Abstract
Management of high energy intra-articular fractures of the proximal tibia, associated with marked soft-tissue trauma, can be challenging, requiring the combination of accurate reduction and minimal invasive techniques. The purpose of this study was to evaluate whether minimal intervention and hybrid external fixation of such fractures using the Orthofix system provide an acceptable treatment outcome with less complications. Between 2002 and 2006, 33 patients with a median ISS of 14.3 were admitted to our hospital, a level I trauma centre, with a bicondylar tibial plateau fracture. Five of them sustained an open fracture. All patients were treated with a hybrid external fixator. In 19 of them, minimal open reduction and stabilization, by means of cannulated screws, was performed. Mean follow-up was 27 months (range 24 to 36 months). Radiographic evidence of union was observed at 3.4 months (range 3 to 7 months). Time for union was different in patients with closed and grade I open fractures compared to patients with grade II and III open fractures. One non-union (septic) was observed (3.0%), requiring revision surgery. Pin track infection was observed in 3 patients (9.1%).
Compared to previously reported series of conventional open reduction and internal fixation, hybrid external fixation with or without open reduction and minimal internal fixation with the Orthofix system, was associated with satisfactory clinical and radiographic results and limited complications.
Similar content being viewed by others
Introduction
Intra-articular fractures of the proximal end of the tibia, the so-called 'plateau fractures', are serious, complex injuries difficult to treat [1]. The mechanism of injury is based on the presence of an initial axial load, which fractures the tibial articular surface resulting in impaction. In most of the cases the initial load is combined with angular forces, leading to comminution not only of the articular surface, but of the metaphysis as well. The medial compartment is split in a medio-lateral direction with a postero-medial main fragment, combined with various amounts of multifragmental lateral compartment depression [2].
According to Schatzker's classification [3, 4], these fractures are divided into six groups: S-I to S-VI. Of these types, those involving both condyles (S-V) and those separating tibial metaphysis from diaphysis (S-VI) are the most challenging fractures for the Orthopaedic Surgeon to treat not only for the osseous damage but for the restoration of the soft tissue envelope as well.
Standard radiographic imaging includes anteroposterior and lateral views. Suspicion of distal extension of the fracture mandates that full-length tibia and fibula x-rays should be obtained. The CT scan is becoming more and more useful in the evaluation of the size, comminution and orientation of the articular fragments, allowing proper classification and preoperative planning, thus facilitating reduction, especially for the less invasive techniques of treatment [5].
Over the years, many treatment modalities have been proposed for these complex fractures. All of them, from simple traction to demanding surgery, presented fair results but also serious complications.
Traction, in terms of ligamentotaxis and casting, do not properly reduce the articular surface and lack the necessary stability, leading to unacceptable rate of varus/valgus deformity, collapsed articular surface and post-immobilization stiffness [6–9]. On the other hand, open surgical procedures, despite their good reduction results, do not protect the already damaged "soft-tissue envelope", leading to skin or muscle necrosis and to high rates of infection [10, 11].
The use of a "minimal invasive technique", an external fixator, in the treatment of S-V and S-VI fractures may provide fair reduction results without endangering the soft-tissue elements. Moreover, it facilitates the access to any endangered soft tissue elements requiring interventions along the treatment period. The addition of minimal internal fixation with cannulated screws and k-wires prior to an external fixator application provides minimum soft tissue striping and greater fixation stability, allowing for early mobilization and greater range of motion [12–17].
The purpose of the current study was to test the hypothesis whether minimal intervention and hybrid external fixation using the Orthofix system can provide a fair outcome with less complications and to compare our results and complications with previously reported data of internal and external fixation for types V and VI high energy tibial plateau fractures.
Materials and methods
After receiving approval from our Institutional Review Board, we retrospectively examined a consecutive series of 33 patients (33 bicondylar tibial plateau fractures (Schatzker type V, VI) admitted at our level I trauma centre between 2002 and 2006. Fractures were identified through our trauma database and were cross-matched with operating room records. Median ISS was 14.3, ranging from 9 to 33. Inclusion criteria were the presence of a bicondylar tibial plateau fracture Schatzker type V-VI, patients' age over 18 years and the ability to walk without assistance before injury. Polytrauma patients with tibial plateau fractures requiring prolonged ICU care (AIS>3 for head and chest) and patients with bilateral plateau fractures, were excluded from the study. All patients were followed according to a protocol. All fractures were treated with either closed reduction and hybrid external fixation (14 fxs/36.6%) or with minimal open reduction and a hybrid system (19 fxs/63.4%). The study group was consisted of 20 males (60.6%) and 13 females (39.4%) with an average age for males of 40.3 years (range 30 - 62 years) and for females 49 years (range 17 - 86 years). In 27 patients (81.8%) the mechanism of injury was high energy trauma (motor vehicle accident or fall from height greater than 3 m). All patients had anteroposterior and lateral radiographs as well as a CT-scan for proper preoperative evaluation of their fracture.
The preoperative radiographs were used to classify the fractures according to Schatzker's classification system. There were 16 S-V (48.5%), and 17 S-VI (51.5%) fractures. Twenty eight (28) were closed (84.8%) and five (5) were open fractures (15.2%). Of those, one (1) fracture was type I, two (2) type II and two (2) were type IIIA open fractures according to Gustilo-Anderson classification. Peroneal nerve injury occurred in one (1) patient (3.0%), at the time of the injury. Two patients (6.0%) had major knee instability with rupture of ACL and LCL.
Nineteen (19) patients (57.5%) were submitted to minimal open reduction by means of cannulated screws prior to the application of an external fixator. In seventeen (17) of these patients (51.5%), cortical allografts were used. All patients were available for follow up (average 27 months, range 24 - 36 months) with repeated anteroposterior and lateral radiographs at 1.5, 3, 6, 12, 18, 24 and 36months.
Soft tissue condition had a crucial importance on our planning for the time of the operation. All patients with open fractures (5) (15.2%) were operated immediately with irrigation, debridement, intravenous antibiotics. 18 (54.5%) closed fractures were treated in the first day after the accident while 7 fractures (21.2%) were treated with an average of 5 days delay (range 3 - 9 days) in order to allow soft tissue edema to subside. For the latter group a posterior long leg splint was placed to the affected limb.
Prophylactic antibiotics were administered intravenously in all cases. In the open fracture cases, antibiotics were prescribed as necessary for the first days and subsequently replaced according to the cultures results. All open fractures received initially a combination of a 2nd generation cephalosporin with an aminoglycoside. Both open and closed fractures received preoperatively a single dose of teicoplanin.
Surgical technique
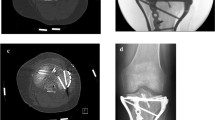
We used the Orhtofix hybrid external fixation system. Surgery was performed under general or spinal anesthesia with the patient positioned on the operating table with the knee flexed at 30°. A tourniquet is not a significant advantage in closed reduction, but if used, should be deflated as soon as possible. The fracture reduction was visualized with an image intensifier. Through a small incision over the antero-medial aspect of the tibial metaphysis, a small "window" was made in the tibial cortex. A blunt tipped curved 3 mm k-wire or a simple pusher was inserted through the hole, up to the articular fragments, which were elevated under image intensifier control. In most of the cases, more than one k-wire was required to reduce the articular fracture. Bone grafts were applied to feel osseous gaps. Through a small lateral incision, a Kirschner wire was inserted across the tibial plateau to stabilize the reduced fragments and a cannulated screw was introduced over it. After closed or minimal open reduction of fracture fragments, an Orthofix hybrid external fixator was applied. A ring of appropriate size was positioned at the level of the fibular head. All wires were applied in the transverse plane, 2 from lateral to medial and the remaining 2 from antero-lateral to postero-medial. Each wire was tensioned to 1,400 N and locked to the frame. The metaphyseal fracture was reduced accurately and the body of the external fixator was applied on the ring on the antero-medial aspect of the tibia. Two pin guides were inserted down to the skin which was then incised. Pin holes were pre-drilled with a 4.8 mm drill bit and three 5/6 mm tapered self-tapping cortical pins were inserted. The fixator was clamped to the screws. It was of crucial importance that the fracture was reduced before the permanent fixation of the hybrid system. After achieving adequate reduction, the system was locked and secured. The reduction was then confirmed by C-arm. If alignment was not satisfactory, a minimal exposure of the fracture site was performed to enable the desirable reduction (Figure 1, 2).
For mini open exposures, wound was closed primarily for close fractures. For open fractures, we preferred either to leave the wound open for surgical debridement or to proceed to a delayed primary closure 72 h postoperatively. Skin graft coverage was needed only for one patient (S-V(G-IIIA).
Post-operative care consisted of daily performed thorough pin care, from the first postoperative day, with hydrogen peroxide and betadine as well as immediate passive range of motion of the knee. For highly comminuted fractures, a posterior splint was applied and after 48 hours the patient was encouraged to start controlled knee movement as soon as possible. Patients were discharged from the hospital between the 5th and 15th postoperative day, depending on their general condition. Patients with Gustilo grade II and III open fractures were checked weekly in the outpatient department. All the other patients were checked monthly. They were instructed not to bear weight on the operated limb and to regularly perform pin site care. Progressive weight bearing was allowed between the 8th and 12th week depending on the radiographic appearance of callus. The weight bearing started with 10 kg and, based on the clinical and radiographic signs of union, advanced to 30 kg after one month. In most of our cases, the external fixator was removed at 3.4 months after surgery depending on the radiological appearance of union.
Results
Patient results are given in Table 1. All fractures in this series except one (3.0%) healed. Union was determined by the presence of a bridging callus on the follow-up radiographs and by the clinical impression of stability. Follow-up evaluation was available for all fractures. Based on the parameters considered at the follow-up (radiological results, knee ROM, pain, ability to perform sport activities, and patient's satisfaction), according to KSS criteria [18], the results were evaluated as excellent in 18 patients (55%), good in 10 patients (30%), fair in 4 patient (12%), and poor in 1 (3%) (Table 1).
There were no systemic complications attributable to our surgical treatments. All associated ligamentous and meniscal lesions were repaired at a second stage after fracture healing. All fractures healed, with an average time of treatment with the frame of 3.4 months (Figure 3, 4). The external fixator was tolerated for the entire treatment period in all cases. Two fractures (6.0%) took longer than 6 months to heal.
In our series only one (1) fracture was complicated with deep infection leading to septic non-union (3.0%). It was treated with surgical debridement and i.v. antibiotics until CRP and ESR reached normal values. Later on, open reduction and internal fixation with plate and autologus bone grafting was performed. Deep venous thrombosis was detected in one patient (3.0%) and was treated successfully with low molecular weight heparin.
There were 3 pin track infections (9.1%). These infections were superficial or limited to the soft tissue and did not extend to the bone. None of the patients required hospital admission. There were treated with oral antibiotic and local pin care. All pin track infections healed without requiring wire or half-pin removal that could compromise frame's stability. Two fractures (6.0%) resulted in malunion (10° of valgus, < 5° procurvatum), but faced no symptoms. In one case of an open fracture, local skin necrosis occurred requiring a skin graft.
A total of 26 (78.8%) patients regained functional use of the knee joint, good axis, without pain or instability. Patients' knee ROM was gradually increasing at consecutive clinical evaluations. Patients were discharged from the hybrid fixator after an average time of 3.4 months (range 3 - 7 months). At the one year follow-up, range of motion averaged 115° of flexion (range 75° to 125°) and 5° lack of extension (range 0°- 8°). During the radiographic follow-up evaluation, early osteoarthritic changes at the knee joint were noticed in one (1) patient (3.0%) (SVI/GII fracture).
Overall, 5 patients (15.1%) faced with at least 1 minor complication such as pin track infection, stiffness, malunion and 1 patient (3.0%) came up with at least one (1) major complication including septic-nonunion and osteomyelitis. No amputation was performed.
Discussion
The importance of the soft-tissue envelope in the healing of plateau fractures has been analyzed in the literature and a correlation of poor results with severely damaged soft-tissues has already been established [19]. High energy trauma is considered as a major cause of poor results in the treatment of tibial plateau fractures. Different methods for treating these complex injuries have been proposed, including limited open reduction and stabilization with percutaneous screws, open reduction and internal fixation [4, 20–23] and indirect reduction and application of a hybrid [24–26] or a circular external fixation device [27, 28].
Internal fixation, despite the advantages of direct visualization, proper and stable reduction of the articular surface as well as the acute repair of soft tissue injuries, presents also serious disadvantages, including skin or soft-tissue necrosis caused by surgical manipulations on an already damaged soft-tissue envelope and the high rate of infection, which may compromise the final result. Tscherne et al, comparing the results of surgical versus conservative treatment for tibial plateau fractures, reported improved range of motion, decreased percentage of malunion and 5% reoperation rate for the surgical group [29]. Stevens et al, presented several transoperative - postoperative complications [30], while Young and Barrack, in their series of dual plating for complex bicondylar tibial plateau fractures reported an 88% deep infection rate [31, 32]. Certain authors have treated bicondylar tibial fractures by means of a lateral fixed angular plate (FAP) through a single lateral approach, thus avoiding medial periosteal striping [33, 34]. Jiang R et al, in their prospective study comparing locked plates, to classic double plates (DP), for the repair of bicondylar tibial plateau fractures reported similar results for the two groups [35]. Nevertheless, as presented by Higgins et al., bicondylar fractures stabilized by means of a FAP present a higher rate of subsidence compared to dual plating stabilized fractures [36].
The external fixation as a definite treatment for the polytrauma patient with multiple osseous and soft tissue injuries has been described in the literature [37, 38]. Certain authors believe that external fixation should be limited to bicondylar tibial fractures with a compromised soft-tissue envelope, as a temporary stabilizing technique, prior to definite treatment [39]. In the last 2 decades, the evolution of devices and techniques of external fixation has led many surgeons to apply the principles of biologic osteosynthesis and minimally invasive surgery for the treatment of comminuted tibial plateau fractures [4, 28, 32, 39]. The development of circular and hybrid frames, the capability of axial, lateral compression and dynamization, the development of olive wires have offered new possibilities to the external fixators for the treatment of complex fractures [40]. Mahadena et al, comparing external to internal fixation, concluded that hybrid external fixation possesses theoretical advantages in terms of the soft tissues protection; however the benefit over internal fixation is modest as far as accuracy of reduction is concerned [41]. Chin et al presented 38.9% good/excellent, and 61.1% fair/poor results in his type V and VI fracture series [42]. Catagni et al, in their series of high-energy Schatzker V and VI tibial plateau fractures treated with circular external fixator, reported excellent and good results in 30 (50.85%) and 27 (45.76%) patients respectively [23]. In a similar study on type V and VI tibial plateau fractures, Katsenis et al recorded excellent or good final clinical results in 36 patients (76%) [24]. In 2009, the Canadian Orthopaedic Trauma Association, in a multicenter, prospective, randomized clinical trial of 83 S-V, VI tibial plateau fractures treated with internal or external fixation, reported similar quality of osseous reduction and ROM for both groups but lower rate of early postoperative complications and improved HSS scores for the external fixation group at the six months' follow up. However, at the two years' follow up, no significant difference in ROM, HSS scores, WOMAC and SF-36 was observed between the two groups [43].
In our series, we used the Orthofix hybrid external fixator as a definite treatment for Schatzker V, VI closed fractures as well as for some open tibial plateau fractures. When necessary, open reduction and minimal internal fixation by means of k-wires or screws were performed prior to external fixation application. Overall, we had an incidence of infection of 12.1%. This rate compares favorably with historical controls as seen in table 1. The rate drops to 3.0% (1 pt) if we look only at deep infections. All the other cases (3 pts), were superficial pin tract infections that resolved with proper care and oral antibiotics. Malunion (valgus-procurvatum) was observed in two patients. It is important to note that the case of deep infection as well as the two cases of malunion occurred in the group of Schatzker VI-open fractures. In many older articles, authors do not break down their complications according to the type of the tibial plateau fracture [4, 22, 44]. Our cohort by contrast is essentially a homogeneous group composed of Schatzker V and VI fractures secondary to a high-energy mechanism. A similar homogenous group was presented by Covall et al. The authors treated 32 bicondylar tibial plateau fractures during a 7-year period and reported a 42% deep infection rate in the cases treated acutely with internal fixation [15].
As far as minor complications are concerned, Hutson et al, in a meta-analysis of 16 studies with a total of 568 patients found pin site infection rates of 10% for tibial plateau fractures [45]. This number is similar to the rate of pin tract infection (9.1%) observed in our series. Moreover, the two cases of malunion (6.1%) represent an acceptable rate as compared with other series [23]. Complications concerning the external fixation device such as intolerance or pin loosening were not observed in our study.
Limitations
As limitations of this study, one should consider its retrospective nature. Additionally, since our study group is composed of high energy plateau fractures with a high complication rate, the average follow up of 27 months can be considered as inadequate to draw safe conclusions for the development of post-traumatic osteoarthritis. This report may be the basis for a new study examining the development of post- traumatic arthritis in patients with high energy plateau fractures.
Conclusions
Schatzker's type V and VI tibial plateau fractures represent serious injuries with substantial residual limb-specific and general health deficits [43]. We believe that the use of Orthofix external fixation, as a definite treatment, for high-energy proximal tibia bicondylar fractures proved to be beneficial. While confronting such limb-threatening injuries, external fixation successfully provided continuous access on the surrounding tissues as well as proper osseous stabilization without compromising the sensitive soft tissue envelope.
References
Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN: Complications after tibia plateau fracture surgery. Injury. 2006, 37: 475-84. 10.1016/j.injury.2005.06.035.
Eggli S, Hartel MJ, MD S, Haupt U, Exadaktylos AK, Roder C: Unstable Bicondylar Tibial Plateau Fractures: A Clinical Investigation. J Orthop Trauma. 2008, 22: 673-679. 10.1097/BOT.0b013e31818b1452.
Schatzker J: Fractures of the tibial plateau. Edited by: Schatzker J, Tile M. 1988, The Rationale of Operative Orthopaedic Care, Springer-Verlag, New York, 279-295.
Schatzker J, McBroom R, Bruce D: The tibial plateau fracture: The Toronto experience (1968-1975). Clin Orthop Relat Res. 1979, 138: 94-104.
Hackl W, Riedl J, Reichkendler M, Benedetto KP, Freund M, Bale R: Preoperative computerized tomography diagnosis of fractures of the tibial plateau. Unfallchirurg. 2001, 104: 519-523. 10.1007/s001130170115.
Appley AG: Fractures of the tibial plateau. Orthop Clin North Am. 1979, 10: 61-74.
Delamarter R, Hohl M: The cast brace and tibial plateau fractures. Clin Orthop Relat Res. 1989, 242: 26-31.
Scotland T, Wardlaw D: The use of cast-bracing as treatment for fractures of the tibial plateau. J Bone Joint Surg Br. 1981, 63: 575-578.
Oestern HJ, Tscherne H: Pathophysiology and Classification of Soft Tissue Injuries Associated with Fractures. Fractures with Soft Tissue Injuries, Springer-Verlag. Edited by: Tscherne H, Gotzen L. 1984, Berlin, 1-9.
Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke SK: Complications Associated With Internal Fixation of High-Energy Bicondylar Tibial Plateau Fractures Utilizing a Two-Incision Technique. J Orthop Trauma. 2004, 18: 649-657. 10.1097/00005131-200411000-00001.
Mallik AR, Coval DJ, Whitelaw GP: Internal versus external fixation of bicondylar tibial plateau fractures. Orthop Rev. 1992, 21: 1433-1436.
Murphy CP, D'Ambrosia R, Dabezies EJ: The small pin circular fixator for proximal tibial fractures with soft tissue compromise. Orthopedics. 1991, 14: 273-280.
Swiontkowski MF, Bucholz RW: Knee and Leg Trauma: Bone Trauma. Orthopaedic Knowledge Update 4, American Academy of Orthopaedic Surgeons. Edited by: Frymoyer JW. 1993, Rosemont, 579-592.
Coval DJ, Fowble CD, Foster TE, Whitelaw GP: Bicondylar tibial plateau fractures: Principles of treatment. Contemp Orthop. 1994, 28: 115-122.
Duwelius PJ, Conolly JF: Closed reduction of tibial plateau fractures. A comparison of functional and roentgenographic end results. Clin Orthop Rel Res. 1988, 230: 116-26.
Duwelius PJ, Rangitsch MR, Colville MR, Woll TS: Treatment of tibial plateau fractures by limited internal fixation. Clin Orthop Relat Res. 1997, 339: 47-57.
Giannoudis PV: Surgical priorities in damage control in polytrauma. J Bone Joint Surg Br. 2003, 85: 478-483. 10.1302/0301-620X.85B4.14217.
Insall JN, Dorr LD, Scott RD, Scott WN: Rationale of the knee Society clinical rating system. Clin Orthop Relat Res. 1989, 248: 13-4.
Delamarter RB, Hohl M, Hopp E: Ligament injuries associated with tibial plateau fractures. Clin Orthop Relat Res. 1990, 250: 226-233.
Blokker CP, Rorabeck CH, Bourne RB: Tibial plateau fractures. An analysis of the results of treatment in 60 patients. Clin Orthop Relat Res. 1984, 182: 193-199.
Reichard AK, Seligson D, Alt V: External fixation of tibial plateau fractures: a retrospective evaluation and case report. Osteo Trauma Care. 2004, 12: 33-36.
Waddell JP, Johnston DW, Neidre A: Fractures of the tibial plateau: a review of ninety-five patients and comparison of treatment methods. J Trauma. 1981, 21: 376-381. 10.1097/00005373-198105000-00007.
Catagni MA, Ottaviani G, Maggioni M: Treatment strategies for complex fractures of the tibial plateau with external circular fixation and limited internal fixation. J Trauma. 2007, 63: 1043-1053. 10.1097/TA.0b013e3181238d88.
Katsenis D, Athanasiou V, Megas P, Tillianakis M, Lambiris E: Minimal internal fixation augmented by small wire transfixion frames for high-energy tibial plateau fractures. J Orthop Trauma. 2005, 19: 241-248. 10.1097/01.bot.0000155309.27757.4c.
Weiner LS, Kelley M, Yang E, Steuer J, Watnick N, Evans M, Bergman M: The use of combination internal fixation and hybrid external fixation in severe proximal tibial fractures. J Orthop Trauma. 1995, 9: 244-250. 10.1097/00005131-199506000-00011.
Weigel DP, Marsh JL: High-energy fractures of the tibial plateau. Knee function after longer follow-up. J Bone Joint Surg Am. 2002, 84: 1541-1551.
Watson JT, Coufal C: Treatment of complex lateral plateau fractures using Ilizarov techniques. Clin Orthop Relat Res. 1998, 353: 97-106.
Dendrinos GK, Kontos S, Katsenis D, Dalas A: Treatment of high energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br. 1996, 78: 710-717.
Tscherne H, Obenhofferm P: Tibia1 plateau fractures. Management and expected results. Clin Orthop Relat Res. 1993, 292: 87-100.
Stevens DG, Beharry R, McKee MD, Waddell PJ, Schemitsch EH: The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma. 2001, 15: 312-320. 10.1097/00005131-200106000-00002.
Young MJ, Barrack RL: Complications of internal fixation of tibial plateau fractures. Orthop Rev. 1994, 23: 149-54.
Keogh P, Kelly C, Cashman WF, McGuinness AJ, O'Rourke SK: Percutaneous screw fixation of tibial plateau fractures. Injury. 1992, 23: 387-389. 10.1016/0020-1383(92)90013-I.
Partenheimer A, Gösling T, Müller M, Schirmer C, Kääb M, Matschke S, Ryf C, Renner N, Wiebking U, Krettek C: Management of bicondylar fractures of the tibial plateau with unilateral fixed-angle plate fixation. Unfallchirurg. 2007, 110: 675-83. 10.1007/s00113-007-1271-1.
Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C: Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res. 2005, 439: 207-14. 10.1097/00003086-200510000-00036.
Jiang R, Luo CF, Wang MC, Yang TY, Zeng BF: A comparative study of Less Invasive Stabilization System (LISS) fixation and two-incision double plating for the treatment of bicondylar tibial plateau fractures. Knee. 2008, 15: 139-143. 10.1016/j.knee.2007.12.001.
Higgins TF, Klatt J, Bachus KN: Biomechanical Analysis of Bicondylar Tibial Plateau Fixation: How Does Lateral Locking Plate Fixation Compare to Dual Plate Fixation?. J Orthop Trauma. 2007, 21: 301-306. 10.1097/BOT.0b013e3180500359.
Scalea TM, Boswell SA, Scott JD: External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: damage control orthopaedics. J Trauma. 2000, 48: 613-621. 10.1097/00005373-200004000-00006.
Sirkin M, Sanders R, Di Pasquale T, Herscovici D: A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 1999, 13: 78-84. 10.1097/00005131-199902000-00002.
Lemon RA, Bartlett DH: Arthroscopic assisted internal fixation of certain fractures about the knee. J Trauma. 1985, 25: 355-358. 10.1097/00005373-198504000-00015.
Schwartsman V, Martin SN, Ronquist RA, Schwartsman R: Tibial fractures. Clin Orthop Relat Res. 1992, 278: 207-216.
Mahadeva D, Costa ML, Gafrey A: Open reduction and internal fixation versus hybrid fixation for bicondylar/severe tibial plateau fractures: a systematic review of the literature. Arch Orthop Trauma Surg. 2008, 128: 1169-75. 10.1007/s00402-007-0520-7.
Chin TYP, Bardana D, Bailey M, Williamson OD, Miller R, Edwards ER, Esser MP: Functional outcome of tibial plateau fractures treated with the fine-wire fixator. Injury. 2005, 36: 1467-1475. 10.1016/j.injury.2005.05.008.
Hall JA, Beuerlein MJ, McKee MD, Canadian Orthopaedic Trauma Society: Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Surgical technique. J Bone Joint Surg Am. 2009, 91: 74-88.
Anglen JO, Healey WV: Tibial plateau fractures. Orthopedics. 1988, 11: 1527-1534.
Hutson JJ, Zych GA: Infections in periarticular fractures of the lower extremity treated with tensioned wire hybrid fixators. J Orthop Trauma. 1998, 12: 214-8. 10.1097/00005131-199803000-00014.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
All authors contributed equally to this work. BGC, DSE, PK, KN and PNS participated in the design of the study and drafted the manuscript. BGC and DSE participated in the design of the study. BGC and KN conceived of the study, participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Babis, G.C., Evangelopoulos, D.S., Kontovazenitis, P. et al. High energy tibial plateau fractures treated with hybrid external fixation. J Orthop Surg Res 6, 35 (2011). https://doi.org/10.1186/1749-799X-6-35
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1749-799X-6-35