Abstract
Background
Mucopolysaccharidosis type I (MPS I) is traditionally divided into three phenotypes: the severe Hurler (MPS I-H) phenotype, the intermediate Hurler-Scheie (MPS I-H/S) phenotype and the attenuated Scheie (MPS I-S) phenotype. However, there are no clear criteria for delineating the different phenotypes. Because decisions about optimal treatment (enzyme replacement therapy or hematopoietic stem cell transplantation) need to be made quickly and depend on the presumed phenotype, an assessment of phenotypic severity should be performed soon after diagnosis. Therefore, a numerical severity scale for classifying different MPS I phenotypes at diagnosis based on clinical signs and symptoms was developed.
Methods
A consensus procedure based on a combined modified Delphi method and a nominal group technique was undertaken. It consisted of two written rounds and a face-to-face meeting. Sixteen MPS I experts participated in the process. The main goal was to identify the most important indicators of phenotypic severity and include these in a numerical severity scale. The correlation between the median subjective expert MPS I rating and the scores derived from this severity scale was used as an indicator of validity.
Results
Full consensus was reached on six key clinical items for assessing severity: age of onset of signs and symptoms, developmental delay, joint stiffness/arthropathy/contractures, kyphosis, cardiomyopathy and large head/frontal bossing. Due to the remarkably large variability in the expert MPS I assessments, however, a reliable numerical scale could not be constructed. Because of this variability, such a scale would always result in patients whose calculated severity score differed unacceptably from the median expert severity score, which was considered to be the 'gold standard'.
Conclusions
Although consensus was reached on the six key items for assessing phenotypic severity in MPS I, expert opinion on phenotypic severity at diagnosis proved to be highly variable. This subjectivity emphasizes the need for validated biomarkers and improved genotype-phenotype correlations that can be incorporated into phenotypic severity assessments at diagnosis.
Similar content being viewed by others
Background
Mucopolysaccharidosis type I (MPS I; OMIM #252800) is a rare autosomal recessive lysosomal storage disorder caused by a deficiency in the alpha-L-iduronidase (IDUA) enzyme, which is involved in the breakdown of the glycosaminoglycans (GAGs) heparan sulfate and dermatan sulfate [1]. The resulting GAG accumulation leads to cellular and organ dysfunction. More than 140 different mutations in the IDUA gene have been described [2, 3]. The birth prevalence varies from 1 in 26,000 (in the Irish Republic) to less than 1 in 900,000 (in Taiwan) [4, 5].
MPS I is traditionally divided into three phenotypes: the severe Hurler (MPS I-H) phenotype, the intermediate Hurler-Scheie (MPS I-H/S) phenotype, and the attenuated Scheie (MPS I/S) phenotype. In reality, however, MPS I presents with a continuous spectrum of phenotypic severity [1, 6, 7].
MPS I-H patients have marked cognitive delay, coarse facial features, corneal clouding, hearing impairment, ear-nose-throat infections, hepatosplenomegaly, umbilical and inguinal hernias, restricted joint mobility and orthopedic, cardiac and respiratory problems in early childhood. Without appropriate treatment, their life expectancy is severely limited. At the other end of the spectrum, MPS I-S patients have normal intelligence and near-normal life expectancy but experience significant morbidity as a consequence of restricted joint mobility, carpal tunnel syndrome, skeletal dysplasia, cardiac disorders and pulmonary dysfunction. Patients with the intermediate MPS I-H/S phenotype are generally described as having no or only mild cognitive impairment and relatively severe somatic symptoms that limit life expectancy to the 2nd or 3rd decade in the absence of treatment [1, 6–9].
Two therapeutic options are currently available: hematopoietic stem cell transplantation (HSCT) and intravenous enzyme replacement therapy (ERT). HSCT can stabilize neurocognitive function, prevent fatal cardio-pulmonary complications, and improve overall survival [10]. However, HSCT can only preserve cognitive function if successfully performed at an early age [10–12], before the onset of significant central nervous system involvement, and it still carries a considerable risk of procedure-related morbidity and mortality. Weekly ERT with recombinant IDUA (laronidase) can improve the respiratory and cardiac symptoms and some of the skeletal and joint manifestations, reduce hepatosplenomegaly, and improve the overall quality of life [13–17]. Because intravenously administered laronidase does not cross the blood-brain barrier [18], ERT cannot prevent cognitive decline in patients with MPS I-H. Therefore, HSCT is the preferred treatment strategy for patients with a presumed MPS 1-H phenotype who are diagnosed before the age of approximately 2.5 years, while patients with the MPS I-H/S and MPS I-S phenotypes may benefit significantly from ERT [12].
When an MPS I diagnosis is made, the phenotype needs to be assessed as soon as possible so that the optimal treatment strategy can be quickly determined. The outcome of HSCT in MPS I-H is less favorable when there is a longer delay between diagnosis and transplant [19, 20]. If ERT is the treatment of choice, it probably should be initiated early to prevent irreversible damage [12, 21]. Because the predictive value of genotyping is still limited, the phenotypic severity often needs to be assessed solely on the basis of clinical signs and symptoms. However, clear criteria for delineating the different phenotypes are lacking, particularly at the time of diagnosis.
The aim of this study was to develop a consensus scale for phenotypically classifying MPS I patients at diagnosis based on clinical signs and symptoms.
Methods
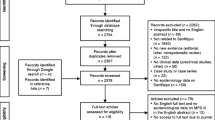
The process for constructing a diagnostic disease severity scale included two written rounds, a consensus meeting and a combined modified Delphi method and nominal group technique [22, 23]. All of the 16 internationally recognized MPS I experts who were invited to join this project agreed to collaborate. In the first written round, the experts were asked to assess the relative importance of potential criteria for classifying disease severity. For this purpose, a list of 30 criteria selected from a review of the literature was composed by three experts (CEH, FAW and JEW) (Table 1 top panel). The participants rated the 30 criteria (major, intermediate, minor or redundant) according to their perceived importance for phenotypic classification at diagnosis and also proposed additional criteria. Nine additional criteria were suggested (Table 1, bottom panel). Based on these results, seven items that were rated of major importance by the majority of the experts and not rated as redundant by any were selected ('results, first written round', Table 2).
In the second written round, 20 MPS I case descriptions were sent to the experts. The case descriptions were based on clinical information available at the time of diagnosis and were retrieved from two participating centers (Amsterdam and Manchester). The cases were selected to represent a wide range of MPS I phenotypes. The experts rated each case description for severity on an 11-point scale (0 = mildest; 10 = most severe). If one of the experts was involved in treating one of the specific cases, that expert's rating for that case was excluded from the analyses. The median expert rating for a case was considered to be the 'gold standard' severity score.
All 20 case descriptions were scored by one investigator (QGAT) according to the presence or absence of the 39 criteria in Table 1. Mann-Whitney U tests were used to investigate the associations between the median expert case scores and the presence or absence of each of the 39 items. An item was considered to be "key" when there was a significant difference (p < 0.05) between the median expert rating of the cases for which the item was present and the median expert rating of the cases for which the item was not present. The list of key items resulting from this analysis constituted the 'results, second written round' (Table 2).
A face-to-face consensus meeting was subsequently held in Amsterdam (in May 2008). To investigate the intra-observer reproducibility [24], all 20 case descriptions were presented in a random order and rated by the experts for severity again. The experts were then informed of the results of the two written rounds, and all of the case descriptions were then separately discussed. The experts were asked to explain which items they considered to be most important for assessing disease severity in a particular case, which led to discussions about which of the items were most important and how they should be defined. Next, every expert proposed a list of the items they deemed important for a severity scale. These items were ranked according to the frequency with which they had been proposed (Table 3) and compared with the items in the 'results, second written round' (Table 2). Finally, a consensus was reached on the list of items considered to be most important for phenotypic classification ('results, consensus meeting'; Table 2).
For the three items in which the severity definition or grading was complicated, working groups of 3-5 experts were asked to make a proposal for each item based on the best evidence.
After the meeting, the scores of the items in the final consensus list that were present in each patient description were equally weighted and summed to obtain an objective MPS I phenotypic severity score at diagnosis. The correlation between the scores on this 'MPS I severity scale' and the median expert scores ('gold standard') for the 20 case descriptions was calculated.
To assess the validity of this scale, a set of 18 new MPS I case descriptions, again representing the full MPS I phenotypic spectrum, was compiled. Care was taken to include information on all six of the items in the final consensus list (Table 2) in each case description. The experts rated the new cases for severity (0-10), and the correlation between the objective phenotypic severity scores and the median expert scores for the 18 case descriptions was calculated.
Statistical analysis
The association between the presence or absence of each item and the median expert severity scores for the individual cases was investigated using the Mann-Whitney U test (SPSS 18.0). To quantify the intra- and inter-rater reproducibility of the expert scores, the variance components were calculated using a three-way random effects analysis of variance model with the scores as the dependent variable. The following variance components were estimated using the model: between patients (σP2), between experts (σE2), between rounds (σR2), the patients × experts interaction (σPE2), the patients x rounds interaction (σPR2), the experts × rounds interaction (σER2), and the residual (σPER2). Because the absolute values of the expert scores were not of interest, intraclass correlation coefficients (ICCs) were calculated to assess consistency [25].
The intra-rater ICCconsistency was calculated using the following formula:
The inter-rater ICCconsistency was calculated as follows:
There was no 'rounds' factor in the inter-rater reproducibility of the subjective expert scores of the 18 patient descriptions, which therefore use the following formula:
Spearman correlation coefficients were used to investigate correlations between the median expert scores and the objective phenotypic severity scores. Numerical weights were assigned to the items used in the objective score according to the experts' assessment of their clinical relevance. The goal was to maximize the correlation with the median subjective expert score and thus achieving the best phenotypic differentiation. The level of statistical significance was set at p < 0.05.
Results
Of the 30 items included in the first-round questionnaire (Table 1), 7 were scored as being of ' major importance' by ≥ 50% of the experts and as 'redundant' by none of the experts (Table 2). Nine additional items were proposed (Table 1). The median expert scores of the 20 case descriptions used in the second written round ranged from 1 to 9. There was considerable variation in the expert scores for each case description (Figure 1). The difference between the highest and lowest expert case scores ranged from 2 (for a case with a median expert score of 3) to 8 points (for a case with a median expert score of 6). The intra- and inter-observer ICCs for the expert scores were 0.79 and 0.75, respectively.
Of the 39 items identified in the 'first written round' (Table 1), 12 were not found in any of the 20 case descriptions. The case scores obtained by summing the remaining 27 items (with an item scoring 1 if it was present and 0 otherwise) ranged from 4 to 18. The frequencies of the 27 items in the 20 case descriptions ranged from 5% to 90% (Table 4). The correlation between the case scores from the 27 items and the median expert scores was 0.61, p = 0.004. A significant difference in median expert scores was found between the groups determined by the presence or absence of 7 items ('results, second written round', Table 2): 1) age at onset of symptoms (<1.5 yr) (median difference 4, p = 0.015); 2) developmental delay (median difference 4.5, p = 0.002); 3) kyphosis (median difference 5, p = 0.001); 4) large head/frontal bossing (median difference 4, p = 0.037); 5) early diagnosis (<1.5 yr) (median difference 4, p = 0.001); 6) dysostosis multiplex (median difference 4, p < 0.001) and 7) coarse facial features (median difference 3.5, p = 0.012). The correlation between the unweighted sum score of these seven items and the median expert score was 0.91; p < 0.001.
The 24 items proposed by the individual experts are shown in Table 3 in order of descending frequency. During the meeting, these 24 items were compared with the 7 items from the 'results, second written round' (Table 2). Consensus was reached on including nine of the items in the list of those considered most important for phenotypically classifying MPS I patients (Table 2, 'results, consensus meeting'). For three items, additional discussion was considered necessary in separate working groups after the meeting. Within several weeks after the consensus meeting, the working groups proposed deleting three items from the final consensus list: 1) dysostosis multiplex, 2) growth retardation, and 3) obstructive sleep apnea syndrome (OSAS). The main reason for the exclusions was the inability of the items to differentiate between the phenotypes. All experts agreed with deleting these three items from the final consensus list.
The median expert scores of the 18 case descriptions used in the validation phase ranged from 2 to 8.5. The inter-observer ICC of the expert scores was 0.71. Again, there was considerable variation in the expert severity assessments of the case descriptions (Figure 2). The differences between the highest and lowest expert scores ranged from 3 (for 7 cases with median expert scores of 2.0, 2.5, 7.0, 8.0, 8.0, 8.5 and 8.5) to 8 points (for a case with a median expert score of 7.0).
Despite the reasonable correlations between both the weighted and unweighted sum scores of the six items in the 'final consensus list' and the median expert scores, it became clear that there would always be patients whose calculated severity score differed unacceptably from the median expert severity score, which was considered the 'gold standard'. For this reason, and because of the considerable variability between the experts, we decided to refrain from presenting the six criteria in a numerical 'severity scale'.
Discussion
This consensus procedure was designed to develop a numerical scale for assessing MPS I phenotypic severity at diagnosis to facilitate treatment decisions and patient communication.
Consensus was reached on a list of six items that were considered to be most important for phenotypically classifying MPS I patients at diagnosis (Table 2, 'final consensus list'). Our consensus procedure also identified several items generally considered to be major hallmarks of MPS I that were nevertheless excluded from the list of key items for the following reasons. First, the signs and symptoms important for establishing an MPS I diagnosis often do not differentiate between mild and severe phenotypes, e.g., umbilical or inguinal hernias, coarse facial features, and the presence or severity of corneal clouding and hepatosplenomegaly. Second, although some symptoms (e.g., hydrocephalus) are frequently encountered in young patients with severe phenotypes, the experts did not consider their absence to be an indicator of a mild phenotype. The 'diagnosis at a young age' item was also excluded because it can be influenced by several factors, such as diagnostic difficulties or delays in seeking medical attention. The age of onset of any of the six key signs and symptoms was considered to be a more valuable indicator of phenotypic severity. Finally, cognitive decline was not included as a key item because this item can only be assessed during follow-up (in contrast to developmental delay, which can usually be ascertained at the time of diagnosis).
As a result of the process of item generation, selection and validation, we decided that constructing a reliable numerical scale for assessing phenotypic severity in MPS I patients was not feasible due to the remarkable variability in the expert assessments (Figures 1 and 2), which resulted in a large inter-observer variability. As a result, the expert score that served as the 'gold standard' proved to be unreliable. Even in the patients with high median expert scores, indicating a severe phenotype, the individual expert scores varied considerably, with some experts also assigning the cases intermediate scores (Figures 1 and 2). As a result of this variability among the expert assessments, there would always be patients (even those with the most severe MPS I-H phenotype) whose severity scores from a system based on the six selected items would differ considerably from the median expert score and from a severity score given by several of the experts.
Comparably significant variability in expert severity assessment will likely also occur for other rare diseases, including other lysosomal storage diseases, in which there are pleiotropic and progressive disease manifestations. Although the methods applied in our study may be used to tease out factors related to assessing disease severity that are comparable to the six key items that we obtained for MPS I (Table 2), constructing a reliable severity scale based on clinical signs and symptoms may often be impossible.
The need for reliable and early prediction of MPS I phenotypic severity has become even more pressing with the development of high-throughput newborn screening (NBS) techniques based on measuring IDUA activity and/or immune-quantification of the IDUA protein in dried blood spots [26–28]. A severity score based on clinical signs and symptoms will certainly not be useful in this context, given that a number of signs and symptoms will not be present in the neonatal period.
Because clinical signs and symptoms appear to be insufficiently reliable to assess phenotypic severity at diagnosis, other methods should be vigorously investigated. Combined genotyping and biomarker analysis in plasma and/or urine, such as the recently reported plasma heparin cofactor II-thrombin (HCII-T) complex and the urinary dermatan sulfate:chondroitin sulfate (DS:CS) ratio, promises to be a good strategy for determining disease severity in newly diagnosed MPS I patients [2, 3, 29, 30]
Our study has several limitations. First, the experts differed with respect to the age, phenotype and ethnic background of their patient experiences. These observations may have influenced their opinion of disease severity. Second, the patient information used to write the case descriptions was gathered retrospectively. Thus, some follow-up results were known for most of the patients, which may have biased the data retrieval and the description of the cases. Moreover, the information that had been recorded in the patient files may have been influenced by knowledge of which interventions had (or had not) been performed. Finally, assessing phenotypic severity is hampered by the subjective rating of certain items, e.g., the presence or absence of kyphosis and frontal bossing on clinical examination, the parents' report of the age of symptom onset and the influence of decreased range of motion due to joint disease on performing activities of daily living.
Conclusions
This robust and transparent consensus procedure did not result in a reliable and validated numerical MPS I severity scale. However, the process did produce a list of six items rated by the experts as being most important for phenotypic classification, which may be useful for classifying newly diagnosed MPS I patients. Further studies into the possible roles of genotypes and biomarkers as indicators of disease severity are necessary to optimize clinical diagnosis and decision-making in MPS I patients.
Abbreviations
- ERT:
-
Enzyme replacement therapy
- GAG:
-
Glycosaminoglycan
- HSCT:
-
Hematopoietic stem cell transplantation
- ICC:
-
Intraclass correlation coefficient
- IDUA:
-
Alpha-L-iduronidase
- MPS I:
-
Mucopolysaccharidosis type I
- NBS:
-
Newborn screening
- OSAS:
-
Obstructive sleep apnea syndrome.
References
Neufeld EF, Muenzer J: The mucopolysaccharidoses. In The Online Metabolic and Molecular Bases of Inherited Disease chapter 136 edition. Edited by: Valle D, Beaudet AL, Vogelstein B, Kinzler KW, Antonarakis SE, Ballabio A. New York: McGraw-Hill; 2007.
Terlato NJ, Cox GF: Can mucopolysaccharidosis type I disease severity be predicted based on a patient's genotype? A comprehensive review of the literature. Genet Med. 2003, 5: 286-294. 10.1097/01.GIM.0000078027.83236.49.
Bertola F, Filocamo M, Casati G, Mort M, Rosano C, Tylki-Szymanska A, Tüysüz B, Gabrielli O, Grossi S, Scarpa M, Parenti G, Antuzzi D, Dalmau J, Rocco MD, Vici CD, Okur I, Rosell J, Rovelli A, Furlan F, Rigoldi M, Biondi A, Cooper DN, Parini R: IDUA mutational profiling of a cohort of 102 European patients with Mucopolysaccharidosis type I: identification and characterization of 35 novel α-L-iduronidase (IDUA) alleles. Hum Mutat. 2011, 32: E2189-E2210. 10.1002/humu.21479.
Murphy AM, Lambert D, Treacy EP, O'Meara A, Lynch SA: Incidence and prevalence of mucopolysaccharidosis type 1 in the Irish republic. Arch Dis Child. 2009, 94: 52-54. 10.1136/adc.2007.135772.
Lin HY, Lin SP, Chuang CK, Niu DM, Chen MR, Tsai FJ, Chao MC, Chiu PC, Lin SJ, Tsai LP, Hwu WL, Lin JL: Incidence of the mucopolysaccharidoses in Taiwan, 1984-2004. Am J Med Genet A. 2009, 149A: 960-964. 10.1002/ajmg.a.32781.
Muenzer J, Wraith JE, Clarke LA: Mucopolysaccharidosis I: management and treatment guidelines. Pediatrics. 2009, 123: 19-29. 10.1542/peds.2008-0416.
Pastores GM, Arn P, Beck M, Clarke JT, Guffon N, Kaplan P, Muenzer J, Norato DY, Shapiro E, Thomas J, Viskochil D, Wraith JE: The MPS I registry: design, methodology, and early findings of a global disease registry for monitoring patients with mucopolysaccharidosis type i. Mol Genet Metab. 2007, 91: 37-47. 10.1016/j.ymgme.2007.01.011.
Pastores GM, Meere PA: Musculoskeletal complications associated with lysosomal storage disorders: gaucher disease and Hurler-Scheie syndrome (mucopolysaccharidosis type I). Curr Opin Rheumatol. 2005, 17: 70-78. 10.1097/01.bor.0000147283.40529.13.
Vijay S, Wraith JE: Clinical presentation and follow-up of patients with the attenuated phenotype of mucopolysaccharidosis type I. Acta Paediatr. 2005, 94: 872-877. 10.1080/08035250510031584.
Boelens JJ, Prasad VK, Tolar J, Wynn RF, Peters C: Current international perspectives on hematopoietic stem cell transplantation for inherited metabolic disorders. Pediatr Clin North Am. 2010, 57: 123-145. 10.1016/j.pcl.2009.11.004.
Aldenhoven M, Boelens JJ, de Koning TJ: The clinical outcome of Hurler syndrome after stem cell transplantation. Biol Blood Marrow Transplant. 2008, 14: 485-498. 10.1016/j.bbmt.2008.01.009.
de Ru MH, Boelens JJ, Das AM, Jones SA, van der Lee JH, Mahlaoui N, Mengel E, Offringa M, O'Meara A, Parini R, Rovelli A, Sykora KW, Valayannopoulos V, Vellodi A, Wynn RF, Wijburg FA: Enzyme Replacement Therapy and/or Hematopoietic Stem Cell Transplantation at diagnosis in patients with Mucopolysaccharidosis type I: results of a European consensus procedure. Orphanet J Rare Dis. 2011, 10 (6): 55..
Kakkis ED, Muenzer J, Tiller GE, Waber L, Belmont J, Passage M, Izykowski B, Philips J, Doreshow R, Walot I, Hoft R, Neufeld EF: Enzyme replacement therapy in mucopolysaccharidosis I. N Engl J Med. 2001, 344: 182-188. 10.1056/NEJM200101183440304.
Wraith JE, Clarke LA, Beck M, Kolodny EH, Pastores GM, Muenzer J, Rapoport DM, Berger KI, Swiedler SJ, Kakkis ED, Braakman T, Chadbourne E, Walton-Bowen K, Cox GF: Enzyme replacement therapy for mucopolysaccharidosis I: a randomized, double-blinded, placebo-controlled, multinational study of recombinant human alfa-l-iduronidase (laronidase). J Pediatr. 2004, 144: 581-588. 10.1016/j.jpeds.2004.01.046.
Sifuentes M, Doroshow R, Hoft R, Mason G, Walot I, Diament M, Okazaki S, Huff K, Cox GF, Swiedler SJ, Kakkis ED: A follow-op study of MPS I patients treated with laronidase enzyme replacement therapy for 6 years. Mol Genet Metab. 2007, 90: 171-180. 10.1016/j.ymgme.2006.08.007.
Wraith JE, Beck M, Lane R, van der Ploeg A, Shapiro E, Xue Y, Kakkis ED, Guffon N: Enzyme replacement therapy in patients who have mucopolysaccharidosis I and are younger than 5 years: results of a multinational study of recombinant human alfa-l-iduronidase (laronidase). Paediatrics. 2007, 120: e37-e46. 10.1542/peds.2006-2156.
Clarke LA, Wraith JE, Beck M, Kolodny EH, Pastores GM, Muenzer J, Rapoport DM, Berger KI, Sidman M, Kakkis ED, Cox GF: Long-term efficacy and safety of laronidase in the treatment of Mucopolysaccharidosis I. Pediatrics. 2009, 123: 229-240. 10.1542/peds.2007-3847.
Kakkis ED, McEntee MF, Schmidtchen A, Neufeld EF, Ward DA, Gompf RE, Kania S, Bedolla C, Chien SL, Shull RM: Long-term and high-dose trials of enzyme replacement therapy in the canine model of mucopolysaccharidosis I. Biochem Mol Med. 1996, 58: 156-167. 10.1006/bmme.1996.0044.
Boelens JJ, Rocha V, Aldenhoven M, Wynn R, O'Meara A, Michel G, Ionescu I, Parikh S, Prasad VK, Szabolcs P, Escolar M, Gluckman E, Cavazzana-Calvo M, Kurtzberg J: EUROCORD, inborn error working party of ebmt and duke university: risk factor analysis of outcomes after unrelated cord blood transplantation in patients with hurler syndrome. Biol Blood Marrow Transplant. 2009, 15: 618-625. 10.1016/j.bbmt.2009.01.020.
Boelens JJ, Aldenhoven M, Purtill D, Eapen M, DeForr T, Wynn R, Cavazanna-Calvo M, Tolar J, Prasad VK, Escolar M, Gluckman E, Orchard P, Veys P, Kurtzberg J, Rocha V: Outcomes of transplantation using a various cell source in children with Hurlers syndrome after myelo-ablative conditioning. An Eurocord-EBMT-CIBMTR collaborative study. Biol Blood Marrow Transplant. 2010, 16 (Suppl 2): 180-181.
Gabrielli O, Clarke LA, Bruni S, Coppa GV: Enzyme-replacement therapy in a 5-month-old boy with attenuated presymptomatic MPS I: 5-year follow-up. Pediatrics. 2010, 125: e183-e187. 10.1542/peds.2009-1728.
Jaeschke R, Guyatt GH, Dellinger P, Schünemann H, Levy MM, Kunz R, Norris S, Bion J: GRADE Working Group: Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ. 2008, 337: a744-10.1136/bmj.a744.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B: Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997, 39: 214-223.
Streiner DL, Norman GR: Health measurement scales; a practical guide to their development and use. 2003, Oxford: Oxford University Press
McGraw KO, Wong SP: Forming inferences about some intraclass correlation coefficients. Psychol Methods. 1996, 1: 30-46.
Blanchard S, Sadilek M, Scott CR, Turecek F, Gelb MH: Tandem mass spectrometry for the direct assay of lysosomal enzymes in dried blood spots: application to screening newborns for mucopolysaccharidosis I. Clin Chem. 2008, 54: 2067-2070. 10.1373/clinchem.2008.115410.
Wang D, Eadala B, Sadilek M, Chamoles NA, Turecek F, Scott CR, Gelb MH: Tandem mass spectrometric analysis of dried blood spots for screening of mucopolysaccharidosis I in newborns. Clin Chem. 2005, 51: 898-900. 10.1373/clinchem.2004.047167.
Meikle PJ, Grasby DJ, Dean CJ, Lang DL, Bockmann M, Whittle AM, Fietz MJ, Simonsen H, Fuller M, Brooks DA, Hopwood JJ: Newborn screening for lysosomal storage disorders. Mol Genet Metab. 2006, 88: 307-314. 10.1016/j.ymgme.2006.02.013.
Randall DR, Colobong KE, Hemmelgarn H, Sinclair GB, Hetty E, Thomas A, Bodamer OA, Volkmar B, Fernhoff PM, Casey R, Chan AK, Mitchell G, Stockler S, Melancon S, Rupar T, Clarke LA: Heparin cofactor II-thrombin complex: a biomarker of MPS disease. Mol Genet Metab. 2008, 94: 456-461. 10.1016/j.ymgme.2008.05.001.
Langford-Smith KJ, Mercer J, Petty J, Tylee K, Church H, Roberts J, Moss G, Jones S, Wynn R, Wraith JE, Bigger BW: Heparin cofactor II-thrombin complex and dermatan sulphate:chondroitin sulphate ratio are biomarkers of short- and long-term treatment effects in mucopolysaccharide diseases. J Inherit Metab Dis. 2010, 34: 499-508.
Acknowledgements
We thank Dr. M. Offringa (Amsterdam, the Netherlands, currently Toronto, Canada) for moderating the face-to-face meeting. J. Mercer (Manchester, UK) is acknowledged for assisting with collecting the case histories. This international consensus procedure was made possible by an unrestricted educational grant by Genzyme Corp., Boston, USA.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
FAW, CEH, JHL, JEW and QGAT were part of the planning committee, were involved in the methodological process, and wrote the first draft of the manuscript. MHdR was involved in the validation phase and wrote later drafts of the manuscript. JHL performed the statistical analysis. ATS, CEH, EPT, FAW, GMP, JAR, JEW, JZ, LAC, MB, MS, MVMR, OAB, and SPL participated in written rounds 1 and 2 and the face-to-face consensus meeting. All of the authors reviewed and corrected earlier versions of the manuscript and participated in the creation of its final form.
Minke H de Ru, Quirine GA Teunissen contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
de Ru, M.H., Teunissen, Q.G., van der Lee, J.H. et al. Capturing phenotypic heterogeneity in MPS I: results of an international consensus procedure. Orphanet J Rare Dis 7, 22 (2012). https://doi.org/10.1186/1750-1172-7-22
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1750-1172-7-22