Abstract
Background
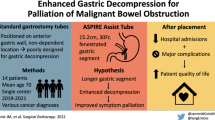
Malignant bowel obstruction affect a patient’s quality of life, but, management of MBO is controversial.
Case presentation
A 51-year-old woman who had been diagnosed as uterine cervix cancer 2 years ago and had undergone surgery, chemotherapy and radiotherapy, was admitted to our hospital. She was diagnosed as having a recurrence of peritoneal metastasis and bowel obstruction. For her nasal pain, we considered insertion of a postpyloric decompression tube through the gastrostomy instead of via the nasal cavity. After insertion of a percutaneous gastrostomy tube was performed endoscopically, we introduced a postpyloric decompression tube through her gastrostomy. She could be discharged home, and 91 days later, she died in her home under hospice care, as she had wished.
Conclusions
Insertion of a postpyloric decompression tube through a gastrostomy might be useful in the management of advanced cancer patients with bowel obstruction.
Similar content being viewed by others
Case presentation
A 51-year-old woman who had been diagnosed as having stage 2b uterine cervix cancer 2 years ago and had undergone surgery, chemotherapy and radiotherapy, was admitted to our hospital with nausea and abdominal pain. She was diagnosed as having a recurrence of peritoneal metastasis with complicating ascites and bowel obstruction. We first treated her conservatively however, a month later, her symptoms recurred and a postpyloric decompression tube was introduced via the nasal cavity. After the procedure, she complained of severe nasal pain and expressed her wish for treatment by a different method.
We therefore considered insertion of a postpyloric decompression tube through the gastrostomy instead of via the nasal cavity. Following obtainment of informed consent, insertion of a percutaneous gastrostomy tube was performed endoscopically (Figure 1). Two weeks later, we introduced a postpyloric decompression tube through her gastrostomy instead of via the nasal cavity. The postpyloric decompression was effective (Figure 2), she was discharged home, and 91 days later, she died in her home under hospice care, as she had wished.
Conclusions
Palliation of symptoms is the treatment goal terminal disease patients with MBO. Hospitalization and conservative management by nasogastric tube decompression and bowel rest is the first step in the management of MBO. However, when continuous postpyloric decompression is required, insertion of the postpyloric decompression tube through the gastrostomy instead of via the nasal cavity may be a reasonable approach, especially in patients hesitating to undergo tube placement via the conventional nasal approach and/or in gynecologic malignancies patients who are not good surgical candidates.
In conclusion, insertion of a postpyloric decompression tube through a gastrostomy might be useful in the management of advanced cancer patients with bowel obstruction.
Consent
Written informed consent was obtained from the patient and her family for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
References
Mori M, Bruera E, Dev R: Complications of a gastrostomy tube used for decompression of an inoperable bowel obstruction in a patient with advanced cancer. J Pain Symptom Manage. 2009, 38: 466-472. 10.1016/j.jpainsymman.2008.11.009.
Mangili G, Aletti G, Frigerio L, Franchi M, Panacci N, Viganò R, DE Marzi P, Zanetto F, Ferrari A: Palliative care for intestinal obstruction in recurrent ovarian cancer: a multivariate analysis. Int J Gynecol Cancer. 2005, 15: 830-835. 10.1111/j.1525-1438.2005.00144.x.
Meyer L, Pothuri B: Decompressive percutaneous gastrostomy tube use in gynecologic malignancies. Curr Treat Options Oncol. 2006, 7: 111-120. 10.1007/s11864-006-0046-1.
Dolan EA: Malignant bowel obstruction: a review of current treatment strategies. Am J Hosp Palliat Care. 2011, 28: 576-582. 10.1177/1049909111406706.
Rezk Y, Timmins PF, Smith HS: Review article: palliative care in gynecologic oncology. Am J Hosp Palliat Care. 2011, 28: 356-374. 10.1177/1049909110392204.
Roeland E, von Gunten CF: Current concepts in malignant bowel obstruction management. Curr Oncol Rep. 2009, 11: 298-303. 10.1007/s11912-009-0042-2.
Acknowledgements
Special thanks to medical staff of Yokohama City University Hospital.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interest.
Authors’ contributions
TK, AK and MI gave information about gastrostomy. SW and MI collect clinical data. YS, HI and TN gave information about endoscopy. AK gave information about palliative care. YK, TO and MI wrote the manuscript. EG, SM and AN supervised the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kurita, Y., Koide, T., Watanabe, S. et al. Postpyloric decompression tube placement through a gastrostomy for malignant bowel obstruction. BMC Res Notes 6, 217 (2013). https://doi.org/10.1186/1756-0500-6-217
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-0500-6-217