Abstract
Background
The objective of this analysis was to measure changes in items on the Pediatric Adverse Event Rating Scale (PAERS) that relate to emotional well-being of children and adolescents with Attention-Deficit/Hyperactivity Disorder (ADHD) during treatment with atomoxetine for up to 24 weeks from the perspective of the patient, the parent, and the physician.
Methods
Patients aged 6–17 years with ADHD were treated with atomoxetine (target dose 1.2 mg/kg/day). In the two studies on which this secondary analysis is based the PAERS was used to assess the tolerability of atomoxetine in children and adolescents. This scale has a total of 48 items. The ten items that reflect emotional well-being were selected to measure changes over time from a patient, parent, and physician perspective.
Results
421 patients were treated with atomoxetine. 355 patients completed the 8-week treatment period, and 260 patients completed the 24-week treatment period. The ten items that reflect emotional well-being were grouped in five dimensions: depressed mood, self-harm, irritability/agitation, drowsiness, and euphoria. The scores of these dimensions decreased over time, both from a patient as well as from a parent and physician perspective. Only the dimension self-harm was extremely low at baseline and stayed low over time. The mean scores for the ten items depended on the rater perspective.
Conclusion
The emotional well-being of children and adolescents with ADHD improved in terms of depressed mood, irritability/agitation, drowsiness, and euphoria during treatment with atomoxetine for up to 24 weeks.
Similar content being viewed by others
Background
Attention-deficit/hyperactivity disorder (ADHD) is a disorder characterized by inattention, impulsivity, and hyperactivity that affects 3–7% of school-age children [1]. ADHD is usually associated with significant impairment of cognitive and psychosocial functioning [2, 3] and can have a significant impact on the emotional well-being [4–6] and the quality of life (QoL) of both patients and their families [7–12].
Psychostimulants and behavioral therapy are known to be effective in the treatment of ADHD, as reported in the MTA study [13]. Atomoxetine is a non-stimulant treatment option for ADHD [14, 15], for which efficacy and tolerability in children and adolescents have been demonstrated in a number of randomized, placebo-controlled trials [16–19], supported by a recent meta-analysis [20]. In most of these studies, questionnaires such as the ADHD-Rating Scale (ADHD-RS) [21, 22] or the Clinical Global Impression (CGI) [23, 24] have been used as outcome measures for the core symptoms of ADHD. Other questionnaires such as the Child Health Questionnaire (CHQ) [25] or the Child Health and Illness Profile, Child Edition (CHIP-CE) [26] assess aspects of ADHD that go beyond the core symptoms of the disorder and reflect various dimensions of health-related quality of life. However, such questionnaires are often rated by the investigator alone, resulting in an assessment from one perspective only. Therefore, several studies have attempted to compare the perspectives of the various individuals involved, such as the patient, the parent, or the physician, as these perspectives have been shown to differ [12, 27]. The newly devised Global Impression of Perceived Difficulties (GIPD) is one such instrument with which the three perspectives can be compared [28, 29]. The Pediatric Adverse Event Rating Scale (PAERS) also allows the comparison between patient, parent, and physician perspectives, although it was designed to capture the tolerability of medication rather than efficacy [30].
This report is based on a secondary analysis of data from two almost identical multi-center, single-arm, open-label studies in two different age groups (children and adolescents). These studies were designed to investigate the quality of life in patients with ADHD treated with atomoxetine as reflected by the degree of difficulties perceived by patients, parents and physicians [28, 29]. The two studies were undertaken to address the need for further research on evidence-based psychopharmacological treatments in children and adolescents [31]. One of the aims of the two studies on which this post-hoc analysis is based [28, 29] was to assess the tolerability of atomoxetine in these patients and compare the tolerability as perceived from the three perspectives (patient, parent, physician) using the Pediatric Adverse Event Rating Scale (PAERS). The PAERS is a 48-item questionnaire designed to assess any type of adverse event occurring in pediatric patients who are treated with psychotropic medication, especially as participant in clinical trials, and was developed as part of the Child and Adolescent Psychiatry Trials Network (CAPTN) [30, 32–34]. The response captures the severity of 48 adverse event items on a five-point Likert scale (0–4).
The main assumption of this post-hoc analysis was that 10 of the 48 items of the PAERS are directly related to the patients' emotional state and can therefore be considered to reflect the patient's emotional well-being. Based on this assumption, the hypothesis of this analysis was that the emotional well-being of children and adolescents with ADHD responds well to treatment with atomoxetine as reflected by the 10 items of the PAERS directly related to the patient's emotional state. Differences between the three perspectives (patient, parent, physician) were also explored.
Methods
Study design and procedures
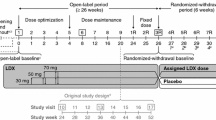
This is a secondary analysis of data from two almost identical multi-center, single-arm, open-label studies in two different age groups (children and adolescents) that were designed to investigate the quality of life in patients with ADHD treated with atomoxetine as reflected by the degree of difficulties perceived by patients, parents and physicians [28, 29]. Patients were recruited from child and adolescent psychiatric and pediatric practices and outpatient clinics throughout Germany. Patients aged 6–17 years with ADHD as defined in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) [1] were eligible for the studies. The diagnosis was confirmed using the "Diagnose-Checkliste Hyperkinetische Störungen" (Diagnostic Checklist for Hyperkinetic Disorders), a structured instrument which is routinely used for the diagnostic assessment of ADHD in Germany [35]. The items of this instrument correspond to those of the ADHD-RS [21, 22]. Patients had to have an IQ of ≥70 based on the clinical judgment of the investigator. The exclusion criteria included clinically significant abnormal laboratory findings, acute or unstable medical conditions, cardiovascular disorder, history of seizures, pervasive developmental disorder, psychosis, bipolar disorder, suicidal ideation, any medical condition that might increase sympathetic nervous system activity, or the need for psychotropic medication other than study drug. Patients already being treated with atomoxetine were also excluded. Other previous treatments were allowed, provided they were discontinued prior to enrolment in the study. The protocol was approved by an ethics committee, and the study was conducted in accordance with the principles of the Declaration of Helsinki. Following a wash-out period, baseline assessments were carried out with all the instruments used. During the first week of treatment, the patients received atomoxetine at a dose of approximately 0.5 mg/kg body weight (BW) per day. During the following 7 weeks, the recommended target dose was 1.2 mg/kg BW per day, but could be adjusted within a range of 0.5–1.4 mg/kg BW per day, depending on effectiveness and tolerability. Medication was given once a day in the morning. Assessments were carried out weekly during the first two weeks of treatment, and every two weeks thereafter. After the 8 week treatment period, the physicians decided in accordance with the patients and their parents whether the patient was to continue treatment for additional 16 weeks. Those who participated in this extension period continued on the same atomoxetine dose which again could be adjusted within a range of 0.5–1.4 mg/kg BW per day as considered appropriate by the physician. During the extension period, three assessments were carried out, after 12, 16, and 24 weeks after baseline. The following instruments were used to assess efficacy: Global Impression of Perceived Difficulties (GIPD), Attention-Deficit/Hyperactivity Disorder Rating Scale (ADHD-RS), Clinical Global Impression-Severity (CGI-S), and the Weekly Rating of Evening and Morning Behavior – Revised (WREMB-R). The results from these scales have been published elsewhere [28, 29].
In order to assess the tolerability of atomoxetine in more detail than is possible using spontaneous adverse event reports, the Pediatric Adverse Event Rating Scale (PAERS) [30] was used in the two studies reported here. The data from both studies were combined and analyzed together. Tolerability assessments included monitoring vital signs at every visit and recording all spontaneously reported adverse events, followed by a systematic elicitation of any further adverse events using the PAERS. First, the physician asked an open question as to any adverse events. Then, the patient and the parent (or other primary caregiver) filled out the PAERS independently and without any interference by the physician. Both the patient and the parent had to rate each adverse event in terms of how bothersome or how much of a problem it was during the past week on a scale from 0 (= not present) to 4 (= a lot). If the patient was unable to fill out the scale all by him or her self, an independent person (e. g. a study nurse, but not the parent or physician) was allowed to provide assistance. As the spontaneous adverse event reports captured by the physician preceded the elicitation of any further adverse events using the PAERS, the number of adverse events captured by these two methods potentially differed.
Although the PAERS was designed to measure adverse events, some items are reflecting ADHD symptoms and difficulties associated with ADHD rather than adverse events. These items can be expected to improve but not worsen during ADHD treatment. Of these, all ten items of the PAERS that were thought to reflect emotional well-being by face validity were selected for this post-hoc analysis to measure changes over time.
Noncompliance was defined as missing intake of study drug on more than five consecutive days, failure to take at least 70% of study medication for at least two weeks, or repeated intentional intake of more than the prescribed dose.
Sample size and statistical analysis
Details on the sample size calculation for the two studies have been published elsewhere [28, 29]. The data of all patients were evaluated (Full Analysis Set, FAS) using SAS version 8. The dataset for all analyses of changes from baseline to endpoint consisted of all patients with a baseline measurement and at least one post-baseline measurement during the 8-week treatment phase.
Evaluation was largely descriptive. All tests of statistical significance were carried out at a nominal level of 5% using two-tailed test procedures. Two-sided confidence intervals (CIs) were computed using a 95% confidence level. All inferences regarding statistical significance were based on comparisons of the 95% confidence intervals (CI). This is equivalent to significance tests with p-values and a two-sided α-level of 5%. To avoid correlations of imputed values, only observed cases (OC) analysis were performed. No imputation of missing values like last observation carried forward (LOCF) was applied as the intention was to describe the patterns for patients still on medication.
Spearman's correlation coefficients were computed between all items within each perspective in order to identify patterns of interdependency among items. This analysis was based on all visits. A sensitivity analysis was done using the baseline visit only. 95% confidence intervals for the correlation coefficients were computed based on Fisher's z-transformation.
Results
Patient population and disposition
Of the 425 patients screened, 421 patients (100%) were enrolled in the two studies and treated with atomoxetine [28, 29]. All patients were diagnosed with ADHD according to DSM-IV criteria. The mean age of the patients was 11.1 years, 338 (80.3%) were boys, 83 (19.7%) were girls. The 8-week treatment period was completed by 355 (84.3%) patients. 27 (6.4%) of these did not continue into the extension period because of physician decision. 68 (16.1%) patients discontinued the study between week 8 and week 24. The extension period was completed at week 24 by 260 (61.8%) patients. The reasons for discontinuation at any time during the 24-month observation period were lack of efficacy (12.4%), parent decision (6.9%), adverse event (4.8%), protocol violation 3.6%, patient decision (2.4%), entry criteria exclusion (0.7%), physician decision (0.7%), and patient lost to follow-up (0.5%). The patient disposition is shown in Figure 1.
Table 1 shows the patient characteristics. Boys and patients with the combined subtype ADHD according to DSM-IV [1] tended to be younger and tended to be diagnosed earlier than girls or patients with predominantly inattentive subtype. 239 (70.7%) of the boys and 39 (47.0%) of the girls were diagnosed with the combined subtype. The predominantly inattentive subtype was diagnosed in 86 (25.4%) of the boys and 38 (45.8%) of the girls. The subgroups "predominantly hyperactive-impulsive subtype" and "ADHD, not otherwise specified" were small (6 and 13 individuals, respectively). The mean ADHD-RS total score at baseline was 32.6 [CI 31.5 to 33.6] points. This score decreased to 16.3 [CI 15.1 to 17.5] points at week 8, and was 14.5 [CI 13.1 to 15.8] points at the end of week 24.
Pre-existing comorbid conditions were reported for 310 (73.6%) patients, the most frequent being psychiatric comorbidities, specifically conduct disorder (19.7%), oppositional defiant disorder (17.6%), enuresis (4.3%), tic disorder (2.4%), emotional disorder of childhood (2.6%), and depression (1.4%). Physical comorbidities that were reported at a rate of >2% were headache (5.7%), seasonal allergy (4.3%), asthma (3.3%), neurodermatitis (2.6%), acne (2.4%), upper respiratory tract infection (2.1%), and rhinitis (2.1%).
349 (82.9%) of the 421 patients had previously been treated for ADHD. The percentage was similar for the predominantly inattentive subtype (N = 101, 81.5%) and the combined subtype (N = 231, 83.1%). Medications most frequently used before study entry were short-acting methylphenidate (N = 290, 68.9%), long-acting methylphenidate (N = 196, 46.6%), amphetamines (N = 56, 13.3%), antipsychotic drugs (N = 12, 2.9%) and herbal/complementary therapies (N = 10, 2.4%). Commonly reported non-drug therapies prior to study were: occupational therapy (N = 48, 11.4%), "other" psychotherapy (N = 31, 7.4%), structured psychotherapy (N = 42, 10.0%), and remedial education (N = 10, 2.4%). The most frequent reason for discontinuation of previous therapy in patients with pre-treatment was inadequate response (N = 216, 61.9%). N = 68 patients (16.2%) discontinued previous therapy because of adverse events.
The mean atomoxetine dose given during the first week of treatment was 0.50 mg/kg per BW day (SD 0.07, range 0.40 – 0.80 mg/kg BW per day). Thereafter, the mean dose for the respective visit intervals ranged between 1.17 and 1.18 mg/kg per day (min. 0.40, max. 1.50 mg/kg per day). Compliance as defined above was present in 91.2% of all patients over the course of the entire study.
Concomitant medication was taken by 272 (64.6%) of the patients. Cough and cold remedies, analgesics, antibiotics and herbal/complementary medicines were given most frequently. Whilst continuous medication with any psychotropic compound other than the study medication led to discontinuation of the patient in the study, 3.8% (N = 16) of patients did receive a psychotropic medication at least once over the entire course of the 24-week study. The medication included compounds such as St. John's Wort, imipramine or a benzodiazepine. Concomitant behavioral therapy was given to 27 (6.4%) patients, and 20 (4.8%) patients received additional occupational therapy.
Results from ten items of the PAERS
The following ten items of the Pediatric Adverse Event Rating Scale (PAERS) were selected to investigate emotional well-being: "feeling withdrawn or numb" (item 8), "nervous, tense, or uptight" (item 16), "trying to hurt him or her self" (item 20), "feeling restless or keyed up" (item 26), "sad or low mood/unhappy" (item 32), "drowsy or 'out of it"' (item 37), "unusually good mood/super happy" (item 38), "not interested/no enthusiasm" (item 39), "angry or irritable/in a bad mood" (item 42), and "thinking about or wanting to hurt self" (item 43). Each of these items was rated from three perspectives (patient, parent, and physician) like all PAERS items. If present, the severity of the respective behavior or emotional state was rated on a 5 point Likert scale (0 = not present, 1 = mild, 2 = moderate, 3 = severe, and 4 = extreme).
The following five groups of items were identified, whose correlations were larger than 0.4 between items: (a) items relating to depressed mood (items 8, 32, and 39), (b) items relating to self-harm (items 20 and 43), (c) items relating to irritability/agitation (items 16, 26, and 42), (d) one item relating to drowsiness (item 37), and (e) one item relating to euphoria (item 38) (Table 2). The correlation of the various items in the five groups is shown in Table 3.
In general, the correlations were moderate to high only for parent and physician ratings, but not for patient ratings. The pattern of moderate to high correlations was similar between parent and physician ratings. In the sensitivity analyses using baseline ratings only (rather than all ratings), the correlations were generally lower, but confirmed the overall pattern of correlations based on the other points in time. A total score of all the items was not calculated as correlations were low between items that belonged to different groups (Table 2). These correlations are not reported here.
Items relating to depressed mood
Based on the confidence intervals at baseline, the parent ratings of the items "feeling withdrawn or numb" (item 8), "sad or low mood/unhappy" (item 32), and "not interested/no enthusiasm" (item 39), were significantly higher compared to both the patients and the physician ratings, which were similar. However, mean scores for all items were below 0.81 (Table 4). The scores for the items relating to depressed mood decreased over time. The mean change from baseline was statistically significant for all three items and all three perspectives both at week 8 and at week 24 (Table 4). Generally, there was a tendency for mean scores to decrease further the longer patients stayed on medication. Moreover, the decrease in scores was generally most pronounced in parent ratings, followed by patient and physician ratings.
Items relating to self-harm
The scores for the items relating to self-harm were extremely low at baseline and stayed low over time (Table 4). The scores were comparable in terms of the three perspectives. No significant changes were observed compared to baseline.
Items relating to irritability/agitation
At baseline, a similar pattern was observed for items "nervous, tense, or uptight" (item 16), "feeling restless or keyed up" (item 26), and "angry or irritable/in a bad mood" (item 42). Based on the confidence intervals, the parent rating was significantly higher than the physician rating, which was again significantly higher than the patient rating for all three items. The scores for the items relating to irritability/agitation decreased over time (Table 4). The decreases from baseline were largest for parents, followed by physicians and patients: the mean changes from baseline were statistically significant for all perspectives, all three items, and both at week 8 and week 24, as shown by non-overlapping confidence intervals.
Item relating to drowsiness
Based on the confidence intervals at baseline, the item "drowsy or 'out of it"' (item 37) was scored similarly by parents and patients, and significantly higher than by physicians. The scores for the item relating to drowsiness decreased over time (Table 4). Also the changes from baseline were more pronounced in parent and patient ratings than in physician ratings. The mean changes from baseline were statistically significant for all perspectives and both at week 8 and week 24, as shown by non-overlapping confidence intervals.
Item relating to euphoria
Based on the confidence intervals at baseline, the item "unusually good mood/super happy" (item 38) was scored significantly higher by patients than by parents, and significantly higher than by physicians. The scores for the item relating to euphoria decreased over time (Table 4). The changes from baseline were scored similarly by patients and physicians, but the decreases were smaller in the physician rating. The mean changes from baseline were statistically significant in terms of all three perspectives and were significant both at week 8 and week 24, as shown by non-overlapping confidence intervals.
Discussion
The aim of this post-hoc analysis was to evaluate the scores of the ten items of the Pediatric Adverse Event Rating Scale (PAERS) that were considered to be related to emotional well-being by face validity. Each of these ten items was rated from three perspectives: the patient, the parent, and the physician perspective. These perspectives were subsequently compared in terms of the height of scores and changes in the scores over time.
Emotional well-being as reflected by the scores on the respective ten items of the PAERS showed both similarities as well as differences both regarding the course of the scores over time and comparisons between the three perspectives (patient, parent, physician). Generally, scores for all items rated from all three perspectives decreased over the 24-week duration of the two studies. Thus, emotional well-being as reflected by the scores on the ten items of the PAERS was seen to improve during treatment with atomoxetine.
Correlations between parent and physician scores were generally higher than correlations between parent and patient scores as well as correlations between physician and patient scores. There were, however, distinct differences between the patterns observed for the five groups of items relating to depressed mood, self-harm, irritability/agitation, drowsiness, and euphoria.
For the items relating to depressed mood, parent ratings resulted in higher scores than either patient or physician ratings at baseline. This may be due to parents being particularly concerned about the emotional well-being of their children. Over time, however, there is a reduction in the scores for these items from all three rater perspectives. Obviously, all individuals concerned recognize an improvement in the emotional well-being of the patients over time. Surprisingly, both patient and physician ratings on the PAERS were similar, although children and adolescents seemed to dissimulate their difficulties or failed to perceive their difficulties correctly according to the Global Impression of Perceived Difficulties (GIPD), whilst physicians perceived the child's difficulties as being considerably greater [28, 29]. Mean changes for most items and ratings were approximately one third of a standard deviation (Table 4). This can be considered a moderate change, given the low scores at baseline.
For the items relating to self-harm, scores from all three perspectives were very low at baseline and did not change significantly whilst the child or adolescent is being treated with atomoxetine. Mean changes from baseline for these items and ratings were negligible. This finding is encouraging, because it suggests that attempts to self-harm or thoughts of self-harm are not aggravated by treatment with atomoxetine.
For the items relating to irritability/agitation, scores differed significantly depending on the rater. Whilst baseline scores rated by parents were the highest, baseline scores rated by patients were lowest, and baseline scores rated by physicians were in between. These findings may be due to the high impact that a child's irritability/agitation may have on the parents. The physician may be less likely to observe irritability/agitation than a parent might, and children or adolescents seemed to dissimulate their difficulties in these two studies [28, 29]. Mean changes for most items in this dimension and for physician and parent ratings were greater than one half of the standard deviation (Table 4). This is a considerable change. In contrast, the patient ratings for these items changed to a smaller degree. This finding may be a result of the lower patient-rated scores at baseline.
The scores for the item relating to drowsiness as rated by patients and parents were similar whilst the scores rated by the physicians differed from the scores rated either by the patients or the parents at baseline. Physician-rated baseline scores were lower, which may be due to the physicians not having as much opportunity to witness any drowsiness as parents may do. Patients can be expected to experience this well-known adverse event related to atomoxetine [36]. Mean changes for this item were just below one third of the standard deviation. This can be considered a moderate change, given the low scores at baseline.
The scores for the item relating to euphoria differed between all three perspectives (patient, parent, physician). Whilst patient ratings resulted in the highest scores for euphoria, the scores from physician ratings were the lowest and scores from parent ratings were in between. The greater euphoria experienced by the patients compared to the euphoria seen by the parents or physicians seems to correspond to the lower degree of ADHD-related difficulties perceived by patients compared to the parent or physician perspectives as measured by the GIPD in these two studies [28, 29]. The rating of euphoria by the parents may have resulted in scores that more objectively reflect the actual situation, whilst the physicians may not have had adequate opportunity to witness the euphoria before carrying out their rating. Mean changes for this item were approximately one third of the standard deviation. This can be considered a moderate change, given the low to moderate scores at baseline.
This study has several limitations. Most importantly, the study did not include a placebo control, so that the degree to which the results reflect drug-specific effects cannot be determined definitely. More specifically, placebo-controlled studies would be needed to distinguish direct medication effects on emotional well-being from indirect effects caused by improvement of core symptoms. Furthermore, the age-distribution of the sample does not reflect the age-distribution of individuals with ADHD in the general pediatric population. This is due to the fact that this analysis is based on two studies, one in children and one in adolescents. Whilst the age-distribution is normal within each of the two otherwise identical studies, the age-distribution of the combined samples is not quite normal, as it shows two peaks. Due to the open-label design, unspecific factors such as rater bias, expectation effects, and time effects cannot be ruled out. However, this does not automatically compromise the validity of the results [37]. Furthermore, although both mean symptom reduction and improvement in emotional well-being were considerable, the results do not allow direct comparison against changes of these parameters upon treatment with other ADHD medications. Treatment emergent adverse events occurring in the two studies on which this analysis is based have been reported and discussed elsewhere in more detail [28, 29]. For evaluating the adverse event profile, it needs to be taken into account that only those patients for whom the physician decided to continue atomoxetine treatment at week 8 were followed for additional 16 weeks until week 24.
Taken together, these findings could be expected, as cognition and the regulation of emotion are known to influence one another [38]. Furthermore, cognitive control of emotion involves frontal structures of the brain [39], areas of the brain that play an important role in the pathophysiology of ADHD [3]. Thus, any pharmacological treatment that is effective on the core symptoms of ADHD and executive functioning can also be expected to improve the emotional regulation and thus the emotional well-being of patients with ADHD. This hypothesis is supported by the findings from this secondary analysis. These findings appear particularly relevant in face of the important role that emotional regulation plays in children, adolescents, and adults with ADHD [4, 5, 39–43].
References
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Text Revision (DSM-IV-TR). 2000, Washington, DC: American Psychiatric Association, 4
Barkley RA: Major life activity and health outcomes associated with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2002, 10-15. Suppl 12
Biederman J, Faraone SV: Attention-deficit hyperactivity disorder. Lancet. 2005, 366: 237-248. 10.1016/S0140-6736(05)66915-2.
Maedgen JW, Carlson CL: Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. J Clin Child Psychol. 2000, 29: 30-42. 10.1207/S15374424jccp2901_4.
Martel MM, Nigg JT: Child ADHD and personality/temperament traits of reactive and effortful control, resiliency and emotionality. J Child Psychol Psychiatry. 2006, 47: 1175-1183. 10.1111/j.1469-7610.2006.01629.x.
Strine TW, Lesesne CA, Okoro CA, McGuire LC, Chapman DP, Balluz LS, Mokdad AH: Emotional and behavioral difficulties and impairments in everyday functioning among children with a history of attention-deficit/hyperactivity disorder. Public Health Res Practice and Policy. 2006, 3: 1-10.
Escobar R, Soutullo CA, Hervas A, Gastaminza X, Polavieja P, Gilaberte I: Worse quality of life for children with newly diagnosed attention-deficit/hyperactivity disorder, compared with asthmatic and healthy children. Pediatrics. 2005, 116: e364-e369. 10.1542/peds.2005-0386.
Harpin VA: The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2007, i2-i7. Suppl 1
Klassen AF, Miller A, Fine S: Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics. 2004, 114: e541-e547. 10.1542/peds.2004-0844.
Matza LS, Rentz AM, Secnik K, Swensen AR, Revicki DA, Michelson D, Spencer T, Newcorn JH, Kratochvil CJ: The link between health-related quality of life and clinical symptoms among children with attention-deficit hyperactivity disorder. J Dev Behav Pediatr. 2004, 25: 166-174. 10.1097/00004703-200406000-00005.
Riley AW, Spiel G, Coghill D, Döpfner M, Falissard B, Lorenzo MJ, Preuss U, Ralston SJ, ADORE Study Group: Factors related to Health-Related Quality of Life (HRQoL) among children with ADHD in Europe at entry into treatment. Eur Child Adolesc Psychiatry. 2006, i38-i45. 10.1007/s00787-006-1006-9. Suppl 1
Sawyer MG, Whaites L, Rey JM, Hazell PL, Graetz BW, Baghurst P: Health-related quality of life of children and adolescents with mental disorders. J Am Acad Child Adolesc Psychiatry. 2002, 41: 530-537. 10.1097/00004583-200205000-00010.
Jensen PS, Hinshaw SP, Swanson JM, Greenhill LL, Conners CK, Arnold LE, Abikoff HB, Elliott G, Hechtman L, Hoza B, March JS, Newcorn JH, Severe JB, Vitiello B, Wells K, Wigal T: Findings from the NIMH multimodal treatment study of ADHD (MTA): implications and applications for primary care providers. J Dev Behav Pediatr. 2001, 22 (1): 60-73.
Banaschewski T, Roessner V, Dittmann RW, Santosh PJ, Rothenberger A: Non-stimulant medications in the treatment of ADHD. Eur Child Adolesc Psychiatry. 2004, 102-116. Suppl 1
Becker K, Wehmeier PM, Schmidt MH: The Noradrenergic Transmitter System in ADHD: Principles and Implications for Treatment. 2006, Stuttgart: Thieme
Michelson D, Allen AJ, Busner J, Casat C, Dunn D, Kratochvil C, Newcorn J, Sallee FR, Sangal RB, Saylor K, West S, Kelsey D, Wernicke J, Trapp NJ, Harder D: Once-daily atomoxetine treatment for children and adolescents with attention deficit hyperactivity disorder: a randomized, placebo-controlled study. Am J Psychiatry. 2002, 159: 1896-1901. 10.1176/appi.ajp.159.11.1896.
Michelson D, Faries D, Wernicke J, Kelsey D, Kendrick K, Sallee R, Spencer T, Atomoxetine ADHD Study Group: Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, dose-response study. Pediatrics. 2001, 108: Ae83-e91. 10.1542/peds.108.5.e83.
Kelsey DK, Sumner CR, Casat CD, Coury DL, Quintana H, Saylor KE, Sutton VK, Gonzales J, Malcolm SK, Schuh KJ, Allen AJ: Once-daily atomoxetine treatment for children with attention-deficit/hyperactivity disorder, including an assessment of evening and morning behavior: a double-blind, placebo-controlled trial. Pediatrics. 2004, 114: e1-e8. 10.1542/peds.114.1.e1.
Spencer T, Heiligenstein JH, Biederman J, Faries DE, Kratochvil CJ, Conners CK, Potter WZ: Results from 2 proof-of-concept, placebo-controlled studies of atomoxetine in children with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2002, 63: 1140-1147.
Cheng JYW, Chen RYL, Ko JSN, Ng EML: Efficacy and safety of atomoxetine for attention-deficit/hyperactivity disorder in children and adolescents. Meta-analysis and meta-regression analysis. Psychopharmacology. 2007, 194 (2): 197-209. 10.1007/s00213-007-0840-x. published online, DOI 10.1007/s00213-007-0840-x
DuPaul GJ, Power TJ, Anastopoulos AD, Reid R: ADHD Rating Scale-IV: Checklists, Norms, and Clinical Interpretations. 1998, New York: Guilford
Faries DE, Yalcin I, Harder D, Heiligenstein JH: Validation of the ADHD Rating Scale as a clinician administered and scored instrument. J Atten Disord. 2001, 5: 39-47. 10.1177/108705470100500204.
Guy W: ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76–338. 1976, Washington, DC: US Department of Health, Education and Welfare, 218-222.
National Institutes of Mental Health (NIMH): Psychopharmacology Bulletin. 1985, 21: 839-943.
Landgraf J, Abetz L, Ware J: Child Health Questionnaire (CHQ): A Users Manual. 1996, Boston: Integrated Therapeutics Group
Riley AW, Robertson J, Forrest CB, Green B, Rebok G, Starfield B: Manual for the Child Health and Illness Profile-Child Edition (CHIP-CETM). 2001, Baltimore, MD: The Johns Hopkins University
Klassen AF, Miller A, Fine S: Agreement between parent and child report of quality of life in children with attention-deficit/hyperactivity disorder. Child Care Health Dev. 2006, 32: 397-406. 10.1111/j.1365-2214.2006.00609.x.
Dittmann RW, Wehmeier PM, Lehmann M, Schacht A, Helsberg K, Lehmkuhl G: Behandlung von ADHS bei Jugendlichen in Deutschland: Offene Studie zur Effektivität und Verträglichkeit von Atomoxetin aus Sicht von Arzt, Eltern und Patient. Nervenarzt. 2006, S300-suppl 3
Wehmeier PM, Dittmann RW, Schacht A, Minarzyk A, Lehmann M, Sevecke K, Lehmkuhl G: Effectiveness of atomoxetine in children with attention-deficit/hyperactivity disorder and quality of life as perceived by patients, parents and physicians in an open-label study. J Child Adolesc Psychopharmacol. 2007, 17: 813-829. 10.1089/cap.2007.0025.
March J, Karayal O, Chrisman A: CAPTN: The Pediatric Adverse Event Rating Scale. The Scientific Proceedings of the 2007 Annual Meeting of the American Academy of Child and Adolescent Psychiatr: 23–28 October 2007; Boston. Edited by: Novins DK, DeYoung. 2007, 241.
Vitiello B: Research in child and adolescent psychopharmacology: recent accomplishments and new challenges. Psychopharmacology. 2007, 191: 5-13. 10.1007/s00213-006-0414-3.
Greenhill LL, Vitiello B, Abikoff H, Levine J, March JS, Riddle MA, Capasso L, Cooper TB, Davies M, Fisher P, Findling RL, Fried J, Labellarte MJ, McCracken JT, McMahon D, Robinson J, Skrobala A, Scahill L, Veripatis E, Walkup JT, Zito JM: Developing methodologies for monitoring long-term safety of psychotropic medications in children: Report on the NIMH conference, September 25, 2000. J Am Acad Child Adolesc Psychiatry. 2003, 42: 651-655. 10.1097/01.CHI.0000046842.56865.EC.
Greenhill LL, Vitiello B, Fisher P, Levine J, Davies M, Abikoff H, Chrisman AK, Chuang S, Findling RL, March J, Scahill L, Walkup J, Riddle MA: Comparison of increasingly detailed eliciation methods for the assessment of adverse events in pediatric psychopharmacology. J Am Acad Child Adolesc Psychiatry. 2004, 43: 1488-1496. 10.1097/01.chi.0000142668.29191.13.
March J, Silva SG, Compton S, Anthony G, DeVeaugh-Geiss J, Califf R, Krishnan R: The Child and Adolescent Psychiatry Trials Network (CAPTN). J Am Acad Child Adolesc Psychiatry. 2004, 43: 515-518. 10.1097/00004583-200405000-00004.
Döpfner M, Lehmkuhl G: DISYPS-JK: Diagnostik-System für psychische Störungen im Kindes- und Jugendalter nach ICD-10 und DSM-IV. 2000, Bern: Verlag Hans Huber
Thomason C, Michelson D: Atomoxetine: treatment of attention deficit hyperactivity disorder: beyond stimulants. Drugs of Today. 2004, 40: 465-473. 10.1358/dot.2004.40.5.850493.
Concato J, Shah N, Horwitz RI: Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000, 342: 1887-1892. 10.1056/NEJM200006223422507.
Berger A, Kofman O, Livneh U, Henik A: Multidisciplinary perspectives on attention and the development of self-regulation. Progress in Neurobiology. 2007, 82: 256-286. 10.1016/j.pneurobio.2007.06.004.
Ochsner KN, Gross JJ: The cognitive control of emotion. Trends in Cogn Sciences. 2005, 9: 242-249. 10.1016/j.tics.2005.03.010.
Hinshaw SP: mpulsivity, emotion regulation, and developmental psychopathology: Specificity versus generality of linkages. Ann NY Acad Sci. 2003, 1008: I149-159. 10.1196/annals.1301.016.
Klimkeit I, Graham C, Lee P, Morling M, Russo D, Tonge B: Children should be seen and heard. Self-report of feelings and behavior in primary-school-age children with ADHD. Journal of Attention Disorders. 2006, 10: 181-191. 10.1177/1087054706289926.
Kratochvil CJ, Faries D, Vaughan B, Perwien A, Busner J, Saylor K, Kaplan S, Buermeyer C, Swindle R: Emotional expression during Attention-Deficit/Hyperactivity Disorders treatment: Initial assessment of treatment effects. J Child Adolesc Psychopharm. 2007, 17 (1): 51-62. 10.1089/cap.2006.0018.
Reimherr FW, Marchant BK, Strong RE, Hedges DW, Adler L, Spencer TJ, West SA, Soni P: Emotional dysregulation in adult ADHD and response to atomoxetine. Biol Psychiatry. 2005, 58: 125-131. 10.1016/j.biopsych.2005.04.040.
Acknowledgements
We wish to thank Ms. Karin Helsberg and Ms. Anette Minarzyk for their help in preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Research was funded by Lilly Deutschland GmbH, Bad Homburg, Germany. Peter M. Wehmeier, Ralf W. Dittmann and Alexander Schacht are full-time employees of Lilly Deutschland GmbH.
Authors' contributions
PMW, RWD, ML and AS developed the two clinical trials, SGS and JSM developed the PAERS scale, ML had the idea and AS developed the analyses for this manuscript. All authors participated in the interpretation of data, PMW and AS drafted the manuscript, RWD, SGS, ML and JSM revised it critically for important intellectual content. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Wehmeier, P.M., Schacht, A., Lehmann, M. et al. Emotional well-being in children and adolescents treated with atomoxetine for attention-deficit/hyperactivity disorder: Findings from a patient, parent and physician perspective using items from the pediatric adverse event rating scale (PAERS). Child Adolesc Psychiatry Ment Health 2, 11 (2008). https://doi.org/10.1186/1753-2000-2-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1753-2000-2-11