Abstract
Background
Healthy individuals can host Staphylococcus aureus in the nasopharynx, body surface and vagina. Most invasive infections by this bacterium are endogenous, caused by strains spread from the nasopharynx of carriers. S. aureus is a pathogen involved in the etiology of hospital- and community-acquired infections. Transplant and dialysis patients are at risk of colonization or infection by multi-resistant S. aureus. Infection is directly linked to individual immunity, and the major histocompatibility complex (MHC) plays a crucial role in determining susceptibility to diseases. Different MHC specificities have been shown to be more frequent in individuals suffering from certain diseases. This study aimed to investigate the association between HLA class I (HLA-A and -B) and class II (HLA-DRB1) molecules and nasal carriage of S. aureus in dialysis and kidney transplant patients at a hospital in Southern Brazil.
Results
The sample consisted of 70 dialysis and 46 kidney transplant patients, totaling 116 patients. All subjects were typed for HLA molecules using LABType® SSO (One Lambda). Nasal swab samples of S. aureus were isolated from the nasal cavity (both nostrils) of patients undergoing dialysis or kidney transplantation.
In renal dialysis patients, HLA-A*02 was the most frequent allele in both carriers (25.5%) and non-carriers (21.2%) of S. aureus. Allele A*68 was not observed in the carrier group, but the allele was observed six times in the non-carrier group (p = 0.0097). Regarding HLA-B and HLA-DRB1, no allele was shown to be involved in protection against or susceptibility to carriage of S. aureus. In kidney transplant patients, allele A*03 was more frequent in the non-carrier (20.83%) than in the carrier (5.88%) group (p = 0.0486). HLA-B*15 was present in carriers (5.88%) and non-carriers (25%) (p = 0.0179). Regarding class II alleles, DRB1*03 appeared to be related to susceptibility to carriage of S. aureus (p = 0.0319).
Conclusions
Our findings suggest that HLA-DRB1*03 may be involved in susceptibility to nasal carriage of S. aureus in transplant patients. In addition, HLA-A*68 (dialysis patients) and HLA-A*03 and HLA-B*15 (transplant patients) appear to be associated with increased resistance to S. aureus nasal carriage.
Similar content being viewed by others
Background
Staphylococcus aureus is considered an important etiologic agent due to its high frequency and pathogenicity, causing diseases in both healthy and immunocompromised individuals. This microorganism is able to spread easily in the hospital environment and to develop resistance to antimicrobial agents [1, 2].
Approximately 20% of adults are carriers of S. aureus in the nasopharynx, another 30% carry it intermittently, and 50% are not carriers [3, 4]. Persistent nasal carriers of S. aureus are at higher risk of developing infection [5, 6]. Dialysis and kidney transplant patients are particularly prone to infection due to constant exposure to risk factors and immunosuppression [2, 7].
Infection is directly related to individual immunity and the major histocompatibility complex (MHC)--a set of genes found on the short arm of human chromosome 6--plays a crucial role in determining susceptibility to diseases. Specifically, MHC contains a group of genes that code for several proteins expressed on the surface of a variety of cell types. In humans, these molecules are known as human leukocyte antigens (HLA) [8].
Molecules of the HLA system are classified as class I (HLA-A, -B and -C), class II (HLA-DR, -DQ and -DP), and class III. These molecules are highly polymorphic glycoproteins that differentiate themselves from one another by their location in tissues and their function. Class I molecules are present on the surface of all nucleated cells and are responsible for presenting peptides to cytotoxic T cells (CD8+). Class II molecules are distributed less widely, being found primarily on the surface of cells linked directly to the immune response (such as macrophages, monocytes, dendritic cells, Langerhans cells, B lymphocytes, and activated T lymphocytes), with the purpose of presenting peptides to regulatory T cells (CD4+). The class III region does not encode histocompatibility molecules, but rather other molecules such as tumor necrosis factors, C4 and C2 proteins, complement factor B, heat shock protein, and 21-hydroxylase enzyme [9–12].
Different HLA specificities have been shown to be more frequent in individuals suffering from certain diseases, and characterizing these molecules may have important clinical implications [13–15].
The role of the HLA system in pathogenesis has been studied in several diseases, such as skin diseases [16–18], tuberculosis [19, 20], psychiatric illnesses [21, 22], as well as hearing [23, 24], sight [25, 26] and kidney [27] problems. Nasal carriage of Staphylococcus spp. has been investigated in dialysis and kidney transplant patients [28, 29]; however, only a few studies have investigated the involvement of genetic factors in this carriage. A literature review returned only one study, published in 1983, investigating the association between HLA molecules and nasal carriage of S. aureus in healthy laboratory workers and outpatients [30].
Thus, this study aimed to investigate the association between HLA class I (HLA-A and -B) and class II (HLA-DRB1) molecules and nasal carriage of S. aureus in dialysis and kidney transplant patients at a hospital in Southern Brazil.
Methods
The study population consisted of 70 renal patients undergoing dialysis and 46 kidney transplant patients, totaling 116 patients. All subjects were typed for HLA class I (A, B) and class II (DRB1) molecules and evaluated for nasal carriage. Biological material, nasal discharge and blood were collected between June and November 2009.
Staphylococcus aureus identification
Nasal swab samples of S. aureus were isolated from the nasal cavity of patients undergoing dialysis or kidney transplantation by inserting sterile swabs into both nostrils. The material was placed in Petri dishes (90 × 15 mm) containing mannitol salt agar (MSA) (Becton Dickinson & Co., BD Diagnostic Systems, USA), transferred to a test tube containing trypticase soy broth (TSB) with 6.5% NaCl, and then placed in a stove for 24 hours. After 24-48 hours of incubation at 37°C, suspected S. aureus colonies were subjected to Gram staining and immersion microscopy. Those identified as Gram-positive cocci arranged in grape-like clusters were transferred to a TSB medium with 6.5% NaCl. The tube coagulase test was performed after six hours of incubation. After the identification tests, samples were stored in a TSB medium with glycerol (20%) and frozen at -20°C for later analysis.
HLA typing
Human DNA extraction: Peripheral blood was collected by venipuncture in vacuum tubes containing EDTA anticoagulant, and genomic DNA was extracted using EZ-DNA reagent, according to the manufacturer's instructions (Biological Industries, Kibbutz Beit, Haemek, Israel).
Genetic polymorphism of HLA molecules: One Lambda LABType® SSO kit was used in combination with the Luminex™ technology for typing of HLA class I (HLA-A and -B) and class II (HLA-DRB1) alleles.
Statistical analysis
For data analysis, dialysis and transplant patients were subdivided into carriers and non-carriers of S. aureus. The number of times a given allele was found (n) and allele frequency (Af) were quantified in both patient groups. P-value was calculated using Fisher's exact test (P-value). Bonferroni correction (Pc-value) was used to calculate p values below 0.05. The odds ratio (OR) and confidence interval (95%CI) were calculated whenever the p value was lower than 0.05.
Ethical aspects
The study was approved by the Research Ethics Committee of Universidade Estadual de Maringá (protocol no. 212/2009), and written informed consent was obtained from all participants. The study was conducted in accordance with the provisions of the Declaration of Helsinki.
Results
Of 70 dialysis patients, 30 (42.8%) were female and 40 (57.1%) male. Age ranged from 22 to 85 years. Thirty-seven patients (52.8%) were nasal carriers of S. aureus and 33 (47.1%) were non-carriers.
Of 46 patients evaluated in the transplant group, 16 (34.7%) were female and 30 (65.2%) male. Age ranged from 18 to 64 years. Thirty-four patients (74%) were nasal carriers of S. aureus and 12 (26%) were non-carriers.
Study association with dialysis patients and their status as nasal carriers or non-carriers of Staphylococcus aureus
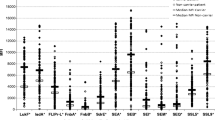
Analysis of the frequency of class I, A and B alleles, and class II, DRB1 alleles, (Table 1) showed that HLA-A*02 was the most frequent allele in both carriers (25.5%) and non-carriers (21.2%). HLA-A*68 was not observed in the carrier group, but the allele was observed six times in the non-carrier group (p = 0.0097). This result suggests a tendency towards protection or resistance against nasal carriage of S. aureus. Regarding HLA-B and -DRB1, no allele was shown to be involved in protection against or susceptibility to carriage of S. aureus.
Study association with kidney transplant patients and their status as nasal carriers or non-carriers of Staphylococcus aureus
As shown in Table 2, HLA-A*03 was more frequent in the non-carrier group (20.83%) than in the carrier group (5.88%) (p = 0.0486), which suggests a tendency towards protection against carriage of S. aureus. HLA-B*15 also showed a trend towards protection against carriage (carriers: 5.88%; non-carriers: 25%) (p = 0.0179). Regarding class II alleles, DRB1*03 appeared to be related to susceptibility to carriage of S. aureus (p = 0.0319).
Discussion
The molecules of the HLA system, which are directly linked to the immune response, play a crucial role in the susceptibility to or protection against infectious diseases [31]. The determination of these molecules is often used in association studies with various illnesses, allowing a search for specific markers of susceptibility or resistance [32, 33]. In our study, we demonstrated that certain HLA alleles could be involved in nasal carriage of S. aureus in dialysis and kidney transplant patients.
During the literature review, we found only one study on HLA and nasal carriage of S. aureus [30], which employed the serological method of HLA typing. That study analyzed healthy laboratory workers and patients attending an outpatient clinic in Dublin and Galway, Ireland. A positive association was found between HLA-DR3 antigen and carriage of S. aureus, making individuals more susceptible to carrying the bacterium. Class I (HLA-Bw35) and class II (HLA-DR2 and HLA-DR1) antigens were also shown to be involved in resistance against non-carriage of the bacterium.
The present study contributed to confirm the involvement of HLA-DRB1*03 (serological equivalent DR3) as a possible genetic marker for susceptibility to nasal carriage of S. aureus. It also contributed to demonstrate the involvement of HLA class I specificities (-A*03, -A*68, and -B*15) as protective factors against nasal carriage of S. aureus in renal patients.
The importance of identifying patients carrying S. aureus, in particular those with a multi-resistant profile, lies in the fact that this pathogen is linked to endogenous infections [34]. In that sense, it is worth noting that infectious diseases exert selective genetic pressure, and the genes involved in the immune response are the most numerous and polymorphic of the human genome, thereby indicating the evolutionary advantages of the immune response to a wide variety of pathogens. This is evidenced by the participation of HLA in the presentation of foreign peptides to immune system cells [35].
Conclusions
Our findings suggest that HLA-DRB1*03 may be involved in susceptibility to nasal carriage of S. aureus in transplant patients. In addition, HLA-A*68 (dialysis patients) and HLA-A*03 and HLA-B*15 (transplant patients) appear to be associated with increased resistance to S. aureus nasal carriage.
Further studies are warranted to clarify the role of HLA as a genetic marker in resistance against or susceptibility to carriage of S. aureus. Establishing the role of host genetic factors should contribute to a better understanding of infectious conditions as well as to develop new therapies according to the progress in the field of pharmacogenetics.
Availability of supporting data
The data set supporting the results of this article is available in the repository of Universidade Estadual de Maringá (UEM), at UEM Digital Library, under no. VTLS 000184756/www.bce.uem.br.
References
Enright MC, Robinson DA, Randle G, Feil EJ, Grundmann H, Spratt BG: The evolutionary history of methicillin-resistant Staphylococcus aureus (MRSA). Proc Natl Acad Sci USA. 2002, 99 (11): 7687-7692. 10.1073/pnas.122108599.
Vandecasteele SJ, Boelaert JR, De Vriese AS: Staphylococcus aureus infections in hemodialysis: what a nephrologist should know. Clin J Am Soc Nephrol. 2009, 4 (8): 1388-1400. 10.2215/CJN.01590309.
Boyce JM: Methicillin-resistant Staphylococcus aureus: a continuing infection control challenge. Eur J Clin Microbiol Infect Dis. 1994, 13 (1): 45-49. 10.1007/BF02026126.
Wertheim HF, Melles DC, Vos MC, van Leeuwen W, van Belkum A, Verbrugh HA, Nouwen JL: The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis. 2005, 5 (12): 751-762. 10.1016/S1473-3099(05)70295-4.
Gonzalez-Zorn B, Senna JP, Fiette L, Shorte S, Testard A, Chignard M, Courvalin P, Grillot-Courvalin C: Bacterial and host factors implicated in nasal carriage of methicillin-resistant Staphylococcus aureus in mice. Infect Immun. 2005, 73 (3): 1847-1851. 10.1128/IAI.73.3.1847-1851.2005.
van Leeuwen WB, Melles DC, Alaidan A, Al-Ahdal M, Boelens HA, Snijders SV, Wertheim H, van Duijkeren E, Peeters JK, van der Spek PJ, et al: Host- and tissue-specific pathogenic traits of Staphylococcus aureus. J Bacteriol. 2005, 187 (13): 4584-4591. 10.1128/JB.187.13.4584-4591.2005.
Ghasemian R, Najafi N, Makhlough A, Khademloo M: Frequency of nasal carriage of Staphylococcus aureus and its antimicrobial resistance pattern in patients on hemodialysis. Iran J Kidney Dis. 2010, 4 (3): 218-222.
Peakman M, Vergan D: Basic and clinical immunology. 1997, New York: Churchill Livingstone
Pamer E, Cresswell P: Mechanisms of MHC class I-restricted antigen processing. Annu Rev Immunol. 1998, 16: 323-358. 10.1146/annurev.immunol.16.1.323.
Navarrete CV: The HLA system in blood transfusion. Baillieres Best Pract Res Clin Haematol. 2000, 13 (4): 511-532. 10.1053/beha.2000.0097.
Turner D: The human leucocyte antigen (HLA) system. Vox Sang. 2004, 87 (Suppl 1): 87-90.
Alves C, Vieira N, Meyer I, Alves CO, Toralles MBP, Oliveira MdFSP: Human histocompatibility antigens and Dermatology: from research to clinical practice. An bras dermatol. 2006, 81 (1): 65-73. 10.1590/S0365-05962006000100009.
Neustadt DH: Ankylosing spondilitis. Postgrad Med. 1977, 61 (1): 124-135.
Singh R, Kaul R, Kaul A, Khan K: A comparative review of HLA associations with hepatitis B and C viral infections across global populations. World J Gastroenterol. 2007, 13 (12): 1770-1787.
Jacobson EM, Huber A, Tomer Y: The HLA gene complex in thyroid autoimmunity: from epidemiology to etiology. J Autoimmun. 2008, 30 (1-2): 58-62. 10.1016/j.jaut.2007.11.010.
Arnett FC: HLA and genetic predisposition to lupus erythematosus and other dermatologic disorders. J Am Acad Dermatol. 1985, 13 (3): 472-481. 10.1016/S0190-9622(85)70191-0.
Biral AC, Magalhaes RF, Wastowski IJ, Simoes R, Donadi EA, Simoes AL, Mendes-Junior CT, Tanaka AM, Kraemer MH: Association of HLA-A, -B, -C genes and TNF microsatellite polymorphism with psoriasis vulgaris: a study of genetic risk in Brazilian patients. Eur J Dermatol. 2006, 16 (5): 523-529.
Belazarian L: New insights and therapies for teenage psoriasis. Curr Opin Pediatr. 2008, 20 (4): 419-424. 10.1097/MOP.0b013e328305e24b.
John GT, Murugesan K, Jeyaseelan L, Pulimood RB, Jacob CK, Shastry JC: HLA phenotypes in Asians developing tuberculosis on dialysis or after renal transplantation. Natl Med J India. 1995, 8 (3): 144-146.
Harfouch-Hammoud EI, Daher NA: Susceptibility to and severity of tuberculosis is genetically controlled by human leukocyte antigens. Saudi Med J. 2008, 29 (11): 1625-1629.
Gaughran F: Immunity and schizophrenia: autoimmunity, cytokines, and immune responses. Int Rev Neurobiol. 2002, 52: 275-302.
Nunes SO, Borelli SD, Matsuo T, Watanabe MA, Itano EN: The association of the HLA in patients with schizophrenia, schizoaffective disorder, and in their biological relatives. Schizophr Res. 2005, 76 (2-3): 195-198. 10.1016/j.schres.2005.02.005.
Yeo SW, Chang KH, Suh BD, Kim TG, Han H: Distribution of HLA-A, -B and -DRB1 alleles in patients with sudden sensorineural hearing loss. Acta Otolaryngol. 2000, 120 (6): 710-715. 10.1080/000164800750000225.
Amor-Dorado JC, Paco L, Martin J, Lopez-Nevot MA, Gonzalez-Gay MA: Human leukocyte antigen-DQB1 and -DRB1 associations in patients with idiopathic sudden sensorineural hearing loss from a defined population of Northwest Spain. Acta Otolaryngol. 2005, 125 (12): 1277-1282. 10.1080/00016480510012228.
Quiroz-Mercado H, Suarez-Licona A, Fromow-Guerra J, Lopez-Carasa G, Cardenas-Hernandez R, Ruiz-Morales JA, Portal-Celhay C, Granados J: Human lymphocyte antigen DR7 protects against proliferative retinopathy with type II diabetes mellitus. Arch Med Res. 2002, 33 (2): 123-127. 10.1016/S0188-4409(01)00378-2.
Ueta M, Tokunaga K, Sotozono C, Inatomi T, Yabe T, Matsushita M, Mitsuishi Y, Kinoshita S: HLA class I and II gene polymorphisms in Stevens-Johnson syndrome with ocular complications in Japanese. Mol Vis. 2008, 14: 550-555.
Koonin EV, Altschul SF, Bork P: BRCA1 protein products ... Functional motifs. Nat Genet. 1996, 13 (3): 266-268. 10.1038/ng0796-266.
Alonso-Morquecho A, Flores-Preciado H, Martínez-García MC: Prevalence of infection in patients with central venous catheters. Revista Enf IMSS. 2000, 8 (3): 139-143.
Ferreira V, Andrade D, Santos CB, Neto MM: Infection in patient with temporary double-lumen catheter for hemodialysis. Rev Panam Infectol. 2005, 7 (2): 16-21.
Kinsman OS, McKenna R, Noble WC: Association between histocompatability antigens (HLA) and nasal carriage of Staphylococcus aureus. J Med Microbiol. 1983, 16 (2): 215-220. 10.1099/00222615-16-2-215.
Blackwell JM, Jamieson SE, Burgner D: HLA and infectious diseases. Clin Microbiol Rev. 2009, 22 (2): 370-385. 10.1128/CMR.00048-08. Table of Contents
Caillat-Zucman S: Molecular mechanisms of HLA association with autoimmune diseases. Tissue Antigens. 2009, 73 (1): 1-8. 10.1111/j.1399-0039.2008.01167.x.
Schlosstein L, Terasaki PI, Bluestone R, Pearson CM: High association of an HL-A antigen, W27, with ankylosing spondylitis. N Engl J Med. 1973, 288 (14): 704-706. 10.1056/NEJM197304052881403.
Burian M, Wolz C, Goerke C: Regulatory adaptation of Staphylococcus aureus during nasal colonization of humans. PLoS One. 2010, 5 (4): e10040-10.1371/journal.pone.0010040.
Burgner D, Jamieson SE, Blackwell JM: Genetic susceptibility to infectious diseases: big is beautiful, but will bigger be even better?. Lancet Infect Dis. 2006, 6 (10): 653-663. 10.1016/S1473-3099(06)70601-6.
Acknowledgements
The authors gratefully acknowledge the participation of the patients. This study received financial support from Fundação Araucária, Paraná, Brazil.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SDB carried out HLA typing, drafted the manuscript and revised it critically for the intellectual content. RRS participated in the collection of biological material, processing and analysis of data. JB participated in the design of the study, helped to draft the manuscript and revised it critically for the intellectual content. WVSJ participated in the design of the study and performed the statistical analysis. LBG participated in the collection of biological material, processing and analysis of data, helped to draft the manuscript and revised it critically for the intellectual content. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Giarola, L.B., dos Santos, R.R., Bedendo, J. et al. HLA molecules and nasal carriage of Staphylococcus aureus isolated from dialysis and kidney transplant patients at a hospital in Southern Brazil. BMC Res Notes 5, 90 (2012). https://doi.org/10.1186/1756-0500-5-90
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-0500-5-90