Abstract
Alpha-thalassaemia is inherited as an autosomal recessive disorder characterised by a microcytic hypochromic anaemia, and a clinical phenotype varying from almost asymptomatic to a lethal haemolytic anaemia.
It is probably the most common monogenic gene disorder in the world and is especially frequent in Mediterranean countries, South-East Asia, Africa, the Middle East and in the Indian subcontinent. During the last few decades the incidence of alpha thalassaemia in North-European countries and Northern America has increased because of demographic changes. Compound heterozygotes and some homozygotes have a moderate to severe form of alpha thalassaemia called HbH disease. Hb Bart's hydrops foetalis is a lethal form in which no alpha-globin is synthesized. Alpha thalassaemia most frequently results from deletion of one or both alpha genes from the chromosome and can be classified according to its genotype/phenotype correlation. The normal complement of four functional alpha-globin genes may be decreased by 1, 2, 3 or all 4 copies of the genes, explaining the clinical variation and increasing severity of the disease. All affected individuals have a variable degree of anaemia (low Hb), reduced mean corpuscular haemoglobin (MCH/pg), reduced mean corpuscular volume (MCV/fl) and a normal/slightly reduced level of HbA2. Molecular analysis is usually required to confirm the haematological observations (especially in silent alpha-thalassaemia and alpha-thalassaemia trait). The predominant features in HbH disease are anaemia with variable amounts of HbH (0.8-40%). The type of mutation influences the clinical severity of HbH disease. The distinguishing features of the haemoglobin Bart's hydrops foetalis syndrome are the presence of Hb Bart's and the total absence of HbF. The mode of transmission of alpha thalassaemia is autosomal recessive. Genetic counselling is offered to couples at risk for HbH disease or haemoglobin Bart's Hydrops Foetalis Syndrome. Carriers of alpha+- or alpha0-thalassaemia alleles generally do not need treatment. HbH patients may require intermittent transfusion therapy especially during intercurrent illness. Most pregnancies in which the foetus is known to have the haemoglobin Bart's hydrops foetalis syndrome are terminated due to the increased risk of both maternal and foetal morbidity.
Similar content being viewed by others
Introduction
Why should α thalassaemia be considered in a forum dedicated to rare diseases? It is certainly not a rare genetic trait. On the contrary, it is one of the most common human genetic abnormalities known. Carriers of α thalassaemia are found at polymorphic frequencies (>1%) in all tropical and subtropical populations that have been studied and, in some areas, the carrier state has almost gone to fixation. This is because carriers of α thalassaemia are thought to be at a selective advantage in areas where falciparum malaria is or has been endemic. In areas where the carrier state is common, two clinically important diseases (HbH disease and Hb Bart's hydrops foetalis) occur in compound heterozygotes and homozygotes. The reason for discussing this here is therefore not because these diseases are rare, rather that they may be rarely considered by physicians outside of the regions where thalassaemia commonly occurs. For example, a retrospective study of obstetric records in the U.K. by Petrou et al. revealed an underdiagnosis of both α0-thalassaemia trait and α-thalassaemia hydrops foetalis[1]. With the massive migrations that have occurred over the past few decades it is important to bring these rarely considered diseases to the general attention of clinicians in Northern Europe and North America.
Disease names and synonyms
The generic term α thalassaemia encompasses all of those conditions in which there is a deficit in the production of the α globin chains of haemoglobin (Hb) which is a tetrameric molecule including two α-like and two β-like globin chains (α2β2). Underproduction of α globin chains gives rise to excess β-like globin chains which form γ4 tetramers, called Hb Bart's (in foetal life) and β4 tetramers, called HbH (in adult life). Individuals who carry mutations affecting the α globin genes on one chromosome, associated with minimal anaemia, are said to have α thalassaemia trait. Compound heterozygotes and some homozygotes for α thalassaemia have a moderately severe anaemia characterised by the presence of HbH in the peripheral blood. This condition is referred to as HbH disease. Finally some individuals who make very little or no α globin chains have a very severe form of anaemia which, if untreated, causes death in the neonatal period. This condition is called the Hb Bart's hydrops foetalis syndrome [2–5].
Rarely patients have been seen with very large deletions which remove the α globin genes but also remove many other genes that surround them. This condition is associated with developmental abnormalities (including intellectual disability) and is referred to as the α thalassaemia/mental retardation syndrome on chromosome 16 (ATR16 syndrome: OMIM:141750, reviewed in Higgs et al., 2009 [6] and Wilkie et al., 1990 [7]). Also patients with a rare form of syndromal X-linked mental retardation associated with α thalassaemia have been described, in which the intellectual disability is more severe and the dysmorphic features show striking similarities among patients. This rare condition is called ATR-X syndrome and has been found to involve mutations in a chromatin associated protein called ATRX on the X-chromosome (ATR-X syndrome: OMIM:301040, reviewed elsewhere)[6, 8–11]. Finally, an acquired form of alpha-thalassaemia referred to as the ATMDS syndrome has been described. This predominantly occurs in elderly males with a pre-malignant, clonal haematopoietic disease called myelodysplasia (MDS). This rare syndrome involves acquired mutations in the ATRX gene causing α thalassaemia (OMIM:300448, reviewed in Gibbons et al., 2003;Higgs et al., 2009)[6, 12]. Since these rare conditions have all been reviewed elsewhere they will not be discussed further in this synopsis.
Definition/Diagnostic Criteria
Alpha thalassaemia is most frequently suspected initially on the basis of a routine full blood count. All affected individuals have a variable degree of anaemia (Hb), reduced mean corpuscular haemoglobin (MCH/pg), reduced mean corpuscular volume (MCV/fl) and a normal or slightly reduced level of the minor HbA2. These parameters are discussed in greater detail below. When the level of α globin synthesis falls below ~70% of normal, in the foetal period, excess γ globin chains form Hb Bart's which can be detected on routine Hb analysis [13–19]. In adult life, excess β globin chains form β4 tetramers of HbH in the cell and these can be identified by staining the peripheral blood with 1% brilliant cresyl blue (BCB)[20–22], or when present in sufficient quantity by routine Hb analysis[20, 23]. Previously α thalassaemia was confirmed by globin chain biosynthesis, when the α/β globin chain biosynthesis ratio was reduced to less than ~0.8[24–28]. All of these parameters are reduced in α thalassaemia but none of them alone or in combination can accurately or consistently predict the genotype for which directed molecular analysis of the α globin cluster is required and this is discussed below.
Epidemiology
Like all common globin gene disorders (sickle cell trait and β thalassaemia) α thalassaemia occurs at high frequencies throughout all tropical and subtropical regions of the world (Figure 1). In some areas, the carrier frequency of α thalassaemia may be as high as 80-90% of the population, almost at fixation[29–33]. It is thought that all of these globin gene disorders (including α thalassaemia) have been selected because in some way they protect carriers from the ravages of falciparum malaria. The micro epidemiological evidence supporting this is very strong[34, 35]. The mechanisms underlying this protection have been extensively studied but remain unknown. Of all globin disorders, α thalassaemia is the most widely distributed and therefore many individuals in these areas have interacting combinations of these variants (e.g. both α and β thalassaemia). Due to differences in the interactions between the various molecular defects underlying α thalassaemia (see below) HbH disease is predominantly seen in South East Asia, the Middle East and the Mediterranean. Similarly the Hb Bart's Hydrops foetalis syndrome is predominantly seen in South East Asia[36–41]. In passing it should be mentioned that ATR16, ATR-X and ATMDS syndromes show no geographical bias in their distributions.
The world distribution of haemoglobinopathies overlaps the geographic distribution of malaria. The prevalence has increased in previously non-endemic areas as a consequence of historical and recent immigration flows, slave-trade, trading activities and colonization. In all these regions there is a high prevalence of a thalassaemia. It is believed that carriers of α thalassaemia are protected against malaria and that natural selection is responsible for elevating and maintaining their gene frequencies.
Although the previously established distribution of α thalassaemia is represented in Figure 1, over the past few decades there have been massive population movements so that now the globin gene disorders, thought to be rarities in North European and North American clinical practice, have become major diagnostic and therapeutic challenges for our current health care systems[42].
Clinical description
The clinical phenotypes of most individuals with α thalassaemia are very mild and may not be noticed during life other than when a routine full blood count is examined. Patients with HbH disease have a variable phenotype and those with Hb Bart's hydrops foetalis have a lethal form of anaemia.
α Thalassaemia trait
Apart from mild to moderate microcytic hypochromic anaemia (detected on a routine blood count), carriers (heterozygotes) of α thalassaemia, whatever the molecular basis (see below), are clinically asymptomatic and the diagnosis (when made) is often established during a regular health check or during antenatal screening. Complaints related to more severe anaemias, such as fatigue, listlessness and shortness of breath are uncommon and almost certainly related to other concomitant disorders.
HbH disease
HbH disease is most frequently seen in patients who are compound heterozygotes for two different mutations or less frequently homozygotes for a moderately severe molecular defect. They usually produce less than 30% of the normal amount of α globin. The predominant features in HbH disease are anaemia (2.6-13.3 g/dl) with variable amounts of HbH (0.8-40%), occasionally accompanied by Hb Bart's in the peripheral blood. The patients usually have splenomegaly (which may be severe) and occasionally this is complicated by hypersplenism. Jaundice may be present in variable degrees and children may show growth retardation. Other complications include infections, leg ulcers, gall stones, folic acid deficiency and acute haemolytic episodes in response to drugs and infections[5, 43]. Older patients often have some degree of iron overload. The severity of the clinical features is clearly related to the molecular basis of the disease[5, 43, 44]. Patients with non-deletional types of HbH disease are more severely affected than those with the common deletional types of HbH disease[45–53].
Hb Bart's Hydrops Foetalis Syndrome
Infants with the Hb Bart's hydrops foetalis syndrome have the most severe deficiencies in α globin expression. While it most frequently results from the inheritance of no α globin genes from either parent, in some cases it results from the inheritance of a severe nondeletion mutation from one parent and no α genes from the other. Patients on the borderline between severe HbH disease and Hb Bart's hydrops foetalis syndrome are said to have HbH hydrops syndrome [45, 52, 54–56]. Physiologically non-functional homotetramers γ4 and β4 make up most of the haemoglobin in the erythrocytes in infants with the Bart's hydrops foetalis syndrome. They also have variable amounts of an embryonic Hb Portland (ζ2γ2), which is the only functional Hb in these infants and must be the only oxygen carrier keeping these infants alive. The clinical features are those of a pale oedematous infant with signs of cardiac failure and prolonged intra-uterine anaemia (Figure 2). Pronounced hepatosplenomegaly, retardation in brain growth, skeletal and cardiovascular deformities and gross enlargement of the placenta are characteristic features. Infants with the Hb Bart's hydrops foetalis syndrome almost always either die in utero (23-38 weeks) or shortly after birth, although few cases have been described in which the neonate is given intensive life-support therapy and treated with blood transfusion [57–60].
The Haemoglobin Bart's hydrops syndrome. a. peripheral blood film with immature red-cell precursors and hypochromic, microcytic, red cells showing anisocytosis and poikilocytosis; b. stillborn hydropic infant [5].
Aetiology (Molecular Basis)
In normal individuals α globin synthesis is regulated by four α globin genes two on each copy of chromosome 16 (in band 16p13.3 Figure 3) and this genotype is written as αα/αα. Expression of these genes is dependent on remote regulatory elements (named Multispecies Conserved Sequences or MCS-R1 to R4) located far upstream of the α globin genes in the introns of a flanking, widely expressed gene (Figure 3). Alpha thalassaemia most frequently results from deletion of one (-α) or both (--) α genes from the chromosome. Occasionally point mutations in critical regions of the α2 (αTα) or α1 (ααT) genes may cause, so-called, nondeletional α thalassaemia. Very rarely, α thalassaemia results from deletion of the MCS-R regulatory elements (written as (αα)T), in all of these deletions MCS-R2 is always removed and thus appears to be the major regulatory element. When a mutation(s) completely abolishes expression from a chromosome this is called α0-thalassaemia and when the mutation(s) only partially downregulate expression from the chromosome this is called α+-thalassaemia.
The structure of the α-globin gene cluster on chromosome 16. The telomere is shown as an oval, genes in the region are shown as boxes. The α-globin regulatory region (MCS-R 1 to 4) is indicated as vertical bars. The scale is in kilobases as indicated above. The alpha-gene cluster is enlarged showing the traditional gene names above and the HGVS gene names below. The table below shows the classification of gene defects and phenotypic expression.
α+-thalassaemia due to deletions
The α-globin genes are embedded within two highly homologous 4 kb duplication units [61–65]. One very common α-thalassaemia deletion is the rightward deletion, a 3.7 kb deletion caused by reciprocal recombination between Z segments producing a chromosome with only one functional α-gene (α-3.7 or rightward deletion) causing α-thalassaemia and an α-triplication allele without a thalassaemic effect (Figure 4). Likewise a reciprocal recombination between mispaired X-boxes results in a 4.2 kb deletion, called leftward deletion (-α4.2) [61, 66–68]. An increasing number of deletions resulting in the loss of a single α-gene are reported due to non-homologous recombination events, most of which are rare, or highly region specific. The most common α+-thalassaemia deletions are shown in Figure 5. More extensive overviews of all deletions are reported elsewhere (in: Disorders of Hemoglobin Cambridge University Press 2009) [69, 70].
Deletions that cause α+-thalassaemia. The homologous duplication units X, Y and Z in which the α-genes are embedded are indicated as colored boxes. A cross-over between the mis-paired Z boxes during meiosis gives rise to the -α3.7 and αααanti 3.7 chromosomes. Cross-over between misaligned X-boxes give rise to -α4.2 and αααanti 4.2.
α+-thalassaemia due to non-deletion types of α-thalassaemia
Alpha-thalassaemia is more frequently caused by deletion than single point mutations or nucleotide insertions and deletions involving the canonical sequences controlling gene expression. In general the non-deletion α+-thalassaemia determinants may give rise to a more severe reduction in α-chain synthesis than the -α deletion type of chromosomes. Many mutations have been described affecting mRNA processing, mRNA translation, and α-globin stability. Table 1 shows all the currently known non-deletion mutants causing α+-thalassaemia. Of these the most common non-deletional variants are the αIVSI(-5 nt)α (in Mediterraneans), polyadenylation site mutations α2AATAAG, α2AATGAA and α2AATA-- (in the Mediterranean and Middle East)[71–74], termination codon mutations leading to elongated Hb variants, such as Hb Constant Spring (HbCS), Hb Icaria, Hb Koya Dora, Hb Seal Rock and Hb Paksé (middle East, Mediterranean and South East Asia) [75–79] and structural mutations causing highly unstable α-globin variants; for example, Hb Quong Sze, Hb Suan Dok, Hb Petah Tikvah, Hb Adana, Hb Aghia Sophia [54, 80–84]. These common mutations are summarised in Tables 1 and 2. A regularly updated overview is provided by the HbVar web-site [85].
α0-thalassaemia due to deletions
The complete or partial deletion of both α-genes in cis results in no α-chain synthesis directed by these chromosomes in vivo (Figures 6 and 7a). Homozygotes for such deletions have the Hb Bart's Hydrops Foetalis Syndrome. Many deletions were described which remove the ζ- and α-genes and although heterozygotes appear to develop normally, it is unlikely that homozygotes could survive even the early stages of gestation since neither embryonic (ζ2γ2) nor foetal (α2γ2) haemoglobins could be made. Rare deletions causing α0-thalassaemia remove the regulatory region, which lies 40-50 kb upstream of the α-globin gene cluster leaving the α-genes intact. This region composed of four multispecies conserved sequences (MCS), called MCS-R1 to R4, correspond to the previously identified erythroid-specific DNAse1 hypersensitive sites referred to as HS-48, HS-40, HS-33 and HS-10. Of these elements, only MCS-R2 (HS-40), 40 kb upstream from the ζ globin mRNA cap-site has been shown to be essential for α globin expression. An overview showing all currently known (αα)T deletions is given in Figure 7b, a regularly updated summary is given elsewhere (deletions are reviewed in detail in Higgs et al Disorders of Hemoglobin Cambridge University Press 2009 [69].
A different spectrum of both α+- and α0-thalassaemia mutations is often found in different populations as indicated in Table 2 {Bain, 2006 126/id}. Ethnic origin may therefore guide molecular diagnosis. Knowledge of the mutations found in a specific population may allow strategic choice in laboratory diagnostics, especially in selection of the molecular techniques to be applied.
Genotype/Phenotype Correlations
Although there are now ~128 different molecular defects known to cause α thalassaemia and an ever increasing number of potential interactions, the clinical phenotypes (broadly classified as α thalassaemia trait, HbH disease and Hb Bart's hydrops foetalis) resulting from the interactions between these various molecular defects can be simply summarised as in Table 3. The severity of the clinical phenotype correlates very well with the degree of α globin chain deficiency. An important additional point is that, in general, interactions involving non-deletional forms of α+-thalassaemia result in a more severe phenotype than in those with deletional forms of α+-thalassaemia [69, 87–100].
Diagnosis and diagnostic methods
Initial laboratory testing should include a complete blood count with red cell indices, HPLC or Hb electrophoresis and eventually α/β-globin chain synthesis ratio measurement. The latter procedure, however, is sometimes bypassed by DNA analysis as a less complicated method to diagnose α-thalassaemia.
Haematology
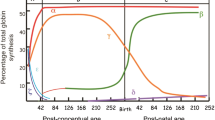
The red blood cell indices in patients with various genotypes associated with α-thalassaemia are depicted in figure 8 and 9. In general, the degree of microcytic (low MCV), hypochromic (low MCH) anaemia (low Hb) depends roughly on the number of α genes mutated and correlates well with the reduction in α-chain synthesis predicted for each mutant [5, 44, 101]. The combined use of HPLC and Capillary Electrophoresis to separate abnormal haemoglobin fractions is of particular importance to demonstrate HbH in individuals with HbH disease (figure 10) and Hb Bart's in newborns carrying α-thalassaemia determinants or any Hb variant associated with an α-thalassaemia phenotype (figure 11). Hb Bart's is found in a large proportion of neonates with α-thalassaemia but does not detect all cases with mild α-3.7/αα interactions and does not clearly distinguish the various α thalassaemia genotypes [11, 19, 102]. A reduction in HbA2 level is sometimes indicative of α-thalassaemia trait. Although this nicely distinguishes α and β thalassaemia trait it can hardly be relied upon as a guide to the degree or type of α thalassaemia. A reduction in the level of HbA2 is only distinctive in patients with HbH disease (see figure 12)[103]. Staining the peripheral blood cells with 1% Brilliant Cresyl Blue is a sensitive method to visualise inclusion bodies in the red cells. The typical inclusion-body cells have a golf-ball like appearance with stippling regularly distributed over a blue stained background (Figure 13). They appear occasionally (one to two cells in approximately 10 fields 1000× magnification) in carriers of the --/αα genotype and in carriers of many nondeletional defects. Numerous red cells containing inclusions can be seen in the BCB-stained peripheral blood smears of patients with HbH disease.
Red blood cell indices in patients with various genotypes associated with α-thalassaemia. The bar shows the mean and standard deviation. a. Haemoglobin level (Hb in g/dl), b. Red Cell Count (RBC indicated as × 1012/l), these are sex-dependent (blue for male distribution, pink female distribution). (adapted from Higgs 1993, Wilkie 1991) [44, 101].
HPLC and Capillary Hb electrophoresis patterns of a neonate with α thalassaemia trait (--/αα) and a significant amount of Hb Bart's (γ4 tetramers). Hb Bart's in newborns with α thalassaemia disappears rapidly after birth. In newborns with Hb H disease, Hb Bart's will be substituted by HbH after birth. In Hb Bart's hydrops foetalis syndrome due to homozygosity of α0-thalassaemia only Hb Bart's is seen.
An inclusion body positive cell seen in Brilliant Cresyl Blue stained red cells of a α0-thalassaemia carrier. Inclusion Bodies are β4-tetramers precipitating on the red cell membrane, which damages the membrane and induces haemolysis. HbH is unstable and inclusion body positive cells are more difficult to find in older blood samples. The number of inclusion body cells seen after staining is much lower in α0-thalassaemia carriers than in patients with HbH disease (1 in 5-10 fields versus several per field at 1000× microscopic magnification).
Alpha/beta-globin chain synthesis
Measuring the ratio of α- and β-globin chain synthesis is the most direct approach (at the protein level) to diagnose α-thalassaemia. The procedure was first described by Weatherall and Clegg in 1965 [27] and consists of several steps, including removal of white blood cells, reticulocyte enrichment, in vitro globin chain synthesis in the presence of radio-actively labelled Leucine, separation of the newly synthesized, radio-actively labelled α- and β-globin chains and measurement of the radio-active signal. If the α/β ratio appears lower than ~0.8 this is indicative of α-thalassaemia, a ratio around 0.75 being consistent with the loss of expression of a single α gene (-α/αα), 0.5 for two α genes (--/αα) and 0.25 for three α-genes (--/-α) [24, 25, 27, 28].
Molecular analysis
Over the past 30 years it has become increasingly possible to diagnose α thalassaemia accurately and define the precise defects underlying these disorders using a variety of molecular genetic approaches. Ultimately, most α globin rearrangements have been characterised by Southern blotting and DNA sequence analysis. However, for today's diagnostic demands these techniques are far too laborious to apply in each case, and from the original work defining these mutations, rapid screening assays have been developed.
Gap-PCR has been developed for the 7 most common α-thalassaemia deletions. This method is applied to detect the 2 most common α+ thalassaemia deletions -α3.7 and α-4.2 and the 5 α0-thalassaemia deletions -(α)20.5, - - SEA, - - Med I, - - Thai and - - Fil [104–106].
When a point mutation (non-deletional mutation) is suspected re-sequencing the α genes has become a routine procedure. The α genes are relatively small (~1.2 kb) which allows them to be sequenced rather easily compared to many other genes involved in human genetic disease, like for instance Duchenne Muscular Dystrophy (DMD gene; ~2.3 Mb), Cystic Fibrosis (CF-gene; ~250 kb) and Breast Cancer (BRCA1 and BRCA2 genes, ~16 and ~10 kb respectively)[107–109]. However, the GC-richness and the high homology between the duplicated α-genes require the use of high fidelity, heat stable polymerases, specific reaction conditions (using DMSO and betaine) and limits the choice of specific primers for PCR. The α-genes can be conveniently sequenced in two overlapping fragments for each of the duplicated α1 and α2 genes [19, 110, 111].
For suspected but currently unknown rearrangements, Southern blotting or MLPA analysis may be used. Southern blot is the classical method to detect deletions causing α-thalassaemia [112–117]. More recently Multiplex Ligation-dependent Probe Amplification (MLPA) is used, based on ligation of multiple probe-pairs hybridised across a (usually large) region of interest (Figure 14), followed by semi-quantitative amplification using universal-tag PCR primers and subsequently fragment analysis. This is a valuable alternative for Southern blot analysis and a supplementary method to gap-PCR when investigating known and unknown deletions causing α-thalassaemia [111, 118–120].
The principle of Multiplex Ligation dependent Probe Amplification (MLPA). a. Probe pairs at different locations along the region of interest are hybridised specifically head-to-tail to the target sequence and subsequently ligated. The ligated probes are amplified by quantitative PCR using fluorescent labelled primers complementary to the tag-sequences and separated by capillary electrophoresis on an automated fragment analyzer. b. peak heights represent the amount of amplified product of each separate probe pair. c. By dividing the peak heights of the patient sample and a normal control for each fragment, the ratio's of 0.5 shown in the graph mark the deletion of certain probes located along the genome, indicating the presence of a deletion of one allele.
Differential diagnosis
Sometimes carriers of α+-thalassaemia present with normal haematology, especially carriers of -α3.7 and nondeletional mutations affecting the α1-gene. Such individuals may be normocytic or borderline hypochromic without anaemia. These can only be found by chance during routine molecular analysis for haemoglobinopathies.
Occasionally, especially in countries where thalassaemia is uncommon, α-thalassaemia trait may be confused with iron deficiency anaemia, especially when the iron status is not carefully assessed. Haematological parameters for thalassaemia and iron deficiency are quite similar therefore ferritin levels should be measured. If the microcytic hypochromic parameters persist in a patient with normal levels of ferritin or Zinc Protoporphyrin (ZPP, a measure for long-lasting iron depletion), elevated RBC and normal (or low) HbA2, (especially in patients originating from areas where haemoglobinopathies are common) there is a good chance that the individual is a carrier of α-thalassaemia. Molecular analysis is usually required, especially in silent α-thalassaemia and α-thalassaemia trait to confirm the haematological observations.
There is a difference in clinical severity between deletional (most common) and non-deletional HbH disease [43, 47, 69, 89, 91, 94–96, 98, 99]. The clinical diagnosis of deletional HbH disease (the mildest form) is often made only after the detection of complications, such as exacerbations of the anaemia induced by infections, growth failure (in children) or findings of splenomegaly [5, 43, 121, 122]. The laboratory findings show a pronounced microcytic hypochromic anaemia and the presence of inclusion bodies. HbH and Hb Bart's are fast moving haemoglobins appearing on electrophoresis or HPLC, however, they are unstable and may go undetected. The more severe forms of HbH disease are predominantly those involving non-deletion mutations, of which Hb CS is the most common in South-East Asia. This form is characterized by a significantly more ineffective erythropoiesis and erythroid apoptosis than the deletion types of HbH disease. The haemoglobin is lower (on average 2 g/dL), but the MCV higher due to overhydration of cells containing HbCS [2, 123–127].
Hydrops Foetalis without α-thalassaemia is a common non-specific finding in a wide variety of foetal and maternal disorders [128–131]. The distinguishing features of the Hb Bart's hydrops foetalis syndrome is the presence of Hb Bart's and the total absence of HbF, which is easily differentiated by HPLC or Hb-electrophoresis. Although there have been a few reports of Hydrops Foetalis infants with very low levels of α-chain synthesis and HbH hydrops [45, 52, 54, 55, 99, 127].
Genetic counselling and antenatal diagnosis
When both parents carry an αo thalassaemia mutation (--/αα) the risk of their offspring having Hb Bart's hydrops foetalis is 1:4 (25%). When one parent carries αo thalassaemia (--/αα) and the other carries an α+ thalassaemia (-α/αα) the risk of their offspring having HbH disease is 1:4 (25%). If the carrier of α+ thalassaemia is a homozygote clearly the risk of HbH disease is 1:2 (50%). Since there are many different alleles of αo and α+ thalassaemia, genetic counselling may be more complex than outlined in this simple model.
In families with α thalassaemia the main reason for offering prenatal diagnosis is to avoid pregnancies with the Hb Bart's hydrops foetalis syndrome which causes neonatal death. Continued pregnancy may also present a considerable risk to the mother. Prenatal diagnosis for Hb Bart's is offered when both parents are found to be carriers of α0-thalassaemia trait. This is of most importance in individuals of South East Asian origins. Although some reports have demonstrated the feasibility of treating this syndrome, the lack of knowledge of the long-term prognosis and the capacity for treating such individuals probably do not justify changing the conventional management of offering prenatal diagnosis and selective abortion for Hb Bart's Hydrops Foetalis syndrome.
The syndrome of HbH disease is usually mild (thalassaemia intermedia) but there is considerable variability in the clinical and haematological severity. Although, precise characterisation of the mutations involved allows some prediction of the severity of the disease this is by no means certain, which makes prenatal diagnosis offered to parents at risk of having a child with HbH disease a complicated ethical issue. Most cases resulting from simple deletion of the α globin genes are mildly affected. Nearly all severe cases have at least one nondeletional allele. However the clinical course can be influenced by other genetic factors, environmental factors and infections. In rare cases the interaction of α0-thalassaemia with a non-deletional α+-thalassaemia allele has led to individuals with hydrops foetalis syndrome [54, 99, 127]. When there is a risk of such severely affected individuals there may be a case for considering prenatal diagnosis.
Management including treatment
Alpha thalassaemia trait
Carriers of α+- or α0-thalassaemia alleles generally do not need treatment, because their anaemia is either very mild or absent due to a compensating high red blood cell count. On the other hand, once a diagnosis of α thalassaemia trait is made, there is a tendency to discard iron-deficiency as a subsequent cause of anaemia. Carriers of α thalassaemia can be anaemic as a consequence of co-existing nutritional deficiencies, such as iron deficiency, folate or vitamin B12 deficiencies and should be managed correctly from this point of view. Of course prophylactic iron should never be given to carriers of α thalassaemia who are at risk of developing iron overload if treated inappropriately.
HbH disease
HbH disease may be a mild disorder, but recent studies suggest its clinical course is often more severe than previously recognized [43, 122, 123, 125–127]. As discussed above, the type of mutation influences the clinical severity of HbH disease. The most common form is the deletion type, which causes a milder form of HbH disease. These patients may require intermittent transfusion therapy especially during intercurrent illness. Chronic transfusion therapy is very uncommonly required in this group. However, patients with non-deletional types of HbH disease may have moderately severe splenomegaly and require more regular transfusion and ultimately splenectomy [5, 69, 125]. In some studies almost half of such patients have required repeated transfusions, particularly in early infancy and later adulthood [2, 5, 69, 124, 132]. However, there is a marked clinical variation in both categories. Iron overload is uncommon in HbH disease patients (compared with β thalassaemia) but has been recorded in older patients (>45 years) and those treated with regular blood transfusion.
Hb Bart's Hydrops Foetalis Syndrome
Most pregnancies in which the foetus is known to have the Bart's hydrops foetalis syndrome are terminated. In a very small number of cases intra-uterine transfusions following early detection of homozygous α0-thalassaemia have resulted in the birth of non-hydropic infants, some without significant neurological or congenital abnormalities, however, most survivors experience a stormy perinatal course and a high prevalence of congenital urogenital and limb defects [5, 133–137]. Affected infants who survive are good candidates for haematopoietic stem cell transplantation[60, 138]. Obstetric complications and the necessity for long-term transfusion therapy are however serious arguments for counselling and selective abortion. Increased risk of both maternal and foetal morbidity should be taken into account when counselling couples at risk for having a child affected with this syndrome [5, 44, 134].
Prognosis
There is no reason to think that carriers for α thalassaemia have any altered prognosis for life compared to the normal population. The prognosis for patients with HbH disease who are newly emerging in previously non-endemic countries, like Northern Europe and Northern America, is less clear. Anecdotally many patients with HbH disease appear to lead a normal life in all respects. Some even remain undiagnosed throughout their lives. However, detailed actuarial studies are not available. When complications arise, of course the outcome depends on the awareness and availability of health care systems. Certainly some complications suffered by patients with HbH disease are life threatening in the absence of adequate medical care [5, 44, 123, 124]. A long term problem for all patients with HbH disease is the unwanted accumulation of iron which may be more of a problem for those with severe HbH disease with non-deletional α- thalassaemia [43, 139, 140].
Clearly, previously undiagnosed and untreated infants with the Hb Bart's hydrops foetalis syndrome die in the perinatal period. The recent attempts to rescue infants with this syndrome either by intra-uterine transfusion or by transfusion in the perinatal period have met with variable success. As discussed above many infants develop other irreversible abnormalities during foetal life and even with rescue the infant will be required, either to receive lifelong blood transfusion and iron chelation therapy, or bone marrow transplantation with its attendant risks.
Unresolved questions
-
1.
How is the expression of genes in the α- (and β-) globin gene cluster regulated and how can it be influenced? A detailed understanding of globin gene regulation might hold the key to developing new treatments for both α and β thalassaemia.
-
2.
What other factors (genetic and environmental) influence the clinical severity of HbH disease and might explain the large variability even between individuals with the same α globin genotypes?
-
3.
What role does α-thalassaemia play in modifying the natural history of sickle cell disease and β-thalassaemia major? These interactions are not always well understood.
-
4.
In what way are carriers of α-thalassaemia protected from some of the effects of malaria?
References
Petrou M, Brugiatelli M, Old J, Hurley P, Ward RH, Wong KP, Rodeck C, Modell B: Alpha thalassaemia hydrops fetalis in the UK: the importance of screening pregnant women of Chinese, other South East Asian and Mediterranean extraction for alpha thalassaemia trait. Br J Obstet Gynaecol. 1992, 99: 985-989.
Chui DH, Waye JS: Hydrops fetalis caused by alpha-thalassemia: an emerging health care problem. Blood. 1998, 91: 2213-2222.
Liang ST, Wong VC, So WW, Ma HK, Chan V, Todd D: Homozygous alpha-thalassaemia: clinical presentation, diagnosis and management. A review of 46 cases. Br J Obstet Gynaecol. 1985, 92: 680-684.
Nakayama R, Yamada D, Steinmiller V, Hsia E, Hale RW: Hydrops fetalis secondary to Bart hemoglobinopathy. Obstet Gynecol. 1986, 67: 176-180. 10.1097/00006250-198602000-00004.
Weatherall DJ, Clegg JB: The Thalassaemia Syndromes. 2001
Higgs DR, Buckle V, Gibbons R, Steensma D: Unusual Types of Alpha Thalassaemia. Disorders of Hemoglobin second edition. Cambridge University Press;2009.
Wilkie AO, Buckle VJ, Harris PC, Lamb J, Barton NJ, Reeders ST, Lindenbaum RH, Nicholls RD, Barrow M, Bethlenfalvay NC, et al.: Clinical features and molecular analysis of the alpha thalassemia/mental retardation syndromes. I. Cases due to deletions involving chromosome band 16p13.3. Am J Hum Genet. 1990, 46: 1112-1126.
Gibbons R: Alpha thalassaemia-mental retardation, X linked. Orphanet J Rare Dis. 2006, 1: 15-10.1186/1750-1172-1-15.
Gibbons RJ, Picketts DJ, Villard L, Higgs DR: Mutations in a putative global transcriptional regulator cause X-linked mental retardation with alpha-thalassemia (ATR-X syndrome). Cell. 1995, 80: 837-845. 10.1016/0092-8674(95)90287-2.
Wilkie AO, Zeitlin HC, Lindenbaum RH, Buckle VJ, Fischel-Ghodsian N, Chui DH, Gardner-Medwin D, MacGillivray MH, Weatherall DJ, Higgs DR: Clinical features and molecular analysis of the alpha thalassemia/mental retardation syndromes. II. Cases without detectable abnormality of the alpha globin complex. Am J Hum Genet. 1990, 46: 1127-1140.
Wilkie AO, Gibbons RJ, Higgs DR, Pembrey ME: X linked alpha thalassaemia/mental retardation: spectrum of clinical features in three related males. J Med Genet. 1991, 28: 738-741. 10.1136/jmg.28.11.738.
Gibbons RJ, Pellagatti A, Garrick D, Wood WG, Malik N, Ayyub H, Langford C, Boultwood J, Wainscoat JS, Higgs DR: Identification of acquired somatic mutations in the gene encoding chromatin-remodeling factor ATRX in the alpha-thalassemia myelodysplasia syndrome (ATMDS). Nat Genet. 2003, 34: 446-449. 10.1038/ng1213.
Kutlar F, Reese AL, Hsia YE, Kleman KM, Huisman TH: The types of hemoglobins and globin chains in hydrops fetalis. Hemoglobin. 1989, 13: 671-683. 10.3109/03630268908998844.
Lie-Injo LE, Jo BH: A fast-moving haemoglobin in hydrops foetalis. Nature. 1960, 185: 698-10.1038/185698a0.
Lin TM, Eng HL, Kuo PL, Wu HL: Neonatal screening for alpha-thalassemia in southern Taiwan. J Formos Med Assoc. 1992, 91: 1213-1215.
Todd D, Lai MC, Beaven GH, Huehns ER: The abnormal haemoglobins in homozygous alpha-thalassaemia. Br J Haematol. 1970, 19: 27-31. 10.1111/j.1365-2141.1970.tb01598.x.
Velati C, Sampietro M, Sciariada L, Allievi E, Mosconi L, Cappellini MD, Fiorelli G: Neonatal screening for Hb Bart's in Italian subjects of heterogeneous regional origin born in Lombardy. Haematologica. 1983, 68: 20-29.
Weatherall DJ, Clegg JB, Boon WH: The haemoglobin constitution of infants with the haemoglobin Bart's hydrops foetalis syndrome. Br J Haematol. 1970, 18: 357-367. 10.1111/j.1365-2141.1970.tb01449.x.
Zorai A, Harteveld CL, Bakir A, Van DP, Falfoul A, Dellagi K, Abbes S, Giordano PC: Molecular spectrum of alpha-thalassemia in Tunisia: epidemiology and detection at birth. Hemoglobin. 2002, 26: 353-362. 10.1081/HEM-120016372.
Chui DH: Alpha-thalassemia: Hb H disease and Hb Barts hydrops fetalis. Ann N Y Acad Sci. 2005, 1054: 25-32. 10.1196/annals.1345.004.
Galanello R, Paglietti E, Melis MA, Giagu L, Cao A: Hemoglobin inclusions in heterozygous alpha-thalassemia according to their alpha-globin genotype. Acta Haematol. 1984, 72: 34-36. 10.1159/000206353.
Pan LL, Eng HL, Kuo CY, Chen WJ, Huang HY: Usefulness of brilliant cresyl blue staining as an auxiliary method of screening for alpha-thalassemia. J Lab Clin Med. 2005, 145: 94-97. 10.1016/j.lab.2004.11.019.
Ingram VM, Stretton AO: Genetic basis of the thalassaemia diseases. Nature. 1959, 184: 1903-1909. 10.1038/1841903a0.
Clegg JB, Weatherall DJ: Haemoglobin synthesis in alpha-thalassaemia (haemoglobin H disease). Nature. 1967, 215: 1241-1243. 10.1038/2151241a0.
Giordano PC, van Delft P, Batelaan D, Harteveld CL, Bernini LF: Haemoglobinopathy analyses in the Netherlands: a report of an in vitro globin chain biosynthesis survey using a rapid, modified method. Clin Lab Haematol. 1999, 21: 247-256. 10.1046/j.1365-2257.1999.00197.x.
Hunt DM, Higgs DR, Old JM, Clegg JB, Weatherall DJ, Marsh GW: Determination of alpha-thalassaemia phenotypes by messenger RNA analysis. Br J Haematol. 1980, 45: 53-10.1111/j.1365-2141.1980.tb03810.x.
Weatherall DJ, Clegg JB, Naughton MA: Globin synthesis in thalassaemia: an in vitro study. Nature. 1965, 208: 1061-1065. 10.1038/2081061a0.
Weatherall DJ, Clegg JB: Haemoglobin synthesis in thalassaemia. Biochem J. 1970, 119: 68P.
Bernini L: Geographic distribution of alpha-thalassemia. Disorders of Hemoglobin. first edition. Edited by: Steinberg MH, Forget BG, Higgs DR, Nagel RL. Cambridge University Press; 2001:878-894.
Flint J, Harding RM, Clegg JB, Boyce AJ: Why are some genetic diseases common? Distinguishing selection from other processes by molecular analysis of globin gene variants. Hum Genet. 1993, 91: 91-117. 10.1007/BF00222709.
Flint J, Harding RM, Boyce AJ, Clegg JB: The population genetics of the haemoglobinopathies. Baillieres Clin Haematol. 1993, 6: 215-262. 10.1016/S0950-3536(05)80071-X.
Fodde R, Losekoot M, Broek van den MH, Oldenburg M, Rashida N, Schreuder A, Wijnen JT, Giordano PC, Nayudu NV, Khan PM: Prevalence and molecular heterogeneity of alfa+ thalassemia in two tribal populations from Andhra Pradesh, India. Hum Genet. 1988, 80: 157-160. 10.1007/BF00702860.
Modiano G, Morpurgo G, Terrenato L, Novelletto A, Di RA, Colombo B, Purpura M, Mariani M, Santachiara-Benerecetti S, Brega A: Protection against malaria morbidity: near-fixation of the alpha-thalassemia gene in a Nepalese population. Am J Hum Genet. 1991, 48: 390-397.
Higgs DR, Weatherall DJ: The alpha thalassaemias. Cell Mol Life Sci. 2009, 66: 1154-1162. 10.1007/s00018-008-8529-9.
Weatherall DJ: Genetic variation and susceptibility to infection: the red cell and malaria. Br J Haematol. 2008, 141: 276-286. 10.1111/j.1365-2141.2008.07085.x.
Fischel-Ghodsian N, Vickers MA, Seip M, Winichagoon P, Higgs DR: Characterization of two deletions that remove the entire human zeta-alpha globin gene complex (- -THAI and - -FIL). Br J Haematol. 1988, 70: 233-238. 10.1111/j.1365-2141.1988.tb02469.x.
Fucharoen S, Winichagoon P: Thalassemia in SouthEast Asia: problems and strategy for prevention and control. Southeast Asian J Trop Med Public Health. 1992, 23: 647-655.
Liao C, Wei J, Li Q, Li J, Li L, Li D: Nonimmune hydrops fetalis diagnosed during the second half of pregnancy in Southern China. Fetal Diagn Ther. 2007, 22: 302-305. 10.1159/000100796.
Suwanrath-Kengpol C, Kor-anantakul O, Suntharasaj T, Leetanaporn R: Etiology and outcome of non-immune hydrops fetalis in southern Thailand. Gynecol Obstet Invest. 2005, 59: 134-137. 10.1159/000082997.
Waye JS, Eng B, Chui DH: Identification of an extensive zeta-alpha globin gene deletion in a Chinese individual. Br J Haematol. 1992, 80: 378-380. 10.1111/j.1365-2141.1992.tb08148.x.
Winichagoon P, Fucharoen S, Wasi P: The molecular basis of alpha-thalassemia in Thailand. Southeast Asian J Trop Med Public Health. 1992, 23 (Suppl 2): 7-13.
Vichinsky EP: Changing patterns of thalassemia worldwide. Ann N Y Acad Sci. 2005, 1054: 18-24. 10.1196/annals.1345.003.
Laosombat V, Viprakasit V, Chotsampancharoen T, Wongchanchailert M, Khodchawan S, Chinchang W, Sattayasevana B: Clinical features and molecular analysis in Thai patients with HbH disease. Ann Hematol. 2009, 88: 1185-1192. 10.1007/s00277-009-0743-5.
Higgs DR: alpha-Thalassaemia. Baillieres Clin Haematol. 1993, 6: 117-150. 10.1016/S0950-3536(05)80068-X.
Chan V, Chan TK, Liang ST, Ghosh A, Kan YW, Todd D: Hydrops fetalis due to an unusual form of Hb H disease. Blood. 1985, 66: 224-228.
Fucharoen S, Thonglairuam V, Winichagoon P: Hematologic changes in alpha-thalassemia. Am J Clin Pathol. 1988, 90: 193-196.
Galanello R, Pirastu M, Melis MA, Paglietti E, Moi P, Cao A: Phenotype-genotype correlation in haemoglobin H disease in childhood. J Med Genet. 1983, 20: 425-429. 10.1136/jmg.20.6.425.
Kanavakis E, Papassotiriou I, Karagiorga M, Vrettou C, Metaxotou-Mavrommati A, Stamoulakatou A, Kattamis C, Traeger-Synodinos J: Phenotypic and molecular diversity of haemoglobin H disease: a Greek experience. Br J Haematol. 2000, 111: 915-923. 10.1046/j.1365-2141.2000.02448.x.
Kattamis C, Tzotzos S, Kanavakis E, Synodinos J, Metaxotou-Mavrommati A: Correlation of clinical phenotype to genotype in haemoglobin H disease. Lancet. 1988, 1: 442-444. 10.1016/S0140-6736(88)91234-2.
Mirabile E, Samperi P, Di CA, Poli A, La SM, Schiliro G: Phenotype-genotype correlation in Sicilian patients with Hb H. Eur J Haematol. 2000, 65: 306-309. 10.1034/j.1600-0609.2000.065005306.x.
Origa R, Sollaino MC, Giagu N, Barella S, Campus S, Mandas C, Bina P, Perseu L, Galanello R: Clinical and molecular analysis of haemoglobin H disease in Sardinia: haematological, obstetric and cardiac aspects in patients with different genotypes. Br J Haematol. 2007, 136: 326-332. 10.1111/j.1365-2141.2006.06423.x.
Trent RJ, Wilkinson T, Yakas J, Carter J, Lammi A, Kronenberg H: Molecular defects in 2 examples of severe Hb H disease. Scand J Haematol. 1986, 36: 272-279. 10.1111/j.1600-0609.1986.tb01734.x.
Wajcman H, Traeger-Synodinos J, Papassotiriou I, Giordano PC, Harteveld CL, Baudin-Creuza V, Old J: Unstable and thalassemic alpha chain hemoglobin variants: a cause of Hb H disease and thalassemia intermedia. Hemoglobin. 2008, 32: 327-349. 10.1080/03630260802173833.
Chan V, Chan VW, Tang M, Lau K, Todd D, Chan TK: Molecular defects in Hb H hydrops fetalis. Br J Haematol. 1997, 96: 224-228. 10.1046/j.1365-2141.1997.d01-2017.x.
Ko TM, Hsieh FJ, Hsu PM, Lee TY: Molecular characterization of severe alpha-thalassemias causing hydrops fetalis in Taiwan. Am J Med Genet. 1991, 39: 317-320. 10.1002/ajmg.1320390314.
McBride KL, Snow K, Kubik KS, Fairbanks VF, Hoyer JD, Fairweather RB, Chaffee S, Edwards WH: Hb Dartmouth [alpha66(E15)Leu-->Pro (alpha2) (CTG-->CCG)]: a novel alpha2-globin gene mutation associated with severe neonatal anemia when inherited in trans with Southeast Asian alpha-thalassemia-1. Hemoglobin. 2001, 25: 375-382. 10.1081/HEM-100107874.
Beaudry MA, Ferguson DJ, Pearse K, Yanofsky RA, Rubin EM, Kan YW: Survival of a hydropic infant with homozygous alpha-thalassemia-1. J Pediatr. 1986, 108: 713-716. 10.1016/S0022-3476(86)81048-4.
Bianchi DW, Beyer EC, Stark AR, Saffan D, Sachs BP, Wolfe L: Normal long-term survival with alpha-thalassemia. J Pediatr. 1986, 108: 716-718. 10.1016/S0022-3476(86)81049-6.
Lee SY, Chow CB, Li CK, Chiu MC: Outcome of intensive care of homozygous alpha-thalassaemia without prior intra-uterine therapy. J Paediatr Child Health. 2007, 43: 546-550. 10.1111/j.1440-1754.2007.01131.x.
Yi JS, Moertel CL, Baker KS: Homozygous alpha-thalassemia treated with intrauterine transfusions and unrelated donor hematopoietic cell transplantation. J Pediatr. 2009, 154: 766-768. 10.1016/j.jpeds.2008.11.031.
Embury SH, Miller JA, Dozy AM, Kan YW, Chan V, Todd D: Two different molecular organizations account for the single alpha-globin gene of the alpha-thalassemia-2 genotype. J Clin Invest. 1980, 66: 1319-1325. 10.1172/JCI109984.
Hess JF, Schmid CW, Shen CK: A gradient of sequence divergence in the human adult alpha-globin duplication units. Science. 1984, 226: 67-70. 10.1126/science.6474190.
Lauer J, Shen CK, Maniatis T: The chromosomal arrangement of human alpha-like globin genes: sequence homology and alpha-globin gene deletions. Cell. 1980, 20: 119-130. 10.1016/0092-8674(80)90240-8.
Michelson AM, Orkin SH: Boundaries of gene conversion within the duplicated human alpha-globin genes. Concerted evolution by segmental recombination. J Biol Chem. 1983, 258: 15245-15254.
Zimmer EA, Martin SL, Beverley SM, Kan YW, Wilson AC: Rapid duplication and loss of genes coding for the alpha chains of hemoglobin. Proc Natl Acad Sci USA. 1980, 77: 2158-2162. 10.1073/pnas.77.4.2158.
Higgs DR, Pressley L, Clegg JB, Weatherall DJ, Higgs S, Carey P, Serjeant GR: Detection of alpha thalassaemia in Negro infants. Br J Haematol. 1980, 46: 39-46. 10.1111/j.1365-2141.1980.tb05985.x.
Higgs DR, Hill AV, Bowden DK, Weatherall DJ, Clegg JB: Independent recombination events between the duplicated human alpha globin genes; implications for their concerted evolution. Nucleic Acids Res. 1984, 12: 6965-6977. 10.1093/nar/12.18.6965.
Trent RJ, Higgs DR, Clegg JB, Weatherall DJ: A new triplicated alpha-globin gene arrangement in man. Br J Haematol. 1981, 49: 149-152. 10.1111/j.1365-2141.1981.tb07207.x.
Higgs DR: The molecular basis of alpha -thalassemia. Disorders of Hemoglobin. second edition. Edited by: Steinberg MH, Forget BG, Higgs DR, Nagel RL. Cambridge University Press; 2009.
Rugless MJ, Fisher CA, Old JM, Sloane-Stanley J, Ayyub H, Higgs DR, Garrick D: A large deletion in the human alpha-globin cluster caused by a replication error is associated with an unexpectedly mild phenotype. Hum Mol Genet. 2008, 17: 3084-3093. 10.1093/hmg/ddn205.
Hall GW, Higgs DR, Murphy P, Villegas A, de MA: A mutation in the polyadenylation signal of the alpha 2 globin gene (AATAAA-->AATA--) as a cause of alpha thalassaemia in Asian indians. Br J Haematol. 1994, 88: 225-227. 10.1111/j.1365-2141.1994.tb05008.x.
Harteveld CL, Losekoot M, Haak H, Heister GA, Giordano PC, Bernini LF: A novel polyadenylation signal mutation in the alpha 2-globin gene causing alpha thalassaemia. Br J Haematol. 1994, 87: 139-143. 10.1111/j.1365-2141.1994.tb04883.x.
Higgs DR, Goodbourn SE, Lamb J, Clegg JB, Weatherall DJ, Proudfoot NJ: Alpha-thalassaemia caused by a polyadenylation signal mutation. Nature. 1983, 306: 398-400. 10.1038/306398a0.
Yuregir GT, Aksoy K, Curuk MA, Dikmen N, Fei YJ, Baysal E, Huisman TH: Hb H disease in a Turkish family resulting from the interaction of a deletional alpha-thalassaemia-1 and a newly discovered poly A mutation. Br J Haematol. 1992, 80: 527-532. 10.1111/j.1365-2141.1992.tb04568.x.
Bradley TB, Wohl RC, Smith GJ: Elongation of the alpha-globin chain in a black family:interaction with HbG Philadelphia. [abstract]. clinical research. 1975, 23:
Clegg JB, Weatherall DJ, Milner PF: Haemoglobin Constant Spring--a chain termination mutant?. Nature. 1971, 234: 337-340. 10.1038/234337a0.
Clegg JB, Weatherall DJ, Contopolou-Griva I, Caroutsos K, Poungouras P, Tsevrenis H: Haemoglobin Icaria, a new chain-termination mutant with causes alpha thalassaemia. Nature. 1974, 251: 245-247. 10.1038/251245a0.
De Jong WW, Meera KP, Bernini LF: Hemoglobin Koya Dora: high frequency of a chain termination mutant. Am J Hum Genet. 1975, 27: 81-90.
Waye JS, Eng B, Patterson M, Chui DH, Olivieri NF: Identification of a novel termination codon mutation (TAA-->TAT, Term-->Tyr) in the alpha 2 globin gene of a Laotian girl with hemoglobin H disease. Blood. 1994, 83: 3418-3420.
Curuk MA, Dimovski AJ, Baysal E, Gu LH, Kutlar F, Molchanova TP, Webber BB, Altay C, Gurgey A, Huisman TH: Hb Adana or alpha 2(59)(E8)Gly-->Asp beta 2, a severely unstable alpha 1-globin variant, observed in combination with the -(alpha)20.5 Kb alpha-thal-1 deletion in two Turkish patients. Am J Hematol. 1993, 44: 270-275. 10.1002/ajh.2830440410.
Goossens M, Lee KY, Liebhaber SA, Kan YW: Globin structural mutant alpha 125Leu leads to Pro is a novel cause of alpha-thalassaemia. Nature. 1982, 296: 864-865. 10.1038/296864a0.
Honig GR, Shamsuddin M, Zaizov R, Steinherz M, Solar I, Kirschmann C: Hemoglobin Petah Tikva (alpha 110 ala replaced by asp): a new unstable variant with alpha-thalassemia-like expression. Blood. 1981, 57: 705-711.
Sanguansermsri T, Matragoon S, Changloah L, Flatz G: Hemoglobin Suan-Dok (alpha 2 109 (G16) Leu replaced by Arg beta 2): an unstable variant associated with alpha-thalassemia. Hemoglobin. 1979, 3: 161-174. 10.3109/03630267908998911.
Traeger-Synodinos J, Harteveld CL, Kanavakis E, Giordano PC, Kattamis C, Bernini LF: Hb Aghia Sophia [alpha62(E11)Val-->0 (alpha1)], an "in-frame" deletion causing alpha-thalassemia. Hemoglobin. 1999, 23: 317-324. 10.3109/03630269909090747.
Patrinos GP, Giardine B, Riemer C, Miller W, Chui DH, Anagnou NP, Wajcman H, Hardison RC: Improvements in the HbVar database of human hemoglobin variants and thalassemia mutations for population and sequence variation studies. Nucleic Acids Res. 2004, 32: D537-D541. 10.1093/nar/gkh006.
Bain BJ: Hemoglobinopathy diagnosis. second edition. Blackwell Publishing Ltd; 2006.
Cao A, Rosatelli C, Pirastu M, Galanello R: Thalassemias in Sardinia: molecular pathology, phenotype-genotype correlation, and prevention. Am J Pediatr Hematol Oncol. 1991, 13: 179-188. 10.1097/00043426-199122000-00015.
Eng B, Patterson M, Walker L, Hoppe C, Azimi M, Lee H, Giordano PC, Waye JS: Three new alpha-thalassemia point mutations ascertained through newborn screening. Hemoglobin. 2006, 30: 149-153. 10.1080/03630260600642021.
Galanello R, Aru B, Dessi C, Addis M, Paglietti E, Melis MA, Cocco S, Massa P, Giagu N, Barella S: HbH disease in Sardinia: molecular, hematological and clinical aspects. Acta Haematol. 1992, 88: 1-6. 10.1159/000204585.
Harteveld CL, Beijer C, Van DP, Zanardini R, Bernini LF, Giordano PC: alpha-thalassaemia as a result of a novel splice donor site mutation of the alpha1-globin gene. Br J Haematol. 2000, 110: 694-698. 10.1046/j.1365-2141.2000.02225.x.
Henderson S, Chapple M, Rugless M, Fisher C, Kinsey S, Old J: Haemoglobin H hydrops fetalis syndrome associated with homozygosity for the alpha2-globin gene polyadenylation signal mutation AATAAA-->. Br J Haematol. 2006, 135: 743-745. 10.1111/j.1365-2141.2006.06362.x.
Moi P, Cash FE, Liebhaber SA, Cao A, Pirastu M: An initiation codon mutation (AUG----GUG) of the human alpha 1-globin gene. Structural characterization and evidence for a mild thalassemic phenotype. J Clin Invest. 1987, 80: 1416-1421. 10.1172/JCI113220.
Noguera NI, Gonzalez FA, Davoli RA, Milani AC, Villegas A: A novel splice acceptor site mutation of the alpha2-globin gene causing alpha-thalassemia. Hemoglobin. 2001, 25: 311-315. 10.1081/HEM-100105224.
Olivieri NF, Chang LS, Poon AO, Michelson AM, Orkin SH: An alpha-globin gene initiation codon mutation in a black family with HbH disease. Blood. 1987, 70: 729-732.
Pressley L, Higgs DR, Clegg JB, Perrine RP, Pembrey ME, Weatherall DJ: A new genetic basis for hemoglobin-H disease. N Engl J Med. 1980, 303: 1383-1388. 10.1056/NEJM198012113032402.
Tabone P, Henni T, Belhani M, Colonna P, Verdier G, Godet J: Hemoglobin H disease from Algeria: genetic and molecular characterization. Acta Haematol. 1981, 65: 26-31. 10.1159/000207145.
Thein SL, Wallace RB, Pressley L, Clegg JB, Weatherall DJ, Higgs DR: The polyadenylation site mutation in the alpha-globin gene cluster. Blood. 1988, 71: 313-319.
Traeger-Synodinos J, Papassotiriou I, Karagiorga M, Premetis E, Kanavakis E, Stamoulakatou A: Unusual phenotypic observations associated with a rare HbH disease genotype (- -Med/alphaTSaudialpha): implications for clinical management. Br J Haematol. 2002, 119: 265-267. 10.1046/j.1365-2141.2002.03777.x.
Viprakasit V, Green S, Height S, Ayyub H, Higgs DR: Hb H hydrops fetalis syndrome associated with the interaction of two common determinants of alpha thalassaemia (--MED/(alpha)TSaudi(alpha)). Br J Haematol. 2002, 117: 759-762. 10.1046/j.1365-2141.2002.03427.x.
Whitelaw E, Proudfoot N: Alpha-thalassaemia caused by a poly(A) site mutation reveals that transcriptional termination is linked to 3' end processing in the human alpha 2 globin gene. EMBO J. 1986, 5: 2915-2922.
Wilkie AO: The alpha-thalassaemia/mental retardation syndromes: model systems for studying the genetic contribution to mental handicap. PhD Thesis. University of Oxford; 1991.
Higgs DR, Old JM, Pressley L, Clegg JB, Weatherall DJ: A novel alpha-globin gene arrangement in man. Nature. 1980, 284: 632-635. 10.1038/284632a0.
Delft van P, Lenters E, Bakker-Verweij M, de KM, Baylan U, Harteveld CL, Giordano PC: Evaluating five dedicated automatic devices for haemoglobinopathy diagnostics in multi-ethnic populations. Int J Lab Hematol. 2009, 31: 484-495. 10.1111/j.1751-553X.2009.01158.x.
Chong SS, Boehm CD, Higgs DR, Cutting GR: Single-tube multiplex-PCR screen for common deletional determinants of alpha-thalassemia. Blood. 2000, 95: 360-362.
Liu YT, Old JM, Miles K, Fisher CA, Weatherall DJ, Clegg JB: Rapid detection of alpha-thalassaemia deletions and alpha-globin gene triplication by multiplex polymerase chain reactions. Br J Haematol. 2000, 108: 295-299. 10.1046/j.1365-2141.2000.01870.x.
Tan ASC, Quah TC, Low PS, Chong SS: A rapid and reliable 7-deletion multiplex polymerase chain reaction assay for alpha-thalassemia. Blood. 2001, 98: 250-251. 10.1182/blood.V98.1.250.
Bellosillo B, Tusquets I: Pitfalls and caveats in BRCA sequencing. Ultrastruct Pathol. 2006, 30: 229-235. 10.1080/01913120500521281.
Richards CS, Grody WW: Prenatal screening for cystic fibrosis: past, present and future. Expert Rev Mol Diagn. 2004, 4: 49-62. 10.1586/14737159.4.1.49.
Stockley TL, Akber S, Bulgin N, Ray PN: Strategy for comprehensive molecular testing for Duchenne and Becker muscular dystrophies. Genet Test. 2006, 10: 229-243. 10.1089/gte.2006.10.229.
Molchanova TP, Pobedimskaya DD, Postnikov Y: A simplified procedure for sequencing amplified DNA containing the alpha 2- or alpha 1-globin gene. Hemoglobin. 1994, 18: 251-255. 10.3109/03630269409043628.
Traeger-Synodinos J, Harteveld CL: Disease services: Haemoglobinopathies. Molecular Diagnosis of Genetic Disease. third edition. Edited by: Rob Elles, Andrew Wallace. Totowa, New Jersey: Humana Press; 2009.
Higgs DR, Ayyub H, Clegg JB, Hill AV, Nicholls RD, Teal H, Wainscoat JS, Weatherall DJ: Alpha thalassaemia in British people. Br Med J (Clin Res Ed). 1985, 290: 1303-1306. 10.1136/bmj.290.6478.1303.
Higgs DR, Wainscoat JS, Flint J, Hill AV, Thein SL, Nicholls RD, Teal H, Ayyub H, Peto TE, Falusi AG: Analysis of the human alpha-globin gene cluster reveals a highly informative genetic locus. Proc Natl Acad Sci USA. 1986, 83: 5165-5169. 10.1073/pnas.83.14.5165.
Higgs DR, Vickers MA, Wilkie AO, Pretorius IM, Jarman AP, Weatherall DJ: A review of the molecular genetics of the human alpha-globin gene cluster. Blood. 1989, 73: 1081-1104.
Hill AV, Bowden DK, Trent RJ, Higgs DR, Oppenheimer SJ, Thein SL, Mickleson KN, Weatherall DJ, Clegg JB: Melanesians and Polynesians share a unique alpha-thalassemia mutation. Am J Hum Genet. 1985, 37: 571-580.
Kattamis AC, Camaschella C, Sivera P, Surrey S, Fortina P: Human alpha-thalassemia syndromes: detection of molecular defects. Am J Hematol. 1996, 53: 81-91. 10.1002/(SICI)1096-8652(199610)53:2<81::AID-AJH5>3.0.CO;2-#.
Tan J, Tay JS, Wong HB: Detection and molecular analysis of alpha and beta thalassaemia genes--recent developments in screening protocols. J Singapore Paediatr Soc. 1992, 34: 53-56.
Harteveld CL, Voskamp A, Phylipsen M, Akkermans N, den Dunnen JT, White SJ, Giordano PC: Nine unknown rearrangements in 16p13.3 and 11p15.4 causing alpha- and beta-thalassaemia characterised by high resolution multiplex ligation-dependent probe amplification. J Med Genet. 2005, 42: 922-931. 10.1136/jmg.2005.033597.
Schouten JP, McElgunn CJ, Waaijer R, Zwijnenburg D, Diepvens F, Pals G: Relative quantification of 40 nucleic acid sequences by multiplex ligation-dependent probe amplification. Nucleic Acids Res. 2002, 30: e57-10.1093/nar/gnf056.
White SJ, Vink GR, Kriek M, Wuyts W, Schouten J, Bakker B, Breuning MH, den Dunnen JT: Two-color multiplex ligation-dependent probe amplification: detecting genomic rearrangements in hereditary multiple exostoses. Hum Mutat. 2004, 24: 86-92. 10.1002/humu.20054.
Bernini LF, Harteveld CL: Alpha-thalassaemia. Baillieres Clin Haematol. 1998, 11: 53-90. 10.1016/S0950-3536(98)80070-X.
Slomp J, Bosschaart A, Dousma M, van ZR, Giordano PC, Bergh van den FA: [Acute anaemia in a Vietnamese patient with alpha-thalassaemia and a parvovirus infection]. Ned Tijdschr Geneeskd. 2006, 150: 1577-1582.
Chen FE, Ooi C, Ha SY, Cheung BM, Todd D, Liang R, Chan TK, Chan V: Genetic and clinical features of hemoglobin H disease in Chinese patients. N Engl J Med. 2000, 343: 544-550. 10.1056/NEJM200008243430804.
Chui DH, Fucharoen S, Chan V: Hemoglobin H disease: not necessarily a benign disorder. Blood. 2003, 101: 791-800. 10.1182/blood-2002-07-1975.
Cohen AR, Galanello R, Pennell DJ, Cunningham MJ, Vichinsky E: Thalassemia. Hematology Am Soc Hematol Educ Program. 2004, 14-34.
Lau YL, Chan LC, Chan YY, Ha SY, Yeung CY, Waye JS, Chui DH: Prevalence and genotypes of alpha- and beta-thalassemia carriers in Hong Kong -- implications for population screening. N Engl J Med. 1997, 336: 1298-1301. 10.1056/NEJM199705013361805.
Lorey F, Charoenkwan P, Witkowska HE, Lafferty J, Patterson M, Eng B, Waye JS, Finklestein JZ, Chui DH: Hb H hydrops foetalis syndrome: a case report and review of literature. Br J Haematol. 2001, 115: 72-78. 10.1046/j.1365-2141.2001.03080.x.
Arcasoy MO, Gallagher PG: Hematologic disorders and nonimmune hydrops fetalis. Semin Perinatol. 1995, 19: 502-515. 10.1016/S0146-0005(05)80057-6.
Holzgreve W, Curry CJ, Golbus MS, Callen PW, Filly RA, Smith JC: Investigation of nonimmune hydrops fetalis. Am J Obstet Gynecol. 1984, 150: 805-812.
Jauniaux E, Van ML, De MC, Moscoso G, Gillerot Y: Nonimmune hydrops fetalis associated with genetic abnormalities. Obstet Gynecol. 1990, 75: 568-572.
Nicolaides KH, Rodeck CH, Lange I, Watson J, Gosden CM, Miller D, Mibashan RS, Moniz C, Morgan-Capner P, Campbell S: Fetoscopy in the assessment of unexplained fetal hydrops. Br J Obstet Gynaecol. 1985, 92: 671-679.
Schrier SL, Bunyaratvej A, Khuhapinant A, Fucharoen S, Aljurf M, Snyder LM, Keifer CR, Ma L, Mohandas N: The unusual pathobiology of hemoglobin constant spring red blood cells. Blood. 1997, 89: 1762-1769.
Dame C, Albers N, Hasan C, Bode U, Eigel A, Hansmann M, Brenner R, Bartmann P: Homozygous alpha-thalassaemia and hypospadias--common aetiology or incidental association? Long-term survival of Hb Bart's hydrops syndrome leads to new aspects for counselling of alpha-thalassaemic traits. Eur J Pediatr. 1999, 158: 217-220. 10.1007/s004310051053.
Lee SY, Li CK, Ling SC, Shiu YK: Survival of homozygous alpha-thalassemia with aplasia/hypoplasia of phalanges and jejunal atresia. J Matern Fetal Neonatal Med. 2009, 1-3. 10.1080/14767050903156692.
Lucke T, Pfister S, Durken M: Neurodevelopmental outcome and haematological course of a long-time survivor with homozygous alpha-thalassaemia: case report and review of the literature. Acta Paediatr. 2005, 94: 1330-1333. 10.1111/j.1651-2227.2005.tb02096.x.
Ng PC, Fok TF, Lee CH, Cheung KL, Li CK, So KW, Wong W, Yuen PM: Is homozygous alpha-thalassaemia a lethal condition in the 1990s?. Acta Paediatr. 1998, 87: 1197-1199. 10.1080/080352598750031220.
Singer ST, Styles L, Bojanowski J, Quirolo K, Foote D, Vichinsky EP: Changing outcome of homozygous alpha-thalassemia: cautious optimism. J Pediatr Hematol Oncol. 2000, 22: 539-542. 10.1097/00043426-200011000-00014.
Zhou X, Ha SY, Chan GC, Luk CW, Chan V, Hawkins B, Lam YH, Liang RH, Lau YL: Successful mismatched sibling cord blood transplant in Hb Bart's disease. Bone Marrow Transplant. 2001, 28: 105-107. 10.1038/sj.bmt.1703104.
Chan V, Wong MS, Ooi C, Chen FE, Chim CS, Liang RH, Todd D, Chan TK: Can defects in transferrin receptor 2 and hereditary hemochromatosis genes account for iron overload in HbH disease?. Blood Cells Mol Dis. 2003, 30: 107-111. 10.1016/S1079-9796(03)00013-5.
Ooi GC, Chen FE, Chan KN, Tsang KW, Wong YH, Liang R, Chan V, Ngan H: Qualitative and quantitative magnetic resonance imaging in haemoglobin H disease: screening for iron overload. Clin Radiol. 1999, 54: 98-102. 10.1016/S0009-9260(99)91068-1.
Acknowledgements
The authors want to express their gratitude to all colleagues in the field who contributed to the present knowledge about α-thalassaemia and to all patients and their families for their cooperation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
The authors CLH and DRH have contributed equally to the draft of the manuscript. Both authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Harteveld, C.L., Higgs, D.R. α-thalassaemia. Orphanet J Rare Dis 5, 13 (2010). https://doi.org/10.1186/1750-1172-5-13
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1750-1172-5-13