Abstract
Contagious keratoconjunctivitis is a rather common disease in Norwegian sheep. Since the knowledge of its aetiology is limited, the present study was performed to determine the microorganisms involved. Local veterinarians throughout the country collected conjunctival swabs from both sick (n = 43) and healthy (n = 42) sheep on 15 farms with outbreaks of ovine keratoconjunctivitis, and further from healthy sheep (n = 50) on 17 farms not showing any signs of conjunctival disease. All samples were cultivated for bacteria and mycoplasma.
Listeria monocytogenes was isolated from 3 cases (1%) in one single herd. Staphylococcus aureus (5%), Corynebacterium spp. (2%) and Escherichia coli (4%) were isolated only in herds with keratoconjunctivitis, but from both sick and healthy animals. Moraxella (Branhamella) ovis was isolated from 28% of sampled animals in affected herds and from 10% of sampled animals in healthy herds. The corresponding numbers for Moraxella spp. were 9%/12%, for Pseudomonas spp. 7%/8%, for Staphylococcus spp. 22%/22%, for Bacillus spp. 12%/14%, for Micrococcus spp. 6%/2% and for Streptococcus/Enterococcus spp. 2%/2%. Mycoplasma conjunctivae was isolated from 16 animals with keratoconjunctivitis (37%) and from 3 animals without clinical signs (7%) in farms with keratoconjunctivitis. In farms without clinical signs of keratoconjunctivitis, M. conjunctivae was isolated in 4 animals (8%).
To our knowledge, this is the first time M. conjunctivae has been isolated in Norway. Other predisposing agents found were Moraxella (Branhamella) ovis and Listeria monocytogenes. The etiological importance of different microorganisms in ovine keratoconjunctivitis seems to vary; some are probably only present as secondary invaders. Other possible causes of ovine keratoconjunctivitis in Norway, such as Chlamydia psittaci, remain to be investigated.
Sammendrag
Bakteriologisk undersøkelse av smittsom øyebetennelse hos norsk sau.
Smittsom øyebetennelse (infeksiøs keratokonjunktivitt) er relativt vanlig hos norsk sau. Siden årsaksforhold i stor grad er ukjent, ble denne studien gjennomført for å bestemme involverte mikroorganismer. Praktiserende veterinærer fra hele landet svabret konjunktiva fra både syk (n=43) og frisk (n=42) sau i 15 besetninger med utbrudd av øyebetennelse, og dessuten fra frisk sau (n=50) i 17 besetninger uten konjunktivittsymptomer. Alle prøver ble dyrket for bakterier og mykoplasmer. Listeria monocytogenes ble isolert fra 3 kasus (1%) i én besetning. Staphylococcus aureus (5%), Corynebacterium spp. (2%) og Escherichia coli (4%) ble kun isolert i besetninger med keratokonjuntivitt, men både fra syke og friske dyr. Moraxella (Branhamella) ovis ble isolert fra 28% av prøvetatte dyr i angrepne besetninger og fra 10% av prøvetatte dyr i friske besetninger. Tilsvarende tall for Moraxella spp. var 9%/12%, for Pseudomonas spp. 7%/8%, for Staphylococcus spp. 22%/22%, for Bacillus spp. 12%/14%, for Micrococcus spp. 6%/2% og for Streptococcus/Enterococcus spp. 2%/2%. Mycoplasma conjunctivae ble isolert fra 16 dyr med keratokonjunktivitt (16%) og fra 3 dyr uten kliniske tegn (7%) i besetninger med keratokonjunktivitt. I besetninger uten kliniske tegn for keratokonjunktivitt, ble M. conjucnctivae isolert fra 4 dyr (8%). Etter hva vi kjenner til, er dette første gang Mycoplasma conjunctivae ble isolert i Norge. Andre predisponerende smittestoffer som ble påvist var Moraxella (Branhamella) ovis og Listeria monocytogenes. Etiologisk betydning av ulike mikroorganismer for smittsom øyebetennelse synes å variere; noen er trulig kun tilstede som sekundærinfeksjon. Andre mulige årsaker til smittsom øyebetennelse, som for eksempel Chlamydia psittaci, gjenstår å undersøke.
Similar content being viewed by others
Introduction
Keratoconjunctivitis in sheep is a painful disease. It may cause temporary, or in severe cases permanent blindness. The first signs are hyperaemia, serous lachrymation, increased blinking and blepharospasm [11]. Both eyes usually become affected, although the clinical signs may start in one eye only. Later, the conjunctival blood vessels become dilatated and migrate across the cornea. The cornea may become blackened or greyish, especially in the periphery. After 2 to 5 days the exudate becomes purulent. Occasionally a corneal ulcer develops. Rarely, further infection of the anterior chamber leads to panophthalmitis, and shrinking of the ocular globe. Usually animals begin to recover after a week, but some lambs remain ill for 3 to 4 weeks with weakness and fever [24]. They are anorectic, resulting in weight loss and reduced slaughter weights. According to the last available official veterinary statistics, keratoconjunctivitis is rather common in Norwegian sheep [28]. Practitioners reported 4,470 clinical cases in 1996, most of which were referred to as contagious. The actual incidence is probably higher, since many cases are treated by the owner or not treated at all. Most cases are observed during autumn and winter, after the animals have been taken down from the mountains and are housed indoors. Only scarce information is available on bacteriological findings on cases in Norway. [27] described Neisseria ovis, today termed Moraxella (Branhamella) ovis, while [24] demonstrated Rickettsia (Colesiota) conjunctivae from conjunctival smears and [26] isolated Listeria monocytogenes.
Knowledge of the incidence of keratoconjunctivitis, the microorganisms involved and the predisposing and environmental factors are important for correct treatment and prophylaxis. The aim of this study was to clarify the microorganisms involved and their significance. The study has previously been presented at the Sheep Veterinary Society's meeting at Sandnes Norway [1].
Materials and methods
Study design
A multicentric case-control study was performed between October 1993 and February 1994. Two local veterinarians from each of 6 counties located in South, East, West and North Norway participated in the study. Each veterinarian should sample animals from 4 farms, 2 with and 2 without outbreaks of keratoconjunctivitis. On the farms with signs of keratoconjunctivitis, both affected and unaffected animals were sampled. One infected group and 2 control groups were thus created. The animals were sampled when outbreaks occurred. The healthy controls showed no signs of keratoconjunctivitis and had not been treated with antibiotics systemically or locally during the 3 weeks prior to sampling. Animals with entropion were excluded from the study.
Sampling
Sampling equipment and questionnaires were distributed to the veterinarians prior to the study. Sampling on the conjunctiva was carried out on the lower eyelid of one eye with 2 sterile cotton swabs; one was put into a mycoplasma broth (see below) and the other into a bacterial transport medium (Copan, Bovezzo, Italy). Information regarding animal and farm was noted on the questionnaire. The samples and questionnaires were sent via mail to the laboratory.
Cultivation of bacteria
The conjunctival swab was streaked onto 2 heart infusion agar plates with 5% bovine blood (blood agar) and onto one bromthymolblue lactose sucrose agar plate, as described elsewhere (Stuve et al. 1992), and inoculated in heart infusion broth with 5% horse serum. A Staphylococcus aureus culture was lined onto one of the blood agar plates before cultivation in an atmosphere containing 5% CO2 in air. The other media were cultivated aerobically. All media were incubated at 37°C for 24 h. The growth of the plates was examined visually. If no growth was observed, the plates were incubated for a further 24 h and the broth was subcultivated on blood agar. The numbers of colonies for each type of bacteria present was recorded as rich, moderate or poor. Representative colonies of bacteria were subcultivated onto blood agar plates and identified through biochemical tests, if necessary through the use of additional identification kits (API – bioMérieux, Marcy l'Etolie, France), to genus or species level (listed in Table 1). The following bacteria were identified to species level: Listeria monocytogenes, Staphylococcus aureus, Escherichia coli and Moraxella (Branhamella) ovis.
Cultivation of mycoplasmas
Two media were used for cultivation of mycoplasmas [16, 19], NHS-20 for fastidious acid-producing species and a Hayflick's medium enriched with arginine and urea (HAU) [17] for arginine-metabolizing species and for ureaplasma. The transport medium was a Hayflick's type with bacitracin (0.3 mg/ml), cycloserine (0.2 mg/ml) and vancomycine (0.15 mg/ml) (all Sigma Chemical Company, St. Louis, MO, USA).
At the laboratory, 0.2 ml of the transport medium was transferred by serial 10 fold dilutions to 10-5 in NHS-20 and HAU-medium [19]. The media were incubated aerobically at 37°C up to 3 weeks while rolling in a drum. Growth was indicated by a yellow or blue colour change in the medium (pH indicator: phenol red) and a new passage to 10-4 was set up.
Following approximately 5 passages, the mycoplasmas were adapted to the culture media, and the following diagnostic tests were carried out: cultivation on Sabourauds medium for fungal growth, cultivation on an antibiotic-free medium for growth of bacterial L-forms, cultivation on urea-free medium where ureaplasmas would not grow, cultivation on solid HS-medium to record colony morphology, and for the SPS and digitonin tests [15]. Mycoplasmas were identified to species level with rabbit hyperimmune serum by the disc growth inhibition test (DGI) [31] and indirect Epi-immunofluorescence [29] of colonies on solid medium. Mycoplasma conjunctivae type chain (HRC 581) antiserum was used to identify this species.
Statistical method
The Fisher exact test was used to test statistical differences between cases and controls in relation to bacteriological findings [2].
Results
One hundred and thirty-five animals were sampled, comprising 43 sick animals and 42 healthy animals on 15 farms with outbreaks of keratoconjunctivitis, and 50 animals on 17 farms without signs of keratoconjunctivitis. Both case and control animals had similar age, sex and breed distributions.
The bacteria and mycoplasma isolated from the conjunctiva of the 135 sampled sheep are presented in Table 1. More than one type of microorganism was isolated from some of the animals. No bacteria were cultivated from 7 sheep (2 sick animals and 5 healthy animals) on farms with disease, and from 2 animals on farms without signs of keratoconjunctivitis.
Listeria monocytogenes was isolated from 3 animals with keratoconjunctivitis in one single herd from northern Norway. S. aureus (5%), Corynebacterium spp. (2%) and E. coli (4%) were isolated only in herds with keratoconjunctivitis. For these bacteria, there were no significant differences between cases and controls for numbers of isolates.
M. (B.) ovis was isolated from 24 sampled animals in affected herds (28%) and from five sampled animals in healthy herds (10%). No significant difference was found when comparing cases and controls within the affected farms. Significant differences were found when comparing cases or controls from farms with outbreaks of keratoconjunctivitis to controls from farms without keratoconjunctivitis (p < 0.05).
For all other bacteria found, there were no statistical differences between cases and controls. Mycoplasma strains were isolated from 16 animals with keratoconjunctivitis (37%) and from 3 animals without clinical signs (7%) on farms with keratoconjunctivitis. In farms without clinical signs of keratoconjunctivitis, mycoplasma was isolated from 4 animals (8%). Isolations were made in all 6 counties. The difference between cases and controls was significant (p < 0.001).
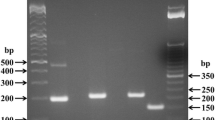
All 23 mycoplasma isolates grew equally well with a yellow colour change in the media NHS-20 and HAU, including M. conjunctivae type strain HRC 581. No evidence of growth of alkali-producing strains was noted. All isolates produced acid, displayed fried-egg colony morphology on solid medium, did not revert to a parent L-form, and were distinctly inhibited in the SPS/digitonin test. All the strains showed similar growth characteristics. Five of them were examined serologically using the DGI test and immunofluorescence of colonies. Antiserum against Mycoplasma conjunctivae inhibited growth of all 5 isolates.
Discussion
The present study was conducted to estimate the role of various microorganisms in keratoconjunctivitis in Norwegian sheep. Ovine keratoconjunctivitis is considered to have a worldwide distribution. Flies and sun light have been regarded as predisposing factors, and a variety of microorganisms have been listed as causative [11].
In Norway, most cases of ovine infectious keratoconjunctivitis are observed in autumn and winter, perhaps due to the way sheep husbandry is practised in this country. Lambs are born from April to May. In the summer, both ewes and offspring are taken to graze in the mountains or forests, where they stay spread over large areas and receive little human intervention. The predominance of recorded cases during autumn may be linked to the increased contact level between animals and/or the closer level of supervision by farmers that occurs when the sheep are again collected into barns before the winter.
Mycoplasma conjunctivae and Chlamydia psittaci are generally regarded as pathogens involved in ovine infectious keratoconjunctivitis [22]. C. psittaci sometimes causes isolated outbreaks of follicular ovine infectious keratoconjunctivitis [3, 6], and is also responsible for polyarthritis in lambs [21]. However, this manifestation was not recorded and the presence of C. psittaci was not investigated in the present study. Mycoplasma strains were isolated predominantly from animals with keratoconjunctivitis.
Different species of mycoplasma species can be distinguished by their ability to ferment glucose, utilize arginine, or hydrolyse urea. Arginine hydrolysing mycoplasmas and ureaplasmas both turn HAU medium red, while acid producers, like M. conjunctivae, turn it yellow. All our isolated strains lowered the pH of HAU and NHS-20 media at the same speed, i.e. the medium turned yellow in the same dilution and after the same time. Other mycoplasmas (Mycoplasma arginini, Acholeplasma oculi and M. ovipneumoniae) isolated from cases of ovine keratoconjunctivitis from other countries differ in the above listed properties [7]. Five of the strains were identified as M. conjunctivae, and we find it likely that all isolated strains in fact are M. conjunctivae.
Coles probably described M. conjunctivae when he reported Rickettsiae (Colesiota) conjunctivae as the main cause of ovine infectious keratoconjunctivitis in 1931. May Grünwald Giemsa-stained conjunctival smears revealed cytoplasmatic inclusion bodies from sheep with keratoconjunctivitis. [33] used acridine orange and iodine stains and isolated mycoplasma from such smears. The proposed cytoplasmatic inclusion bodies were then demonstrated to be extracellular mycoplasma, namely M. conjunctivae [4]. M. conjunctivae has probably already been demonstrated from conjunctival smears from both sheep and reindeer in Norway [24, 25], but to our knowledge, the present study isolated M. conjunctivae for the first time. Previous studies, and our study, have isolated M. conjunctivae significantly more often from sheep with signs of keratoconjunctivitis than from animals without clinical signs [10, 13, 35, 36]. Keratoconjunctivitis has been induced experimentally by instillation of M. conjunctivae in ovine eye sacs [8, 12, 23, 34].
[27] demonstrated M. (B.) ovis in ovine infectious keratoconjunctivitis, but was uncertain as to its aetiological role. In some reports M. (B.) ovis was isolated more often from eyes with keratoconjunctivitis than from healthy eyes [9, 20]. Like [35] we could isolate M. (B.) ovis equally often from animals with signs of keratoconjunctivitis as from animals in the same farms without signs of the disease. However, there were only a few isolates from the farms without keratoconjunctivitis. The etiological role of M. (B.) ovis is still controversial. Instillation of M. (B.) ovis did not induce keratoconjunctivitis, even after previous scarification of the cornea [14, 30, 9] showed that a smooth type of M. (B.) ovis, previously isolated from a field case of keratoconjunctivitis, could increase the severity of clinical signs when introduced into sheep eyes with M. conjunctive. It is possible that virulent strains of M. (B.) ovis cause keratoconjunctivitis or at least contribute to severity of concurrent M. conjunctivae infections [18], as is the case in bovine infectious keratoconjunctivitis, where Moraxella bovis is the aetiological agent. These strains may also be unstable under laboratory conditions, explaining why it has been difficult to cause disease experimentally. Before this possibility may be elucidated, however, it will be necessary to determine the virulence factors involved.
The isolation of L. monocytogenes from 3 sick animals is an interesting finding. L. monocytogenes has previously been isolated from silagefed winter-housed animals [26, 37], as it also was in the present study, and is probably only rarely a cause of keratoconjunctivitis.
No significant differences could be demonstrated between the cases of keratoconjunctivitis and controls for the other bacteria isolated, suggesting that these are without significant importance. [13] isolated S. aureus from about the same number of sheep with keratoconjunctivitis as from sheep without clinical signs of this disease, but found a possible role in converting mild infection to severe. They also found significantly more E. coli isolates in affected sheep than in unaffected animals, but since the prevalence rate was low (7,5%) they considered this agent not to be a primary causal agent. In our study only a few isolates were made of S. aureus, Corynebacterium spp. and E. coli from animals with and without clinical signs of keratoconjunctivitis, and only in farms having cases of keratoconjunctivitis.
Conclusion
While ovine infectious keratoconjunctivitis has been described throughout the world, this is to our knowledge the first time M. conjunctivae was isolated in Norway in association with the disease. The etiological importance of other microorganisms involved in ovine keratoconjunctivitis seems to vary, and some are probably only important as secondary invaders. Other possible causes of keratoconjunctivitis in sheep, such as C. psittaci, remain to be investigated.
References
Åkerstedt J, Hofshagen M: Conjunctivitis in sheep – a bacteriological study. Proc Sheep Veterinary Society, Scandinavian Meeting. 1995, 135-137.
Altman DG: Practical statistics for medical research. 1993, Chapman & Hall, London, 1
Andrews AH, Goddard PC, Wilsmore AJ, Dagnall GJ: A chlamydial keratoconjunctivitis in a British sheep flock. Vet Rec. 1987, 120: 238-239.
Barile MF, Giudice RAd, Tully JG: Isolation and Characterization of Mycoplasma conjunctivae sp. n. from Sheep and Goats with Keratoconjunctivitis. Infect Immun. 1972, 5: 70-76.
Coles JD: A rickettsia-like organism in the conjunctiva of sheep. 17th Report of the Director of Veterinary Services and Animal Industry. 1931, 175-186.
Cooper BS: Transmission of a Chlamydia-like agent isolated from contagious conjunctivokeratitis of sheep. N Z Vet J. 1974, 22: 181-184.
Cottew GS: Caprine-ovine mycoplasmas. 1979, Academic Press, New York
Dagnall GJ: Experimental infection of the conjunctival sac of lambs with Mycoplasma conjunctivae. Br vet J. 1993, 149: 429-435.
Dagnall GJ: An investigation of colonization of the conjunctival sac of sheep by bacteria and mycoplasmas. Epidem Infect. 1994, 112: 561-567.
Dagnall GJ: The role of Branhamella ovis, Mycoplasma conjunctivae and Chlamydia psittaci in conjunctivitis of sheep. Br vet J. 1994, 150: 65-71.
Egwu GO: Ovine infectious keratoconjunctivitis: some studies on the role of Mycoplasma conjunctivae. 1989, PhD., University of Liverpool
Egwu GO, Faull WB: Humoral immune responses in lambs following ocular experimental infection with a pure cloned culture of Mycoplasma conjunctivae. Bull Anim Hlth Prod Afr. 1991, 39: 333-337.
Egwu GO, Faull WB, Bradbury JM, Clarkson MJ: Ovine infectious keratoconjunctivitis: a microbiological study of clinically unaffected and affected sheep's eyes with special reference to Mycoplasma conjunctivae. Vet Rec. 1989, 125: 253-256.
Fairlie G: The Isolation of a Haemolytic Neisseria from cattle and sheep in the North of Scotland. Vet Rec. 1966, 78: 101-112.
Freundt EA, Andrews BE, Ernø H, Kunze M, Black FT: The sensitivity of Mycoplasmateles to sodium-polyanethol-sulfonate and digitonin. Zbl Bakt A Orig. 1973, 225: 104-112.
Friis NF: Some recommendations concerning primaryisolation of Mycoplasma suipneumoniae and Mycoplasma flocculare. Nord Vet-Med. 1975, 27: 337-339.
Friis NF, Krogh HV: Isolation of mycoplasmas from Danish cattle. Nord Vet-Med. 1983, 35: 74-81.
Friis NF, Pedersen KB: Isolation of Mycoplasma bovoculi from cases of infectious bovine keratoconjunctivitis. Acta vet scand. 1979, 20: 51-59.
Friis NF, Ahrens P, Larsen HJ: Mycoplasma hyosynoviae isolation from the upper respiratory tract and tonsils of pigs. Acta vet scand. 1991, 32: 425-429.
Hansson NE, Lindqvist Å, Wierup M: Moraxella ovis isolerat vid ett utbrott av keratokonjunktivit i en fårbesättning. Sven vet Tidn. 1984, 36: 823-826.
Hopkins JB, Stephenson EH, Storz J, Pierson RE: Conjunctivitis associated with chlamydial polyarthritis in lambs. J Am vet med Ass. 1973, 163: 1157-1160.
Jones GE: Infectious keratoconjunctivitis. 1991, Blackwell, Oxford, 2
Jones GE, Foggie A, Sutherland A, Harker DB: Mycoplasmas and ovine keratoconjunctivitis. Vet Rec. 1976, 99: 137-141.
Kjølleberg K: Smittsom øyebetennelse hos sau. Nor vet T. 1971, 71: 233-237.
Kummeneje K: Isolation of Neisseria ovis and a Colesiota conjunctivae-like organism from cases of kerato-conjunctivitis in reindeer in northern Norway. Acta vet scand. 1976, 17: 107-108.
Kummeneje K, Mikkelsen T: Isolation of Listeria monocytogenes Type O4 from cases of keratoconjunctivitis in cattle and sheep. Nord Vet-Med. 1975, 27: 144-149.
Lindqvist K: A Neisseria species associated with infectious keratocnjunctivitis of sheep – Neisseria ovis nov. spec. J infect Dis. 1960, 106: 162-165.
The Norwegian Animal Health Authority: Animal disease report. 1996
Rosendal S, Black FT: Direct and indirect immunofluorescence of unfixed mycoplasma colonies. Acta pathol microbiol scand. 1972, 80B: 615-622.
Spradbrow PB: Experimental infection of the ovine cornea with Neisseria ovis. Vet Rec. 1971, 88: 615-616.
Stanbridge E, Hayflick L: Growth inhibition test for identification of mycoplasma sp. utilizing dried antiserum impregnated paper discs. J Bact. 1967, 93: 1392-1396.
Stuve G, Hofshagen M, Holt G: Necrotizing lesions in the intestine, gizzard, and liver in captive capercailles (Tetrao urogallus) associated with Clostridium perfringens. J Wildl Dis. 1992, 28: 598-602.
Surman PG: Cytology of 'pink-eye' of sheep, including a reference to trachoma of man, by employing acridine orange and iodine stains, and isolation of Mycoplasma agents from infected sheep eyes. Aust J exp med Biol Sci. 1968, 21: 447-467.
ter Laak EA, Schreuder BE, Kimman TG, Houwers DJ: Ovine keratoconjunctivitis experimentally induced by instillation of Mycoplasma conjunctivae. Vet Quart. 1988, 10: 217-224.
ter Laak EA, Schreuder BE, Smith-Buys CM: The occurance of Mycoplasma conjunctivae in the Netherlands and its association with infectious keratoconjunctivitis in sheep and goats. Vet Quart. 1988, 10: 73-83.
van Halderen A, Rensburg W, Geyer A, Vorster JH: The identification of Mycoplasma conjunctivae as an aetiological agent of infectious keratoconjunctivitis of sheep in South Africa. Onderstepoort J Vet Res. 1994, 61: 231-237.
Walker JK, Morgan JH: Ovine ophthalmitis associated with Listeria monocytogenes. Vet Rec. 1993, 132: 636-
Acknowledgements
The authors want to thank the following veterinary practitioners who kindly collected the samples for the study: Jostein Rise, Per Gillund, Per Helge Seltveit, Magnus Solberg, Olav Hermansen, Oddmund Grøtte, Gunnar Dragset, Anja Lindegård and last but not least Berit Hansen.
Grateful acknowledgement is expressed to Dr. N. F. Friis at the Danish Institute for Food and Veterinary Research, Copenhagen, Denmark for supplying mycoplasma strains and antiserum, carrying out the serological identification of M. conjunctivae and critically reviewing the manuscript, and Dr. E. A. ter Laak, Central Veterinary Institute, Lelystad, The Netherlands for providing the M. conjunctivae type strain HRC 581.
Author information
Authors and Affiliations
Additional information
Reprints may be obtained from: J. Åkerstedt, National Veterinary Institute, P.O. box 8156 Dep., NO-0033 Oslo, Norway. E-mail johan.akerstedt@vetinst.no, tel: +47 23 21 64 02, fax +47 23 21 63 01.
Rights and permissions
About this article
Cite this article
Åkerstedt, J., Hofshagen, M. Bacteriological Investigation of Infectious Keratoconjunctivitis in Norwegian Sheep. Acta Vet Scand 45, 19 (2004). https://doi.org/10.1186/1751-0147-45-19
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1751-0147-45-19