improvements are coming rapidly. "Highly active" HCV therapies are being developed, and approval of new compounds (often called direct acting agents, or DAAs) is expected in 2011. It is already clear that DAAs improve cure rates and will probably also reduce treatment durations [45]. In addition, clinical trials of interferon-free treatments are already in phase 2. Thus, it is reasonable to anticipate a day when 90% of HCV-infected persons could be cured by 24 weeks or less of treatment.
Even elimination of HCV is possible
There are many reasons why HCV could (and should) be eliminated. Humans are the only reservoir of HCV infection. Unlike HIV or HBV, there is no latent reservoir of HCV. When a patient is cured, they are no longer infectious to others. If environmental reservoir is reduced enough, infection will not be sustained. It is simply a matter of better drugs, which are anticipated, and then the allocation of resources to treat a sufficient number to break the transmission chain.
HCV outcome disparities
It is likely that existing inequities in HCV outcomes will expand markedly as therapies improve. Discrepancies already exist in the prevention and treatment of HCV infections worldwide. HCV transmission by transfusion has been eliminated from the USA and Europe, but continues in areas in the world in which donations are not screened effectively. HCV infection can be diagnosed, but fewer than 10% of the 170 million persons with HCV worldwide are aware of their infections. Even fewer have the opportunity for treatment.
In an interview with the United Nations Office on Drugs and Crime, Loon Gangte, President of the Dehli Network of Positive People, observed that the price of peginterferon and ribavirin exceeds the lifetime income of most Indians http://www.unodc.org/india/interview-with-mr.-loon-gangte.html.
Conclusions
In this way, HCV is much like HIV in the mid 1990s. HCV is about to enter an exciting era of more potent treatment that will reduce the mortality and morbidity associated with the infection. Treatments will continue to improve as newer generations of medications are developed. Like HIV, the benefits of treatment will be narrow unless there is a global response, such as what has occurred to bring antiretroviral therapy to millions of additional persons worldwide.
Will there be a Global Fund or PEPFAR for HCV? Even if all those who take HCV treatment are cured, if fewer than 10% receive care, the global impact of treatment remains minimal (Figure 5). The effectiveness of efficacious therapy will be low.
The disparity between potential HCV treatment efficacy and projected HCV treatment effectiveness. Adapted from Thomas DL [47].
On 21 May 2010, the World Health Assembly passed a resolution that called for the World Health Organization to observe World Hepatitis Day on July 28 and to develop a comprehensive approach to control of chronic hepatitis. This is an exciting first step. However, a tremendous amount of work still needs to be done to bring new HCV treatments to those who need them and, perhaps some day, to eradicate another global infectious disease.
References
Rockstroh JK, Mocroft A, Soriano V, Tural C, Losso MH, Horban A, Kirk O, Phillips A, Ledergerber B, Lundgren J: Influence of hepatitis C virus infection on HIV-1 disease progression and response to highly active antiretroviral therapy. J Infect Dis 2005, 192:992–1002.
Abdala N, Carney JM, Durante AJ, Klimov N, Ostrovski D, Somlai AM, Kozlov A, Heimer R: Estimating the prevalence of syringe-borne and sexually transmitted diseases among injection drug users in St Petersburg, Russia. Int J STD AIDS 2003, 14:697–703.
Thomas DL, Vlahov D, Solomon L, Cohn S, Taylor E, Garfein R, Nelson KE: Correlates of hepatitis C virus infections among injection drug users in Baltimore. Medicine 1995, 74:212–220.
Lincoln D, Petoumenos K, Dore GJ: HIV/HBV and HIV/HCV coinfection, and outcomes following highly active antiretroviral therapy. HIV Med 2003, 4:241–249.
Solomon SS, SriKrishnan AK, Mehta SH, Vasudevan CK, Murugavel KG, Thamburaj E, Anand S, Kumar MS, Latkin C, Solomon S, Celentano DD: High prevalence of HIV, HIV/hepatitis C virus coinfection, and risk behaviors among injection drug users in Chennai, India: a cause for concern. J Acquir Immune Defic Syndr 2008, 49:327–332.
Quan VM, Go VF, Nam LV, Bergenstrom A, Thuoc NP, Zenilman J, Latkin C, Celentano DD: Risks for HIV, HBV, and HCV infections among male injection drug users in northern Vietnam: a case-control study. AIDS Care 2009, 21:7–16.
Tan Y, Wei QH, Chen LJ, Chan PC, Lai WS, He ML, Kung HF, Lee SS: Molecular epidemiology of HCV monoinfection and HIV/HCV coinfection in injection drug users in Liuzhou, Southern China. PLoS ONE 2008, 3:e3608.
Garten RJ, Lai S, Zhang J, Liu W, Chen J, Vlahov D, Yu XF: Rapid transmission of hepatitis C virus among young injecting heroin users in Southern China. Int J Epidemiol 2004, 33:182–188.
McGovern BH, Wurcel A, Kim AY, Schulze zur WJ, Bica I, Zaman MT, Timm J, Walker BD, Lauer GM: Acute hepatitis C virus infection in incarcerated injection drug users. Clin Infect Dis 2006, 42:1663–1670.
Holsen DS, Harthug S, Myrmel H: Prevalence of antibodies to hepatitis C virus and association with intravenous drug abuse and tattooing in a national prison in Norway. Eur J Clin Microbiol Infect Dis 1993, 12:673–676.
Sulkowski MS, Thomas DL: Hepatitis C in the HIV-infected patient. Clin Liver Dis 2003, 7:179–194.
Danta M, Brown D, Bhagani S, Pybus OG, Sabin CA, Nelson M, Fisher M, Johnson AM, Dusheiko GM: Recent epidemic of acute hepatitis C virus in HIV-positive men who have sex with men linked to high-risk sexual behaviours. AIDS 2007, 21:983–991.
Fierer DS, Uriel AJ, Carriero DC, Klepper A, Dieterich DT, Mullen MP, Thung SN, Fiel MI, Branch AD: Liver fibrosis during an outbreak of acute hepatitis C virus infection in HIV-infected men: a prospective cohort study. J Infect Dis 2008, 198:683–686.
van de Laar T, Pybus O, Bruisten S, Brown D, Nelson M, Bhagani S, Vogel M, Baumgarten A, Chaix ML, Fisher M, Gotz H, Matthews GV, Neifer S, White P, Rawlinson W, Pol S, Rockstroh J, Coutinho R, Dore GJ, Dusheiko GM, Danta M: Evidence of a large, international network of HCV transmission in HIV-positive men who have sex with men. Gastroenterology 2009, 136:1609–1617.
Gerberding JL: Incidence and prevalence of human immunodeficiency virus, hepatitis B virus, hepatitis C virus, and cytomegalovirus among health care personnel at risk for blood exposure: Final report from a longitudinal study. J Infect Dis 1994, 170:1410–1417.
Goedert JJ, Chen BE, Preiss L, Aledort LM, Rosenberg PS: Reconstruction of the Hepatitis C Virus Epidemic in the US Hemophilia Population, 1940–1990. Am J Epidemiol 2007.
Ticehurst JR, Hamzeh FM, Thomas DL: Factors affecting serum concentrations of hepatitis C virus (HCV) RNA in HCV genotype 1-infected patients with chronic hepatitis. J Clin Microbiol 2007, 45:2426–2433.
Mellors JW, Rinaldo CRJ, Gupta P, White RM, Todd JA, Kingsley LA: Prognosis in HIV-1 infection predicted by the quantity of virus in plasma. Science 1996, 272:1167–1170.
Drucker E, Alcabes PG, Marx PA: The injection century: massive unsterile injections and the emergence of human pathogens. Lancet 2001, 358:1989–1992.
Magiorkinis G, Magiorkinis E, Paraskevis D, Ho SY, Shapiro B, Pybus OG, Allain JP, Hatzakis A: The global spread of hepatitis C virus 1a and 1b: a phylodynamic and phylogeographic analysis. PLoS Med 2009, 6:e1000198.
Frank C, Mohamed MK, Strickland GT, Lavanchy D, Arthur RR, Magder LS, El Khoby T, Abdel-Wahab Y, Aly Ohn ES, Anwar W, Sallam I: The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet 2000, 355:887–891.
Garfein RS, Doherty MC, Monterroso ER, Thomas DL, Nelson KE, Vlahov D: Prevalence and incidence of hepatitis C virus infection among young adult injection drug users. J Acquir Immune Defic Syndr Hum Retrovirol 1998,18(Suppl 1):S11-S19.
Quinn TC, Groseclose SL, Spence M, Provost V, Hook EW III: Evolution of the human immunodeficiency virus epidemic among patients attending sexually transmitted disease clinics: a decade of experience. J Infect Dis 1992, 165:541–544.
Kelen GD, Green GB, Purcell RH, Chan DW, Qaqish BF, Sivertson KT, Quinn TC: Hepatitis B and hepatitis C in emergency department patients. N Engl J Med 1992, 326:1399–1404.
Thomas DL, Astemborski J, Rai RM, Anania FA, Schaeffer M, Galai N, Nolt K, Nelson KE, Strathdee SA, Johnson L, Laeyendecker O, Boitnott J, Wilson LE, Vlahov D: The natural history of hepatitis C virus infection: host, viral, and environmental factors. JAMA 2000, 284:450–456.
Thomas DL, Astemborski J, Vlahov D, Strathdee SA, Ray SC, Nelson KE, Galai N, Nolt KR, Laeyendecker O, Todd JA: Determinants of the quantity of hepatitis C virus RNA. J Infect Dis 2000, 181:844–851.
Torriani FJ, Rodriguez-Torres M, Rockstroh JK, Lissen E, Gonzalez-Garcia J, Lazzarin A, Carosi G, Sasadeusz J, Katlama C, Montaner J, Sette H, Passe S, De Pamphilis J, Duff F, Schrenk UM, Dieterich DT: Peginterferon Alfa-2a plus ribavirin for chronic hepatitis C virus infection in HIV-infected patients. N Engl J Med 2004, 351:438–450.
Hadziyannis SJ, Sette H, Morgan TR, Balan V, Diago M, Marcellin P, Ramadori G, Bodenheimer H, Bernstein D, Rizzetto M, Zeuzem S, Pockros PJ, Lin A, Ackrill AM: Peginterferon-alpha2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann Intern Med 2004, 140:346–355.
Graham CS, Baden LR, Yu E, Mrus JM, Carnie J, Heeren T, Koziel MJ: Influence of human immunodeficiency virus infection on the course of hepatitis c virus infection: a meta-analysis. Clin Infect Dis 2001, 33:562–569.
Goedert JJ, Eyster ME, Lederman MM, Mandalaki T, De Moerloose P, White GC, Angiolillo AL, Luban NL, Sherman KE, Manco-Johnson M, Preiss L, Leissinger C, Kessler CM, Cohen AR, DiMichele D, Hilgartner MW, Aledort LM, Kroner BL, Rosenberg PS, Hatzakis A: End-stage liver disease in persons with hemophilia and transfusion- associated infections. Blood 2002, 100:1584–1589.
Chung RT, Evans SR, Yang Y, Theodore D, Valdez H, Clark R, Shikuma C, Nevin T, Sherman KE, AIDS Clinical Trials Groups 383 Study Team: Immune recovery is associated with persistent rise in hepatitis C virus RNA, infrequent liver test flares, and is not impaired by hepatitis C virus in co-infected subjects. AIDS 2002, 16:1915–1923.
Lohse N, Hansen AB, Pedersen G, Kronborg G, Gerstoft J, Sorensen HT, Vaeth M, Obel N: Survival of persons with and without HIV infection in Denmark, 1995–2005. Ann Intern Med 2007, 146:87–95.
Weber R, Sabin CA, Friis-Moller N, Reiss P, El Sadr WM, Kirk O, Dabis F, Law MG, Pradier C, De Wit S, Akerlund B, Calvo G, Monforte A, Rickenbach M, Ledergerber B, Phillips AN, Lundgren JD: Liver-related deaths in persons infected with the human immunodeficiency virus: the D:A:D study. Arch Intern Med 2006, 166:1632–1641.
Bica I, McGovern B, Dhar R, Stone D, McGowan K, Scheib R, Snydman DR: Increasing Mortality Due to End-Stage Liver Disease in Patients with Human Immunodeficiency Virus Infection. Clin Infect Dis 2001, 32:492–497.
Janke EA, McGraw S, Garcia-Tsao G, Fraenkel L: Psychosocial issues in hepatitis C: a qualitative analysis. Psychosomatics 2008, 49:494–501.
Marcellin F, Preau M, Ravaux I, Dellamonica P, Spire B, Carrieri MP: Self-reported fatigue and depressive symptoms as main indicators of the quality of life (QOL) of patients living with HIV and Hepatitis C: implications for clinical management and future research. HIV Clin Trials 2007, 8:320–327.
Mahoney FJ, Stewart K, Hu HX, Coleman P, Alter MJ: Progress toward the elimination of hepatitis B virus transmission among health care workers in the United States. Arch Intern Med 1997, 157:2601–2605.
Rockstroh JK, Bhagani S, Benhamou Y, Bruno R, Mauss S, Peters L, Puoti M, Soriano V, Tural C: Europeans AIDS Clinical Society (EACS) guidelines for the clinical management and treatment of chronic hepatitis B and C coinfection in HIV-infected adults. HIV Med 2008, 9:82–88.
Ghany MG, Strader DB, Thomas DL, Seeff LB: Diagnosis, management, and treatment of hepatitis C: An update. Hepatology 2009,49(4):1335–1374.
Centers for Disease Control and Prevention: Guidelines for Preventing Opportunistic Infections in HIV-Infected Adults and Adolescents - Recommendations from the CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR 2009, 58:1–206.
Zhou J, Dore GJ, Zhang F, Lim PL, Chen YM: Hepatitis B and C virus coinfection in The TREAT Asia HIV Observational Database. J Gastroenterol Hepatol 2007, 22:1510–1518.
Lee SR, Yearwood GD, Guillon GB, Kurtz LA, Fischl M, Friel T, Berne CA, Kardos KW: Evaluation of a rapid, point-of-care test device for the diagnosis of hepatitis C infection. J Clin Virol 2010, 48:15–17.
Soriano V, Maida I, Nunez M, Garcia-Samaniego J, Barreiro P, Martin-Carbonero L, Gonzalez-Lahoz J: Long-term follow-up of HIV-infected patients with chronic hepatitis C virus infection treated with interferon-based therapies. Antivir Ther 2004, 9:987–992.
Berenguer J, Alvarez-Pellicer J, Martin PM, Lopez-Aldeguer J, Von-Wichmann MA, Quereda C, Mallolas J, Sanz J, Tural C, Bellon JM, Gonzalez-Garcia J: Sustained virological response to interferon plus ribavirin reduces liver-related complications and mortality in patients coinfected with human immunodeficiency virus and hepatitis C virus. Hepatology 2009, 50:407–413.
McHutchison JG, Everson GT, Gordon SC, Jacobson IM, Sulkowski M, Kauffman R, McNair L, Alam J, Muir AJ: Telaprevir with peginterferon and ribavirin for chronic HCV genotype 1 infection. N Engl J Med 2009, 360:1827–1838.
Villano SA, Vlahov D, Nelson KE, Lyles CM, Cohn S, Thomas DL: Incidence and risk factors for hepatitis C among injection drug users in Baltimore, Maryland. J Clin Microbiol 1997, 35:3274–7.
Thomas DL: Curing hepatitis C with pills: a step toward global control. Lancet 2010, 376:1441–2.
Acknowledgements
We gratefully acknowledge grant R01016078 for supporting the project.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
DLT has served as a scientific advisor to Merck and has received from Gilead and Merck antiretroviral therapy to support research studies. The other authors have no competing interests to declare.
Authors' contributions
All authors contributed to the concept of the work and reviewed the paper. DLT chiefly wrote the paper. MSK and DT performed the research that contributed to the figures cited. All authors have read and approved the final manuscript.
Rights and permissions
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Thomas, D.L., Leoutsakas, D., Zabransky, T. et al. Hepatitis C in HIV-infected individuals: cure and control, right now. JIAS 14, 22 (2011). https://doi.org/10.1186/1758-2652-14-22
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1758-2652-14-22