Abstract
There are several unresolved issues through out the literature regarding the entity of primary lung lymphoma. Extensive literature review of this uncommon pathology is carried out.
By taking into consideration the reported experience, the author discuss the classification, clinical features, histological differential diagnosis, prognostic criteria, therapeutic management and outcome of primary lung parenchyma lymphocytic infiltrates.
Similar content being viewed by others
Introduction
Primary Lung Lymphoma (PLL) is a rare entity (0.4% of all lymphomas[1] & 3.6% of non- Hodgkins lymphomas[2]) of heterogenous group of patients with some common characteristics: 1) difficult to be diagnosed due to an indolent course (with a tendency to relapse) with a non specific clinical and radiological presentation 2) low diagnostic yield and 3) sometimes difficult to differentiate from pseudo-lymphomas and 4)overall good outcome especially in disease amenable to surgical resection.
The main diagnostic criterion for PLL is the absence of extra-pulmonary involvement. That means unilateral or bilateral involvement of the lung with or without hilar or mediastinal lumph node involvement and with or without chest wall involvement [3]. Therefore, in patients with biopsy-proven lymphoma of the lung, PLL is diagnosed if extra-pulmonary involvement is ruled out.
In this article we aim to review the literature in order to delineate from the surgeons prospective, the overall experience of the rare entity of PLL and also to bring up to date the variables leading to a favorable outcome following surgery.
Materials and methods
Pertinent medical literature in the English language was identified through a Medline computerized literature search and a manual search of selected articles using as Key-words: Primary pulmonary Lymphoma, Lung Lymphoma, Pseudolymphoma of the lung, Non-Hodgkin lymphoma of the lung or extranodal lymphoma. The search terms were combined using the Boolean operator term "or" to find all abstracts pertaining to the chosen search terms. These individual terms were then combined using the Boolean operator term "and" to find articles that contained information of all search terms (as per Greenhaligh et al)[4]. The reference lists of articles found through these searches were also reviewed for relevant articles. Links provided on the web sites of published articles were searched for relevant articles. The primary search yielded 81 relevant articles. Of those 14 were excluded as they pertained to pseudolymphoma.
The Ann Arbor pulmonary lymphoma staging system was used for classification
Stage
IE: Lung only, could be bilateral
II 1E: Lung and hilar lymph nodes
II 2E: Lung and mediastinal lymph nodes
II 2EW: Lung & chest wall or diaphragm
III: lung and lymph nodes below the diaphragm
IV: diffuse
Characteristics of the various reports
We reviewed the reported literature from 1966 to 2007. We divide the reports into 2 groups. The first group (Table 1 [5–62]) contains case reports with fewer patients compare to the second group (Table 2 [63–71]).
Results
Group A
58 reports were identified and reviewed. There were 309 cases of PLL. The largest series in this group [58] included 31 patients.
Non Hodgkin Lymphomas (nHL) consist the majority of PLL with mucosa-associated lymphoid tissue (MALTomas) being 70-80%. Hodgkin lymphoma was reported in a small number of cases 1.5-2.4%.
The course of the disease is long and indolent spanning from 1.5 to 108 months [31].
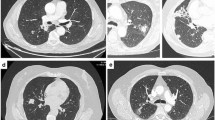
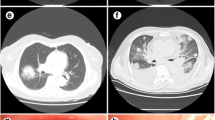
Radiological appearance have shown that non specific patchy opacities or mass-like consolidation was the case in the majority of the patients (up to 68%) and multiple nodules in more than 50% of the cases. [31, 57, 58].
Nodal involvement (stage II1E, II2E) was reported in 35%-45% of the cases [6, 18, 58].
Bronchoscopy obtained a diagnostic yield in 30%-40% [20, 48] of the cases and invasive surgical procedure revealed the diagnosis in up to 70% of the cases[20].
There was no uniform protocol throughout the literature regarding the indications for surgery. Despite nodal involvement (stage II 1E and 2E) surgery was advocated in few studies [33] and some authors concluded that several treatment methods can be used to achieve good outcomes [23].
Group B
The second group consisted of 506 reported cases of PLL.
In the majority of the studies the male to female ratio is variable (from 1/1 [68] to 1/2 [70]). Average age of disease presentation is 53±12 years [65, 68–70]. 83% of the patients have been reported to be above 40 years of age [65].
Symptoms are present in 2/3 of the patients (62.5% to 78% of patients) [69, 70]. The mean duration of symptoms was 5 months [65]. Mild symptoms with no resolving consolidation should be managed with a high index of suspicion.
Again, nHL consist the majority of PLL with MALTomas being 60-78% [69–71].
The radiographic appearance shows nodules or mass lesions in 60-72%,[69, 70]. Single lesions are present in 55% of the cases [65]. Multiple nodules are present in 40% of the patients [65, 67]. Bilateral disease varies in different reports: 21%. [68], 27%[65], 39% [70], 44% [69].
Nodal involvement (stage II1E, II2E) was reported in 28 to 39% of the cases [65, 69] and Pleural effusions 15-22%[69, 70].
There was again, no uniform protocol throughout the literature regarding the indications for surgery. Nevertheless, surgery was advocated in 60-70% of the patients. The MALToma patients tend to have complete resections. Broadly speaking, following surgery, patients had more favorable outcome [71].
Diagnosis
The role of monoclonal protein in the electrophoresis of serum protein: ie. Serum IgG >5000 mgr/dl has been stated in some reports [19, 21, 51]. Stained for Kappa & Lambda chains, using the immunoperoxidase technique on paraffin sections has been reported. Serum protein electrophoresis abnormalities could be present in up to 33% of the cases [65]. Serum or immunofluorescence monoclonal gammopathy should exclude pseudoL. Furthermore the presence of a serum monoclonal gammopathy is associated with worse prognosis [66].
The significant role of Broncho Alveolar Lavage (BAL) with a cell count of plasma cells of 40% and lymphocytes of 17% with prominence of CD19 positive lymphocytes has been reported by Umino et al [51]. IgG/albumin ratio 13 times higher and IL-6/albumin ratio 29 times higher in lavage fluid than in serum. Furthermore TBLB and immunohistochemical stains mainly CD20 could be helpful. DNA extraction from the surgical specimen and PCR reveals rearrangement band of the genes to the heavy chain immunoglobulin (Fr3a & VLJH primers) [51]. The diagnostic value of Cell surface markers analysis using fresh tissue was also stated in some reports [35, 65].
Staging workup should include bone marrow biopsy and CT of the abdomen to exclude extrathoracic disease. Lymphangiograms and bone scans could be part of the preoperative staging [65].
The role of PET scan is equivocal due to the low avidity and the multifocal nature of the disease. The low yield of bronchoscopy and Transcutaneous needle CT guided biopsy has been stated in few reports[13, 20]. There is however, a high role for VATS or open surgical lung biopsy with a diagnostic yield more than 90%.
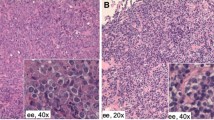
Histology
PLL arises from centrocyte-like cells normally present in bronchus associated lymphoid tissue. Monomorphic cell population and invasion of bronchial cartilage, pleura or lymph nodes are suggestive of malignancy. Some cases of PLL appeared as complications of a pre existing dysimmune disease (Pigeon breeder disease), Gougerot-Sjogren, Lymphomatoid granulomatosis (LYG) and Liebows lymphomatoid granulomatosis)[12, 19, 32].
The gross classification of Low Grade malignant Lymphoma higher grade MALTomas (large cell type) and others (ie. Follicular, Diffuse large B-cell, anaplastic large cell)
has been used through out the literature. A detail attempt to estimate the biological potential of lymphomas by their histologic type and correlate this with outcome was attempted with the use of various systems of histologic classification of non Hodgkins lymphomas.
Although from the surgeons prospective the classification seems complicated, one could grossly divide the tumors into small round lymphocytes (50-60%), with varying degrees of plasmacytic change, ("plasmacytoid" well differentiated) and large lymphocytic tumors.
More specifically the Kiel classification [32] essentially differentiates Lymphoplasmacytic (LP) from Centroblastic lymphoma (CB). The LP type is the most common (55-65%) [65]. The tumor is composed of uniform small round lympocytes; they often grow as solid masses; infiltration of bronchial and vascular wall is often however necrosis does not present. The incidence of recurrence is less than 35% through out the literature [65].
Contrary CB type makes up 40% of the cases. It consists of a centrocytic diffuse or follicular population including the rare immunoblastic type. In general those tumors are aggressive, present as pulmonary infiltrates therefore are not amenable to surgical resection and have a higher tendency to recur.
The term MALTomas was described by Bienenstock et al [72]. They are the most common amongst nHL (76% according to Cordier et al). The MALTomas are characterized by: extranodal, small lymphocytic b-cell tumor, cellular heterogeneity, infiltration of the bronchial mucosa by centrocyte cells and presence of reactive lymphoid follicles. The etiology of this mucosal transformation is probably acquired in response to long-term exposure to various antigenic stimuli; Synchronus MALTomaS involving the lung, stomach & ocular adnexa have been reported in the literature [68, 70].
Pulmonary lymphomas of nH type could be divided into 4 groups [48]according to the properties and behavior of the tumor: B-cells small or medium size (those tumors are frequently associated with consolidations and air bronchograms), B-cell large lymphoid cell (frequently radiologic presentation is consistent with a mass) and T-cell tumors (bad prognosis). Furthermore the REAL classification sums up the histological variations of all types of lymphomas [73] however, from the surgical prospective it is detailed and probably not widely applicable.
Differentiating between Lymphoma (especially Lymphoplasmacytic (LP) type) and pseudolymphoma
Mixture of mature lymphocytes and plasma cells with reactive follicles are suggestive of pseudolymphoma.
Pulmonary pseudolymphoma is a rare lesion; Up till 1980, only 30 cases were reported in the literature. True lymphoma was developed in four cases [34].
The diagnosis of pseudolymphoma is based on: 1) pulmonary nodules composed of cytologically benign lymphoid cells 2) presence of infiltrates with plasma cells, histiocytes and monocytes 3) presence of germinal centers. In addition, the presence of pleural effusion does not preclude the diagnosis of pseudolymphoma.
Immunological studies aim to define whether the lymphoid proliferation is monoclonal or polyclonal. It is suggested that PPL arises from centrocyte-like cells normally present in bronchus -associated lymphoid tissue. In addition to malignant population reactive follicles and polytypic plasma cells are frequently present so one should be aware that cases previously diagnosed as pseudo-lymphoma or lymphoid interstitial pneumonia need to be reconsidered. Moreover when recurrent tumors are present then pseudo L is rare; however pseudolymphomas do not necessary follow a benign course [18]
Surgical Treatment strategies
Resection rate varies from series to series [18, 37, 68, 69]. There are no guidelines as to when surgery is indicated. While reviewing the literature one gets the impression that surgery is advocated on an institutional basis.
Surgery for solitary lesions and adjuvant therapies for more extensive disease has been the general consensus. Overall 60-70% of the patients with PLL are surgical candidates [68]; however, incomplete resection is reported to be the case in more than 50% of the cases [69]. Surgical candidate could potentially be any patient with locally resectable tumor up to stage II 2EW. Lymph node involvement does not appear to be a contraindication to surgery. Likewise bilateral disease could also be tackled surgically. However the surgical ablation of such lesions must be economical [37] because of frequent recurrence, sometimes bilateral. Hu et al [71] concluded that patients who had received surgery tended to have a better 5 year overall survival.
The MALTomas are slow growing tumors with an indolent course; tent to be localized and therefore amenable to surgery (73% complete resection was achieved [69]).
Combined modality therapy appears to be superior in patients with bulky disease, residual disease following operation and an unfavorable non-MALT type of histology.
Recurrence rates
Pulmonary recurrences are either within the ipsilateral lung or in both lungs. Extrapulmonary recurrent disease occurs mainly in lymph nodes, however skin, bone marrow or visceral organs could be affected [63, 65].
The overall local recurrence rate is 50% [69]. More specifically the incidence of recurrence for the LP group is 33% with an average time of 69 months versus 50% for the CB group [65].
The median time to disease recurrence or death has been reported to be 6-7 years [70, 68]. Late recurrences up to 14 years have also been reported [23].
There are not enough data in the literature regarding Surgery for recurrences; nevertheless the general consensus dictates that recurrences should be treated with aggressive chemotherapy regimes.
Survival data
This is a heterogenous group of patients. Nevertheless the overall reported median time to death was 7 years or the overall reported mean survival was 71.3 months. More specifically for low grade lymphomas the median survival was 117 months and for disseminated lymphoma 33 months according to Kennedy et al [66].
The overall survival at 3 years was 86% and at 5 years 57% [68, 65]. For the MALTomas the five year survival was 68% and the ten year 53% [69].
The prognostic factors influencing survival are: the histologic type, T cell lymphoma [67] the presence of pleural effusion [63] as well as bilateral disease and the need for adjuvant therapy [70]. In contrary according to Ferraro et al [69] complete Vs incomplete resection, the stage of the disease, the presence of mediastinal lumph node involvement or bilateral disease did not significantly influence survival.
Discussion
Extensive literature review of the medical literature the last 40 years was carried out. We have excluded cases of primary pulmonary AIDS related lymphoma and lymphoma following immuno-suppression and transplantation (200 fold higher than the general population).
The incidence of PLL has two peaks: the first on in the fifth decade of life and the second late six and seventh decade. The diagnostic criteria for PLL include bilateral pulmonary lesions as PPL. The reason for that is the fact that several of those patients when treated never showed evidence of extapulmonary involvement. Also the definition includes absence of extrapulmonary disease for 3 months following the initial diagnosis. This is because invariably extrathoracic and extranodular lymphoma may present (ie. Pulmonary and stomach Lymphoma)
High index of suspicious facilitates the diagnosis of this rare, indolent disease. One third of patients have no symptoms, furthermore out of the symptomatic cohort the duration of symptoms prior to the diagnosis is at least 5 months. Serum protein electrophoresis abnormalities are present in 33% of the patients [65].
The frequency of imagine features of PLL is difficult to assess in the literature because of varying radiological terminology & heterogeneity of several series including all lymphomas of the lung. The radiography is non informative (solitary nodule, multiple ill defined nodules, consolidated mass with air bronchograms, ground glass opacity or reticular lesions in one or both lung fields, pleura effusions, atelectasis and cavities) and non specific. Multiple lesions can be present in up to 25% of the patients [65], air space consolidation with air bronchograms is the most frequent imaging in up to 65%-70% of the cases and pleural effusions in 25% of the cases [31].
The histological classification having kept the principles of low grade (87% of the patients, as per Cordier et al[68]) and high grade disease, has evolved into more complex classifications taking into account the cell morphology and histological characteristics. Although, that does not necessarily correlate with prognosis the gross differentiation into MALTs and non MALTs somehow reflects prognosis[71].
The Staging systems considers bilateral pulmonary lesion as stage I disease and stage II as disease confined to the thoracic cavity;
Only surgical biopsy and resection obtains high yield (64% of the patients as per Cordier et al[68] & 90% of the patients as per Ferraro et al[69].
The prognostic factors affecting survival are not well defined; the stage of the disease, extend of resection (complete Vs incomplete) and the presence of mediastinal lymphadenopathy does is not associated with worse prognosis [69]. In contrary, the report by Hu et al [71] suggested that hilar or mediastinal node involvement negatively influences survival. Higher stage disease was associated with statistically not significantly worse outcome according to Graham et al [70]. The authors reported that bilateral disease was the most significant factor predicting disease recurrence and death.
The evaluations of the role of surgery as well as the indications for surgery are scarce in the literature; positive surgical margins do not alter survival therefore the role of surgery may be applicable in the majority of the cases following by chemotherapy.
The long term outcome of PLL is favorable; 56% of the patients recovered from the disease [70] with an overall 5 year survival across the border of >60% and a recurrence rate of less than 50%.
During the analysis of the presented series we observed a low consistency in publishing specific variables (ie. Incidence of recurrence, etc) and this precluded us from carrying out detailed statistics; therefore our paper carries the biases not only from the studies examined but also from its observational character. Nevertheless, we believe that our report has attempted to give an insight in this rare and not well addressed pathology.
References
Rosenberg SA, Diamond HD, Jaslowitz B, Craver LF: Lymphosarcoma: A review of 1269 cases. Medicine. 1961, 40: 31-84. 10.1097/00005792-196102000-00002.
Freeman C, Berg JW, Cutler SJ: Occurrence and prognosis of extranodal lymphomas. Cancer. 1972, 29: 252-260. 10.1002/1097-0142(197201)29:1<252::AID-CNCR2820290138>3.0.CO;2-#.
Saltzstein SL: Pulmonary malignant lymphomas and pseudolymphomas: Classification, therapy and prognosis. Cancer. 1963, 16: 928-955. 10.1002/1097-0142(196307)16:7<928::AID-CNCR2820160709>3.0.CO;2-H.
Greenhaligh : How to read a paper: the MEDLINE database. Br Med J. 1997, 315: 180-183.
Gao J, Huang X, Wang R, Cai B, Lu W, Lin Y: Primary pulmonary lymphoma: analysis of cases and review of the literature. Zhonghua Jie He He Hu Xi Za Zhi. 2002, 25 (8): 484-7.
Zhang LB, Sun YE, Yu CH, Liu Y: Clinical diagnosis and surgical treatment of primary pulmonary lymphoma. Zhonghua Wai Ke Za Zhi. 2006, 44 (2): 97-9.
Tian XL, Feng RE, Shi JH, Duan MH, Wang JL, Liu HR, Cai BQ, Gao JM, Xu WB, Zhu YJ: Primary pulmonary lymphoma: analysis of 18 cases.
Varona JF, Guerra JM, Grande C, Villena V, Gonzalez-Lois C, Martinez MA: Primary pulmonary lymphoma: diagnosis and follow up of 6 cases and review of an uncommon entity.
Peterson H, Snider HL, Yam LT, Bowlds CF, Arnn EH, Li CY: Primary pulmonary lymphoma. A clinical and immunohistochemical study of six cases. Cancer. 1985, 56 (4): 805-13. 10.1002/1097-0142(19850815)56:4<805::AID-CNCR2820560418>3.0.CO;2-Q.
Muller C, Grivaux M, Schwattz F, Blanchon F: Primary pulmonary lymphoma. Current data. Apropos of 9 cases. Rev Pneumol Clin. 1990, 46 (4): 166-71.
Mu XD, Wang GF, Diao XL, Que CL: A case of marginal zone B-cell lymphoma of the pulmonary mucosa- associated lymphoid tissue type. Beijing Da Xue Xue Bao. 2007, 39 (4): 346-50.
Natali F, Merlet P, Le Vagueresse R, Allard P, Jourdain de Muizon H, Kermarec J: Primary pulmonary lymphoma. Rev Pneumol Clin. 1984, 40 (6): 355-62.
Deng LP, Hu HJ, Zhang SZ, Dong DJ, Tan HQ: Radiological features of primary pulmonary non-Hodgkin lymphoma:report of three cases. Zhonghua Jie He He Hu Xi Za Zhi. 2003, 26 (4): 223-6.
Nakachi S, Nagasaki A, Owan I, Uchihara T, Fujita J, Ohshima K, Miyagi T, Taira T, Taira N, Takasu N: Primary pulmonary Hodgkin lymphoma-two case reports and a review of the literature. Gan To Kagaku Ryoho. 2007, 34 (13): 2279-82.
Martinez Rivera C, Bonnin Vilaplana M, Simon Adiego C, Palacin Forgue A, Puig Zuza J, Sampablo Lauro I: Primary pulmonary lymphoma presenting as a pulmonary mass with cavitation. Arch Bronconeumol. 2004, 40 (2): 94-6.
Colby TV, Carrington CB: Pulmonary lymphomas simulating lymphomatoid granulomatosis. Am J Surg Pathol. 1982, 6 (1): 19-32. 10.1097/00000478-198201000-00002.
Toh HC, Ang PT: Primary pulmonary lymphoma-clinical review from a single institution in Singapore. Leuk Lymphoma. 1997, 27 (1-2): 153-63.
Marchevsky A, Padilla M, Kaneko M, Kleinerman J: Localazed lymphoid nodules of the lung. A reappraisal of the lymphoma versus pseudolymphoma dilemma. Cancer. 1983, 51 (11): 2070-7. 10.1002/1097-0142(19830601)51:11<2070::AID-CNCR2820511120>3.0.CO;2-R.
Morisako T, kobayashi H, Kanou S, Uwabe Y, Nagata N, Aoki T, Ozeki Y, Aida S, Tamai S: Clinicopathological study of six cases of primary pulmonary lymphoma diagnosed by gene rearrangement analysis. Nihon Kokyuki Gakkai Zasshi. 1998, 36 (3): 236-40.
Kim JH, Lee SH, Park J, Kim HY, Lee SI, Park JO, Kim K, Kim WS, Jung CW, Park YS, Im YH, Kang WK, Lee MH, Park K, Han JH, Ko YH: Primary pulmonary non- Hodgkin lymphoma. Jpn J Clin Oncol. 2004, 34 (9): 510-4. 10.1093/jjco/hyh095.
Addis BJ, Hyjek E, Isaacson PG: Primary pulmonary lymphoma: a re-appraisal of its histogenesis and its relationship to pseudolymphoma and lymphoid interstitial pneumonia. Histopathology. 1988, 13 (10): 1-17. 10.1111/j.1365-2559.1988.tb02000.x.
Arinc S, Yilmaz A: Primary pulmonary lymphoma. Tuberk Toraks. 2006, 54 (2): 197-202.
Xu HY, Jin T, Li RY, Ni YM, Zhou JY, Wen XH: Diagnosis and treatment of pulmonary mucosa-associated lymphoid tissue lymphoma. Chin Med J. 2007, 120 (8): 648-51.
Pagani M, Antico A, Bellarosa S, Cavazzini G, Aitini E: Primary pulmonary high grade non-Hodgkin lymphoma in an elderly patient. A case report. Tumori. 2007, 93 (6): 622-4.
Cao MS, Cai HR, Yin HL, Zhang DP, Xiao YL, Cao M, Dai LJ, Hou J: Primary natural killer/T cell lymphoma of the lung: two cases report and clinical analysis. Zhonghua Jie He He Hu Xi Za Zhi. 2008, 31 (2): 120-4.
Baas AA, van Herwaarden CL: Primary non- Hodgkin lymphoma of the lung. Eur J Respir Dis. 1986, 68 (3): 218-23.
Ziade N, Khayat G, Sader-Ghorra C, Abadjian G: Primary pulmonary lymphoma. A case report and review of the literature. J Med Liban. 2005, 53 (1): 50-4.
Habermann TM, Ryu JH, Inwards DJ, Kurtin PJ: Primary pulmonary lymphoma. Semin Oncol. 1999, 26 (3): 307-15.
Uematsu M, Okada M, Ishii N, Watanabe N, Yasufuku M: Surgical treatment of primary pulmonary malignant lymphoma: a report of successful case. Kyobu Geka. 1997, 50 (4): 325-30.
Tillawi IS: Primary pulmonary Hodgkins lymphoma. A report of 2 cases and review of the literature. Saudi Med J. 2007, 28 (6): 943-8.
Chu HQ, Ren SX, Yi XH: The clinical diagnosis and analysis of pulmonary mucosa associated lymphoid tissue lymphoma. Zhonghua Jie He He hu Xi Za Zhi. 2007, 30 (3): 167-9.
Le Tourneau A, Audouin J, Garbe L, Capron F, Servais B, Monges G, Payan H, Diebold J: Primary pulmonary malignant lymphoma, clinical and pathological findings, immunocytochemical and ultrastructural studies in 15 cases. Hematol Oncol. 1983, 1 (1): 49-60. 10.1002/hon.2900010107.
Loh KC, Chan KW, Sng I: Primary pulmonary lymphoma:report of three cases and a brief review of the literature. Ann Acad Med Singapore. 1994, 23 (3): 400-5.
Cordier JF, Bernaudin JF, Mary P, Guillaud C, Loire R, Brune J, Touraine R: Primary pulmonary pseudolymphomas and lymphomas.4 cases. Rev Mal Respir. 1984, 1 (2): 105-11.
Watanabe J, Yamaguchi K, Sugiyama Y, Yotsumoto H, Takaku F: Primary pulmonary lymphoma demonstration of monoclonality by lymphocyte surface marker study. Jpn J Med. 1987, 26 (3): 377-80.
Toishi M, Miyazawa M, Takahashi K, Hyogotani A, Haba Y, Kato K, Muramatsu A, Nishiyama M, Ozawa K, Nanbu A, Miyata K: Mucosa-associated lymphoid tissue lymphoma; report of two cases. Kyobu Geka. 2004, 57 (1): 75-9.
Jayet A, Wertheim U, Crausaz PH, Saegesser F: Pulmonary granuloma, pseudolymphoma and lymphoma. Helv Chir Acta. 1980, 47 (1-2): 37-40.
Kuroishi S, Nakano Y, Ono T, Shirai m, Hayakawa H, Murakami M, Suda T, Chida K, Nakamura H, Kobashi Y: A case of primary pulmonary MALT lymphoma as a nodular shadow on CT scan, and relapsed with diffuse micronodular shadows after surgical resection at 7 years ago. Nihon Kokyuki Gakkai Zasshi. 2003, 41 (12): 922-7.
Sakula A: Primary malignant lymphoma of lung. Postgrad Med J. 1979, 55 (639): 46-9. 10.1136/pgmj.55.639.46.
Hashizume T, Honda A, Eto T, Akiyama J, Yamakawa H, Ikehara K, Ito M, Fujii M, Suzuki M, Arai K: Primary pulmonary lymphoma diagnosed from monoclonality of lymphocytes in a transbronchial biopsy specimen. Nihon Kyobu Shikkan Gakkai Zasshi. 1997, 35 (1): 95-9.
Gouldesbrough DR, McGoogan E: Primary pulmonary lymphoma: a case diagnosed by bronchial cytology and immunocytochemistry. Histopathology. 1988, 13 (4): 465-7. 10.1111/j.1365-2559.1988.tb02064.x.
Bosanko CM, Korobkin M, Fantone JC, Rubin SB, Lynch JP: Lobar primary pulmonary lymphoma: CT findings. J Comput Assist Tomogr. 1991, 15 (4): 679-82. 10.1097/00004728-199107000-00028.
Chee YC, Yap CH, Poh SC: Pulmonary lymphoma or pseudolymphoma: a diagnostic dilemma. Ann Acad Med Singapore. 1986, 15 (1): 113-7.
Bolton- Maggs PH, Colman A, Dixon GR, Myskow MW, Williams JG, Donnelly RJ, Hind CR: Mucosa associated lymphoma of the lung. Thorax. 1993, 48 (6): 670-2. 10.1136/thx.48.6.670.
Xu TR: Pulmonary lymphoma of mucosa-associated lymphoid tissue. A clinical, pathological, immunochemical and ultrastructural study of 2 cases. Zhonghua Jie He He Hu Xi Za Zhi. 1987, 10 (5): 269-70.
Konig G, Huhn D, Albrecht J: Diagnosis of pulmonary manifestations of malignant lymphoma by bronchopulmonary lavage. Prax Klin Pneumol. 1986, 40 (5): 183-5.
Ehrenstein F: Primary pulmonary lymphoma. Review of the literature and two case reports. J Thorac Cardiovasc Surg. 1966, 52 (1): 31-9.
Tamura A, Komatsu H, Yanai N, Homma J, Nagase A, Nemoto E, Hirai T, Hashizume T, Kawata K, Ishikawa S: Primary Pulmonary Lymphoma: relationship between clinical features and pathological finings in 24 cases. The Japan National Chest Hospital Study Group for Lung Cancer. Jpn J Clin Oncol. 1995, 25 (4): 140-52.
Sakuraba M, Onuki T, Mae M, Yoshida T, Nitta S: Three cases of primary pulmonary malignant lymphoma. Nihon Kokyuki Gakkai Zasshi. 2000, 38 (9): 714-9.
Abe Y, Hayashi A, Yasufuku K, Oiwa T, Kurosu K, Mikata A: Nihon Kokyuki Gakkai Zasshi. 1998, 36 (4): 403-7.
Umino T, Ohdama S, Sawada M, Tachibana S, Takano S, Miyake S, Aoki N, Yamamoto N, Matsubara O, Masuda S: A case of surgically resected primary pulmonary lymphoma with IgG-paraproteinemia: gene analysis was effective for establishing its diagnosis. Nihon Kokyuki Gakkai Zasshi. 1993, 31 (8): 1012-8.
Zinzani PL, Tani M, Gabriele A, Poletti V, Stefoni V, Alinari L, Musuraca G, Bonifazi F, Pileri S, Tura S, Baccarani M: Extranodal marginal zone B-cell lymphoma of MALT type of the lung: Single center experience with 12 patients. Leuk Lymphoma. 2003, 44 (5): 821-4. 10.1080/1042819031000067972.
Herbert A, Wright DH, Isaacson PG, Smith JL: Primary malignant lymphoma of the lung:histopathologic and immunologic evaluation of nine cases. Hum Pathol. 1984, 15 (5): 415-22. 10.1016/S0046-8177(84)80074-X.
Davis WB, Gadek JE: Detection of pulmonary lymphoma by bronchoalveolar lavage. Chest. 1987, 91 (5): 787-90. 10.1378/chest.91.5.787.
Pisani RJ, Witzig TE, Li CY, Morris MA, Thibodeau SN: Confirmation of lumphomatous pulmonary involvement by immunophenotypic and gene rearrangement analysis of bronchoalveolar lavage fluid. Mayo Clin Proc. 1990, 65 (5): 651-6.
Sprague RI, deBlois GG: Small lymphocytic pulmonary lymphoma. Diagnosis by transthoracic fine needle aspiration. Chest. 1989, 96 (4): 929-30. 10.1378/chest.96.4.929.
Julsrud PR, Brown LR, Li CY, Rosenow EC, Crowe JK: Pulmonary processes of mature-appearing lymphocytes: pseudolymphoma, well-differentiated lymphocytic lymphoma and lymphocytic interstitial pneumonitis. Radiology. 1978, 127 (2): 289-96.
Lewis ER, Caskey CI, Fishman EK: Lymphoma of the lung:CT findings in 31 patients. AJR Am J Roentgenol. 1991, 156 (4): 711-4.
Bellotti M, Elsner B, Esteva H, Mackinlay TA, Mazzei JA: Fiberoptic bronchoscopy in the diagnosis of pulmonary lymphomas. Respiration. 1987, 52 (3): 201-4. 10.1159/000195325.
Kilgore TL, Chasen MH: Endobronchial non-Hodgkins lymphoma. Chest. 1983, 84 (1): 58-61. 10.1378/chest.84.1.58.
Rose RM, Grigas D, Strattemeir E, Harris NL, Linggood RM: Endobronchial involvement with non-Hodgkins lymphoma. A clinical -radiological analysis. Cancer. 1986, 57 (9): 1750-5. 10.1002/1097-0142(19860501)57:9<1750::AID-CNCR2820570907>3.0.CO;2-J.
Oka M, Kawano K, Kanda T, Hara K: Bronchoalveolar lavage in primary pulmonary lymphoma with monoclonal gammopathy. Am Rev Respir Dis. 1988, 137 (4): 957-9.
Koss MN, Hochholzer L, Nichols PW, Wehunt WD, Lazarus AA: Primary non-Hodgkins lymphoma and pseuolymphoma of lung: a study of 161 patients. Hum Pathol. 1983, 14 (12): 1024-38. 10.1016/S0046-8177(83)80258-5.
Turner RR, Colby TV, Doggett RS: Well-differentiated lymphocytic lymphoma. A study of 47 patients with primary manifestation in the lung. Cancer. 1984, 54 (10): 2088-96. 10.1002/1097-0142(19841115)54:10<2088::AID-CNCR2820541008>3.0.CO;2-Y.
L Hoste R, Filippa D, Lieberman P, Bretsky S: Primary Pulmonary Lymphomas. A clinicopathologic analysis of 36 cases. Cancer. 1984, 54: 1397-1406. 10.1002/1097-0142(19841001)54:7<1397::AID-CNCR2820540728>3.0.CO;2-4.
Kennedy JL, Nathwani BN, Burke JS, Hill LR, Rappaport H: Pulmonary lymphomas and other pulmonary lymphoid lesions. A clinicopathologic and immunologic study of 64 patients. Cancer. 1985, 56 (3): 539-52. 10.1002/1097-0142(19850801)56:3<539::AID-CNCR2820560322>3.0.CO;2-D.
Li G, Hansmann ML, Zwingers T, Lennert K: Primary lymphomas of the lung: morphological, immunohistochemical and clinical features. Histopathology. 1990, 16 (6): 519-31. 10.1111/j.1365-2559.1990.tb01157.x.
Cordier JF, Chailleux E, Lauque D, Reynauld-Gaubert M, Dietemann-Molard A, Dalphin JC, Blanc-Jouvan F, Loire R: Primary pulmonary lymphomas. A clinical study of 70 cases in nonimmunocompromised patients. Chest. 1993, 103: 201-208. 10.1378/chest.103.1.201.
Ferraro P, Trastek V, Adlakha H, Deschamps C, Allen M, Pairolero P: Primary non Hodgkins lymphoma of the lung. Ann Thorac Surg. 2000, 69: 993-997. 10.1016/S0003-4975(99)01535-0.
Graham BB, Mathisen DJ, Mark EJ, Takvorian RW: Primary pulmonary lymphoma. Ann Thorac Surg. 2005, 80 (4): 1248-53. 10.1016/j.athoracsur.2005.04.014.
Hu YH, Hsiao LT, Yang CF, Chiou TJ, Liu JH, Gau JP, Yen CC, Chou TY, Hsu WH, Chen PM, Tzeng CH: Prognostic factors of Chinese patients with primary pulmonary non-Hodgkins lymphoma: the single-institude experience in Taiwan. Ann Hematol. 2009,
Bienenstock J, Johnston N, Perey D: Bronchial lymphoid tissue. Lab Invest. 1973, 28: 686-98.
Harris NL, Jaffe ES, Stein H: A revised European- American classification of lymphoid neoplasms: a proposal from the InternationalLymphoma Study Group. Blood. 1994, 84: 1361-92.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Parissis, H. Forty years literature review of primary lung lymphoma. J Cardiothorac Surg 6, 23 (2011). https://doi.org/10.1186/1749-8090-6-23
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1749-8090-6-23