Abstract
Introduction
Unwanted contraception through prolonged retention of fetal bone is a rare cause of secondary infertility. It is usually associated with a history of abortion, either spontaneous or induced.
Case presentation
We describe a case of intrauterine retention of fetal bone diagnosed 8 years after the termination of a pregnancy. The patient had no complaints of pain, irregular vaginal bleeding or discharge. A hysteroscopy was performed and irregular structures were removed. These fragments were fetal bones, which probably functioned as an intrauterine contraceptive device. After removal of the fetal bone fragments the patient conceived spontaneously within 6 months.
Conclusion
This case report stresses the importance of taking a thorough history and evaluation of the endometrium by transvaginal ultrasound or hysteroscopy in women with secondary infertility.
Similar content being viewed by others
Introduction
Since 1973 over 38 million legal abortions have been performed in the USA. Approximately 90% of these abortions were performed on patients between 15 and 34 years of age [1].
All recent and large-scale studies show that legally performed abortions were extremely safe procedures with a lethal risk rate of 0 to 0.7 per 100,000. The overall early complication rate due to hemorrhage, uterine perforation or cervical injury is between 0.01% and 1.16% [2]. So far, definite conclusions cannot be made as to the impact of multiple induced abortions and reproductive problems. Complications due to previous abortions such as Asherman's syndrome may occur. Since 50% of abortions are performed on young patients, these women may develop future fertility problems caused by previous procedures.
We describe a rare cause of secondary infertility due to prolonged retention of intrauterine bone after a dilatation and curettage. A number of case reports have been published on the prolonged retention of fetal bones up to 23 years after an abortion, either spontaneous or induced [3]. Most patients complain of dysmenorrhea, dysfunctional uterine bleeding, pelvic pain, dyspareunia, vaginal discharge or spontaneous passage of fetal bones [4]. Cases are discovered by vaginal ultrasound examination [5, 6], hysterosalpingography [7] and, in particular, hysteroscopy [8]. In our case, the patient had no complaints other than secondary infertility.
Case presentation
A 32-year-old woman presented with secondary infertility, her only pregnancy being a termination 8 years previously at 12 weeks' gestation in Nigeria. Fertility work-up showed a regular menstrual cycle, with no biphasic temperature curve. The semen of the male partner was normospermic.
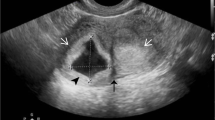
A transvaginal ultrasound revealed a normal-sized, normal-shaped uterus without myoma with an echogenic scarred endometrium (Figure 1). A laparoscopy showed no signs of pathology of the fallopian tubes or Fitz-Hugh-Curtis syndrome. During a hysteroscopy, an Asherman's syndrome was evident, which was treated with adhesiolysis and an intrauterine contraceptive device (IUCD) for a period of 3 months. After removal of the IUCD, a hysterosalpingogram showed no abnormalities (Figure 2).
The patient was treated with six cycles of clomiphene citrate which, despite ovulatory menstrual cycles, did not result in a pregnancy. Thereafter, three in vitro fertilization (IVF) cycles were performed in which qualitative perfect blastocysts were transferred without conception. The cause of this problem was thought to be malfunctioning endometrium. A second hysteroscopy was performed during which irregular structures, suspected to be bone fragments, were removed. Histopathological analysis confirmed that the structures contained five bone fragments (Figure 3). Two months later, a second hysteroscopy showed a normal empty uterine cavity with a normal endometrial lining.
Two months after the last hysteroscopy, while waiting for the IVF to commence, the patient became pregnant spontaneously with twins. Two healthy children were delivered. Two years later she delivered another healthy child.
Discussion
Every year many abortions are performed. Although abortion is an extremely safe procedure, complications do occur. This case illustrates a rare cause of secondary infertility due to the prolonged retention of fetal bones where the patient had no complaints of pain, irregular vaginal bleeding or discharge. Furthermore, this case shows fertility can be increased following removal of the fetal bones: within 6 months of the hysteroscopy and removal of the bone fragments, the patient became pregnant spontaneously. As in other case reports, this suggests that the presence of fetal bone in the uterine cavity may act as an IUCD [3–7]. In [3], a spontaneous pregnancy was possible following the removal of 15-year-old retained fetal bones.
The diagnosis of retained fetal bone can be made by identifying a filling defect on a hysterosalpingogram, an echogenic area on vaginal ultrasound or, as in our case, by direct visualization on hysteroscopy.
When the bone fragments are deeper in the endometrium they can be overlooked by hysteroscopy and the only indication may be an echogenic area in the endometrium on transvaginal ultrasound [5].
Conclusion
We recommend a transvaginal ultrasound or hysteroscopy on every patient with a history of secondary infertility following abortion, regardless of the interval between the preceding termination and presentation. Taking a thorough history is a prerequisite. A high success rate may be expected following the removal of any retained bones.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
- IUCD:
-
intrauterine contraceptive device
- IVF:
-
in vitro fertilization.
References
Strauss LT, Gamble SB, Parker WY, Cook DA, Zane SB, Hamdan S: Abortion surveillance – United States, 2003. MMWR Surveill Summ. 2006, 55: 1-32.
Soulat C, Gelly M: Immediate complications of surgical abortion. J Gynecol Obstet Biol Reprod (Paris). 2006, 35: 157-162.
Basu M, Mammen C, Owen E: Bony fragments in the uterus: an association with secondary subfertility. Ultrasound Obstet Gynecol. 2003, 22: 402-406. 10.1002/uog.221.
Graham O, Cheng LC, Parsons JH: The ultrasound diagnosis of retained foetal bones in West African patients complaining of infertility. BJOG. 2000, 107: 122-124. 10.1111/j.1471-0528.2000.tb11588.x.
Elford K, Claman P: Novel treatment of a patient with secondary infertility due to retained fetal bone. Fertil Steril. 2003, 79: 1028-1030. 10.1016/S0015-0282(02)04919-1.
Moon HS, Park YH, Kwon HY, Hong SH, Kim SK: Iatrogenic secondary infertility caused by residual intrauterine fetal bone after midtrimester abortion. Am J Obstet Gynecol. 1997, 176: 369-370. 10.1016/S0002-9378(97)70500-3.
Tulandi T, Sammour A: Retained fetal bones in the uterine cavity. J Am Assoc Gynecol Laparosc. 2001, 8: 179-180. 10.1016/S1074-3804(05)60574-9.
Makris N, Stefanidis K, Loutradis D, Anastasiadou K, Hatjipappas G, Antsaklis A: The incidence of retained fetal bone revealed in 2000 diagnostic hysteroscopies. JSLS. 2006, 10: 76-77.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
HMCK provided the background data and wrote the manuscript, JPTR provided the patient information, and was involved in drafting the manuscript and providing feedback on earlier drafts. Both authors approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kramer, H.M., Rhemrev, J.P. Secondary infertility caused by the retention of fetal bones after an abortion: a case report. J Med Case Reports 2, 208 (2008). https://doi.org/10.1186/1752-1947-2-208
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1752-1947-2-208