Abstract
Background
India and Pakistan have disputed ownership of the Kashmir Valley region for many years, resulting in high levels of exposure to violence among the civilian population of Kashmir (India). A survey was done as part of routine programme evaluation to assess confrontation with violence and its consequences on mental health, health service usage, and socio-economic functioning.
Methods
We undertook a two-stage cluster household survey in two districts of Kashmir (India) using questionnaires adapted from other conflict areas. Analysis was stratified for gender.
Results
Over one-third of respondents (n = 510) were found to have symptoms of psychological distress (33.3%, CI: 28.3–38.4); women scoring significantly higher (OR 2.5; CI: 1.7–3.6). A third of respondents had contemplated suicide (33.3%, CI: 28.3–38.4). Feelings of insecurity were associated with higher levels of psychological distress for both genders (males: OR 2.4, CI: 1.3–4.4; females: OR 1.9, CI: 1.1–3.3). Among males, violation of modesty, (OR 3.3, CI: 1.6–6.8), forced displacement, (OR 3.5, CI: 1.7–7.1), and physical disability resulting from violence (OR 2.7, CI: 1.2–5.9) were associated with greater levels of psychological distress; for women, risk factors for psychological distress included dependency on others for daily living (OR 2.4, CI: 1.3–4.8), the witnessing of killing (OR 1.9, CI: 1.1–3.4), and torture (OR 2.1, CI: 1.2–3.7). Self-rated poor health (male: OR 4.4, CI: 2.4–8.1; female: OR 3.4, CI: 2.0–5.8) and being unable to work (male: OR 6.7, CI: 3.5–13.0; female: OR 2.6, CI: 1.5–4.4) were associated with mental distress.
Conclusion
The ongoing conflict exacts a huge toll on the communities' mental well-being. We found high levels of psychological distress that impacts on daily life and places a burden on the health system. Ongoing feelings of personal vulnerability (not feeling safe) was associated with high levels of psychological distress. Community mental health programmes should be considered as a way reduce the pressure on the health system and improve socio-economic functioning of those suffering from mental health problems.
Similar content being viewed by others
Background
The Partition of India in 1947 was the start of a long history of dispute between India and Pakistan for control of Kashmir, which today remains divided into three parts governed by India, Pakistan and China. Over the last 20 years, a liberation struggle between India and Kashmiri militants has led to at least 20,000 deaths and 4,000 disappearances in the Indian part of Kashmir [1].
A community survey done by Médecins Sans Frontières in 2005 found high levels of ongoing violence across the region, with civilians caught in the middle. The majority of people surveyed stated having been exposed to crossfire (86%) and round-up raids (83%). High numbers of people reported being subjected to maltreatment (44%), forced labour (33%), kidnapping (17%), torture (13%) and sexual violence (12%). [2]
Exposure to violence has potentially important implications for mental health [3]. This paper presents the findings of the community assessment survey done by Médecins Sans Frontières in 2005. The study, which was done to inform program planning, assessed the mental health and socio-economic impact of the ongoing violence, and the sources of support.
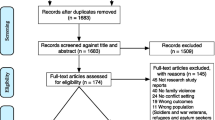
Methods
The survey was conducted in mid-2005 in the Indian part of Kashmir (Kupwara and Badgam, totalling 101 villages and a combined population 145,000 people). The methodology is described in detail elsewhere [2]. Briefly, sample size calculation assumed a prevalence of trauma-related psychological problems of 20% [4]; using a precision of 5% (confidence interval 95%) and a design effect of 2, the minimum sample size was estimated at 492. A two-stage cluster sampling design was used to cover 30 villages (randomly selected), resulted in 17 households per village. Within the household participants aged ≥ 18 years were selected randomly. Informed consent was attained for all participants and MSF's independent Ethical Review Board granted ethical approval.
Instruments
The overall survey questionnaire assessed baseline demographics, confrontation with violence (results presented elsewhere [2]), mental health, health service usage, socio-economic functioning and sources of support. Mental health was assessed using a Self-Reporting Questionnaire (SRQ), with a reference period of 30 days preceding the survey. The SRQ is an instrument developed by the World Health Organization (WHO) to measure general psychological distress, especially in developing countries. It has good validity and reliability for adults (≥ 15 years) [5], and can be used both as a self- or interviewer-administrated questionnaire. It consists of 20 closed questions covering expression of distress, the total score corresponding to the sum of positive responses. Various studies have validated the use of the SRQ in India [6–9]. Currently a cut off score of 11 or 12 is accepted [10] although this has been critiqued as being too high [11]. In our study we used a conservative cut-off score of 12, meaning those respondents scoring ≥ 12 are considered to be suffering from psychological distress.
Four categories of closed questions were applied to establish use of health services (categories: never; once; 2–3 times; 4+) and medications (Categories: never; 1–3 times; 4–6 times; 7+). Closed questions were also used to assess coping mechanisms for dealing with stress. The composition of categories for 'consequences of violence' and 'sources of support' was done with input from national staff.
To establish individual socio-economic functioning in relation to health during the past thirty days the H-section of the WHO-Disability Assessment Schedule-II (WHO-DAS-II) was used. This tool has good internal, convergent validity and good sensitivity for change [12].
The survey was forwarded and back translated from English to Urdu and phonetic Kashmiri and piloted prior to full implementation.
Analysis
Data entry was standardised and checked by supervisors, entered into EXCEL and analysed in EPIINFO-2002. Because males and females differed significantly in the number of confrontations with violence [2], we used univariate analysis to stratify for gender to determine relationships between psychological distress (SRQ ≥ 12) and demographic details, living circumstances, confrontations with violence (witnessing, self-experiencing), health outcomes (physical symptoms, health service use), and socio-economic functioning. We excluded variables such as 'torture while being detained/held hostage' as these responses relate to a sub-sample of those surveyed. We also excluded exposure to violence from this analysis because the proximity to the violence was not defined in detail.
A multivariate statistical model was constructed to investigate relationships between mental health (SRQ ≥ 12) and the above-mentioned variables. We used a logistic regression model including variables that were significant in the univariate analysis (p < 0.05) with backward elimination. In our model we expected each type of event conferring an additional risk over and above any other event experienced. This is in accordance with studies reporting exposure to cumulative traumatic events as a risk factor for the development of PTSD [13, 14].
Results
510 of 548 (93%) interviews were completed. Reasons for refusal to participate (25) and stopping the interview (13) included: lack of time, distrust, and being emotionally upset. The average age of respondents was 37.7 years (range 17–90) with an equal gender distribution (males = 53%; 270; p > 0.05). Demographics are described in detail elsewhere. [2]
Mental health status
Psychological distress was mostly expressed through symptoms such as nervousness, tiredness, being easily frightened and headache (Table 1). The prevalence of suicidal ideation is striking: one-third of those surveyed had had thoughts of ending their life in the past 30 days. Over a third of respondents were categorized as suffering from psychological distress (SRQ ≥ 12) using the Indian validated SRQ (33.3%, 170; CI: 28.3–38.4). The design effect for the SRQ was 1.4. Females scored significantly higher (43.8% vs. 24.1%, OR 2.5; CI: 1.7–3.6; p < 0.001).
Associations between psychological distress (SRQ ≥ 12) and violence, health, socio-economic and sources of support
Univariate analysis of violence and psychological distress (SRQ ≥ 12)
Feelings of personal insecurity were significantly associated with psychological distress (SRQ ≥ 12) for both males and females (Table 2). Psychological distress among males was significantly (p < 0.01) associated with all self-experiences (defined as 'ever happened to you') and most consequences of violence. Psychological distress among females was significantly (p < 0.01) associated with witnessing events (except hearing about/witnessing rape), as well as the self-experience of some events (maltreatment, arrested/kidnapped) and feelings of lack of safety and independence.
Multivariate analysis of mental health (SRQ ≥ 12) and violence
For both genders, not feeling safe is associated with at least twice the odds of suffering from psychological distress (Table 3). For males, violation of modesty, forced displacement, and disability were all associated with a significantly increased likelihood (three times the odds) of suffering from psychological distress. For women, the witnessing of people being killed or tortured or dependency on outside assistance doubled the odds of suffering psychological distress.
Associations between psychological distress (SRQ ≥ 12), health and socio economic outcomes
The majority of respondents (63.9%, 326) had recently visited a health postor clinic: nearly half had visited a health facility more than once (46.3%, 235) in the past 30 days. Overall, nearly half (49.6%, 253) of respondents rated the health facilities as poor. Women more frequently rated their physical health as bad or very bad (male: 24.1% vs. female: 36.3%, OR 1.8; CI: 1.2–2.6; p < 0.005), and visited the health facilities more than men (male: 40.0% vs. female: 54.7%, OR 1.8; CI: 1.3–2.6; p = 0.005). The number of women who had been on medication for six or more days was significantly higher than men (male: 30.7% vs. female: 46.0%, OR 1.9; CI: 1.3–2.8; p < 0.001). A high level of psychological distress (SRQ ≥ 12) was significantly (p < 0.01) associated with poor or very poor self-rated health for both males (OR 4.4) and females (OR 3.4). For males this was also associated with a higher likelihood of visiting the clinic two times or more (Table 4). For both males and females, high psychological distress was also associated with a higher likelihood of being unable to or having to cut back on work or performance of daily activities.
Coping mechanisms
The most common ways of coping were withdrawal (isolation, not talking to people) and aggression (Table 5). Religion was also reported as a helpful source of support.
Discussion
The data presented in this article were gathered to inform MSF's programme to provide mental health support in Kashmir. Using the SRQ (a tool that has been validated in other Indian studies [6–10]) we found the population had been exposed to high levels of violence [2] which resulted in one third of the respondents suffering from psychological distress and considering suicide. For both genders, currently not feeling safe was associated with psychological distress. For males 'violation of modesty', displacement, and disability were associated with psychological distress while risk factors for females included witnessing killing and torture. Respondents with high psychological distress rated their own health and socio economic functioning as poor. The most common coping mechanism was withdrawal.
Overall, one-third of respondents reported psychological distress. This compares to a prevalence of 36% found in a study done in among Afghan women in a refugee camp [15] using the same instrument and similar cutoff score, but differs substantially from another SRQ study done in a non-conflict area in India [16] where 18% prevalence of psychological distress was found among low-income urban women, using a relatively low cut-off score (7/8). (Using this lower cut-off would have given a prevalence of psychological distress of 71.4%). The contextual difference in these studies – exposure to chronic violence as compared to 'common' stressors of daily life for women in low urban settings – may account for this difference.
The Self Reporting Questionnaire (SRQ) showed that a third of respondents had contemplated suicide. Suicidal thoughts are common for depressive disorders [17] but do not always lead to a suicide attempt. Our findings are in line with a previous study that reported high suicide rates in this region [18]. A high prevalence of suicidal thoughts is more often reported among populations suffering from chronic violence, with a similar prevalence (33%, 96, n = 297) reported in a population of Afghan refugee women in Pakistan using the same questionnaire (SRQ).
In our study women had significantly higher psychological distress than man. This is in line with other studies showing women suffering more from anxiety disorders than men after confrontation with violence [20]. Feeling safe was found in other studies to be an important pre-condition for being able to deal with adverse traumatic experiences [21, 22], and this was also found in our study.
For males, the most important risk factors for developing psychological distress were 'violation of modesty', displacement and disability. It is possible that these experiences are the most distressing because they interfere with the cultural values and roles of males in Kashmir society: upholding their dignity and being able to protect and feed their families. Those who self-experienced 'violation of modesty' had a threefold chance of suffering from psychological distress (p = 0.001). 'Violation of modesty' is regarded as very degrading and in the few studies on male sexual violence is associated with multiple perpetrators and high levels of physical beating [23, 24], which can further contribute to psychological distress.
For women most psychological distress was associated with feelings of powerlessness – dependency on others for daily living, and witnessing killing and torture. Women have lower confrontations with violence, which can be partly explained by their being largely confined to the home [2]. The significant association of witnessing and psychological distress among females may relate to feelings of helplessness and guilt caused by the witnessing may be more traumatic than experiencing the violence themselves.
Both males and females with high levels of psychological distress rated their own health as much poorer compared to those who did not have high levels of psychological distress (male: OR 4.4; female: OR 3.4). Non-specific health complaints have been associated with (traumatic) stress in other studies [25–27]. It is also possible that people do not understand the relationship between physical symptoms and mental stress [28] or have difficulty to articulate their emotional status and use physical symptoms to articulate mental distress [29].
High psychological distress among males was significantly associated with visiting health services more frequently. Increased use of medical services by those suffering from traumatic-stress related problems are common [30, 31], with up to a 25% increase in number of visits to health care facilities reported in other studies [32–34]. We found this relationship in our survey for males, but not for females. This may be explained by the fact that for both cultural and security reasons females depend on male escorts in order to access health services, restricting their movements.
In our population, high psychological distress is associated with substantially increased likelihood of socio-economic dysfunction, and this has been reported in both Western [35, 36] and Asian [15] contexts. Socio-economic dysfunction can have broad implications, for example by reducing capacity of females to give care to the children or for males to generate income (according to traditional roles).
The most common coping mechanisms such as withdrawal (self-isolation, stop speaking) and aggression may also be symptomatic of depression and/or anxiety disorder (including post-traumatic stress disorder, PTSD). Religion and family assistance are mentioned less frequently as sources of support. This is in contrast to a study conducted in Afghanistan that showed religion and reading the Koran as the two main coping mechanisms for two being confronted with violence [15].
Potential limitations
General methodological limitations, including sampling methodology, retrospective study design, and terminology, have been discussed previously [2]. There are, in addition, a number of potential limitations related to this specific analysis. First, as this is a cross-sectional survey, no causal inferences between violence and mental health can be conclusively made. Second, individual respondents may have implicitly used the presence of mental health symptoms as a deciding factor for whether they have experienced a traumatic event in case of doubt (i.e. recall bias [37]). We consider this as unlikely as we asked respondents to recall violent events but did not ask them to identify which events were traumatic. Finally, we used the SRQ to avoid labelling populations with a psychiatric diagnosis, but using a self-reporting questionnaire has obvious limitations. A comparative study in India of five questionnaires showed good internal consistency and a high discriminating ability with the SRQ having the best results [9], but in comparison to clinical interview, questionnaires only showed strong positive predictive value when a considerable compromise on sensitivity was made. It was concluded that the choice of an optimum cut-off score (to balance sensitivity and positive predictive value) should be adapted to individual settings, and recommend a higher cut-off score for resource-limited primary-care settings [9]. We used a high cut off score of 12, in line with this recommendation. But in the absence of clinical interview no detailed analysis of the mental health status is possible.
In the context of predominantly Urdu speaking population we considered, but did not use, cut off scores from other Urdu speaking cultures such as in Pakistan. A meta-analysis of psychiatric rating scales in Urdu [38] concluded that only a small number of instruments (including SRQ) were sufficiently evaluated. The same review concluded that for the SRQ no cross-culturally validated gold standard was used, cut-offs varied considerably, as did sensitivity (78–93%) and specificity (77–85%). We consider the Indian validation studies [9] as more appropriate because they used clinical interview as gold standard.
Conclusion
The high levels of violence confronted by the Kashmiri population have resulted in high prevalence (33%) of mental health problems. Poor self-rated health and likelihood of poor socio-economic functioning were associated with high levels of psychological distress. Mental health problems in this context of chronic violence should receive full attention through the provision of appropriate community-based services that would improve access to care and reduce the burden on the health system.
Conflicts of interests
The authors declare that they have no competing interests.
References
The Official Site of the Government of Jammu & Kashmir. [http://jammukashmir.nic.in]
de Jong K, Ford N, van de Kam S, Lokuge K, Fromm S, van Galen R, Reilley B, Kleber R: Conflict in the Indian Kashmir Valley I: Exposure to Violence. Confl Health. 2008, 2 (1): 10.
de Jong J, Komproe IH, van Ommeren M, El Masri M, Araya M, Khaled N, Put van der W, Somasundram D: Lifetime events and posttraumatic stress disorder in 4 post conflicts settings. JAMA. 2001, 86: 555-562. 10.1001/jama.286.5.555.
Kleber RJ, Brom D: Coping with trauma. Theory, prevention and treatment. 1992, Lisse: Swets & Zeitlinger
World Health Organization: User's Guide to the Self Reporting Questionnaire. World Health Organization, Division of Mental Health. 1994, Geneva: WHO/MNH/PSF/94.8, Division of Mental Health
Harding TW, De Arango MV, Baltazar J, Climent CE, Ibrahim HH, Ladrido-Ignacio L, Murthy RS, Wig NN: Mental disorders in primary health care: a study in their frequency and diagnosis in four developing countries. Psychological Medicine. 1980, 10: 231-241.
Kishore J, Reddaiah V, Kapoor V, Gil J: Characteristics of mental morbidity in a rural primary health centre of Haryana. Indian Journal Psychiatry. 1996, 38: 137-42.
Mumford DB, Saeed K, Ahmad I, Akhter S, Mubbashar MH: Stress and psychiatric disorder in rural Punjab. A community survey. Brit J Psychiatry. 1997, 170: 473-8. 10.1192/bjp.170.5.473.
Patel V, Araya R, Chowdhary N, King M, Kirkwood B, Nayak S, Simon G, Weiss H: Detecting common mental disorders in primary care in India: a comparison of five screening questionnaires. Psychol Med. 2008, 38 (2): 221-228. 10.1017/S0033291707002334.
Sen B, Williams P: The extent and nature of depressive phenomena in primary health care: A study in Calcutta, India. Brit J Psychiatry. 1987, 151: 486-93. 10.1192/bjp.151.4.486.
Deshpande SN, Sundaram R: Psychiatric disorders among medical in-patients in an Indian hospital. Brit J Psychiatry. 1989, 154: 504-509. 10.1192/bjp.154.4.504.
Chwastiak L, Vonkroff M: Disability in depression and back pain: Evaluation of the WHO Disability Assessment Schedule (WHO DAS II) in a primary care setting. J Clin Epidemiol. 2003, 56: 507-514. 10.1016/S0895-4356(03)00051-9.
Breslau N, Chilcoat HD, Kessler RC, Davis GC: Previous Exposure to Trauma and PTSD Effects of Subsequent Trauma: Results From the Detroit Area Survey of Trauma. Am J Psychiatry. 1999, 156: 902-907.
Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P, Stern NM: Outcomes of Single Versus Multiple Trauma Exposure in a Screening Sample. J Traumatic Stress. 2000, 13 (2): 271-286. 10.1023/A:1007758711939.
Lopes Cardoso B, Bilukha OO, Gotway Crawford CA, Shaikh I, Wolfe MI, Mitchell I, Gerber ML, Anderson M: Mental health, social functioning, and disability in postwar Afghanistan. JAMA. 2004, 292: 575-584. 10.1001/jama.292.5.575.
Jaswal SKP: Gynaecological and mental health of low-income urban women in India. PhD thesis. 1995, London School of Hygiene and Tropical Medicine
American Psychiatric Association: Diagnostic and statistical manual of mental disorders. 4th edition Text revised. 2001, APA, Washington, DC
Margoob MA, Singh A, Ali Z: A study of suicide attempts in Kashmir valley over the past six months experience from psychiatric outpatient population. Indian Psychiatric Society North Zone. 1997
Rahman A, Hafeez A: Suicidal feelings run high among mothers in refugee camps: a cross-sectional survey. Acta Psychiatrica Scandinavica. 2003, 108: 392-393. 10.1034/j.1600-0447.2003.00220.x.
Tolin DF, Foa EB: Sex Differences in Trauma and Posttraumatic Stress Disorder: A Quantitative Review of 25 Years of Research. Psychological Bulletin. 2006, 132: 959-992. 10.1037/0033-2909.132.6.959.
Creamer M, Burgess P, Pattison P: Cognitive processing in post-trauma reactions. Some preliminary findings. Psychol Med. 1990, 20: 597-604.
Creamer M, Burgess P, Pattison PL: Reaction to trauma: a cognitive processing model. J Abnormal Psychology. 1992, 101: 452-459. 10.1037/0021-843X.101.3.452.
Pino NW, Meier RF: Gender differences in rape reporting. Sex Roles. 1999, 40: 979-990. 10.1023/A:1018837524712.
Kaufman A, Divasto P, Jackson R, Voorhees D, Christy J: Male rape victims: Non institutionalized assault. Am J Psychiatry. 1980, 137: 221-223.
Friedman MJ, Schnurr PP: The relationship between trauma, post-traumatic stress disorder and physical health. Neurobiological and clinical consequences of stress. Edited by: Friedman MJ, Charney DS, Deutch AY. 1995, Lippincott-Raven, Philadelphia
Selye H: The stress of life. 1956, McGraw-Hill Book Company, New York
van der Kolk BA, Pelcovitz D, Roth S, Mandel FS, McFarlane AC, Herman JL: Dissociation, somatization, and affect dysregulation: The complexity of adaptation to trauma. Am J Psychiatry. 1996, 153 (7 Suppl): 83-93.
McFarlane AC, Yehuda R: Resilience, vulnerability and the course of posttraumatic stress reactions. Traumatic stress. The effects of overwhelming experiences on mind, body, and society. Edited by: van der Kolk B, McFarlane AC, Weisaeth L. 1996, Guildford press, New York
Op den Velde W: Post-traumatic stress in life-span perspective: The Dutch resistance veterans adjustment study. 2001, The Netherlands, Aalsmeer: Megaset Design BV
Friedman MJ, Schnurr PP: The relationship between trauma, post-traumatic stress disorder and physical health. Neurobiological and clinical consequences of stress. Edited by: Friedman MJ, Charney DS, Deutch AY. 1995, Lippincott-Raven, Philadelphia
Green BL, Schnurr PP: Trauma and physical health. Clinical Quarterly. 2000, 9: 1-5.
Schnurr PP, Jankowski MK: Physical health and post-traumatic stress disorder: review and synthesis. Semin Clin Neuropsychiatry. 1999, 4 (4): 295-304.
Solomon Z: Combat Stress Reaction: The Enduring Toll of War. 1993, New York: Plenium Press
Schnurr PP, Jankowski MK: Physical health and post-traumatic stress disorder: review and synthesis. Semin Clin Neuropsychiatry. 1999, 4 (4): 295-304.
McFarlane AC, Yehuda R: Resilience, vulnerability and the course of posttraumatic stress reactions. Traumatic stress. The effects of overwhelming experiences on mind, body, and society. Edited by: van der Kolk B, McFarlane AC, Weisaeth L. 1996, Guildford press, New York
Eitinger L, Strom A: Mortality and morbidity after excessive stress: a follow-up investigation of Norwegian concentration camp survivors. 1973, New York: Humanities Press
Brewin CR, Andrews B, Valentine JD: Meta-analysis of risk factors for post-traumatic stress disorder in trauma-exposed adults. J Clin Consult Psychol. 2000, 68: 748-766. 10.1037/0022-006X.68.5.748.
Ahmer S, Faruqui RA, Anita Aijaz A: Psychiatric rating scales in Urdu: a systematic review. BMC Psychiatry. 2007, 7: 59-10.1186/1471-244X-7-59.
Acknowledgements
We gratefully acknowledge the support provided by a number of Kashmir national staff contributed to the conduct of this survey but whose names cannot be mentioned for security reasons. We also thank all survey participants for their time. Finally, thanks to Clair Mills for critical comments on earlier drafts of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
KJ designed and co-ordinated the study and wrote the first draft of the paper. NF supported the conceptual framing of the findings, assisted with the analysis, and led subsequent drafts. SK and KL provided statistical support for the design and analysis, and helped with the writing of the paper. SF, RG and BR oversaw the implementation of the survey, managed data collection in the field, and contributed to the writing of the paper. RK provided conceptual oversight and contributed to the writing of the paper.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
de Jong, K., van de Kam, S., Ford, N. et al. Conflict in the Indian Kashmir Valley II: psychosocial impact. Confl Health 2, 11 (2008). https://doi.org/10.1186/1752-1505-2-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1752-1505-2-11