Abstract
Ovarian cancer affects more than 200,000 women each year around the world. Most women are not diagnosed until the disease has already metastasized from the ovaries with a resultant poor prognosis. Ovarian cancer is associated with an overall 5 year survival of little more than 50%. The mainstay of front-line therapy is cytoreductive surgery followed by chemotherapy. Traditionally, this has been by the intravenous route only but there is more interest in the delivery of intraperitoneal chemotherapy utilizing the pharmaco-therapeutic advantage of the peritoneal barrier. Despite three large, randomized clinical trials comparing intravenous with intraperitoneal chemotherapy showing improved outcomes for those receiving at least part of their chemotherapy by the intraperitoneal route.
Cisplatin has been the most active drug for the treatment of ovarian cancer for the last 4 decades and the prognosis for women with ovarian cancer can be defined by the tumor response to cisplatin. Those whose tumors are innately platinum-resistant at the time of initial treatment have a very poor prognosis. Although the majority of patients with ovarian cancer respond to front-line platinum combination chemotherapy the majority will develop disease that becomes resistant to cisplatin and will ultimately succumb to the disease.
Improving the efficacy of cisplatin could have a major impact in the fight against this disease. Arsenite is an exciting agent that not only has inherent single-agent tumoricidal activity against ovarian cancer cell lines but also multiple biochemical interactions that may enhance the cytotoxicity of cisplatin including inhibition of deoxyribose nucleic acid (DNA) repair. In vitro studies suggest that arsenite may enhance the activity of cisplatin in other cell types. Arsenic trioxide is already used clinically to treat acute promyelocytic leukemia demonstrating its safety profile. Further research in ovarian cancer is warranted to define its possible role in this disease.
Similar content being viewed by others
Review
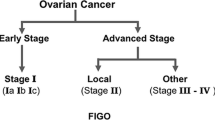
Epithelial ovarian cancer (EOC) affects approximately 204,000 women a year worldwide and is responsible for about 125,000 deaths [1]. The American Cancer Society estimates that in the USA alone the disease will be diagnosed in 21,650 women and cause the death of 15,520 women during 2008 [2]. It is often called the 'silent killer' because it causes few symptoms until it has metastasized within the peritoneal cavity at which time the chance of cure is markedly reduced. Although great strides have been made in the treatment of EOC, the enigma remains that a disease which is highly sensitive to chemotherapy compared to many other types of cancer is associated with an overall 5 year survival of just over 50% [3–6].
Cytoreductive Surgery
The management of advanced EOC has evolved over the last 30 years to become a combination of initial cytoreductive surgery (CRS) followed by chemotherapy. In 1968 Munnell reported an improved survival in patients who had maximal CRS compared to partial removal or biopsy only [7] and over the years, many retrospective reports have confirmed this finding [8–11]. Although no randomized studies have been performed the role of surgery was supported in a meta-analysis of 6885 patients undergoing CRS during the 'platinum era' where on an institutional basis for each 10% increase in the percentage of patients undergoing maximal CRS there was a 5.5% increase in median survival duration [12].
The reason CRS is thought to be effective when combined with chemotherapy is that it removes bulky disease containing poorly-oxygenated, non-proliferating cells which are either resistant to chemotherapy now, or potentially could become resistant, and leaves small volume tumors with a higher proportion of cells in the proliferative phase making them more susceptible to chemotherapy. At one time the concept of 'optimal' residual disease at completion of initial CRS for EOC was accepted as being any nodule < 2 cm in dimension [13] but it is now established that the most favorable prognosis is in patients with no macroscopic residual disease at all [14]. Unfortunately, 'no macroscopic disease' does not signify the complete absence of disease because so many patients in this situation at the end of surgery experience recurrence following front-line treatment. No less than 60% of patients who present with advanced disease and have a complete pathologic response to front-line therapy documented at second-look surgery will recur [15].
Chemotherapy
The most active chemotherapy agents in ovarian cancer are the platinum analogues, cisplatin and carboplatin. The antitumor activity of cisplatin (cis-diamminedichloroplatinum (II)) was discovered by Rosenberg and colleagues in 1961 [16]. Initial studies demonstrated that the whilst the agent had significant activity against several tumor types patients experienced severe renal and gastrointestinal toxicity [17]. Later it was shown that renal toxicity could be minimized by aggressive prehydration and diuresis [18, 19]. Cisplatin was introduced in the late 1970's and platinum-based combination chemotherapy became the most frequently used treatment for EOC. In a trial of single agent therapy, cisplatin was shown to be better than a previously favored agent cyclophosphamide [20]. Three major trials established cisplatin combination therapy as the standard regimen in advanced EOC [21]. A study randomizing patients with advanced EOC to cyclophosphamide with or without cisplatin reported better outcomes in the combination arm [22]. A Gynecologic Oncology Group study which included over 200 patients with advanced EOC reported that patients randomized to treatment with doxorubicin and cyclophosphamide with or without cisplatin had significantly better responses in the cisplatin containing arm [23]. A Dutch study reported a better outcome for a cisplatin containing regimen over combination hexamethylmelamine, cyclophosphamide, methotrexate, 5-fluorouracil (HexaCAF) [24]. The evidence was further supported in a meta-analysis of 45 trials including over 8000 patients with EOC treated with or without cisplatin. Survival was better with platinum alone and with platinum-containing combinations [25].
An additional class of drug, the taxanes, was discovered and came to play a role in the front-line armamentarium against EOC. In 1971 paclitaxel was identified as the active constituent of an extract of the bark of the Pacific yew tree, Taxus brevifolia [26, 27]. In early clinical trials on recurrent EOC paclitaxel was associated with an overall response rate of 36% [28]. It became established as the combination agent of choice with cisplatin after a Gynecologic Oncology Group study in women with advanced, suboptimally cytoreduced EOC showed a significantly better median overall survival in patients randomized to receive intravenous (IV) paclitaxel/cisplatin (37.5 months) in comparison with cyclophosphamide/cisplatin (24.4 months) [3]. Paclitaxel and subsequently its cousin, docetaxel were shown to have a unique mechanism of action binding to tubulin polymers (microtubules) and stabilizing the microtubule against depolymerization [29–32].
During this time analogues of cisplatin were investigated in an effort to maintain efficacy with reduced toxicity. Carboplatin was developed by substituting a cyclobutanedicarboxylate moiety for the two chloride ligands of cisplatin. Phase I and II trials of carboplatin showed that it was much less toxic than cisplatin especially with regard to neurotoxicity, nephrotoxicity and emetogenicity whilst retaining significant chemotherapeutic activity [33–37]. Many trials have been performed comparing cisplatin and carboplatin alone or in combination in patients with EOC and two meta-analyses found no difference in survival [25, 38]. A large, randomized trial comparing intravenous docetaxel with either cisplatin or carboplatin showed equivalency [39] and following initial front-line CRS, intravenous administration of cisplatin or carboplatin together with a taxane, either paclitaxel or docetaxel, has become the standard therapy for patients with EOC [3, 39].
Intraperitoneal Chemotherapy
For over twenty years there has been interest in the delivery of intraperitoneal therapy for ovarian cancer in order to maximize the efficacy and reduce the toxicity. Dedrick proposed that the intraperitoneal delivery of certain chemotherapeutic agents could lead to a significant increase in peritoneal cavity drug exposure compared to that in the systemic vascular compartment [40]. For drugs most active in EOC the ratio of their intraperitoneal to plasma concentrations varies from 18–20× for carboplatin and cisplatin to 120 – > 1000× for the taxanes, docetaxel and paclitaxel [41]. EOC should be a good target for intraperitoneal treatment because it is relatively chemo-sensitive and the cancer remains confined within the peritoneal cavity for much of its natural history. Three large randomized studies [42–44] have each shown improved responses for intraperitoneal (IP) delivery and a meta-analysis of all studies reported a clear benefit for patients receiving at least part of their front-line therapy by the IP route [45]. A recent study (Gynecologic Oncology Group protocol #172) examining experimental intravenous/intraperitoneal (IV/IP) chemotherapy for EOC showed a significant increase in overall survival in those receiving IP chemotherapy from 49 months to 66 months [44]. The National Cancer Institute has suggested that IP chemotherapy should be offered for patients' consideration for front-line treatment of ovarian cancer [46]. Despite large randomized trials indicating benefit, the use of intraperitoneal therapy in EOC is neither offered to the majority of eligible women nor accepted as standard of care by many oncologists
Despite the advances in the treatment of EOC much more effective therapy is necessary. This is exemplified by the results of Gynecologic Oncology Group protocol #172 where even in the IP/IV arm which led to median extension of survival of 16 months over patients treated only with IV therapy the recurrence rate was 65% within the period of the study. This recurrence rate is the current optimum situation in EOC.
One way of improving outcome for patients with EOC is to develop novel methods of enhancing the activity of cisplatin. Ovarian cancers that are resistant to platinum therapy are either innately resistant, shown by a lack of response to front-line therapy, or develop platinum resistance during the cancer's life history. In the patient this is demonstrated by an initial response to platinum agents followed by development of platinum resistance as the cancer progresses. Most of the women die with platinum resistant disease. Methods of preventing or overcoming resistance to cisplatin thus could be extremely beneficial.
Cisplatin Resistance
Cisplatin reacts preferentially with the N7 position guanine to form a variety of monofunctional and bifunctional adducts which result in intrastrand or interstrand cross-links, effectively preventing normal DNA function [17, 47]. Platinum resistance mechanisms fall into two main groups: A) those that limit the formation of cytotoxic platinum-DNA adducts and B) those that prevent cell death from occurring after platinum-DNA adduct formation. Group A includes decreased drug accumulation and increased drug inactivation by cellular protein and non-protein thiols whilst Group B includes increased platinum-DNA adduct repair and increased platinum-DNA damage tolerance [17].
Cisplatin accumulates within the cell by passive diffusion or facilitated transport [48] and the majority of cell lines that have been selected for cisplatin resistance in vitro show a decreased platinum accumulation phenotype most likely due to decreased uptake rather than enhanced drug efflux[17]. There are few experimental methods currently known to increase platinum uptake into cells but one method is to deliver it with mild hyperthermia. Hyperthermia has been shown to increase the cytotoxicity of cisplatin and other chemotherapeutic agents in both human cell culture and animal models [49–53]. Investigations of the cellular effects of the combination have demonstrated increased DNA cross-linking and increased DNA adduct formation [50, 54]. It has also been shown that cisplatin penetrates deeper into peritoneal tumor implants when delivered intraperitoneally with hyperthermia [54]. The mechanism of the effect of hyperthermia on cisplatin cytotoxicity and the role it might play in treatment awaits further investigation.
Multidrug resistance protein (MRP) is a member of a family of transport proteins that facilitates the extrusion of a variety of glutathione-coupled and unmodified drugs out of cells but over-expression of MRP alone does not confer resistance [55]. With regard to inactivation of platinum, the formation of conjugates between glutathione (GSH) and platinum drugs may be an important step for their inactivation and elimination from the cell [17]. There is a strong association between increased platinum drug sensitivity and lower GSH levels [56]. However, reducing GSH levels with drugs such as buthionine sulfoximine has resulted in only low to modest potentiation of cisplatin sensitivity [57]. It has been suggested that this may be due to the fact that formation of GSH-platinum conjugates is a slow process [58].
Inactivation may also occur by binding of the platinum drugs to metallothionein (MT) proteins. MTs are a family of sulfhydryl-rich, small molecular weight proteins that participate in heavy metal binding and detoxication. Modulation of MT levels can alter cisplatin sensitivity but the contribution of MT to clinical platinum drug resistance is unclear [17]. In some cell lines, elevated MT levels have been shown to be associated with cisplatin resistance, whereas in others, they have not [59, 60].
Once platinum-DNA adducts are formed, cells must either repair or tolerate the damage in order to survive. The capacity to repair DNA damage rapidly and efficiently plays a role in determining a tumor cell's sensitivity to platinum drugs [17]. Increased repair of platinum-DNA lesions in cisplatin-resistant cell lines has been compared with their sensitive counterparts in several human cancer cell lines, including ovarian cancer [61, 62]. Repair of platinum-DNA adducts occurs predominantly by nucleotide excision repair (NER) [17].
Inhibiting DNA repair activity to enhance platinum drug sensitivity has been an active area of investigation. Agents that have been used include nucleoside analogues, such as gemcitabine, fludarabine, and cytarabine; the riboncleotide reductase inhibitor hydroxyurea; and the inhibitor of DNA polymerases alpha and gamma, aphidocolin. All interfere with the repair synthesis stage of various repair processes, including nucleotide excision repair. The potentiation of cisplatin cytotoxicity by treatment with aphidicolin has been studied extensively in human OC cell lines with variable synergism [63–65]. The likelihood of a significant improvement in the therapeutic index of cisplatin in refractory patients by the coadministration of a repair inhibitor is limited by the multifactorial nature typical of resistant tumor cells.
Platinum-DNA damage tolerance is a phenotype that has been observed in both cisplatin-resistant cells derived from chemotherapy-refractory patients and cells selected for primary cisplatin resistance in vitro. This phenotype may result from alterations in a variety of cellular pathways. One component of DNA damage tolerance observed in platinum-resistant cells involves loss of function of the DNA mismatch repair (MMR) system. The main function of this is to scan newly synthesized DNA and to remove mismatches that result from nucleotide incorporation errors made by the DNA polymerases [17]. In addition to causing genomic instability, it has been reported that loss of MMR is associated with low-level platinum resistance.
Arsenic
Arsenic in its trivalent form is an interesting agent not only with inherent tumoricidal activity [66] but having multiple interactions that may enhance the cytotoxicity of cisplatin. In particular, arsenic may inhibit DNA repair [67], is clastogenic [68], induces stress response similar to heat shock [69], binds with glutathione and is exported by the multi-drug resistance protein MRP-1 [70], causes oxidative stress [71, 72] and can induce apoptosis [73–78]. One cellular defense mechanism against cisplatin is dependent on glutathione conjugation and export by (MRP-1) [79]. Since arsenite is exported from the cell by the MRP-1 as a glutathione conjugate [70] it may compete for MRP-1 and reduce the efficiency of cisplatin export resulting in increased intracellular concentrations of cisplatin and the formation of more DNA adducts. Additionally, arsenite induces a stress response with substantial overlap with the heat shock induced stress response [69] with many of the same proteins being induced, including several heat shock proteins, heme-oxygenase and metallothionein.
Arsenic has a long history of usage as a medicinal. In western medicine, arsenic was used to treat chronic myelogenous leukemia until radiation treatment became commonplace in the 1930's [80]. Interest in arsenic as a chemotherapeutic was renewed when Chinese physicians reported success in treating acute promyelocytic leukemia (APL) with arsenic trioxide ("Pishi") also called "white arsenic" or "arsenolite". Another form "Xionghuang" is called "red arsenic" or "realgar" and realgar-containing traditional medicines are used in cancer treatments such as "Awei Huapi Gao" [81]. Arsenic trioxide (Trisenox®, As2O3) is now an FDA (Federal Drug Administration) approved chemotherapeutic for treating all-trans retinoic acid (ATRA) resistant APL [82]. There is much interest in the potential use of Trisenox® to treat other malignancies (reviewed in [83, 84]).
In vitro studies of arsenic trioxide induced cytotoxicity in human ovarian cancer cells are promising. Clinically achievable concentrations (2 μM) induced apoptosis in the platinum-resistant human ovarian cancer cell line CI80-13S and the platinum-sensitive human ovarian cancer cell line OVCAR. They also appeared to slow the growth of the cisplatin-sensitive human ovarian cancer cells GG and JAM [85]. Arsenic trioxide and cisplatin had additive effects on human ovarian carcinoma MDAH2774 cells [86]. Growth was slowed but apoptosis was apparently not induced in human ovarian carcinoma SKOV3 cells treated with arsenic trioxide in culture [87]. Arsenic trioxide induced apoptosis in human ovarian cancer 3AO cells and in a cisplatin-resistant derivative cell line 3AO/CDDP was associated with a large increase in percentage of cells expressing Fas [88]. These authors also reported biphasic dose-dependent alterations in cell cycle with increases in S-phase compartment associated with decrease in G2/M compartment at low (< 1 μM) arsenic trioxide and in G1 compartment at high (> 3 μM) arsenic trioxide concentrations. Arsenic trioxide decreased peritoneal metastasis of human ovarian cancer cells (3AO, SW626, HO-8910PM) injected intraperitoneally into nude mice, most likely because arsenic trioxide inhibited matrix metalloproteinase MMP-2 and MMP-9 expression and induced TIMP expression [89]. Thus, arsenic trioxide shows some promise as a single agent in treating EOC.
Arsenic trioxide may be useful in combination therapy. Polyunsaturated fatty acids appear to sensitize arsenic resistant tumor cells, including SKOV3 cells, to arsenic trioxide induced cytotoxicity and apoptosis [90]. There are two reports examining combined exposure to arsenite and cisplatin. One study with hepatocellular carcinoma cells suggests that arsenite and cisplatin act synergistically [91]. Another study reported that arsenite exhibited additivity with cisplatin, Adriamycin and etoposide in an ovarian and two prostate cancer cell lines [86].
The preliminary studies of arsenic trioxide discussed above suggest that arsenic trioxide may be useful in therapy for EOC particularly in combination chemotherapy. Consistent with this hypothesis is that preliminary studies in our laboratories suggest that arsenic trioxide in combination with hyperthermia can overcome cisplatin resistance in A2780/CP70 cells (manuscript in preparation). Clearly, further study is warranted.
Conclusion
Despite modern standard therapy overall survival in women with ovarian cancer remains relatively poor. The most active chemotherapeutic agent remains cisplatin but ironically most patients whilst initially responding to cisplatin ultimately die with platinum-resistant disease. Arsenic is a promising agent for helping overcome platinum resistance. In addition to inherent tumoricidal activity it has multiple biochemical interactions that may enhance cisplatin cytotoxicity. Further research into this agent is needed.
About the author
-
C.
William Helm is Associate Professor in the Division of Gynecologic Oncology at the University of Louisville and the James Graham Brown Cancer Center. His research interests include both normothermic and hyperthermic intraperitoneal chemotherapy (HIPEC) for ovarian cancer.
-
J.
Christopher States is Professor of Pharmacology and Toxicology and Distinguished University Scholar at the University of Louisville. He is an established NIH investigator and recognized expert in disruption of mitosis by arsenicals.
References
Parkin DM, Bray F, Ferlay J, et al.: Global Cancer Statistics. CA Cancer J Clin 2005, 55: 74–108.
Society AC: Cancer Facts and Figures. 2008.
McGuire WP, Hoskins WJ, Brady MF, et al.: Cyclophosphamide and cisplatin versus paclitaxel and cisplatin: a phase III randomized trial in patients with suboptimal stage III/IV ovarian cancer (from the Gynecologic Oncology Group). Semin Oncol 1996, 23: 40–47.
Muggia FM, Braly PS, Brady MF, et al.: Phase III randomized study of cisplatin versus paclitaxel versus cisplatin and paclitaxel in patients with suboptimal stage III or IV ovarian cancer: a gynecologic oncology group study[see comment]. 2000, 18: 106–115.
Ozols RF, Bundy BN, Greer BE, et al.: Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study[see comment]. J Clin Oncol 2003, 21: 3194–3200. 10.1200/JCO.2003.02.153
Alberts DS, Green S, Hannigan EV, et al.: Improved therapeutic index of carboplatin plus cyclophosphamide versus cisplatin plus cyclophosphamide: final report by the Southwest Oncology Group of a phase III randomized trial in stages III and IV ovarian cancer[see comment]. [erratum appears in J Clin Oncol 1992 Sep, 10(9):1505]. J Clin Oncol 1992, 10: 706–717.
Munnell E: The changing prognosis and treatment in cancer of the ovary. Am J Obstet Gynecol 1968, 100: 790–795.
Griffiths CT: Surgical resection of tumor bulk in the primary treatment of ovarian carcinoma. Nat Cancer Inst Monog 1975, 42: 101–104.
Eisenkop SM, Friedman RL, Wang HJ: Complete cytoreductive surgery is feasible and maximizes survival in patients with advanced epithelial ovarian cancer: a prospective study. Gynecol Oncol 1998, 69: 103–108. 10.1006/gyno.1998.4955
Hoskins WJ, Bundy BN, Thigpen JT, et al.: The influence of cytoreductive surgery on recurrence-free interval and survival in small-volume stage III epithelial ovarian cancer: a Gynecologic Oncology Group study. Gynecol Oncol 1992, 47: 159–166. 10.1016/0090-8258(92)90100-W
Guidozzi F, Ball JH: Extensive primary cytoreductive surgery for advanced epithelial ovarian cancer. Gynecol Oncol 1994, 53: 326–330. 10.1006/gyno.1994.1142
Bristow RE, Tomacruz RS, Armstrong DK, et al.: Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol 2002, 20: 1248–1259. 10.1200/JCO.20.5.1248
Hoskins WJ, McGuire WP, Brady MF, et al.: The effect of diameter of largest residual disease on survival after primary cytoreductive surgery in patients with suboptimal residual epithelial ovarian carcinoma. Am J Obstet Gynecol 1994, 170: 974–979.
Eisenkop SM, Spirtos NM: What are the current surgical objectives, strategies, and technical capabilities of gynecologic oncologists treating advanced epithelial ovarian cancer? Gynecol Oncol 2001, 82: 489–497. 10.1006/gyno.2001.6312
Rubin SC, Randall TC, Armstrong KA, et al.: Ten-year follow-up of ovarian cancer patients after second-look laparotomy with negative findings. Obstet Gynecol 1999, 93: 21–24. 10.1016/S0029-7844(98)00334-2
Rosenberg B, VanCamp L, Trosko JE, et al.: Platinum compounds: a new class of potent antitumour agents. Nature 1969, 222: 385–386. 10.1038/222385a0
Johnson SW, Stevenson JP, O'Dwyer PJ, DeVita VT, Hellman S, Rosenberg SA: Cisplatin and Its Analogues. 6th edition. Philadelphia:Lippincott Williams and Wilkins; 2001:376–388.
Cvitkovic E, Spaulding J, Bethune V, et al.: Improvement of cis-dichlorodiammineplatinum (NSC 119875): therapeutic index in an animal model. Cancer 1977, 39: 1357–1361. Publisher Full Text 10.1002/1097-0142(197704)39:4<1357::AID-CNCR2820390402>3.0.CO;2-C
Hayes DM, Cvitkovic E, Golbey RB, et al.: High dose cis-platinum diammine dichloride: amelioration of renal toxicity by mannitol diuresis. Cancer 1977, 39: 1372–1381. Publisher Full Text 10.1002/1097-0142(197704)39:4<1372::AID-CNCR2820390404>3.0.CO;2-J
Lambert HE, Berry RJ: High dose cisplatin compared with high dose cyclophosphamide in the management of advanced epithelial ovarian cancer (FIGO stages III and IV): report from the North Thames Cooperative Group. Br Med J (Clin Res Ed) 1985, 290: 889–893.
Ozols RF, Rubin SC, Thomas GM, Hoskins WJ, Perez CA, Young RC, et al.: Epithelial Ovarian Cancer. Philadelphia:Lippincott Williams and Wilkins; 2000:981–1057.
Decker DG, Fleming TR, Malkasian GD Jr, et al.: Cyclophosphamide plus cis-platinum in combination: treatment program for stage III or IV ovarian carcinoma. Obstet Gynecol 1982, 60: 481–487.
Omura G, Blessing JA, Ehrlich CE, et al.: A randomized trial of cyclophosphamide and doxorubicin with or without cisplatin in advanced ovarian carcinoma. A Gynecologic Oncology Group Study. Cancer 1986, 57: 1725–1730. Publisher Full Text 10.1002/1097-0142(19860501)57:9<1725::AID-CNCR2820570903>3.0.CO;2-J
Neijt JP, ten Bokkel Huinink WW, Burg ME, et al.: Randomized trial comparing two combination chemotherapy regimens (Hexa-CAF vs CHAP-5) in advanced ovarian carcinoma. Lancet 1984, 2: 594–600. 10.1016/S0140-6736(84)90594-4
Group AOCT: Chemotherapy in advanced ovarian cancer: an overview of randomized clinical trials. 1991, 303: 884–893.
Rowinsky EK, Cazenave LA, Donehower RC: Taxol: a novel investigational antimicrotubule agent. J Natl Cancer Inst 1990, 82: 1247–1259. 10.1093/jnci/82.15.1247
Rowinsky EK, Donehower RC: Paclitaxel (taxol). 1995, 332: 1001–1014.
McGuire WP, Rowinsky EK, Rosenshein NB, et al.: Taxol: a unique antineoplastic agent with significant activity in advanced ovarian epithelial neoplasms. 1989, 111: 273–279.
Schiff PB, Fant J, Horwitz SB: Promotion of microtubule assembly in vitro by taxol. Nature 1979, 277: 665–667. 10.1038/277665a0
Schiff PB, Horwitz SB: Taxol stabilizes microtubules in mouse fibroblast cells. Proc Natl Acad Sci USA 1980, 77: 1561–1565. 10.1073/pnas.77.3.1561
Manfredi JJ, Parness J, Horwitz SB: Taxol binds to cellular microtubules. J Cell Biol 1982, 94: 688–696. 10.1083/jcb.94.3.688
Ringel I, Horwitz SB: Studies with RP 56976 (taxotere): a semisynthetic analogue of taxol. J Natl Cancer Inst 1991, 83: 288–291. 10.1093/jnci/83.4.288
Calvert AH, Harland SJ: Early studies with cisdiamine 1, 1, cyclobutane dicarboxylate platinum II. 1982, 9: 140.
Curt GA, Grygiel JJ, Corden BJ, et al.: A phase I and pharmacokinetic study of diamminecyclobutane-dicarboxylatoplatinum (NSC 241240). Cancer Res 1983, 43: 4470–4473.
Evans BD, Raju KS, Calvert AH, et al.: Phase II study of JM8, a new platinum analog, in advanced ovarian carcinoma. Cancer Treat Rep 1983, 67: 997–1000.
Harrap KR: Preclinical studies identifying carboplatin as a viable cisplatin alternative. Cancer Treat Rev 1985,12(Suppl A):21–33. 10.1016/0305-7372(85)90015-5
Canetta R, Bragman K, Smaldone L: Carboplatin: current status and future prospects. 1988, 15: 17.
Aabo K, Adams M, Adnitt P, et al.: Chemotherapy in advanced ovarian cancer: four systematic meta-analyses of individual patient data from 37 randomized trials. Advanced Ovarian Cancer Trialists' Group. Br J Cancer 1998, 78: 1479–1487.
Vasey PA, Jayson GC, Gordon A, et al.: Phase III randomized trial of docetaxel-carboplatin versus paclitaxel-carboplatin as first-line chemotherapy for ovarian carcinoma. 2004, 96: 1682–1691.
Dedrick RI, Myers CE, Bungay PM, et al.: Pharmacokinetic rationale for peritoneal drug administration in the treatment of ovarian cancer. Canc Treat Rep 1978, 62: 1–11.
Markman M: Intraperitoneal chemotherapy in the management of malignant disease. Exp Rev Anticanc Ther 2001, 1: 142–148. 10.1586/14737140.1.1.142
Alberts DS, Liu PY, Hannigan EV, et al.: Intraperitoneal cisplatin plus intravenous cyclophosphamide versus intravenous cisplatin plus intravenous cyclophosphamide for stage III ovarian cancer[see comment]. N Engl J Med 1996, 335: 1950–1955. 10.1056/NEJM199612263352603
Markman M, Bundy BN, Alberts DS, et al.: Phase III trial of standard-dose intravenous cisplatin plus paclitaxel versus moderately high-dose carboplatin followed by intravenous paclitaxel and intraperitoneal cisplatin in small-volume stage III ovarian carcinoma: an intergroup study of the Gynecologic Oncology Group, Southwestern Oncology Group, and Eastern Cooperative Oncology Group[see comment]. J Clin Oncol 2001, 19: 1001–1007.
Armstrong DK, Bundy BN, Wenzel L, et al.: Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med 2006, 354: 34–43. 10.1056/NEJMoa052985
Jaaback K, Johnson N: Intraperitoneal chemotherapy for the initial management of primary epithelial ovarian cancer. Cochrane Database Systemat Rev 2006,25(1):CD005340.
NCI Clinical Announcement For Preferred Method of Treatment for Advanced Ovarian Cancer 2006. [http://ctep.cancer.gov/resources/gcig/icaoa.html]
Eastman A: The formation, isolation and characterization of DNA adducts produced by anticancer platinum complexes. Pharmacol Ther 1987, 34: 155–166. 10.1016/0163-7258(87)90009-X
Gately DP, Howell SB: Cellular accumulation of the anticancer agent cisplatin: a review. Br J Cancer 1993, 67: 1171–1176.
Hahn GM: Potential for therapy of drugs and hyperthermia. Canc Res 1979, 39: 2264–2268.
Meyn RE, Corry PM, Fletcher SE, et al.: Thermal enhancement of DNA damage in mammalian cells treated with cis-diamminedichloroplatinum(II). Cancer Res 1980, 40: 1136–1139.
Alberts DS, Peng YM, Chen HS, et al.: Therapeutic synergism of hyperthermia-cis-platinum in a mouse tumor model. J Nat Cancer Inst 1980, 65: 455–461.
Los G, van Vugt MJ, Pinedo HM: Response of peritoneal solid tumours after intraperitoneal chemohyperthermia treatment with cisplatin or carboplatin. Brit J Cancer 1994, 69: 235–241.
Akaboshi M, Tanaka Y, Kawai K, et al.: Effect of hyperthermia on the number of platinum atoms binding to DNA of HeLa cells treated with 195mPt-radiolabelled cis-diaminedichloroplatinum(II). Int J Radiat Biol 1994, 66: 215–220. 10.1080/09553009414551121
Vaart PJ, Vange N, Zoetmulder FA, et al.: Intraperitoneal cisplatin with regional hyperthermia in advanced ovarian cancer: pharmacokinetics and cisplatin-DNA adduct formation in patients and ovarian cancer cell lines. Eur J Cancer 1998, 34: 148–154. 10.1016/S0959-8049(97)00370-5
Borst P, Kool M, Evers R: Do cMOAT (MRP2), other MRP homologues, and LRP play a role in MDR? Semin Cancer Biol 1997, 8: 205–213. 10.1006/scbi.1997.0071
Godwin AK, Meister A, O'Dwyer PJ, et al.: High resistance to cisplatin in human ovarian cancer cell lines is associated with marked increase of glutathione synthesis. Proc Natl Acad Sci USA 1992, 89: 3070–3074. 10.1073/pnas.89.7.3070
Hamilton T, Winker M, Louie K, et al.: Augmantation of Adriamycin, melphalan and cisplatin cytotoxicity in drug-resistant and -sensitive human ovarian cancer cell lines by buthionine sulfoximine dediated glutathione depletion. 1985, 34: 2583–2586.
Dedon P, Borch RE: Characterization of the reactions of platinum antitumor agents with biologic and nonbiologic sulfur-containing nucleophiles. 1987, 36: 1955–1964.
Hosking LK, Whelan RD, Shellard SA, et al.: An evaluation of the role of glutathione and its associated enzymes in the expression of differential sensitivities to antitumour agents shown by a range of human tumour cell lines. Biochem Pharmacol 1990, 40: 1833–1842. 10.1016/0006-2952(90)90364-Q
Kojima M, Kikkawa F, Oguchi H, et al.: Sensitisation of human ovarian carcinoma cells to cis-diamminedichloroplatinum (II) by amphotericin B in vitro and in vivo. Eur J Cancer 1994, 30A: 773–778. 10.1016/0959-8049(94)90291-7
Johnson SW, Perez RP, Godwin AK, et al.: Role of platinum-DNA adduct formation and removal in cisplatin resistance in human ovarian cancer cell lines. 1994, 47: 689–697.
Johnson SW, Swiggard PA, Handel LM, et al.: Relationship between platinum-DNA adduct formation and removal and cisplatin cytotoxicity in cisplatin-sensitive and -resistant human ovarian cancer cells. 1994, 54: 5911–5916.
Masuda H, Tanaka T, Matsuda H, et al.: Increased removal of DNA-bound platinum in a human ovarian cancer cell line resistant to cis-diamminedichloroplatinum(II). Cancer Res 1990, 50: 1863–1866.
Katz EJ, Andrews PA, Howell SB: The effect of DNA polymerase inhibitors on the cytotoxicity of cisplatin in human ovarian carcinoma cells. 1990, 2: 159–164.
Dempke WC, Shellard SA, Fichtinger-Schepman AM, et al.: Lack of significant modulation of the formation and removal of platinum-DNA adducts by aphidicolin glycinate in two logarithmically-growing ovarian tumour cell lines in vitro. Carcinogenesis 1991, 12: 525–528. 10.1093/carcin/12.3.525
Miller WH Jr, Schipper HM, Lee JS, et al.: Mechanisms of action of arsenic trioxide. 2002, 62: 3893–3903.
Hartwig A, Groblinghoff UD, Beyersmann D, et al.: Interaction of arsenic(III) with nucleotide excision repair in UV-irradiated human fibroblasts. 1997, 18: 399–405.
Lee TC, Tanaka N, Lamb PW, et al.: Induction of gene amplification by arsenic. 1988, 241: 79–81.
Del Razo LM, Quintanilla-Vega B, Brambila-Colombres E, et al.: Stress proteins induced by arsenic. 2001, 177: 132–148.
Leslie EM, Haimeur A, Waalkes MP: Arsenic transport by the human multidrug resistance protein 1 (MRP1/ABCC1). Evidence that a tri-glutathione conjugate is required. 2004, 279: 32700–32708.
Shi H, Hudson LG, Ding W, et al.: Arsenite causes DNA damage in keratinocytes via generation of hydroxyl radicals. 2004, 17: 871–878.
Shi H, Hudson LG, Liu KJ: Oxidative stress and apoptosis in metal ion-induced carcinogenesis. 2004, 37: 582–593.
Ramos AM, Fernandez C, Amran D, et al.: Pharmacologic inhibitors of PI3K/Akt potentiate the apoptotic action of the antileukemic drug arsenic trioxide via glutathione depletion and increased peroxide accumulation in myeloid leukemia cells. 2005, 105: 4013–4020.
Hu J, Fang J, Dong Y, et al.: Arsenic in cancer therapy. 2005, 16: 119–127.
Taylor BF, McNeely SC, Miller HL, et al.: p53 suppression of arsenite-induced mitotic catastrophe is mediated by p21CIP1/WAF1. 2006, 318: 142–151.
McCollum G, Keng PC, States JC, et al.: Arsenite delays progression through each cell cycle phase and induces apoptosis following G2/M arrest in U937 myeloid leukemia cells. 2005, 131: 877–887.
States JC, Reiners JJ Jr, Pounds JG, et al.: Arsenite disrupts mitosis and induces apoptosis in SV40-transformed human skin fibroblasts. [erratum appears in Toxicol Appl Pharmacol 2002 Sep 1, 183(2):152]. 2002, 180: 83–91.
McCabe MJ Jr, Singh KP, Reddy SA, et al.: Sensitivity of myelomonocytic leukemia cells to arsenite-induced cell cycle disruption, apoptosis, and enhanced differentiation is dependent on the inter-relationship between arsenic concentration, duration of treatment, and cell cycle phase. 2000, 295: 724–733.
Cole SP, Sparks KE, Fraser K, et al.: Pharmacological characterization of multidrug resistant MRP-transfected human tumor cells. 1994, 54: 5902–5910.
Waxman S, Anderson KC: History of the development of arsenic derivatives in cancer therapy. 2001, 2: 3–10.
Liu J, Lu Y, Wu Q, et al.: Mineral arsenicals in traditional medicines: orpiment, realgar, and arsenolite. J Pharmacol Exp Ther 2008, 326: 363–368. 10.1124/jpet.108.139543
Cohen MH, Hirschfeld S, Flamm Honig S, et al.: Drug approval summaries: arsenic trioxide, tamoxifen citrate, anastrazole, paclitaxel, bexarotene. 2001, 6: 4–11.
Murgo AJ, McBee WL, Cheson BD: Clinical trials referral resource. Clinical trials with arsenic trioxide. 2000, 14: 206. 211, 215–216
Murgo AJ: Clinical trials of arsenic trioxide in hematologic and solid tumors: overview of the National Cancer Institute Cooperative Research and Development Studies. 2001, 2: 22–28.
Du YH, Ho PC, Du YH, et al.: Arsenic compounds induce cytotoxicity and apoptosis in cisplatin-sensitive and -resistant gynecological cancer cell lines. Cancer Chemother Pharmacol 2001, 47: 481–490. 10.1007/s002800100278
Uslu R, Sanli UA, Sezgin C, et al.: Arsenic trioxide-mediated cytotoxicity and apoptosis in prostate and ovarian carcinoma cell lines. 2000, 6: 4957–4964.
Bornstein J, Sagi S, Haj A, et al.: Arsenic Trioxide inhibits the growth of human ovarian carcinoma cell line. Gynecol Oncol 2005, 99: 726–729. 10.1016/j.ygyno.2005.07.125
Kong B, Huang S, Wang W, et al.: Arsenic trioxide induces apoptosis in cisplatin-sensitive and -resistant ovarian cancer cell lines. Int J Gynecol Cancer 2005, 15: 872–877. 10.1111/j.1525-1438.2005.00251.x
Zhang J, Wang B: Arsenic trioxide (As(2)O(3)) inhibits peritoneal invasion of ovarian carcinoma cells in vitro and in vivo. Gynecol Oncol 2006, 103: 199–206. 10.1016/j.ygyno.2006.02.037
Baumgartner M, Sturlan S, Roth E, et al.: Enhancement of arsenic trioxide-mediated apoptosis using docosahexaenoic acid in arsenic trioxide-resistant solid tumor cells. Int J Cancer 2004, 112: 707–712. 10.1002/ijc.20462
Wang W, Qin SK, Chen BA, et al.: Experimental study on antitumor effect of arsenic trioxide in combination with cisplatin or doxorubicin on hepatocellular carcinoma. 2001, 7: 702–705.
Acknowledgements
Ms. Cathy Buckley for her help with the type-setting and proofing of this manuscript. Supported in part by USPHS grants ES011314 and ES014443.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
Both authors conceived the idea and jointly wrote the manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Helm, C., States, J. Enhancing the efficacy of cisplatin in ovarian cancer treatment – could arsenic have a role. J Ovarian Res 2, 2 (2009). https://doi.org/10.1186/1757-2215-2-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1757-2215-2-2