Abstract
A case of Renal Cell Carcinoma (RCC) presenting to the Emergency Department with pyrexia and rigors is discussed.
Similar content being viewed by others
Case presentation
A 61 year old female patient presented to the Emergency Department with feeling unwell, pyrexia, nausea and headache. She gave a history of fever for the past three weeks with three episodes of rigors. She also gave a history of recent loss of appetite and some weight loss. She had no urinary problems.
On examination she looked pale. A mass was palpable in the right lower quadrant and lumbar region. Liver and spleen were not palpable. There were no signs of peritonitis.
Her pulse rate was 125/minute, BP 120/85 and temp 39.6 degree Centigrade. She had blood tests in the Emergency Department which revealed the following : Hb 12.0 g/dL, WCC 11.6 × 10(9)/litre and Platelets 237 × 10(9)/litre. Electrolytes and urea were as follows: Na 133 mmol/litre, K+ 4.2 mmol/litre, Urea 5.1 mmol/litre and Creatinine 78 micromol/litre. Chest X ray did not reveal any abnormality.
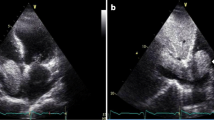
The patient had Ultrasound Scan which showed mass in the right Kidney (Figure 1). Her subsequent CT scan as shown (figure 2) revealed a mass in her right kidney.
She underwent right sided nephrectomy after full staging procedures and appropriate investigations.
Discussion
Malignant neoplasms involving the kidney may be primary or secondary tumors. Although metastatic lesions outnumber primary tumors, secondary renal neoplasms are usually clinically insignificant and are principally discovered at postmortem examination.
Patients with Renal cell carcinoma (RCC) present with a range of symptoms, but many are asymptomatic until the disease is advanced. At presentation, approximately 25 percent of individuals either have distant metastases or significant local-regional disease. Other patients, even some with only localized disease, present with a wide array of symptoms and/or laboratory abnormalities. Because of this unusual characteristic, RCC has been labelled the "internist's tumor"[1]. Today, most tumors are diagnosed incidentally [5, 6].
The classic triad of flank pain, hematuria and flank mass is uncommon (10% cases) and is indicative of advanced disease. The frequency with which Renal Cell Carcinoma clinically presents is shown in table 1[2]. The literature has described several unique clinical presentations of Renal Cell Carcinoma in the form of hoarseness or calverial metastasis of which only five cases have been reported [3, 4].
Renal cell carcinoma represents a heterogenous group of tumors, the most common of which is clear cell adenocarcinoma. RCC accounts for 3% of adult tumors. The incidence has increased more than 30% over the past two decades. It is generally accepted that the increased incidence rates reflect earlier diagnosis at an earlier stage, largely due to more liberal use of radiological imaging techniques. However advanced disease has also been diagnosed more frequently and mortality has increased as well [5].
Symptomatic presentation correlates with aggressive histology and advanced disease. Incidental tumours may be frequently detected in female and elderly patients, as these groups traditionally seek general medical care more regularly. The mode of presentation can independently predict an adverse patient outcome. Indicators of symptomatic presentations include flank pain, flank mass, varicocele, constitutional symptoms, paraneoplastic syndromes and bone pain related to metastatic disease [7].
Ultrasound scan was found to be useful screening test, but CT is the imaging study of choice to identify malignant features. MRI can be used in equivocal cases [7].
Pre-operative clinical variables may be used instead of the pathologic stage to determine the risk of recurrence [8].
Conclusion
Renal cell carcinoma presents with various clinical features. Atypical presentations of RCC should be considered for patients presenting with pyrexia of unknown origin.
References
Gaetani Paolo, Dilene Antonio, Colombo Piergiuseppe: Calverial metastasis as clinical presentation of Renal Cell Carcinoma- a report of two cases and review of literature. Clinical Neurology and Neurosurgery. 2005, 107: 329-333. 10.1016/j.clineuro.2004.07.017.
Greenberg Richard, Cooper Jeffrey, Knigel Robert: Hoarseness, A unique clinical presentation of Renal cell Carcinoma. Urology. 1992, 40: 159-161. 10.1016/0090-4295(92)90518-2.
Kirkali Ziya, Obec Can: Clinical aspects of Renal Cell Carcinoma. EAU Update Series. 2003, 1: 89-196. 10.1016/S1570-9124(03)00056-4.
Luciani Lorezo, Castari Roberto, Tallarigo Carlo: Incidental Renal Cell Carcinoma- age and stage characterization and clinical implications; a study of 1092 patients (1982–1997). Urology. 2000, 56: 58-63. 10.1016/S0090-4295(00)00534-3.
Lee Cheryl, Katz Jared, Fearn Paul, Russo Paul: Mode of presentation of Renal Cell Carcinoma- provides prognostic information. Urologic Oncology. 2000, 7: 135-140. 10.1016/S1078-1439(01)00185-5.
Nassir Anmar, Jollimore Jason, Gupta Rekha, Bell David, Norman Richard: Multilocular cystic Renal Cell Carcinoma; a series of 12 cases and a review of literature. Urology. 2002, 60: 421-427. 10.1016/S0090-4295(02)01742-9.
Yaycioghi Ozgur, Roberts William, Chan Theresa: Prognostic assessment non metastatic Renal Cell Carcinoma – a clinically based model. Urology. 2001, 58: 141-145. 10.1016/S0090-4295(01)01207-9.
Vincenzo F, Tommaso P, Giovanni N: Incidental detection beyond pathological factors as prognostic predictor of Renal Cell Carcinoma. European Urology. 2003, 43: 663-669.
Acknowledgements
Written consent was obtained from the patient for publication of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
DD wrote the first draft of the manuscript and scanned photographs for submission. MS proofread the case report and obtained patient consent. NS performed the literature search.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Doshi, D., Saab, M. & Singh, N. Atypical presentation of renal cell carcinoma: a case report. J Med Case Reports 1, 26 (2007). https://doi.org/10.1186/1752-1947-1-26
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1752-1947-1-26