Abstract
Background
Pituitary apoplexy is a life-threatening endocrine emergency that is caused by haemorrhage or infarction of the pituitary gland, commonly within a pituitary adenoma. Patients classically present with headache, ophthalmoplegia, visual field defects and altered mental state, but may present with a typical symptoms such as fever and altered conscious level.
Case presentation
A 57-year-old female with a known pituitary macroadenoma was treated for suspected acute coronary syndrome with aspirin, clopidogrel and full dose enoxaparin. She developed a severe and sudden headache, nausea and vomiting and visual deterioration. A CT scan showed haemorrhage into the pituitary macroadenoma. She underwent neurosurgical decompression. Post-operatively her visual fields and acuity returned to baseline. She was continued on hydrocortisone and thyroxine replacement on discharge.
Conclusion
This case illustrates the risks of anticoagulation in a patient with a known pituitary macroadenoma, and raises the issue of whether these tumours present a relative contraindication to the use of dual antiplatelet and anticoagulation in acute coronary syndrome.
Similar content being viewed by others
Background
Pituitary apoplexy is defined as haemorrhage or infarction of the pituitary gland. This occurs often in the context of a pituitary adenoma, although it can occur in normal pituitaries in patients with post partum haemorrhage (Sheehan's syndrome) [1]. This is an emergency because of the combination of secondary adrenal insufficiency, with compression of the optic chiasm and the III, IV, V and VI cranial nerves [2].
The prevalence of classical pituitary apoplexy in retrospective case series of patients undergoing pituitary surgery varies from 5% [3] to 9.1% [4]. In patients with non-functioning macroadenomas, who were not operated on and followed up for 85 +/- 13 months, 14% developed pituitary apoplexy [5]. The majority present with no previous history of pituitary adenoma, and their tumour is discovered when the apoplexy occurs [6]. Many precipitating factors have been described, from dopamine agonists [7], anticoagulation [8], head trauma [9], pituitary irradiation [10], to dynamic endocrine testing, most likely triggered by TRH administration [11].
Case presentation
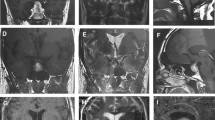
A 57-year-old menopausal female, during evaluation for headache, was incidentally found to have a 20 × 16 mm mixed solid and cystic pituitary mass abutting the optic chiasm on MRI scanning (Figure 1). Endocrine testing showed that she had normal pituitary hormone levels with the exception of gonadotrophin deficiency. Formal perimetry initially showed full visual fields. Within 12 months, however, she developed a mild superior bi-temporal hemianopia. Despite this, she elected not to have surgery.
Several months later, she was admitted to hospital with chest pain and treated for acute coronary syndrome with aspirin, clopidogrel and 1 mg/kg enoxaparin bd. She had no ECG changes suggestive of myocardial ischaemia or infarction. Her troponin level at 12 hours was undetectable. On the 2nd day of admission she developed a severe and sudden headache associated with nausea and vomiting. At this stage, her blood pressure was 144/85 mmHg and there were no neuro-ophthalmological symptoms or signs. The next day her symptoms continued and she noticed a constriction in her visual fields. She was febrile with an elevated C-reactive protein of 155 mg/l (normal < 5 mg/l). An ECG showed a new finding of global ST depression, but without chest pain (Figure 2).
Perimetry confirmed deterioration in the patient's visual fields and acuities (Figure 3), and a CT scan showed haemorrhage into the pituitary macroadenoma (Figure 4). She was given intramuscular hydrocortisone, and underwent urgent trans-sphenoidal surgery and decompression of the apoplectic pituitary.
Visual field tests before and after pituitary surgery. The results of visual field testing are shown. The upper set, taken before the operation, demonstrate a temporal hemianopia in the left eye field and closure of three quadrants in the right eye field, sparing the inferior nasal quadrant. The lower set demonstrates the improved visual fields after surgery.
Post-operatively her visual fields and acuity returned to baseline (Figure 3). Her pyrexia ceased and CRP decreased. The ECG returned to normal. Cardiological investigations including exercise stress testing and a myocardial perfusion scan did not show evidence of ischaemic heart disease, implying that the global ST depression noted pre-operatively was the result of her pituitary apoplexy. She was discharged home on hydrocortisone and thyroxine replacement.
Discussion
We describe a case of pituitary apoplexy in a patient who was already known to have a pituitary adenoma, and who was treated for acute coronary syndrome. With the modern treatment of acute coronary syndrome, an anticoagulation cocktail that includes aspirin, heparin and clopidogrel is employed. The addition of clopidogrel to aspirin and heparin has been demonstrated to reduce the incidence of further vascular events over aspirin and heparin alone. However, this is at the expense of a significant increase in rates of major bleeding (mainly gastrointestinal) from 2.7% to 3.7% [12]. The apoplectic crisis initially presented with fever, headache, nausea, and vomiting, and ST segment depression on ECG, a finding that has been reported with subarachnoid haemorrhage [13], but has not previously been reported in association with pituitary apoplexy. The risks of death or serious visual loss in the event of apoplexy are considerable, especially if there is diagnostic delay occasioned by a non-classical presentation, e.g. with fever of unknown origin, hyponatraemia and altered consciousness [6]. This situation can be compounded by non-diagnostic investigations such as non-specific changes in the CSF [14], or an apparently normal CT scan of the brain, which has been shown to be of lower sensitivity in detecting pituitary apoplexy compared to MRI scanning [15].
Conclusion
Anticoagulation is well known as a precipitating factor for pituitary apoplexy. Like our patient, one case study has reported a patient with pituitary apoplexy precipitated by aspirin, clopidogrel and enoxaparin, although in that case the patient did not have a previously known pituitary adenoma [16]. Our case therefore highlights some important practice points: in patients who are already known to have a pituitary adenoma, this condition should be considered a relative contraindication for anticoagulation. These patients should be warned about the potential risks of anticoagulation with respect to their pituitary adenoma. If these patients are anticoagulated, a high index of suspicion of pituitary apoplexy should guide the clinician if they fall acutely ill: early hydrocortisone replacement should be instituted.
References
Asa SL: Pituitary histopathology in man: normal and abnormal. Endotext.com: Pituitary Disease and Neuroendocrinology. Edited by: DeGroot LJ, Grossman AB. 2002, South Dartmouth, MA, USA: MDText.com, Inc
Cardoso ER, Peterson EW: Pituitary apoplexy: a review. Neurosurgery. 1984, 14: 363-373. 10.1097/00006123-198403000-00021.
Bonicki W, Kasperlik-Zaluska A, Koszewski W, Zgliczynski W, Wislawski J: Pituitary apoplexy: endocrine, surgical and oncological emergency. Incidence, clinical course and treatment with reference to 799 cases of pituitary adenomas. Acta Neurochir (Wien). 1993, 120: 118-122. 10.1007/BF02112028.
Wakai S, Fukushima T, Teramoto A, Sano K: Pituitary apoplexy: its incidence and clinical significance. J Neurosurg. 1981, 55: 187-193.
Dekkers OM, Hammer S, de Keizer RJ, Roelfsema F, Schutte PJ, Smit JW, Romijn JA, Pereira AM: The natural course of non-functioning pituitary macroadenomas. Eur J Endocrinol. 2007, 156: 217-224. 10.1530/eje.1.02334.
Sibal L, Ball SG, Connolly V, James RA, Kane P, Kelly WF, Kendall-Taylor P, Mathias D, Perros P, Quinton R, Vaidya B: Pituitary apoplexy: a review of clinical presentation, management and outcome in 45 cases. Pituitary. 2004, 7: 157-163. 10.1007/s11102-005-1050-3.
Yamaji T, Ishibashi M, Kosaka K, Fukushima T, Hori T, Manaka S, Sano K: Pituitary apoplexy in acromegaly during bromocriptine therapy. Acta Endocrinol (Copenh). 1981, 98: 171-177.
Oo MM, Krishna AY, Bonavita GJ, Rutecki GW: Heparin therapy for myocardial infarction: an unusual trigger for pituitary apoplexy. Am J Med Sci. 1997, 314: 351-353. 10.1097/00000441-199711000-00016.
Holness RO, Ogundimu FA, Langille RA: Pituitary apoplexy following closed head trauma. Case report. J Neurosurg. 1983, 59: 677-679.
Weisberg LA: Pituitary apoplexy. Association of degenerative change in pituitary adenoma with radiotherapy and detection by cerebral computed tomography. Am J Med. 1977, 63: 109-115. 10.1016/0002-9343(77)90122-X.
Masago A, Ueda Y, Kanai H, Nagai H, Umemura S: Pituitary apoplexy after pituitary function test: a report of two cases and review of the literature. Surg Neurol. 1995, 43: 158-64. 10.1016/0090-3019(95)80128-4. discussion 165
Peters RJ, Mehta SR, Fox KA, Zhao F, Lewis BS, Kopecky SL, Diaz R, Commerford PJ, Valentin V, Yusuf S: Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation. 2003, 108: 1682-1687. 10.1161/01.CIR.0000091201.39590.CB.
Kawasaki T, Azuma A, Sawada T, Sugihara H, Kuribayashi T, Satoh M, Shimizu Y, Nakagawa M: Electrocardiographic score as a predictor of mortality after subarachnoid hemorrhage. Circ J. 2002, 66: 567-570. 10.1253/circj.66.567.
Embil JM, Kramer M, Kinnear S, Light RB: A blinding headache. Lancet. 1997, 350: 182-10.1016/S0140-6736(97)05112-X.
Randeva HS, Schoebel J, Byrne J, Esiri M, Adams CB, Wass JA: Classical pituitary apoplexy: clinical features, management and outcome. Clin Endocrinol (Oxf). 1999, 51: 181-188. 10.1046/j.1365-2265.1999.00754.x.
Nagarajan DV, Bird D, Papouchado M: Pituitary apoplexy following anticoagulation for acute coronary syndrome. Heart. 2003, 89: 10-10.1136/heart.89.1.10.
Acknowledgements
Written consent has been obtained from the patient described in this case report.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
All authors participated in the care of the patient described. TMMT drafted the manuscript. CC, ECIH, NMM, KM critically revised the content of the manuscript. All authors have read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Tan, T.M., Caputo, C., Mehta, A. et al. Pituitary macroadenomas: are combination antiplatelet and anticoagulant therapy contraindicated? A case report. J Med Case Reports 1, 74 (2007). https://doi.org/10.1186/1752-1947-1-74
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1752-1947-1-74