Abstract
Background
To evaluate the role of γ-H2AX in peripheral blood lymphocytes (PBLs) as a predictive biomarker of the severity of oral mucositis (OM) in head and neck cancer (HNC) patients with receiving radiotherapy.
Methods
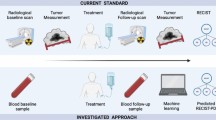
In vitro assays for evaluating DNA damage and repair kinetics were performed on blood samples withdrawn from 25 HNC patients undergoing radiotherapy or chemoradiotherapy before radiotherapy. As for the in vivo study, blood samples were also withdrawn before radiotherapy, and 1 hour after radiotherapy on the fourth and last days. Flow cytometry was used to assess the expression of γ-H2AX in PBLs. OM was assessed using the World Health Organization (WHO) scores twice a week and correlated with the expression of γ-H2AX.
Results
The in vitro assay results showed that patients with severe OM had higher γ-H2AX-specific relative fluorescence at various irradiation doses in the damage kinetics assay, with significantly higher γ-H2AX expression at 8 Gy (p = 0.039), and also at 24 hours after irradiation at a dose of 2 Gy in the repair kinetics assay, compared to the patients with mild OM (p = 0.008). The optimal cutoff value for relative fluorescence of γ-H2AX was 0.960, 24 hours post-irradiation. However, there were no significant differences in γ-H2AX expression at different times between the two groups, as assessed with the in vivo assay.
Conclusions
These results suggest that the damage and repair kinetics of γ-H2AX from PBLs in the in vitro study may have predictive value for identifying the grades of OM among HNC patients prior to radiotherapy.
Similar content being viewed by others
Background
Radiotherapy is one of the main therapies used for treatment of head and neck cancer (HNC). However, even with highly-refined treatment planning, such as intensity-modulated radiation therapy, radiation-induced toxicities in tumor-adjacent normal tissues remain the major limiting factor for the treatment [1]. Oral mucositis (OM) is one of the most common and severe acute normal tissue toxicities for HNC patients treated with radiotherapy [2]. OM is associated with considerable pain, dysphagia, and dysgeusia, resulting in the impairment of the quality of life. Furthermore, OM is a dose-limiting toxicity and can lead to treatment interruption, consequentially compromising the likelihood of cure [3]. There are many factors, including radiation fractionation, dose per fraction, and irradiated volume, that are associated with OM; even if nearly identical irradiation schemes are administered in the clinic, there are inter-individual heterogeneities in OM among HNC patients [4]. Therefore, an assay that enables the prediction of the grades of OM before commencing radiotherapy is highly desirable. Such predictive assays may help differentiate radiosensitive individuals from others and allow the treating physicians to modify the treatment strategies for individual patients to prevent the occurrence of severe side effects [5, 6].
The extent of radiation-induced DNA damage and its repair have been considered to be the most relevant indicators of irradiation-associated toxicity to normal tissue [7]. A key factor in the repair process of damaged DNA is the histone protein H2AX, which is rapidly phosphorylated at sites of DNA double strand breaks (DSBs) and can be visualized using immunofluorescence within a few minutes of exposure of cells to DNA-damaging agents [8]. Therefore, H2AX levels have been used to quantitate the ability of cells to damage and repair DNA after irradiation [9]. The correlation of γ-H2AX with DNA damage in peripheral blood lymphocytes (PBLs), blood mononuclear cells, skin, or other human tissues has been observed [10]. However, studies of the association between the expression of γ-H2AX and the risk of normal tissue toxicities have not yielded conclusive results [11, 12]. A study by Rube et al. [13] indicated that γ-H2AX of lymphocytes from children with solid tumors could be used to identify DSB-repair deficiencies in patients who developed severe toxicities to normal tissue after chemo/radiotherapy. Another study [14] also identified patients who experienced severe atypical toxicities following radiotherapy based on γ-H2AX expression analysis. However, no correlation was found by Werbrouck et al. [15] between the kinetics of the appearance of γ-H2AX foci and the severity of acute normal tissue reactions.
In this study, we measured the expression of γ-H2AX using flow cytometry in PBLs using both in vitro and in vivo assays, and investigated the pattern and kinetics of the appearance of γ-H2AX foci as predictive markers for the severity of OM in HNC patients treated with radiotherapy.
Methods
Patients and clinical conditions
Between November 2011 to June 2012, 31 patients with HNC treated at the Sixth People’s Hospital of Jiao Tong University were considered for enrollment in this study. The study was approved by the local ethics committee, and all patients provided written informed consent. Four patients were excluded from the study due to treatment interruptions. Two patients, who received X-ray examination or scintigraphy within 48 hours before collection of the first blood samples, were also excluded. The patients were irradiated with a 6MV X-ray linear accelerator (Artiste™ Solutions; Siemens, Germany). The mean dose of radiation was (66.2 ± 8.1) Gy, at 2 Gy per day administered 5 days per week. During radiotherapy, all patients received basic oral care.
Assessment of OM
OM assessments were performed by a specially-trained radiation oncologist twice a week. Evaluation of OM was based on the World Health Organization (WHO) classification (1 = soreness and erythema; 2 = ulcers, can eat solids; 3 = ulcers, requires liquid diet; 4 = ulcers, can not tolerate solid or liquid diet). The maximum toxicity score was used for this study. The dose-volume histogram (DVH) of oral mucosa was extracted for each patient. The entirety of the pharyngeal constrictor and oral cavity, which is considered to play an important role in the development of acute OM, was considered as “mucosa”. Contours of the oral cavity and the muscular structures of the swallowing were assessed based on previous reports [16, 17].
Isolation of PBLs
A 10-mL sample of peripheral venous blood was withdrawn from patients and placed into EDTA vacutainers. PBLs were isolated using lymphoprep™ (AXIS-SHIELD PoC AS, Oslo, Norway) according to the manufacturer’s instructions. Briefly, whole blood was diluted with an equal volume of phosphate-buffered saline (PBS), then the 20-mL of diluted blood samples were carefully layered onto 10 mL of lymphoprep™ and centrifuged at 800 × g for 20 minutes. Then, lymphocytes from the interphase were isolated and incubated at 37°C in a humidified atmosphere containing 5% CO2.
For the in vivo assay, blood samples were obtained from patients before radiotherapy (T0), 1 hour after the fourth fraction of radiotherapy (T1), and after the last fraction of radiotherapy (T2).
Blood samples obtained before radiotherapy were used for the in vitro assay. The lymphocytes were separated and divided for different experiments. For the damage kinetics assay, lymphocytes were irradiated at doses of 0, 2, 4, 6, and 8 Gy; for the repair kinetics assay, the cells was irradiated at a dose of 2 Gy and γ-H2AX expression was examined at 0, 0.5, 4, and 24 h post-irradiation.
γ-H2AX expression assay
The lymphocytes were fixed in 4% paraformaldehyde for 10 min and permeabilized in a 0.1% solution of Triton X-100 in PBS for 10 min. Subsequent detection of γ-H2AX expression was performed after blocking in 5% fetal bovine serum (FBS) for 30 min at room temperature, using a 1:1000 dilution of the flourescein isothiocyanate (FITC)-labeled mouse monoclonal antibody against γ-H2AX (Millipore). Following incubation with the primary antibody for 2 hours, the lymphocytes were analyzed by fluorescence-activated cell sorting (FACS) using flow cytometry and the Kaluza software package (Beckman Coulter). The fluorescence intensity in the cells post-irradiation was compared to that in untreated control cells to provide a measure of the relative fluorescence.
Statistical analysis
Statistical analysis was performed using SPSS 13.0 software. The effect of gender, treatment regimen, tumor staging, and tumor types on OM was evaluated using the χ2-square test; the independent t- test was used for analysis of continuous data. The relationship between the irradiation dose and relative fluorescence of γ-H2AX in PBLs was examined by linear regression analysis. Differences were considered significant when the p-value was less than 0.05. Receiver Operating Characteristic (ROC) analysis was performed and the cutoff value was determined based on the Youden index [18], and the corresponding sensitivity, specificity, and positive and negative predictive values were calculated.
Results
Clinical characteristics
The clinical characteristics of the patients are shown in Table 1. There were no differences in the clinical parameters between the mild and severe OM groups. Of the 25 patients, 15 patients had mild OM and were classified as grade 1–2, while 10 patients had severe OM and were classified as grade 3–4. The percentages for patients experiencing grade 1, 2, 3, and 4 OM were 12.0%, 48.0%, 32.0%, and 8.0%, respectively.
Relationship between the dose-distribution parameters of oral mucosa and OM
The correlation between the grades of radiation-induced OM and DVH data were analyzed (Table 2). From the DVHs of oral mucosa, mean dose (Dmean), maximal dose (Dmax), the percentage of mucosa in the contoured regions that received a dose equal to or higher than 15 Gy (V15), 30 Gy (V30), 40 Gy (V40), 50 Gy (V50), and 60 Gy (V60) were calculated. None of dose-distribution parameters of oral mucosa showed significant differences between patients with mild or severe OM (p >0.05).
Assessment of damage kinetics using γ-H2AX expression analysis in vitro
After irradiation of PBLs, the fluorescence of γ-H2AX increased with the irradiation dose (Figure 1). There was a strong linear correlation between the relative fluorescence of γ-H2AX in PBLs and the irradiation dose in the patients with severe (r = 0.998; p = 0.000) and mild (r = 0.976; p = 0.005) OM. The relative fluorescence of γ-H2AX in patients with severe OM was higher than that in patients with mild OM at each irradiation dose, and was particularly high at the irradiation dose of 8 Gy (p = 0.039).
Relationship of the applied dose of irradiation and the relative fluorescence of γ-H2AX. Peripheral blood lymphocytes (PBLs) from patients with severe (grey bard) and mild (white bars) oral mucositis (OM) were irradiated at 0, 2, 4, 6, and 8 Gy. At 1 hour after in vitro irradiation, the γ-H2AX-associated fluorescence intensity in the lymphocytes was assessed using a FACS-based assay. The γ-H2AX-associated fluorescence is expressed relative to that of untreated control PBLs. The values shown are the mean ± SD; *p < 0.05.
Assessment of repair kinetics using in vitro γ-H2AX expression analysis
As shown in Figure 2, the relative fluorescence intensity reached the maximum level at about 0.5 h after irradiation and decreased thereafter. At 24 hours, the relative fluorescence returned to levels comparable to that of un-irradiated PBLs in mild OM patients (Figure 2a), but not in patients with severe OM, indicating a slower rate of DNA repair in patients with severe OM (Figure 2b). Furthermore, there was a significantly higher retention of fluorescence at 24 hours post-irradiation in PBLs from the severe OM group, compared to the residual fluorescence in the mild OM group (p = 0.008) (Figure 2c), while no difference was observed at 0.5 and 4 hours post-irradiation (Figure 2c). These results suggest that higher residual DNA damage is present in patients with severe OM 24 hours after irradiation.
The time-dependent accumulation of irradiation-induced γ-H2AX in PBLs in vitro. The γ-H2AX fluorescence was measured using a FACS-based assay in PBLs isolated from 15 patients mild OM (a) and 10 patients with severe OM (b) at 0, 0.5, 4, and 24 hours after in vitro exposure to 2 Gy of X-ray radiation. (c) The mean level of the relative fluorescence for patients with severe OM (diamonds) and mild OM (squares); *p <0.05.
Cutoff value of γ-H2AX fluorescence for prediction of OM
To estimate the sensitivity and specificity of the relative fluorescence of γ-H2AX at 24 hours post-irradiation for prediction of OM during radiotherapy, ROC analysis was performed. The optimal cutoff value of residual γ-H2AX level 24 hours post-irradiation was determined from the ROC analysis (Figure 3). When a relative fluorescence of 0.960 was used as the cutoff value, the sensitivity and specificity of the γ-H2AX fluorescence in predicting OM were 100% and 53.3%, respectively, and positive and negative predictive values were 62.5% and 100%, respectively. The area under the curve (AUC) was 0.800 (standard error [SE], 0.094; 95% confidence interval [CI], 0.593–0.931; p = 0.002).
ROC curve of residual γ-H2AX fluorescence 24 h post-irradiation for determining the grades of OM. Receiver Operating Characteristic (ROC) analysis was performed by SPSS software and cutoff value was determined based on Youden index. The ordinate represents the true positive rate, the abscissa represents the false positive rate. The area under the curve (AUC) was used to assess the predictive value of γ-H2AX.
The dynamic change of γ-H2AX expression using the in vivo assay
To determine the correlation between the kinetic patterns of DNA damage and repair, as assessed using the γ-H2AX-specific fluorescence with the in vitro assay, and OM, the relative fluorescence of γ-H2AX was estimated in 15 patients with mild OM and 10 patients with severe OM at different time points during radiotherapy (Figure 4). Higher γ-H2AX levels were observed at the later time points of radiotherapy (p <0.05), but the increase in γ-H2AX expression was not statistically different between the two groups of patients at the three time points during radiotherapy (Figure 4, p <0.05).
The relationship of relative fluorescence of γ-H2AX and OM response to radiotherapy in vivo. Blood samples were collected from patients before radiotherapy (T0), 1 hour after the fourth fraction of radiotherapy (T1), and 1 hour after the last fraction of radiotherapy (T2) and the induction of γ-H2AX was assessed using a FACS-based assay.
Discussion
Development of severe radiation-induced OM during radiotherapy for patients with HNC results in treatment interruptions, hospitalization, and increased cost. Screening tests that can identify the patients at higher risk for developing severe OM would enable clinicians to individualize radiotherapy protocols.
The appearance of γ-H2AX foci in PBLs was found to be closely correlated with DNA DSBs after exposure to irradiation [6], and more rapid loss of γ-H2AX foci in human cell lines has been correlated with improved repair of DNA DSBs [10]. In the present study, flow cytometric analysis of γ-H2AX induction and removal was used to predict acute radiation-induced OM in HNC patients. The extent and kinetics of γ-H2AX expression levels were measured after in vitro irradiation of patient-derived PBLs, and the results of the in vitro assays were also compared with those of the in vivo analysis.
We found a strong linear correlation between the relative fluorescence of γ-H2AX in PBLs and irradiation dose in the patients with severe and mild OM, indicating that γ-H2AX might be useful as a biological marker of dosimetry after ionizing radiation exposure, which corroborates results in previous reports [19, 20]. On the other hand, our data showed that the dose per fractionation might be a key parameter that can be applied to estimate the role of the induction of γ-H2AX in predicting OM in HNC patients. In the present study, the induction of γ-H2AX by high-dose irradiation (8 Gy), but not other lower doses of irradiation (2, 4, or 6 Gy), was significantly different between the patients with severe and mild OM. These data suggest that the lack of support for a predictive role for γ-H2AX in OM reported previously may be due to the lower doses of irradiation used in prior study [15]. Werbrouck et al. [15] measured the number of γ-H2AX foci in T-lymphocytes isolated from HNC patients after in vitro irradiation at 0.5 Gy and were unable to predict the development of acute normal tissue complications. An irradiation dose of 2 Gy was used in the study by Vasireddy et al. [21], which suggested that the formation of γ-H2AX foci was not significantly different between patients with severe and mild OM. Taken together, our data suggest that the patients with severe OM had higher radiosensitivity of normal tissue than those with mild OM, and the higher single dose might be necessary in in vitro assays to evaluate the correlation between γ-H2AX induction and OM in the clinical setting.
The results of the repair kinetics assay showed that lymphocytes had a higher residual level of fluorescence of γ-H2AX at 24 h, but not at earlier times ( 0, 0.5, and 4 h), after irradiation with 2 Gy in patients with severe OM, compared with patients with mild OM. Our observations are consistent with those of other studies; Bourton et al. [14] examined γ-H2AX induction and depletion in 12 patients with acute or late normal tissue toxicity using the same technique used in this study and found elevated levels of γ-H2AX fluorescence at 24 h post-irradiation in patients with severe toxicities, compared with those who had experienced little or no adverse reaction. Results from the study by Goutham et al. [22] also suggested that lymphocytes from the patients before radiotherapy had a higher residual level of fluorescence of γ-H2AX at later times (24 h) after in vitro irradiation with 2 Gy, more so in patients who developed severe OM. These results indicate that patients with severe OM are more likely to exhibit DNA repair deficiencies. Therapy-related factors that may have an important bearing on the development of mucositis, such as the use of chemotherapy and the irradiation dose to the oral cavity, were not taken into account as confounding factors in these studies [14, 22]. In the present study, the related parameters from DVH with respect to oral cavity and mucosa, including Dmax, Dmean, and V30, were measured and found to be similar between the patients with severe and mild OM (p >0.05); therefore, the differences between the dose to and volume of the oral mucosa did not account for the differences between the patients with severe and mild OM. Moreover, despite the different proportion of the patients with severe (8/10) and mild (9/15) OM undergoing chemoradiotherapy, there were no differences in treatment regime between patients with mild and severe OM (p = 0.402). Taken together, these confounding factors (concurrent chemo, dose to, and volume of the oral mucosa) were eliminated. However, the absence of the influence of concurrent chemotherapy, dose to, and volume of the oral mucosa on OM in our study may be due to the small sample size, a limitation of this study. In our analyses, the level of γ-H2AX-associated fluorescence at 24 h post-irradiation was a major contributor to the differences in the severity of acute OM. Therefore, along with that of other reports, our data indicated that the patients with severe OM had a reduced capacity for DNA repair.
ROC analysis was further used to confirm the predictive value of γ-H2AX expression, and the relative fluorescence intensity of γ-H2AX (0.965) at 24 h post-irradiation was the optimal cutoff value, with an AUC value close to 0.8 and sensitivity, specificity, and positive and negative predictive values being 100%, 53.8%, 62.5%, and 100%, respectively. These data indicate that the H2AX expression-based method used for predicting OM had fair coverage of the whole cohort and that HNC patients with relative fluorescence intensities <0.96 after in vitro irradiation would be highly likely to experience mild mucositis. The relatively lower value for the specificity and positive predictive value with the γ-H2AX expression-based approach may be a result of pharmaceutical modifiers and the lower irradiation doses applied to two of the patients (with non-hodgkin’s lymphoma) in our study.
To our knowledge, there are no previous reports of clinical data focused on the detection and predictive role of γ-H2AX in radiotherapy-induced OM, using both in vivo and in vitro assays. Measurement of the accumulation of DNA damage with the γ-H2AX-based assay has been demonstrated to enable identification of minor impairments in the DSB-repair capacity, which could not be detected after single-dose irradiation in a preclinical murine model [23]. In our study, although higher levels of γ-H2AX were observed when the patients received a higher dose of irradiation, indicating that the γ-H2AX assay reflected the accumulation of incomplete repair of sublethal damage, the enhancements of γ-H2AX expression on the fourth and last days after fractionated irradiation were not statistically different between the patients with mild and severe OM. The lack of differences between the two groups should not be seen as a failing of the role of DNA damage accumulation, since there are many factors involved in the in vivo analysis of γ-H2AX expression, such as the mixture of irradiated and non-irradiated blood lymphocytes in the blood samples, which may confound the analysis. Other complicating factors include the continuous exchange of lymphocytes between blood and tissues and elimination of highly damaged lymphocytes from blood [24]. Our results prove that the detection of γ-H2AX accumulation induced by irradiation can be used to predict the incidence and severity of normal tissue toxicities like OM. We propose that the in vitro analysis needs to be performed before radiotherapy with higher doses and over a longer observation period. In conclusion, our data support the further development of the H2AX-based method as a rapid and convenient to identify patients with higher risk of developing severe OM during radiotherapy.
Although we have observed a correlation between γ-H2AX induction and the grade of OM prior to radiotherapy, other studies have not demonstrated such a relationship [15, 25]. The discrepancies in results among studies may be primarily due to technical differences in the methodologies implemented, the endpoints, and different clinicopathological characteristics of the study populations. Immunoflurorescence-based microscopic analysis of γ-H2AX is one of the methods for detection of DNA damage after irradiation. However, manual counting used in such microscopic analysis may be less accurate, especially in samples with a greater number of foci, which overlap or coalescence, such as those observed at dose ranges >2 Gy [26]. Flow cytometry is an objective and rapid method for the detection of γ-H2AX signal intensity [14]. These qualities make flow cytometry more attractive for use in the detection and quantification of γ-H2AX intensity in clinical samples.
In addition to the application of γ-H2AX-based approaches for the prediction of acute normal tissue damage, some authors also investigated the role of the γ-H2AX in the prediction of late normal tissue toxicities. However, those studies failed to demonstrate a relationship between the number or intensity of γ-H2AX foci and late radiation sensitivity [27, 28]. The lack of correlation may be explained by the fact that other factors, in addition to DNA repair mechanisms, such as fibrotic and inflammatory processes, play an important role in the induction of late adverse effects.
Conclusion
In conclusion, our data demonstrate that the H2AX-based method is suitable for application in a clinical setting. Flow cytometric analysis of γ-H2AX fluorescence allowed assessment of DNA damage and DSB repair capacity in individual HNC patients after irradiation. The dynamic changes in γ-H2AX fluorescence were evident at higher doses of irradiation and over longer periods of time after in vitro irradiation. However, the limited number of patients is a significant limitation of our study, and these observation need to be extended and confirmed in a larger cohort to thoroughly address the utility of the H2AX expression-based approach in predicting the severity of OM in HNC patients undergoing radiotherapy.
Abbreviations
- OM:
-
Oral mucositis
- HNC:
-
Head and neck cancer
- DSBs:
-
DNA double strand breads
- PBL:
-
Peripheral blood lymphocytes
- DVH:
-
Dose-volume histogram
- PBS:
-
Phosphate-buffered saline
- ROC:
-
Receiver Operating Characteristic
- AUC:
-
The area under the curve.
References
Cox JD, Stetz J, Pajak TF: Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995, 31: 1341-1346. 10.1016/0360-3016(95)00060-C
Giro C, Berger B, Bölke E, Ciernik IF, Duprez F, Locati L, Maillard S, Ozsahin M, Pfeffer R, Robertson AG, Langendijk JA, Budach W: High rate of severe radiation dermatitis during radiation therapy with concurrent cetuximab in head and neck cancer: Results of a survey in EORTC institutes. Radiother Oncol 2009, 90: 166-171. 10.1016/j.radonc.2008.09.007
Rosenthal DI: Consequences of mucositis-induced treatment breaks and dose reductions on head and neck cancer treatment outcomes. J Support Oncol 2007, 5: 23-31.
Tucker SL, Geara FB, Peters LJ, Brock WA: How much could the radiotherapy dose be altered for individual patients based on a predictive assay of normal tissue radiosensitivity? Radiother Oncol 1996, 38: 103-113. 10.1016/0167-8140(95)01669-4
Begg AC: Can the severity of normal tissue damage after radiation therapy be predicted? PLoS Med 2006, 3: e440. 10.1371/journal.pmed.0030440
Bentzen SM: Preventing or reducing late side effects of radiation therapy: radiobiology meets molecular pathology. Nat Rev Cancer 2006, 6: 702-713. 10.1038/nrc1950
Kühne M, Riballo E, Rief N, Rothkamm K, Jeggo PA, Löbrich M: A double-strand break repair defect in ATM-deficient cells contributes to radiosensitivity. Cancer Res 2004, 64: 500-508. 10.1158/0008-5472.CAN-03-2384
Kuo LJ, Yang LX: Gamma-H2AX - a novel biomarker for DNA double-strand breaks. In Vivo 2008, 22: 305-309.
Rübe CE, Grudzenski S, Kühne M, Dong X, Rief N, Löbrich M, Rübe C: DNA double-strand break repair of blood lymphocytes and normal tissues analysed in a preclinical mouse model: implications for radiosensitivity testing. Clin Cancer Res 2008, 14: 6546-6555. 10.1158/1078-0432.CCR-07-5147
Redon CE, Dickey JS, Bonner WM, Sedelnikova OA: γ-H2AX as a biomarker of DNA damage induced by ionizing radiation in human peripheral blood lymphocytes and artificial skin. Adv Space Res 2009, 43: 1171-1178. 10.1016/j.asr.2008.10.011
Olive PL, Banáth JP: Phosphorylation of histone H2AX as a measure of radiosensitivity. Int J Radiat Oncol Biol Phys 2004, 58: 331-335. 10.1016/j.ijrobp.2003.09.028
Fleckenstein J, Kuhne M, Seegmuller K, Derschang S, Melchior P, Graber S, Fricke A, Rube CE, Rube C: The impact of individual in vivo repair of DNA double-strand breaks on oral mucositis in adjuvant radiotherapy of head-and-neck cancer. Int J Radiat Oncol Biol Phys 2011, 81: 1465-1472. 10.1016/j.ijrobp.2010.08.004
Rübe CE, Fricke A, Schneider R, Simon K, Kühne M, Fleckenstein J, Gräber S, Graf N, Rübe C: DNA repair alterations in children with pediatric malignancies: novel opportunities to identify patients at risk for high-grade toxicities. Int J Radiat Oncol Biol Phys 2010,78(2):359-369. 10.1016/j.ijrobp.2009.08.052
Bourton EC, Plowman PN, Smith D, Arlett CF, Parris CN: Prolonged expression of the gamma-H2AX DNA repair biomarker correlates with excess acute and chronic toxicity from radiotherapy treatment. Int J Cancer 2011, 129: 2928-2934. 10.1002/ijc.25953
Werbrouck J, Duprez F, De Neve W, Thierens H: Lack of a correlation between γH2AX foci kinetics in lymphocytes and the severity of acute normal tissue reactions during IMRT treatment for head and neck cancer. Int J Radiat Biol 2011, 87: 46-56. 10.3109/09553002.2010.518213
Werbrouck J, De Ruyck K, Duprez F, Veldeman L, Claes K, Van Eijkeren M, Boterberg T, Willems P, Vral A, De Neve W, Thierens H: Acute normal tissue reactions in head-and-neck cancer patients treated with imrt: influence of dose and association with genetic polymorphisms in DNA DSB repair genes. Int J Radiat Oncol Biol Phys 2009, 73: 1187-1195. 10.1016/j.ijrobp.2008.08.073
Eisbruch A, Schwartz M, Rasch C, Vineberg K, Damen E, Van As CJ, Marsh R, Pameijer FA, Balm AJ: Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: Which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys 2004, 60: 1425-1439. 10.1016/j.ijrobp.2004.05.050
Fluss R, Faraggi D, Reiser B: Estimation of the Youden Index and its associated cutoff point. Biom J 2005, 47: 458-472. 10.1002/bimj.200410135
Roch-Lefevre S, Mandina T, Voisin P, Gaetan G, Mesa JE, Valente M, Bonnesoeur P, Garcia O, Roy L: Quantification of gamma-H2AX foci in human lymphocytes: a method for biological dosimetry after ionizing radiation exposure. Radiat Res 2010, 174: 185-194. 10.1667/RR1775.1
Rothkamm K, Balroop S, Shekhdar J, Fernie P, Goh V: Leukocyte DNA damage after multi-detector row CT: a quantitative biomarker of low-level radiation exposure. Radiology 2007, 242: 244-251. 10.1148/radiol.2421060171
Vasireddy RS, Sprung CN, Cempaka NL, Chao M, McKay MJ: H2AX phosphorylation screen of cells from radiosensitive cancer patients reveals a novel DNA double-strand break repair cellular phenotype. Br J Cancer 2010, 102: 1511-1518. 10.1038/sj.bjc.6605666
Goutham HV, Mumbrekar KD, Vadhiraja BM, Fernandes DJ, Sharan K, Kanive Parashiva G, Kapaettu S, Bola Sadashiva SR: DNA Double-Strand Break Analysis by gamma-H2AX Foci: A Useful Method for Determining the Overreactors to Radiation-Induced Acute Reactions Among Head-and-Neck Cancer Patients. Int J Radiat Oncol Biol Phys 2012, 84: e607-e612. 10.1016/j.ijrobp.2012.06.041
Rube CE, Fricke A, Wendorf J, Stutzel A, Kuhne M, Ong MF, Lipp P, Rube C: Accumulation of DNA double-strand breaks in normal tissues after fractionated irradiation. Int J Radiat Oncol Biol Phys 2010, 76: 1206-1213. 10.1016/j.ijrobp.2009.10.009
Sak A, Grehl S, Erichsen P, Engelhard M, Grannass A, Levegrun S, Pottgen C, Groneberg M, Stuschke M: gamma-H2AX foci formation in peripheral blood lymphocytes of tumor patients after local radiotherapy to different sites of the body: dependence on the dose-distribution, irradiated site and time from start of treatment. Int J Radiat Biol 2007, 83: 639-652. 10.1080/09553000701596118
Brzozowska K, Pinkawa M, Eble MJ, Müller WU, Wojcik A, Kriehuber R, Schmitz S: In vivo versus in vitro individual radiosensitivity analysed in healthy donors and in prostate cancer patients with and without severe side effects after radiotherapy. Int J Radiat Biol 2012, 88: 405-413. 10.3109/09553002.2012.666002
Sak A, Stuschke M: Use of γH2AX and other biomarkers of double-strand breaks during radiotherapy. Semin Radiat Oncol 2010,20(4):223-31. 10.1016/j.semradonc.2010.05.004
Albino AP, Huang X, Jorgensen ED, Gietl D, Traganos F, Darzynkiewicz Z: Induction of DNA double-strand breaks in A549 and normal human pulmonary epithelial cells by cigarette smoke is mediated by free radicals. Int J Oncol 2006, 28: 1491-1505.
Werbrouck J, De Ruyck K, Beels L, Vral A, Van Eijkeren M, De Neve W, Thierens H: Prediction of late normal tissue complications in RT treated gynaecological cancer patients: potential of the gamma-H2AX foci assay and association with chromosomal radiosensitivity. Oncol Rep 2010, 23: 571-578.
Acknowledgements
This article is funded by the research grant (YG2012ZD02, 12JC1407400) from Shanghai Jiaotong University and the Science and Technology Commission of Shanghai, China and the grant (81272506, 61227017) from National Natural Science Foundation of China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests in this study.
Authors’ contributions
PL and SF designed the study. PL, CD, QZ and ZL aided in data collection. PL and CD performed the statistical analysis and draft the manuscript. WX, PL and ZS performed the γ-H2AX analysis. All authors read and approved the final manuscript.
Ping Li, Cheng-run Du contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Li, P., Du, Cr., Xu, Wc. et al. Correlation of dynamic changes in γ-H2AX expression in peripheral blood lymphocytes from head and neck cancer patients with radiation-induced oral mucositis. Radiat Oncol 8, 155 (2013). https://doi.org/10.1186/1748-717X-8-155
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1748-717X-8-155