Abstract
Background
The aim was to quantify severe transient and persisting late term effects in our single institution head neck cancer (HNC) cohort treated with curatively intended intensity modulated radiation therapy (IMRT). Hypothesis was if a 2-year follow up (FU) is sufficient to estimate the long term tolerance in HNC irradiated in the IMRT era.
Methods
Between 01/2002-8/2012, 707/1211 (58%) consecutively treated IMRT patients met the inclusion criteria of a FU time >12 months and loco-regional disease control (LRC). 45% presented with loco-regionally advanced disease; 55% were referred for curative definitive IMRT (66 Gy-72 Gy in 30–35 fractions), 45% underwent postoperative IMRT (60-66 Gy in 30–33 fractions). Systemic concomitant therapy was administered in 85%. Highly consistent treatment procedures were performed with respect to contouring processes, dose constraints, radiation schedules, and the use of systemic therapy. Grade 3/4 late term effects were prospectively assessed and analyzed with respect to subgroups at particular risk for specific late effects.
Results
Mean/median FU of the cohort was 41/35 months (15–124). 13% of the patients (92/707) experienced any grade 3/4 late effects (101 events in 92/707 patients), 81% in the first 12 months after radiation. 4% of all developed persisting late grade 3/4 effects (25 events in 25/707 patients).
Conclusions
IMRT led to a high late term tolerance in loco-regionally disease free HNC patients. The onset of any G3/4 effects showed a plateau at 2 years. The question of the cervical vessel tolerance in disease free long time survivors is still open and currently under evaluation at our institution.
Similar content being viewed by others
Background
Intensity modulated radiation (IMRT) techniques are expected to improve the therapeutic index for head neck cancer (HNC) by limiting the dose to critical organs and possibly increasing loco-regional tumor control. The benefit of normal tissue sparing achievable with IMRT with resulting lower rates of late term effects in HNC survivors is broadly recognized. Data on successful parotid gland sparing, reduction of radio-osteonecrosis (RON) and dysphagia are published [1–7]. The probability of specific late effects depends on the exposed tissue and on the dose, and sometimes on the chemotherapy.
Aim of this prospectively assessed single center data analysis was to evaluate transient and persisting IMRT late term effects related to subgroups at risk. Hypothesis was if a 2-year follow up (FU) is sufficient to estimate the long term tolerance in HNC patients irradiated in the IMRT era.
Methods
Patients
Between 01/2002-8/2012, 1211 HNC patients were consecutively treated with IMRT (or volumetric modulated arc therapy, VMAT) at our department. 707/1211 patients (58%) met the inclusion criteria of a FU time >12 months and loco-regional disease control (LRC), Table 1. 45% presented with advanced disease (T3/4 and/or N2c/N3), 55% were referred for curative definitive IMRT (66 Gy-72 Gy, 30–35 daily fractions), 45% underwent postoperative radiation (60-66 Gy, 30–33 daily fractions). Systemic therapy was administered in 85%. Seven LRC patients were lost after 4.3-10.4 months of FU (median 5.5); 12/707 (2%) LRC patients were lost after 12.2-51.6 months (median 39).
In 26 of the 504 excluded patients with locoregional disease (1211–707), G3/4 late effects were assessed (5%), however this information is of limited value as tumor-related symptoms are not always reliably to disdinguish from treatment-related effects, survival time in patients with disease is shorter, FU of patients undergoing palliative systemic therapy often no longer regularly performed by ENT and maxillofacial surgery joint clinics.
Although acute toxicity was not focus of this work, the following characteristics of the study population may be of some interest: early skin tolerance was obviously better than in the pre-IMRT era (no quantitative comparison data) and has been published elsewhere [8]. The percentage of patients needing a PEG insertion to support or replace oral nutrition (46% in the study population) may serve as a surrogate for acceptable dysphagia and mucositis. In addition, no patient had to interrupt his radiation course due to early radiation related side effects.
Methods
Highly consistent treatment procedures were performed with respect to contouring processes, dose constraints, radiation schedules, use of systemic therapy. Contours and treatment plans were always evaluated by the same two staff radiation oncologists (CG/GS).
Implemented changes as evolved from medical and technical progress over the study time period of 10 years were the following: use of cetuximab in patients with contraindications for cisplatinum (since 04/2006); slight tumor-volume based dose prescription adaptations implemented in 2007 (100% dose coverage of primary GTV in cases with tumor volume >15 cc); clinical implementation of VMAT in 4/2010.
Since 2010, the dose to the brachial plexus has been kept below Dmax 66 Gy, according to the suggestion in most RTOG protocols (http://www.rtog.org/CoreLab/ContouringAtlases/BrachialPlexusContouringAtlas.aspx).
Late normal tissue effects were graded according to the Radiation Therapy Oncology Group (RTOG)/European Organization for Research and Treatment of Cancer (EORTC) radiation morbidity scoring criteria [2].
There are several systems aiming to grade RON. We used the system proposed by Glanzmann and Graetz [9]:
-
1.
Exposed bone without signs of infection for at least 3 months
-
2.
Exposed bone with signs of infection or sequester, but not grades 3–5
-
3.
RON, treated with mandibular resection, with satisfactory result
-
4.
RON with persistent problems despite mandibular resection
-
5.
Death due to RON
The advantage of this classification vs. that of EORTC (LENT/SOMA) or NCI [10] is its connection to therapeutic clinical consequences; nevertheless, grade 2 events mutually correspond in all of the above named classification systems. Most frequent therapy for G2 was limited surgery (partial decortication or debridement, removal of sequesters); these surgical procedures are not defined in our grading system, and were counted as 'G2-3’.
All but the above mentioned 19 lost patients are in regular FU; nearly all (99%) are followed at our HN or maxillofacial surgery joint center clinics at the hospital. Routine tests included, besides the history, physical examination and endoscopy of the pharyngeal–laryngeal region. If these tests showed no evidence of disease, usually no further tests were done but a computed tomography scan (CT) or positron emission tomography (PET)–CT or magnetic resonance imaging at 1 year post-treatment in the majority of patients.
No specific functional swallowing testing was performed to assess subtle (G1-2) dysphagia; reasons to do so were: no baseline examinations available; many patients would have shown mild pathological swallowing findings of no significant impact on the final post treatment function; as we focused on high grade late term effects (G3/4) relevant dysphagia with consecutive swallowing problems (aspiration, aspiration pneumonia, difficulty swallowing solid food, weight loss, need of PEG) is supposed to reliably get communicated by patients themselves and/or diagnosed in the regular FU program in our joint center clinics.
Similarly, no specific tests were performed to assess xerostomia G3/4 but patients’ spontaneous complaints and/or suggestive interview questions in regular FU visits including objective clinical assessment of severe oral mucosal dryness. When we implemented IMRT in the routine, swallowing dysfunction and xerostomia were graded in the first 100 IMRT patients using subjective patient-reported (EORTC head-and-neck 35-item swallowing and aspiration (QLQ-H&N35) quality-of-life (QOL) questionnaire) and objective observer-assessed instruments. As subjective estimations were well fitting with objective assessments in routinely clinical FU interviews [4], we did not continue to use the EORTC subjective estimation questionnaires for assessing clinical FU.
With respect to Lhermittes’ sign, no systematic specific assessments have been performed, which may likely would have revealed more events; however as this symptome is known for transient and spontaneous entire healing without any therapy, this is not of clinical consequence.
No case of brachial plexus neuropathy (BPN) with clinically evident dysfunction (grade >2) was diagnosed in our cohort (patients with post-IMRT neck dissection excluded); mild neuropathy (G1/2) may be missed without specific neurological examination.
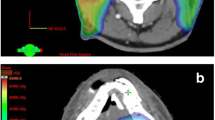
Radiation therapy
In >90% of the cohort the pre-treatment standard imaging modality was PET–CT (mostly with intravenous contrast agent), + tomography (CT or MRI). Planning CT images (2 mm slice thickness) were acquired from the vertex or top of the orbita to the carina with contrast agent infusion in all eligible patients.
Gross tumor volume (GTV) delineation of all patients was based on physical examination and endoscopy as well as on diagnostic preoperative MRI, CT and PET. Contours and treatment plans were always evaluated by the same two staff radiation oncologists (CG/GS), in most cases also by a third staff physician.
Technique: Treatment plans were calculated by the Varian Treatment Planning System (Eclipse® External Beam Planning System, Version 7.3.10 and PRO 8.9, AAA 8.9, Varian Medical Systems).
We used an extended-field SIB-IMRT technique, where the primary tumor is covered in one phase along with the regional lymph nodes by a 6MV dynamic MLC system (Varian Medical Systems, Palo Alto, CA) using a sliding window technique (or using VMAT, since 04/2010). Patients were immobilized from head to shoulders with commercially available thermoplastic masks in the supine position.
Target volumes were delineated as follows: GTV included the gross extent of the primary disease and involved lymph node metastases, taking clinical and radiological findings into account; planning target volume 1 (PTV1) was defined by adding a (5–) 10–20 mm margin to the GTV, dependent on the GTV proximity to critical structures (tight margins mainly if proximity of the GTV to the mandible bone, spinal cord or brachial plexus/CNS, generous margins towards tongue and pharyngeal wall, or in cases with difficult identification of the GTV, or if clinical findings not entirely represented in the available imaging); PTV2 covered areas considered at high risk for potential microscopic disease; PTV3 included the clinically negative cervical lymphatic pathways (elective PTV coverage).
SIB IMRT was performed using the following schedules:
-
SIB2.00: Daily dose 2.00 Gy (PTV1)/1.70 Gy (PTV2)/1.54 Gy (PTV3) to a total dose of 70.00 Gy (5 fractions/week).
-
SIB2.11: Daily dose 2.11 Gy (PTV1)/1.80 Gy (PTV2)/1.64 Gy (PTV3) to a total dose of 69.60 Gy (5 fractions/week).
-
SIB2.2: Daily dose 2.2 Gy (PTV1)/2.0 Gy (PTV2)/1.64 Gy (PTV3) to a total dose of 66.0 Gy (5 fractions/week).
The dose was normalized to the mean dose in PTV1. The prescribed dose encompassed at least 95% of the PTV. In cases with central nervous system involvement, Dmax accepted was 2.00 Gy, to a Dmax of 70.0 Gy total dose (PTV1 = GTV; no margin).
No more than 20% of any PTV received >110% of its prescribed dose, whilst no more than 1% of any PTV received <93% of the prescribed dose. Hundred% of the prescription dose included the primary GTV in patients with a primary tumor volume >15 cc (since ~ 2007).
Our interdisciplinary in-house guidelines recommend an elective neck dissection in patients with initial nodal metastasis >3 cm.
Chemotherapy
Cisplatin was given in weekly doses of 40 mg/m2 at 1 day a week. Since 04/2006, cetuximab was used in patients with contra-indications for concomitant standard cisplatin chemotherapy (400 mg/m2 loading dose, followed by 250 mg/m2 at 1 day a week).
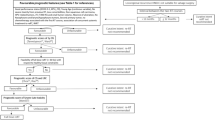
Follow up
3–6 weeks after completion of IMRT, all patients were also regularly seen in our joint clinic at the Department of Head and Neck or Maxillofacial Surgery. Institutional standards for patient assessment included physical examination with additional flexible fiber-optic endoscopy approximately every 2 months in the first year of follow-up, every 3 months in the second to third year and every 6 months in the fourth to fifth year.
Statistics
Kaplan Meier survival curves were performed using the statistics program implemented in StatView® (Version 4.5). P values < 0.05 were considered statistically significant. Unpaired T test and Mann Whitney U test was used to calculate the influence of the tumor volume on late tolerance.
Results
Disease control
823 of 1211 (68%) curatively irradiated HNC patients were alive with no evidence of disease when last seen; 14% died from disease, 7% died for other than HNC reasons, 11% were alive with disease. Kaplan Meier survival rates of the 5-year overall survival (OAS, 74%), LRC (68%), and distant metastasis free survival probability (DMFS, 82%) of the entire IMRT cohort are shown in Figure 1.
707/1211 patients (58%) met the study inclusion criteria of a FU time >12 months and loco-regional disease control (LRC), Table 1. The mean/median FU time of this LRC study cohort was 41/35 months (range 15–124). Five-year DMFS (91%) and OAS (88%) Kaplan Meier curves of these patients are illustrated in Figure 2.
Late term tolerance
The following late term G3-4 effects were diagnosed (Table 2), Additional file 1: Table S1.
-
RON (grade 2–4, [9])
-
Mucosal ulcer (other than uncovered bone)
-
prolonged (>6 months) need of percutaneous endoscopic gastrostomy (PEG)
-
persisting xerostomia/dryness of the pharynx
-
need of post-treatment tracheostomy without tumor
-
need of post-treatment laryngectomy without tumor
-
taste loss >6 months
-
Lhermittes’ sign
The onset of all late term effects (Figure 3) revealed a plateau at 2 years; 81% of all G3/4 events were diagnosed/symptomatic in the first 12 months post radiation. Table 2 (see also Additional file 1: Table S1) shows diagnosed grade 3/4 effects: 92/707 patients (13%) experienced any late term effects, most of them with transient character or complete recovery following specific therapy.
In 4% (25/707), persisting grade 3/4 effects were stated, including:
-
two patients with arterial bleeding, one with lethal exit (GTV mean/max 71.8/75.8 Gy, PTV1 mean/max 69.7/76.2 Gy; 2.2 cc/6.5 cc of the GTV/PTV exposed to 74-75 Gy)
-
5 patient with partial mandibulectomy/persisting problems after RON therapy (Table 3); (doses to the RON area of the mandible were <70.0 Gy in 3 patients, 72 Gy point dose in one, 70–72.3 Gy to 1.5 cc in one)
-
5/28 patients with PEG dependence >6 months remained PEG dependent (severe dysphagia +/- aspirations in 4, in one due to insufficient ability to keep his body weight by oral nutrition despite of normal swallowing ability); initially in 46% of all study patients a PEG was inserted to support or replace oral nutrition
-
3 NPC patients with persisting G3 xerostomia (<26 Gy to 62%/36%, 72%/44%, and 48%/52% to right/left parotid glands)
-
2 disease free patients with tracheostomy inserted post IMRT due to edema,
-
1 patient with persisting secretion from a fistula after removal of tracheostoma,
-
2 LRC patients with post IMRT laryngectomy due to necrosis/edema
-
3 patients with insufficient taste recovery,
-
one LRC patient with persisting mucosal ulcer after post IMRT biopsy
-
one patient with slowly healing oral mucositis (fibrinous mucosal layers >6 months present after 60 Gy postoperative IMRT + concomitant cisplatin)
-
5 nasal/sinonasal tumor patients with persisting repetitive nasal crusts and/or surgical nasal synechiolysis +/- lacrimal duct stenosis stenting
All but 2/25 individuals with persisting late effects presented with advanced HNC; most with personal history of relevant co-morbidities in addition to nicotine and alcohol abuse.
Tumor volume didn’t show to be a statistically significant predictor for G3/4 late effects in the LRC study group: total GTV (tGTV) in study patients with any G3/4 effects compared with patients with no relevant late effects was mean/median (range) 41/33 (1-132 cc) vs 36/27 (1–217), p = 0.13). The tGTV was expectedly highly significantly larger in non-study patients (with local or nodal failure) as compared with the LRC study cohort: mean/median (range) 55/43 (1-319 cc) vs 39/28 (1-267 cc), p <0.0001.
Discussion
Limitations of this study
-
a)
Methodical limitation given by the inclusion criterion of loco-regional disease control: as late term sequelae cannot properly be assessed in patients with persistent or recurrent tumor, locoregional control was a key condition for this evaluation, however, thereby excluding cases with larger tumors and advanced stages, which may be prone to more treatment related late toxicity.
-
b)
The authors are aware of the fact of a still relatively short FU, baring the potential of further upcoming late sequels (e.g. vascular changes)
-
c)
during the study time period of 10 years, several changes due to progresses in medicine and technology have been clinically implemented, like the use of cetuximab 2006, slight own data driven tumor-volume based dose prescription adaptations implemented in 2007, or clinical implementation of VMAT in 2010. These innovations may have influenced treatment tolerance. In addition, since 2010, the dose to the brachial plexus has been kept below Dmax 66 Gy according to the suggestion in most RTOG protocols. Of potential benefit with respect to late tolerance may be our risk adapted pre-IMRT dental care (DC) program (activated 2006), which allows to spare more theeth than after conventional DC [11], and includes tight supervision and care by our dentists also in the periods during and post radiation
-
d)
Finally, the fact of missing self-scoring xerostomia evaluation but from the very first IMRT patients [4] is a lack of information. Self-scoring has been recommended to be assess xerostomia [12]. Main reason not to focus any longer on this topic in the own patients were the detailed early investigations on xerostomia and salivary flow rates after IMRT by Eisbruchs’ group [13]. Their data fitted very well with the own clinical observations.
The presented evaluation revealed a low rate of 4% G3/4 persisting late term effects, reflecting the nowadays expectable level of treatment tolerance. The late effect rate as diagnosed 2 years post treatment completion was found representative and was unchanged at 5 years (Figure 3). Findings (Tables 2 and 3) compare well with published data from other centers on treatment tolerance in the IMRT/VMAT era. The comparability of IMRT late effects with that in published IMRT series is however somewhat limited due to different tumor cohorts assessed, different approaches to analyze and/or grade tolerance parameters (e.g. PEG dependence and/or pharyngeal dryness sometimes included in dysphagia rates, RON events not always graded, side effects related or not to subgroups at risk).
Treatment tolerance is clearly better nowadays compared with conventional pre-IMRT era prospective randomized trials. Reasons for this improvement are multifactorial; the main reason is the use of IMRT techniques allowing better sparing of organs at risk while delivering highly conformal tumor dose. The RTOG 9003 prospective randomized landmark trial compared normo-fractionation versus different other fractionation schedules in >1000 patients after conventional radiation techniques, and found grade >/=3 effects in 26.8-37.2% after a median FU of 23 months [14]. Similarly, the prospective randomized SAKK 10/94 trial investigated the effect of conventional technique hyperfractionated radiotherapy +/- concomitant cisplatin; the corresponding late effect rate was 111 events in 224 treated patients [15].
One of the important advantages of IMRT in oral cavity and oropharyngeal cancer is the reduced RON risk (1% G3/4 RON in our 'patients at risk’ cohort with oral cavity, lateral or central oropharynx cancer (oral cavity patients at highest risk (3%)), Table 2). The low RON rate in HNC patients is characteristic for the IMRT era and comparable with other published series [1, 5, 6]. None of our NPC patients treated with IMRT (n = 67 since 2002) was RON affected. RON rates reported in the SAKK 10/94 trial were 6% [15], in the RTOG 9003 trial 2.3% after a FU of median 23 months [14]. Comparison of the RON incidence after conventional radiation techniques during the period between 1980–1990 with 1990–1998 showed a decrease in the risk to a value of ~5% using three-dimensional (non-IMRT) techniques and hyper- or moderately accelerated fractionation [16].
PEG dependence and/or relevant dysphagia are often multifactorial (mucosal dryness, muscular dysfunction, tumor related anatomical defects) and were observed in hypopharynx, oral cavity or central oropharynx tumor patients; central oropharynx tumor patients were most often affected (3%). PEG dependence in oropharynx cancer patients was also described in a series from Memorial Sloan Kettering Cancer Centre (6/50) [17]. In the pre-MRT era, this rate was substantially higher (>20% permanent xerostomia and dysphagia in both study arms in the SAKK 10/94 trial [15], 10-15% dysphagia and 6-10% xerostomia in the RTOG 9003 [14], respectively). The low rate of persisting xerostomia grade 3 (3/51 NPC patients (6%), oropharyngeal and oral cavity cancer (<1%)) is in concordance with meanwhile numerous reports on parotid sparing in the IMRT literature [3, 7, 13]. The probability of severe xerostomia following radiation remains dependent on the dose and the anatomic distance of GTV to parotid glands and/or submandibular glands and the mucosal area included in PTVs. Considering the missing self-scoring of our patients, the assessed rate of G3/4 xerostomia may be somewhat higher.
Mucosal ulceration occurred in 28/593 (5%) patients with pharyngeal or oral cavity cancer (i.e. in patients with substantial areas of pharyngeal and/or oral mucosa included in the high dose planning target volumes, but in NPC patients), its location was always at the site of the former primary where also the boost dose was delivered. Most mucosal ulcers were painful, and clinically and radiologically hardly to differ from tumor persistence; its treatment was usually analgetic and/or antibiotic therapy. Early exclusion of local recurrence by biopsy is recommended. The onset of mucosal ulcer was diagnosed 0–18 months post IMRT completion (mean/median 5/3 months), comparable to published results [18]; complete healing took 1–12 months (mean 3.5).
In order to quantify the subgroup of risk for BPN, dose distribution plans of the first 100 consecutive patients out of 226 definitively irradiated patients with nodal disease have been reviewed: in 19/100 (~20%), the plexus was in part exposed to >65 Gy. No G3/4 brachial arm plexopathy was diagnosed in extrapolated ~40 patients at risk - in concordance with limited retrospective data from small HNC cohorts published on this topic [19].
Brain necrosis was not diagnosed in our NPC/sinonasal cohort as based on clinical and radiological FU assessments (22 cT4 NPC, 8 cT4 sinonasal cancer patients at risk). In all cases the dose was kept below 70 Gy delivered in 2.0 Gy/session to <1 cc brain.
Lhermittes’ sign in HNC is rarely reported, and was diagnosed in 4 patients. There was no obvious correlation with doses delivered (spinal cord <2.0 Gy/session in all patients, with a maximum dose of 46 Gy). Pak et al. prospectively reported on 73 affected patients and found an incidence rate of 21% which was related to higher spinal doses than in asymptomatic patients [20].
With regard to the question of cervico-vascular changes, no robust dose-volume related data are available so far but descriptions of vascular changes following conventional radiation from several small series [21].
Conclusion
IMRT led to a high late term tolerance in the subgroup of loco-regionally disease free HNC patients, with only 4% persisting G3/4 effects. The onset of any G3/4 effects showed a plateau at 2 years.
The question of the cervical vessel tolerance in disease free long time survivors is still open and currently under evaluation at our institution.
References
Ben-David MA, Diamante M, Radawski JD, Vineberg KA, Stroup C, Murdoch-Kinch CA, Zwetchkenbaum SR, Eisbruch A: Lack of osteoradionecrosis of the mandible after intensity-modulated radiotherapy for head and neck cancer: likely contributions of both dental care and improved dose distributions. Int J Radiat Oncol Biol Phys 2007, 68: 396-402. 10.1016/j.ijrobp.2006.11.059
Eisbruch A, Levendag PC, Feng FY, Teguh D, Lyden T, Schmitz PI, Haxer M, Noever I, Chepeha DB, Heijmen BJ: Can IMRT or brachytherapy reduce dysphagia associated with chemoradiotherapy of head and neck cancer? The Michigan and Rotterdam experiences. Int J Radiat Oncol Biol Phys 2007, 69: S40-42.
Nutting CM, Morden JP, Harrington KJ, Urbano TG, Bhide SA, Clark C, Miles EA, Miah AB, Newbold K, Tanay M, Adab F, Jefferies SJ, Scrase C, Yap BK, A'Hern RP, Sydenham MA, Emson M, Hall E: Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol 2011, 12: 127-136. 10.1016/S1470-2045(10)70290-4
Peponi E, Glanzmann C, Willi B, Huber G, Studer G: Dysphagia in head and neck cancer patients following intensity modulated radiotherapy (IMRT). Radiat Oncol 2011, 6: 1. 10.1186/1748-717X-6-1
Studer G, Graetz KW, Glanzmann C: In response to Dr. Merav a. Ben-David et al. ("Lack of osteoradionecrosis of the mandible after IMRT," Int J radiat oncol biol phys 2007). Int J Radiat Oncol Biol Phys 2007, 68: 1583-1584.
Studer G, Studer SP, Zwahlen RA, Huguenin P, Grätz KW, Lütolf UM, Glanzmann C: Osteoradionecrosis of the mandible: minimized risk profile following intensity-modulated radiation therapy (IMRT). Strahlenther Onkol 2006, 182: 283-288. 10.1007/s00066-006-1477-0
Wang X, Hu C, Eisbruch A: Organ-sparing radiation therapy for head and neck cancer. Nat Rev Clin Oncol 2011, 8: 639-648. 10.1038/nrclinonc.2011.106
Studer G, Brown M, Salgueiro EB, Schmückle H, Romancuk N, Winkler G, Lee SJ, Sträuli A, Kissling B, Dummer R, Glanzmann C: Grade 3/4 dermatitis in head and neck cancer patients treated with concurrent cetuximab and IMRT. Int J Radiat Oncol Biol Phys 2011, 81: 110-117. 10.1016/j.ijrobp.2010.05.018
Glanzmann C, Gratz KW: Radionecrosis of the mandibula: a retrospective analysis of the incidence and risk factors. Radiother Oncol 1995, 36: 94-100. 10.1016/0167-8140(95)01583-3
Jereczek-Fossa BA, Orecchia R: Radiotherapy-induced mandibular bone complications. Cancer Treat Rev 2002, 28: 65-74. 10.1053/ctrv.2002.0254
Studer G, Glanzmann C, Studer SP, Grätz KW, Bredell M, Locher M, Lütolf UM, Zwahlen RA: Risk-adapted dental care prior to intensity-modulated radiotherapy (IMRT). Schweiz Monatsschr Zahnmed 2011, 121: 216-229.
Meirovitz A, Murdoch-Kinch CA, Schipper M, Pan C, Eisbruch A: Grading xerostomia by physicians or by patients after intensity-modulated radiotherapy of head-and-neck cancer. Int J Radiat Oncol Biol Phys 2006, 66: 445-53. 10.1016/j.ijrobp.2006.05.002
Eisbruch A, Dawson LA, Kim HM, Bradford CR, Terrell JE, Chepeha DB, Teknos TN, Anzai Y, Marsh LH, Martel MK, Ten Haken RK, Wolf GT, Ship JA: Conformal and intensity modulated irradiation of head and neck cancer: the potential for improved target irradiation, salivary gland function, and quality of life. Acta Otorhinolaryngol Belg 1999, 53: 271-275.
Fu KK, Pajak TF, Trotti A, Jones CU, Spencer SA, Phillips TL, Garden AS, Ridge JA, Cooper JS, Ang KK: A radiation therapy oncology group (RTOG) phase III randomized study to compare hyperfractionation and two variants of accelerated fractionation to standard fractionation radiotherapy for head and neck squamous cell carcinomas: first report of RTOG 9003. Int J Radiat Oncol Biol Phys 2000, 48: 7-16. 10.1016/S0360-3016(00)00663-5
Huguenin P, Beer KT, Allal A, Rufibach K, Friedli C, Davis JB, Pestalozzi B, Schmid S, Thöni A, Ozsahin M, Bernier J, Töpfer M, Kann R, Meier UR, Thum P, Bieri S, Notter M, Lombriser N, Glanzmann C: Concomitant cisplatin significantly improves locoregional control in advanced head and neck cancers treated with hyperfractionated radiotherapy. J Clin Oncol 2004, 22: 4665-4673. 10.1200/JCO.2004.12.193
Studer G, Gratz KW, Glanzmann C: Osteoradionecrosis of the mandibula in patients treated with different fractionations. Strahlenther Onkol 2004, 180: 233-240. 10.1007/s00066-004-1171-z
de Arruda FF, Puri DR, Zhung J, Narayana A, Wolden S, Hunt M, Stambuk H, Pfister D, Kraus D, Shaha A, Shah J, Lee NY: Intensity-modulated radiation therapy for the treatment of oropharyngeal carcinoma: the memorial Sloan-Kettering cancer center experience. Int J Radiat Oncol Biol Phys 2006, 64: 363-373. 10.1016/j.ijrobp.2005.03.006
Debnam JM, Garden AS, Ginsberg LE: Benign ulceration as a manifestation of soft tissue radiation necrosis: imaging findings. AJNR Am J Neuroradiol 2008, 29: 558-562. 10.3174/ajnr.A0886
Platteaux N, Dirix P, Hermans R, Nuyts S: Brachial plexopathy after chemoradiotherapy for head and neck squamous cell carcinoma. Strahlenther Onkol 2010, 186: 517-520. 10.1007/s00066-010-2099-0
Pak D, Vineberg K, Feng F, Ten Haken RK, Eisbruch A: Lhermitte sign after chemo-IMRT of head-and-neck cancer: incidence, doses, and potential mechanisms. Int J Radiat Oncol Biol Phys 2012, 83: 1528-1533. 10.1016/j.ijrobp.2011.10.052
Fokkema M, den Hartog AG, van Lammeren GW, Bots ML, Pasterkamp G, Vink A, Moll FL, de Borst GJ: Radiation-induced carotid stenotic lesions have a more stable phenotype than de novo atherosclerotic plaques. Eur J Vasc Endovasc Surg 2012, 43: 643-648. 10.1016/j.ejvs.2012.02.023
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GS drafted the article and created the underlying data base; GS, Cl, OR, YN, MB and CG performed the contouring and were in charge for the isodose plan reviewing, and treated the assessed patient cohort; CG and GS double-checked all contouring and isodose plans and are responsible for the IMRT-SIB radiation treatment schedules as defined/applied; BY assessed the dose distribution to the arm plexus region of the cohort; TR was involved in systemic therapy decisions for at risk patients and performed the chemotherapy in NPC patients; GH, MB, SS(4), RZ operated on these patients and performed the regular FU; SS(2) was in charge with dental long term rehabilitation of our patients. All authors read and approved the final manuscript.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Studer, G., Linsenmeier, C., Riesterer, O. et al. Late term tolerance in head neck cancer patients irradiated in the IMRT era. Radiat Oncol 8, 259 (2013). https://doi.org/10.1186/1748-717X-8-259
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1748-717X-8-259