Abstract
Background
Tuberous sclerosis complex (TSC) is an autosomal dominant disorder. It is characterized by seizures, mental retardation and hamartomatous lesions, including facial angiofibroma, subependymal giant cell astrocytoma, cardiac rhabdomyoma and renal angiomyolipoma (AML). AMLs can bleed severely in the retroperitoneal space.
Case presentation
Herein, we present the case of a TSC patient presenting with recurrent severe episodes of retroperitoneal hemorrhage from AMLs successfully managed by angio-embolization.
Conclusion
Transarterial embolization is effective in preventing and controlling hemorrhage in patients with AMLs of the kidney
Similar content being viewed by others
Background
Tuberous sclerosis complex (TSC) or Bourneville's disease is a rare genetic disorder, either sporadic or inherited by an autosomal dominant transmission. Mutations in one of two genes, TSC1 and TSC2, have been identified as causes of TSC. Affected patients develop hamartomatous lesions in different organs, most commonly in the brain, eyes, heart, kidney, skin and lungs. Angiomyolipomas (AML) of the kidney are the most common TSC lesion, occurring in 70 to 80% of adults and older children.[1] These lesions can be a bleeding source.
Case presentation
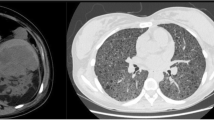
In September 2000, a 48 year-old Caucasian male with sporadic tuberous sclerosis presented to the emergency room with acute right flank pain, large abdominal mass, signs and symptoms of internal bleeding (hypotension, tachycardia and acute anemia). Abdominal CT scan showed bilateral renal giant angiomyolipomatosis with a honey-comb aspect of the kidneys and a right retroperitoneal haematoma. Moreover, an arterial contrast blush was seen within the right retroperitoneal hemorrhagic infarction (Figure 1). The patient underwent angiography (Figure 2), which showed the right kidney to be supplied by two main arteries and the presence of multiple intraparenchymal aneurysms (arrows) in the territory of the lower artery. There was no active bleeding but due to the size of AML and of the aneurysms a selective embolization with metal coils was carried out. Adjunctive features of the syndrome in this patient included sebaceous adenoma of the face (Figure 3), and sub-ependymal calcifications (Figure 4). The course was uneventful and kidney function was maintained. A further episode of massive retroperitoneal bleeding occurred 40 months later. The bleeding source was from a AML lesion of the upper pole of the left kidney (Figure 5). Control was achieved by selective angio-embolization. Since then, there has been no recurrence of retroperitoneal bleeding, but the patient has developed a mild renal failure.
Discussion
The three major renal manifestations of TSC include AML and less frequently polycystic kidney disease (PKD) and renal cell carcinoma (RCC), arising alone or in combination. Of these, however, only AML are a major criterion for TSC diagnosis because neither the presence of cysts nor RCC is sufficiently specific for TSC. Angiomyolipomas are benign tumors composed of abnormal vessels, immature smooth muscle cells and fat cells. Their incidence in the general population is 1–2%, whereas in patients with TSC the incidence of AML has been estimated at 50–80%. In respect to sporadic AML, patients with TSC significantly have multiple and bilateral AML that tend to grow with time. As AML grow, aneurysms develop inside the mass. Bleeding from ruptured aneurysm increases in frequency when tumors become larger than 4 cm. Giant renal AML in Bourneville's syndrome raise a surgical interest because they are a source of life-threatening hemorrhage. Hemorrhage from AML has been reported among the most common causes of death in patients with TSC.[2] Management of AML greater than 4 cm electively identified by imaging series should be balanced between the need to prevent life-threatening bleeding and the issue of preserve as much functional renal parenchyma as possible. For this purpose a variety of methods have been proposed. These include selective renal angiography and embolization, AML ablation by cryotherapy or radiofrequency and partial nephrectomy.[2, 3] In the presence of ongoing bleeding, selective renal embolization is a safe and effective method to achieve hemorrhage control and to reduce the size of AML. This treatment is minimally invasive and preserves renal function. Currently, embolization is proposed as the first choice of intervention for symptomatic AMLs or to prevent hemorrhage when AMLs exceed 4 cm in diameter.[4, 5] Patients with TSC have however a 40% recurrence rate of symptomatic AMLs with a median time interval from embolization to recurrence of approximately 79 months.[6] As genes mutations in TSC result in activation of the mammalian target of rapamycin (mTOR), therapy with sirolimus, a suppressor of the mTOR signaling, has been recently implemented in order to reduce the size of AML and to prevent retroperitoneal bleeding.[7] As result of the treatment, AMLs regressed during the therapy but increased again once the therapy was stopped. Some severe adverse events from sirolimus also were reported. Thus, so far, the role of mTOR suppressors in preventing hemorrhage from AML seems to be very promising, but yet, it cannot be considered as standard of care. Most of TSC patients presenting with recurrence and of re-bleeding may be first safety and effectively managed by redo angio-embolization. However some patients with repetitive renal bleeding will eventually require a nephrectomy. For these cases combined nephrectomy and pre-emptive renal transplantation may be the procedure of choice, as it removes the risk of severe bleeding and represents definitive treatment.[8]
Conclusion
Transarterial embolization is effective in preventing and controlling hemorrhage in patients with AMLs of the kidney. When AMLs are associated to TSC, recurrence of bleeding is not uncommon and redo angio-embolization may be required.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Lendvay TS, Marshall FF: The tuberous sclerosis complex and its highly variable manifestations. J Urol. 2003, 169: 1635-42. 10.1097/01.ju.0000058253.40352.60.
Williams JM, Racadio JM, Johnson ND, Donnelly LF, Bissler JJ: Embolization of renal angimyolipomata in patients with tuberous sclerosis complex. Am J Kidney Dis. 2006, 47: 95-102. 10.1053/j.ajkd.2005.09.028.
Harabayashi T, Shinohara N, Katano H, Nonomura K, Shimizu T, Koyanagi T: Management of angiomyolipomas associated with tuberous sclerosis complex. J Urol. 2004, 171: 102-5. 10.1097/01.ju.0000100100.36354.61.
Hadley DA, Bryant LJ, Ruckle HC: Conservative treatment of renal angiomyolipomas in patients with tuberous sclerosis. Clin Nephrol. 2006, 65: 22-7.
Seyam RM, Bissada NK, Kattan SA, Mokhtar AA, Aslam M, Fahmy WE, Mourad WA, Binmahfouz AA, Alzahrani HM, Hanash KA: Changing trends in presentation, diagnosis and management of renal angiomyolipoma: comparison of sporadic and tuberous sclerosis complex-associated forms. Urology. 2008, 72: 1077-1082. 10.1016/j.urology.2008.07.049.
Kothary N, Soulen MC, Clark TW, Wein AJ, Slanky-Goldberg RD, Crino PB, Stavropoulos SW: Renal angiomyolipoma: long-term results after arterial embolization. J Vasc Interv Radiol. 2005, 16: 45-50.
Corsenca A, Aebersold F, Moch H, Bird P, Weber M, Hofbauer G, Wüthrich RP, Serra AL: Combined nephrectomy and pre-emptive renal transplantation in a tuberous sclerosis patient with angiomyolipoma, renal carcinoma and life-threatening abdominal haemorrhages. Nephrol Dial Transplant. 2007, 22: 3330-3. 10.1093/ndt/gfm552.
Bissler JJ, McCormack FX, Young LR, Elwing JM, Chuck G, Leonard JM, Schmithorst VJ, Laor T, Brody AS, Bean J, Salisbury S, Franz DN: Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis. N Engl J Med. 2008, 358: 140-51. 10.1056/NEJMoa063564.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MC and LD carried out the literature research and drafted the manuscript. MP and MC were major contributor to the writing of this case. CV retrieved and processed the images. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chiarugi, M., Martino, M.C., Pucciarelli, M. et al. Recurrent retroperitoneal hemorrhage in a patient with tuberous sclerosis complex: a case report. Cases Journal 1, 424 (2008). https://doi.org/10.1186/1757-1626-1-424
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1757-1626-1-424