Abstract
Background
Fenton reaction (Fe2++H2O2→Fe3++•OH+OH−) is of special significance in the thyroid gland, as both its substrates, i.e. H2O2 and Fe2+, are required for thyroid hormone synthesis. Also iodine, an essential element supplied by the diet, is indispensable for thyroid hormone synthesis. It is well known that iodine affects red-ox balance. One of the most frequently examined oxidative processes is lipid peroxidation (LPO), which results from oxidative damage to membrane lipids. Fenton reaction is used to experimentally induce lipid peroxidation. The aim of the study was to evaluate effects of iodine, used as potassium iodide (KI) or potassium iodate (KIO3), on lipid peroxidation in porcine thyroid homogenates under basal conditions and in the presence of Fenton reaction substrates.
Methods
Porcine thyroid homogenates were incubated in the presence of either KI (0.00005 – 500 mM) or KIO3 (0.00005 – 200 mM), without or with addition of FeSO4 (30 μM) + H2O2 (0.5 mM). Concentration of malondialdehyde + 4-hydroxyalkenals (MDA + 4-HDA) was measured spectrophotometrically, as an index of lipid peroxidation.
Results
Potassium iodide, only when used in the highest concentrations (≥50 mM), increased lipid peroxidation in concentration-dependent manner. In the middle range of concentrations (5.0; 10; 25; 50 and 100 mM) KI reduced Fenton reaction-induced lipid peroxidation, with the strongest protective effect observed for the concentration of 25 mM. Potassium iodate increased lipid peroxidation in concentrations ≥2.5 mM. The damaging effect of KIO3 increased gradually from the concentration of 2.5 mM to 10 mM. The strongest damaging effect was observed at the KIO3 concentration of 10 mM, corresponding to physiological iodine concentration in the thyroid. Potassium iodate in concentrations of 5–200 mM enhanced Fenton reaction-induced lipid peroxidation with the strongest damaging effect found again for the concentration of 10 mM.
Conclusions
Potassium iodide, used in doses generally recommended in iodide prophylaxis, may prevent oxidative damage to membrane lipids in this gland. Toxic effects of iodide overload may result from its prooxidative action. Potassium iodate does not possess any direct beneficial effects on oxidative damage to membrane lipids in the thyroid, which constitutes an additional argument against its utility in iodine prophylaxis.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
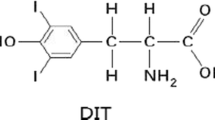
Iodine, an essential trace element, is indispensable for thyroid hormone synthesis in humans and animals [1]. The only natural source of iodine is the diet. However, in numerous areas in the world iodine supply from natural sources is inadequate, resulting in iodine deficiency disorders (IDD) [2, 3]. Precisely elaborated programs of iodine prophylaxis were introduced in different countries to prevent IDD [4]. These programs are mainly based on salt iodization with the use of either potassium iodide (KI) or potassium iodate (KIO3).
These two compounds are characterised by different chemical properties and some differencies in potential toxicity/safety. Iodate is more stable, as iodide is readily oxidized to iodine and lost by evaporation [5]. Whereas reliable methods are validated for quantifying KIO3 salt content, further validation is required for countries that use KI in salt iodization programs [6]. All other differences between KIO3 and KI suggest the superiority of the latter over the former. First, human iodine bioavailability from KI is higher than from KIO3 [7, 8]. Second, in biofortification of vegetables with iodine, KI was found to be much more effective than KIO3 [9, 10].
In turn, according to some health authorities, the safety of KIO3 to humans and animals is not completely documented and in 2002 the French Agency for Food Safety [11] did even question the use of KIO3 instead of KI in iodine prophylaxis. Therefore, several experimental studies have been performed to clarify this issue. For example, it has been shown in experimental studies that KIO3 does not reveal genotoxic effects [12]. Also comparative studies of the oxidative properties of iodate and other halogenate salts, such as bromate and chlorate, have shown that iodate would be of low, if any, genotoxic potential [13]. It is worth mentioning that both, KI and KIO3, reveal similar effectiveness as blockers of radioiodine uptake by the thyroid in rats [14].
Nevertheless, according to similar effectiveness in iodine prophylaxis, both KI and KIO3 were initially proved to be used for fortifying salt by the Joint WHO/FAO Expert Committee on Food Additives and Contaminants [15] and they are, along with other iodine salts, still admitted to be added to foods, including food supplements [16].
It is well known that iodine affects red-ox balance [17]. It is especially known for its excellent antioxidative properties in physiological conditions [18, 19]. However, prooxidative effects of iodine were also demonstrated in experimental models. For example, in studies in vivo, iodine – given as iodide – expectedly increased MDA level in the rat thyroid and liver [20], or it increased Schiff’s bases in rat lung and liver [21] and – when given as KIO3 – in mice liver [22]. The latter change was accompanied by the increased activities of antioxidative enzymes, such as glutathione peroxidase and superoxide dismutase, but only after longer time (3 months) of iodine exposure [22]. Thus, the balance between anti- and prooxidative effects of iodine depends on different factors, such as iodine dose/concentration or the time of action.
However, anti- or prooxidative effects of iodine on the thyroid gland with relation to iodine source, i.e. a chemical compound containing iodine, have never been examined in vitro, thus under conditions reflecting direct effects of these compounds on thyroid follicular cells.
Fenton reaction (Fe2++H2O2→Fe3++•OH+OH−), being the basic reaction of oxidative stress, is of special significance in the thyroid gland, as both its substrates, i.e. H2O2 and Fe2+, are required for thyroid hormone synthesis [23]. One of the most frequently examined oxidative processes is lipid peroxidation (LPO), which results from oxidative damage to membrane lipids. Bivalent iron (Fe2+) and H2O2, which initiate Fenton reaction, have been frequently used to experimentally induce lipid peroxidation in different tissues [24–29], the thyroid gland included [30, 31]. Also oxidative damage to nuclear and mitochondrial DNA has been induced by Fenton reaction substrates [32].
The aim of the study was to evaluate effects of iodine, used as potassium iodide (KI) or potassium iodate (KIO3), on lipid peroxidation in porcine thyroid homogenates under basal conditions and in the presence of Fenton reaction substrates.
Preliminary results of the study were presented (as a poster presentation) during International and European Congress of Endocrinology in 2012 [33].
Methods
Ethical approval
The procedures, used in the study, were approved by the Ethics Committee of the Medical University of Lodz, Poland.
Chemicals
Potassium iodide (KI), potassium iodate (KIO3), ferrous sulfate (FeSO4) and hydrogen peroxide (H2O2) were purchased from Sigma (St. Louis, MO). The ALDetect Lipid Peroxidation Assay Kit was obtained from Enzo Life Sciences, Inc. (Zandhoven, Belgium). MilliQ-purified H2O was used for preparing all solutions. All the used chemicals were of analytical grade and came from commercial sources.
Animals
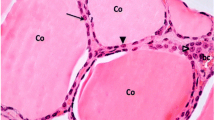
Porcine thyroids were collected from forty five (45) animals at a slaughter-house, frozen on solid CO2, and stored at -80°C until assay. Each experiment was repeated three to five times. Therefore, three to five tissue pools were prepared, with nine (9) thyroid glands used for each homogenate pool.
Assay of lipid peroxidation
Thyroid tissue was homogenized in ice cold 20 mM Tris-HCl buffer (pH = 7.4) (10%, w/v), and then incubated for 30 min at 37°C in the presence of examined substances. Porcine thyroid homogenates were incubated in the presence of either KI (500; 250; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25; 0.1; 0.05; 0.025; 0.01; 0.005; 0.0025; 0.001; 0.0005; 0.00025; 0.0001; 0.00005 mM) or KIO3 (200; 150; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25; 0.1; 0.05; 0.025; 0.01; 0.005; 0.0025; 0.001; 0.0005; 0.00025; 0.0001; 0.00005 mM) without or with addition of Fenton reaction substrates, i.e. FeSO4 (30 μM) + H2O2 (0.5 mM), or with addition of FeSO4 (30 μM) only. According to different solubility of KI and KIO3, different highest concentrations of these compounds were used in the study. Eight (8) separate experiments were performed, as it is specified in the Results section. The reactions were stopped by cooling the samples on ice. Each experiment was run in duplicate and repeated three to five times.
Measurement of lipid peroxidation products
The concentrations of malondialdehyde + 4-hydroxyalkenals (MDA + 4-HDA), as an index of lipid peroxidation, were measured in thyroid homogenates, with the ALDetect Lipid Peroxidation Assay Kit. The homogenates were centrifuged at 3,000 x g for 10 min at 4°C. After obtaining supernatant, each experiment was carried out in duplicate. The supernatant (200 μl) was mixed with 650 μl of a methanol:acetonitrile (1:3, v/v) solution, containing a chromogenic reagent, N-methyl-2-phenylindole, and vortexed. Following the addition of 150 μl of methanesulfonic acid (15.4 M), the incubation was carried out at 45°C for 40 min. The reaction between MDA + 4-HDA and N-methyl-2-phenylindole yields a chromophore, which is spectrophotometrically measured at the absorbance of 586 nm, using a solution of 10 mM 4-hydroxynonenal as the standard. The level of lipid peroxidation is expressed as the amount of MDA + 4-HDA (nmol) per mg protein. Protein was measured, using Bradford’s method [34], with bovine albumin as the standard.
Statistical analyses
Results are expressed as means ± SE. The data were statistically analyzed, using a one-way analysis of variance (ANOVA), followed by the Student-Neuman-Keuls’ test. The level of p < 0.05 was accepted as statistically significant.
Results
Two examined substances, i.e. KI and KIO3, did not reveal the same effects on oxidative damage to membrane lipids in porcine thyroid homogenates, both under basal conditions and in the presence of Fenton reaction substrates.
Potassium iodide, when used in the highest concentrations (≥50 mM), did increase lipid peroxidation in concentration-dependent manner. In turn, KI in concentrations ≤25 mM did not affect lipid peroxidation (Figure 1).
Lipid peroxidation, measured as MDA + 4-HDA level, in porcine thyroid homogenates. Homogenates were incubated in the presence of KI alone [500; 250; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25; 0.1; 0.05; 0.025; 0.01; 0.005; 0.0025; 0.001; 0.0005; 0.00025; 0.0001; 0.00005 mM]. Data are expressed as nmol/mg protein. Data are from four independent experiments. Values are expressed as mean ± SE (error bars). ap < 0.05 vs. control (in the absence of KI); bp < 0.05 vs. KI concentrations ≤100 mM; cp < 0.05 vs. any other KI concentration.
When KI was used together with Fe2++H2O2, the following results were obtained. Potassium iodide used in the middle range of concentrations (5.0; 10; 25; 50 and 100 mM) reduced Fenton reaction-induced lipid peroxidation, with the strongest protective effect observed for the concentration of 25 mM, which completely prevented experimentally-induced lipid peroxidation (Figure 2). Interestingly, KI either in higher (≥250 mM) or lower (≤2.5 mM) concentrations did not affect significantly Fenton reaction-induced lipid peroxidation, which means that the level of lipid peroxidation in the presence of KI (≥250 mM or ≤2.5 mM) plus Fe2++H2O2 was the same as in the presence of Fe2++H2O2 only (Figure 2).
Lipid peroxidation, measured as MDA + 4-HDA level, in porcine thyroid homogenates. Homogenates were incubated in the presence of KI [500; 250; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25; 0.1; 0.05; 0.025; 0.01; 0.005; 0.0025; 0.001; 0.0005; 0.00025; 0.0001; 0.00005 mM] and, additionally, in the presence of both Fenton reaction substrates, namely in the presence of FeSO4 [30 μM] plus H2O2 [0.5 mM]. Data are expressed as nmol/mg protein. Data are from three independent experiments. Values are expressed as mean ± SE (error bars). ap < 0.05 vs. control (in the absence of KI or Fe2++H2O2); bp < 0.05 vs. Fe2++H2O2, vs. KI [500 mM] + Fe2++H2O2, vs. KI [250 mM] + Fe2++H2O2; cp < 0.05 vs. KI [100 mM] + Fe2++H2O2.
Subsequently, to compare prooxidative effects of KI alone to prooxidative effects of KI plus Fenton reaction substrates, the separate experiment was performed, in which thyroid homogenates were incubated in the presence of KI (in concentrations of 0.25-500 mM) alone or together with Fe2++H2O2 (Figure 3). The level of lipid peroxidation was significantly higher when KI (in concentrations ≤100 mM) was used together with Fe2++H2O2. However, KI did not enhanced Fenton reaction-induced lipid peroxidation (Figure 3), which is in agreement with results shown in Figure 2.
Lipid peroxidation, measured as MDA + 4-HDA level, in porcine thyroid homogenates. Homogenates were incubated in the presence of KI alone [500; 250; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25 mM] or in the presence of KI [500; 250; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25 mM] together with both substrates of Fenton reaction, namely in the presence of FeSO4 [30 μM] plus H2O2 [0.5 mM]. Data are expressed as nmol/mg protein. Data are from three independent experiments. Values are expressed as mean ± SE (error bars). *p < 0.05 vs. respective concentration of KI alone (i.e. in the absence of Fe2++H2O2).
In our earlier study [31], Fe2+ used alone (i.e. as only one of Fenton reaction substrates), in opposite to H2O2, induced lipid peroxidation in thyroid homogenates. Therefore, in the present study we have performed the additional experiment with use of KI (in concentrations of 0.25-500 mM) alone or together with Fe2+ (Figure 4). No significant differences in lipid peroxidation were found for respective concentrations of KI in the presence or in the absence of Fe2+ (Figure 4).
Lipid peroxidation, measured as MDA + 4-HDA level, in porcine thyroid homogenates. Homogenates were incubated in the presence of KI alone [500; 250; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25 mM] or in the presence of KI [500; 250; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25 mM] together with one substrate of Fenton reaction, namely in the presence of FeSO4 [30 μM]. Data are expressed as nmol/mg protein. Data are from three independent experiments. Values are expressed as mean ± SE (error bars). No statistical differences between respective concentrations of KI (i.e. in the presence and in the absence of Fe2+) were found.
In the opposite to KI, KIO3 revealed, depending on the concentration or the presence/absence of Fe2++H2O2, either no protective effect at all or even strong prooxidative action (Figures 5 and 6). When KIO3 was used alone, it did increase lipid peroxidation in concentrations ≥2.5 mM (Figure 5). The damaging effect of KIO3 increased gradually from the concentration of 2.5 mM to 10 mM and, then, it decreased again gradually, however still being significantly stronger at the highest used KIO3 concentration (200 mM) than in control (Figure 5). The strongest damaging effect to membrane lipids was observed at the KIO3 concentration of 10 mM (Figure 5).
Lipid peroxidation, measured as MDA + 4-HDA level, in porcine thyroid homogenates. Homogenates were incubated in the presence of KIO3 alone [200; 150; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25; 0.1; 0.05; 0.025; 0.01; 0.005; 0.0025; 0.001; 0.0005; 0.00025; 0.0001; 0.00005 mM]. Data are expressed as nmol/mg protein. Data are from five independent experiments. Values are expressed as mean ± SE (error bars). ap < 0.05 vs. control (in the absence of KIO3); bp < 0.05 vs. any other KIO3 concentration.
Lipid peroxidation, measured as MDA + 4-HDA level, in porcine thyroid homogenates. Homogenates were incubated in the presence of KIO3 [200; 150; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25; 0.1; 0.05; 0.025; 0.01; 0.005; 0.0025; 0.001; 0.0005; 0.00025; 0.0001; 0.00005 mM] and, additionally, in the presence of both Fenton reaction substrates, namely in the presence of FeSO4 [30 μM] plus H2O2 [0.5 mM]. Data are expressed as nmol/mg protein. Data are from five independent experiments. Values are expressed as mean ± SE (error bars). ap < 0.05 vs. control (in the absence of KIO3 or Fe2++H2O2); bp < 0.05 vs. Fe2++H2O2 (in the absence of KIO3); cp < 0.05 vs. any other concentration of KIO3.
When KIO3 was used together with Fe2++H2O2, the following results were obtained. Potassium iodate enhanced Fenton reaction-induced lipid peroxidation, when it was used in concentrations of 5 mM to 200 mM, with the strongest damaging effect of KIO3 found again for the concentration of 10 mM (Figure 6). Concentration-dependent effects of KIO3 used together with Fenton reaction substrates were similar to those caused by KIO3 alone (compare Figures 5 and 6).
In comparative experiment (i.e. in the presence and in the absence of Fenton reaction substrates), the addition of Fe2++H2O2 enhanced KIO3-induced lipid peroxidation, but only for KIO3 concentration ≤10 mM) (Figure 7). Strong prooxidative effects of KIO3 in concentrations ≥25 mM was not enhanced by Fenton reaction substrates (Figure 7).
Lipid peroxidation, measured as MDA + 4-HDA level, in porcine thyroid homogenates. Homogenates were incubated in the presence of KIO3 alone [200; 150; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25 mM] or in the presence of KIO3 [200; 150; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25 mM] together with both substrates of Fenton reaction, namely in the presence of FeSO4 [30 μM] plus H2O2 [0.5 mM]. Data are expressed as nmol/mg protein. Data are from three independent experiments. Values are expressed as mean ± SE (error bars). *p < 0.05 vs. respective concentration of KIO3 alone (i.e. in the absence of Fe2++H2O2).
In turn, no significant differences were found for respective concentrations of KIO3 in the presence or in the absence of Fe2+ (Figure 8).
Lipid peroxidation, measured as MDA + 4-HDA level, in porcine thyroid homogenates. Homogenates were incubated in the presence of KIO3 alone [200; 150; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25 mM] or in the presence of KIO3 [200; 150; 100; 50; 25; 10; 5.0; 2.5; 1.0; 0.5; 0.25 mM] together with one substrate of Fenton reaction, namely in the presence of FeSO4 [30 μM]. Data are expressed as nmol/mg protein. Data are from three independent experiments. Values are expressed as mean ± SE (error bars). No statistical differences between respective concentrations of KI (i.e. in the presence and in the absence of Fe2+) were found.
Discussion
Molar concentrations of KI and KIO3 were calculated in the present study with regard to whole compounds. Among chemical elements forming either KI or KIO3, iodine is characterized by the highest molecular mass – much higher than potassium (K) and oxygen (O), thus it constitutes the crucial part of both compounds concerning their molecular masses, i.e. iodine constitutes 76.45% of molecular mass of KI, and in case of KIO3 it constitutes 59.30% of the molecular mass of this compound. In turn, the molecular mass of KI constitutes 77.57% of that one of KIO3, so the molecular masses of these two compounds are of the same order of magnitude. Therefore, concentrations of KI and of KIO3, calculated in the present study, may be used in comparative analyses either of effects of iodide ions (I-) formed from both KI and KIO3, or of effects of the whole compounds, i.e. KI and KIO3.
It is worth mentioning that in vitro KI treatment of the thyroid cell line PCCl3 resulted in the increased reactive oxygen species production [35]. Similar effect has not been evaluated after KIO3 treatment.
Only few studies have been performed till now to compare effects of iodine present in two different sources, namely in KI and KIO3. No differences were found between tissue (the thyroid gland, liver, kidney, muscle, abdominal fat tissue and skin) iodine content or blood thyroid hormone concentrations after in vivo treatment with high doses of either KI or KIO3 [8]. In similar in vivo model the same group of authors evaluated some parameters of oxidative stress [36]. Different compounds of iodine, i.e. KI or KIO3, have similar effects on lipid peroxidation level (measured as MDA concentration) in the liver and the muscle, however certain differences were observed concerning mRNA expressions or the activities of antioxidative enzymes in different tissues [36]. However, such comparative studies have not been performed under in vitro conditions. The present study is the first one in which KI was found to be superior to KIO3 in the thyroid gland concerning oxidative damage to macromolecules.
More favourable effects of KI comparing to KIO3 were observed both, when each of these compounds was used separately or together with Fenton reaction substrates. Concerning the first situation, both KI and KIO3 revealed – when used in high concentrations – damaging effects to membrane lipids in the thyroid. However, the difference between these unfavourable actions of KI and KIO3 was crucial. Namely, the damaging effect of KI decreased gradually with decreasing concentrations of this compound and these undesired effects were not observed for concentrations below 50 mM, thus concentrations corresponding to inorganic iodine level normally present in the thyroid under physiological conditions. On the basis of experimental findings [37–39] the concentration of inorganic iodine in the human or rat thyroid was calculated by the authors of the present work to be approx. 9 mM. Taking into account close similarity between human and porcine thyroid in terms of thyroid volume and of thyroid hormone synthesis with all elements and all steps of this process [40], it may be estimated that iodine concentration in porcine thyroid (used in the present study) is at similar level. Thus, the concentrations of KI resulting in thyroid level of inorganic iodine close to that observed under physiological conditions do not reveal prooxidative effects, at least in terms of oxidative damage to membrane lipids.
In opposite, when KIO3 was used alone, the highest lipid peroxidation was found for its concentration of 10 mM, thus corresponding to the physiological concentration in the thyroid, which was calculated to be 9 mM. It should be recalled that the same concentration of KI did not increase the level of lipid peroxidation (compare Figures 1 and 2).
When KI or KIO3 were added to the incubation medium together with Fenton reaction substrates, KI appeared to be also superior to KIO3 concerning their influence on lipid peroxidation in the thyroid gland. Whereas KI in concentrations of 5–100 mM (Figure 2), i.e. corresponding to physiological concentrations of inorganic iodine, diminished experimentally-induced lipid peroxidation, KIO3 did not reveal any protective action (Figure 5). Additionally, KI in concentration of 25 mM, thus being one order of magnitude higher than physiological iodine concentration, completely prevented Fenton reaction-induced lipid peroxidation. In turn, KIO3 enhanced Fenton reaction-induced lipid peroxidation, when it was used in concentrations of 5 mM to 200 mM, with the strongest damaging effect of KIO3 found again for the concentration of 10 mM (Figure 6).
Additionally it is clearly visible that prooxidative effects of KI was enhanced by Fenton reaction substrates. At the same time the damaging effects of KIO3 were so strong that they were only weakly enhanced by Fenton reaction substrates (compare Figures 1 and 2, Figures 5 and 6, Figures 3 and 7). These comparative analyses reveal additionally the superiority of KI over KIO3.
Ferrous ion (Fe2+), which was in our earlier study [31] documented to induce lipid peroxidation in the thyroid gland, when it was used as only one of Fenton reaction substrates, did not modify significantly in the present study the effect of either KI or of KIO3. This is probably due to the fact that prooxidative effects of Fe2+ alone is clearly weaker than those ones caused by both Fenton reaction substrates [31]. Potential mechanisms of differences between KI and KIO3 effects on lipid peroxidation in thyroid homogenates, observed in the present study, should be discussed. Thus, the following explanation is proposed.
The reduction of IO3 -, the process occurring when the tissue is exposed to KIO3, requires the time and energy and possibly it is associated with unfavorable oxidative reactions and the damaging effects.
In turn, KIO3 belongs to halogenate salts, which are known for their potentially toxic effects [5, 13, 41]. In our earlier studies, one of halogenate salts, namely potassium bromate (KBrO3), being classified as carcinogen (group 2B according to IARC 1986 [42]), was shown to exert damaging effect to membrane lipids in porcine thyroid under in vitro (5 mM) and in vivo conditions [43]. Thus, KBrO3 and KIO3 increased lipid peroxidation in porcine thyroid homogenates when used in the same range of concentrations. At the same time, iodine used as KI (in concentrations ≤25 mM) did not reveal in the present study any toxic effects to membrane lipids and even it prevented experimentally induced lipid peroxidation, when used in the same range of concentrations (5–100 mM).
However, from among three halogenate salts, i.e. iodate, bromate and chlorate, the first one is characterized by the lowest redox potential. Therefore, KIO3 seems to be potentially less toxic than bromate and chlorate, at least when oxidative mechanisms are considered.
Our study was performed under in vitro conditions and, therefore, it cannot be extrapolated directly into in vivo conditions, especially that IO3 - is reduced to I- before approaching the thyroid cell. However, our study is the first one which supports the statement that the use of KI in iodine prophylaxis is more safe than of KIO3, in terms of their influence on oxidative damage to macromolecules. Additionally, not only the thyroid gland should be considered in the aspect of prooxidative effects of KIO3 but, more importantly, other tissues, in particular digestive system, which is approached by KIO3 earlier, i.e. immediately after exposure to this salt.
Conclusions
Potassium iodide, used in doses generally recommended in iodide prophylaxis, thus resulting in physiological iodine concentration in the thyroid, may prevent oxidative damage to membrane lipids in this gland. Toxic effects of iodide overload may result from its prooxidative action. Potassium iodate does not possess any direct beneficial effects on oxidative damage to membrane lipids in the thyroid, which constitutes an additional argument against its utility in iodine prophylaxis.
References
Thilly CH, Vanderpas JB, Bebe N, Ntambue K, Contempre B, Swennen B, Moreno-Reyes R, Bourdoux P, Delange F: Iodine deficiency, other trace elements, and goitrogenic factors in the etiopathogeny of iodine deficiency disorders (IDD). Biol Trace Elem Res 1992, 32: 229–243. 10.1007/BF02784606
Zimmermann MB, Andersson M: Assessment of iodine nutrition in populations: past, present, and future. Nutr Rev 2012, 70: 553–570. 10.1111/j.1753-4887.2012.00528.x
Pearce EN, Andersson M, Zimmermann MB: Global iodine nutrition: where do we stand in 2013? Thyroid 2013, 23: 523–528. 10.1089/thy.2013.0128
World Health Organization, United Nations Children’s Fund, and the International Council for the Control of Iodine Deficiency Disorders Report of a Joint WHO/UNICEF/ICCIDD Consultation, 3–5 November 1992. In Indicators for Assessment of Iodine Deficiency Disorders and Their Control Programmes. Geneva: World Health Organization; 1993. Document WHO/NUT/93.1
Bürgi H, Schaffner TH, Seiler JP: The toxicology of iodate: a review of the literature. Thyroid 2001, 11: 449–456. 10.1089/105072501300176408
Rohner F, Garrett GS, Laillou A, Frey SK, Mothes R, Schweigert FJ, Locatelli-Rossi L: Validation of a user-friendly and rapid method for quantifying iodine content of salt. Food Nutr Bull 2012,33(Suppl 4):330–335.
Murray MM, Pochin EE: Thyroid uptake of iodine from ingested iodate in man. J Physiol 1951,114(Suppl):1–14.
Li Q, Mair C, Schedle K, Hammerl S, Schodl K, Windisch W: Effect of iodine source and dose on growth and iodine content in tissue and plasma thyroid hormones in fattening pigs. Eur J Nutr 2012, 51: 685–691. 10.1007/s00394-011-0247-7
Zhu YG, Huang YZ, Hu Y, Liu YX: Iodine uptake by spinach (Spinaciaoleracea L.) plants grown in solution culture: effects of iodine species and solution concentrations. Environ Int 2003, 29: 33–37. 10.1016/S0160-4120(02)00129-0
Voogt W, Holwerda HT, Khodabaks R: Biofortification of lettuce (Lactuca sativa L.) with iodine: the effect of iodine form and concentration in the nutrient solution on growth, development and iodine uptake of lettuce grown in water culture. J Sci Food Agric 2010, 90: 906–913.
AFSSA: Avis de l’Agence franc¸aise de se’curite’ sanitaire des aliments relatif a’ la modification de l’arre te’ du 28 mai 1997 portant sur le sel alimentaire et aux substances d’apport nutritionnel pouvant e tre utilise’es pour sa supple’mentation;. 2002.
Poul JM, Huet S, Godard T, Sanders P: Lack of genotoxicity of potassium iodate in the alkaline comet assay and in the cytokinesis-block micronucleus test. Comparison to potassium bromate. Food Chem Toxicol 2004, 42: 203–209. 10.1016/j.fct.2003.08.018
Parsons JL, Chipman JK: The role of glutathione in DNA damage by potassium bromate in vitro. Mutagenesis 2000, 15: 311–316. 10.1093/mutage/15.4.311
Pahuja DN, Rajan MG, Borkar AV, Samuel AM: Potassium iodate and its comparison to potassium iodide as a blocker of 131I uptake by the thyroid in rats. Health Phys 1993, 65: 545–549. 10.1097/00004032-199311000-00014
Joint WHO/FAO Expert Committee on Food Additives: Matters of interest arising from the forty-third World Health Assembly. In Evaluation of Certain Food Additives and Contaminants. Geneva: World Health Organization (WHO technical report series No. 806, Annex5; 1991.
European Commission: Commission Regulation (EC) No 1170/2009 of 30 November 2009 amending Directive 2002/46/EC of the European Parliament and of Council and Regulation (EC) No 1925/2006 of the European Parliament and of the Council as regards the lists of vitamin and minerals and their forms that can be added to foods, including food supplements. Official Journal of the European Union 2009, L 314: 36.
Aceves C, Anguiano B, Delgado G: The extrathyronine actions of iodine. Antioxidant, apoptotic and differentiator factor in iodine-uptake tissues. Thyroid in press
Venturi S, Venturi M: Iodide, thyroid and stomach carcinogenesis: evolutionary story of a primitive antioxidant? Eur J Endocrinol 1999, 140: 371–372. 10.1530/eje.0.1400371
Küpper FC, Carpenter LJ, McFiggans GB, Palmer CJ, Waite TJ, Boneberg EM, Woitsch S, Weiller M, Abela R, Grolimund D, Potin P, Butler A, Luther GW 3rd, Kroneck PM, Meyer-Klaucke W, Feiters MC: Iodide accumulation provides kelp with an inorganic antioxidant impacting atmospheric chemistry. Proc Natl Acad Sci U S A 2008, 105: 6954–6958. 10.1073/pnas.0709959105
Joanta AE, Filip A, Clichici S, Andrei S, Daicoviciu D: Iodide excess exerts oxidative stress in some target tissues of the thyroid hormones. Acta Physiol Hung 2006, 93: 347–359. 10.1556/APhysiol.93.2006.4.11
Sewerynek E, Swierczyńska-Machura D, Lewiński A: Effect of propylthiouracil on the level of Schiff’s bases in tissues of rats on diet with different doses of potassium iodide. Neuro Endocrinol Lett 2006, 27: 595–599.
Xia Y, Qu W, Zhao LN, Han H, Yang XF, Sun XF, Hao LP, Xu J: Iodine excess induces hepatic steatosis through disturbance of thyroid hormone metabolism involving oxidative stress in BALB/c mice. Biol Trace Elem Res 2013, 154: 103–110. 10.1007/s12011-013-9705-9
Karbownik M, Lewiński A: The role of oxidative stress in physiological and pathological processes in the thyroid gland; possible involvement in pineal-thyroid interactions. Neuroendocrinol Lett 2003, 24: 293–303.
Karbownik M, Reiter RJ, Garcia JJ, Tan D: Melatonin reduces phenylhydrazine-induced oxidative damage to cellular membranes: evidence for the involvement of iron. Int J Biochem Cell Biol 2000, 32: 1045–1054. 10.1016/S1357-2725(00)00056-X
Karbownik M, Gitto E, Lewiński A, Reiter RJ: Relative efficacies of indole antioxidants in reducing autoxidation and iron-induced lipid peroxidation in hamster testes. J Cell Biochem 2001, 81: 693–699. 10.1002/jcb.1100
Karbownik M, Lewiński A, Reiter RJ: Anticarcinogenic actions of melatonin which involve antioxidative processes: Comparison with other antioxidants. Int J Biochem Cell Biol 2001, 33: 735–753. 10.1016/S1357-2725(01)00059-0
Cabrera J, Burkhardt S, Tan DX, Manchester LC, Karbownik M, Reiter RJ: Autoxidation and toxicant-induced oxidation of lipid and DNA in monkey liver: reduction of molecular damage by melatonin. Pharmacol Toxicol 2001, 89: 225–230. 10.1034/j.1600-0773.2001.d01-152.x
Gitto E, Tan DX, Reiter RJ, Karbownik M, Manchester LC, Cuzzocrea S, Fulia F, Barberi I: Individual and synergistic antioxidative actions of melatonin: studies with vitamin E, vitamin C, glutathione and desferrioxamine (desferoxamine) in rat liver homogenates. J Pharm Pharmacol 2001, 53: 1393–1401. 10.1211/0022357011777747
Karbownik-Lewińska M, Kokoszko-Bilska A: Oxidative damage to macromolecules in the thyroid - experimental evidence. Thyroid Res 2012, 5: 25. 10.1186/1756-6614-5-25
Karbownik M, Lewiński A: Melatonin reduces Fenton-induced lipid peroxidation in porcine thyroid tissue. J Cell Biochem 2003, 90: 806–811. 10.1002/jcb.10689
Stępniak J, Lewiński A, Karbownik-Lewińska M: Membrane lipids and nuclear DNA are differently susceptive to Fenton reaction substrates in porcine thyroid. Toxicol In Vitro 2013, 27: 71–78. 10.1016/j.tiv.2012.09.010
Karbownik-Lewińska M, Stępniak J, Lewiński A: High level of oxidized nucleosides in thyroid mitochondrial DNA; damaging effects of Fenton reaction substrates. Thyroid Res 2012, 5: 24–32. 10.1186/1756-6614-5-24
Milczarek M, Stępniak J, Lewiński A, Karbownik-Lewińska M: Potassium iodide, but not potassium iodate, as a potential protective agent against oxidative damage to membrane lipids in porcine thyroid. In Proceedings of the 15th International & 14th European Congress of Endocrinology: 05–09 May 2012; Florence, European Society of Endocrinology. Edited by: Bioscientifica KB. Bristol: Euro House; 2012.
Bradford MM: A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 1976, 72: 248–254. 10.1016/0003-2697(76)90527-3
Leoni SG, Kimura ET, Santisteban P, De la-Vieja A: Regulation of thyroid oxidative state by thioredoxin reductase has a crucial role in thyroid responses to iodide excess. Mol Endocrinol 2011, 25: 1924–1935. 10.1210/me.2011-0038
Li Q, Mair C, Schedle K, Hellmayr I, Windisch W: Effects of varying dietary iodine supplementation levels as iodide or iodate on thyroid status as well as mRNA expression and enzyme activity of antioxidative enzymes in tissues of grower/finisher pigs. Eur J Nutr 2013, 52: 161–168. 10.1007/s00394-011-0298-9
Taurog A, Chaikoff IL, Feller DD: The mechanism of iodineconcentration by the thyroid gland: its non-organic iodine-binding capacity in the normal and propylthiouracil-treated rat. J Biol Chem 1947, 171: 189–201.
Taurog A, Tong W, Chaikoff IL: Non-thyroglobulin iodine of the thyroid gland II. Inorganic iodide. J Biol Chem 1951, 191: 677–682.
Tiran B, Karpf E, Tiran A, Lax S, Langsteger W, Eber O, Lorenz O: Iodine content of thyroid tissue in the Styrian population. Acta Med Austriaca 1993, 20: 6–8.
Kuzmuk KN, Schook LB: Pigs as a Model for Biomedical Sciences. In The Genetics of the Pig. 2nd edition. Edited by: Rothschild MF, Ruvinsky A. Wallingford: CAB International; 2011:426–444.
National Toxicology Program (NTP) NIH Publication No. 06–4457. In Toxicology and carcinogenesis studies of sodium chlorate (CAS No. 7775–09–9) in F344/N rats and B6C3F1 mice (drinking water studies), Technical Report Series no. 517.. Research Triangle Park, NC: National Institutes of Health, Public Health Service, U.S. Department of Health and Human Services; 2005.
WHO/IARC: IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans, Vol. 40, Some Naturally Occurring and Synthetic Food Components, Furocoumarins and Ultraviolet Radiation. Lyon: WHO/IARC; 1986:207–220.
Karbownik M, Stasiak M, Zasada K, Zygmunt A, Lewinski A: Comparison of potential protective effects of melatonin, indole-3-propionic acid, and propylthiouracil against lipid peroxidation caused by potassium bromate in the thyroid gland. J Cell Biochem 2005, 95: 131–138. 10.1002/jcb.20404
Acknowledgement
The research was supported by a grant from the National Science Centre (polish abbr. NCN) to the Medical University of Lodz (Project No. N N401 539540). This study constitutes a part of Ph.D. thesis of the first author of the paper (MM).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Authors declare that they have no competing interests.
Authors’ contributions
MM carried out the experiments, performed the statistical evaluation and prepared the draft of the manuscript. JS accompanied the steps of the study related to lipid peroxidation measurement. AL revised the final version of the manuscript. MK-L designed the study, supervised its conducting and prepared the final version of the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Milczarek, M., Stępniak, J., Lewiński, A. et al. Potassium iodide, but not potassium iodate, as a potential protective agent against oxidative damage to membrane lipids in porcine thyroid. Thyroid Res 6, 10 (2013). https://doi.org/10.1186/1756-6614-6-10
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-6614-6-10