Abstract
Purpose
Prostate cancer is the leading form of cancer diagnosed among North American men. Most patients present with localized disease, which can be effectively treated with a variety of different modalities. These are associated with widely different acute and late effects, which can be both physical and psychological in nature. HRQoL concerns are therefore important for these patients for selecting between the different treatment options.
Materials and methods
One year after receiving radiotherapy for localised prostate cancer 117 patients with localized prostate cancer were invited to participate in a quality of life (QoL) self reported survey. 111 patients consented and participated in the survey, one year after completion of their treatment. 88 patients received EBRT and 23 received EBRT and HDRBT. QoL was compared in the two groups by using a modified version of Functional Assessment of Cancer Therapy-Prostate (FACT-P) survey instrument.
Results
One year after completion of treatment, there was no significant difference in overall QoL scores between the two groups of patients. For each component of the modified FACT-P survey, i.e. physical, social/family, emotional, and functional well-being; there were no statistically significant differences in the mean scores between the two groups.
Conclusion
In prostate cancer patients treated with EBRT alone versus combined EBRT and HDRBT, there was no significant difference in the QoL scores at one year post-treatment.
Similar content being viewed by others
Background
Prostate cancer is the leading form of cancer diagnosed among Canadian men and accounts for approximately 27% of new cancer cases and 11.4% of cancer deaths [1, 2]. Most newly diagnosed patients with prostate cancer present with localized disease [3]. EBRT is a treatment option for patients with early-stage or locally advanced prostate cancer [4]. Recent data suggest that local control of prostate cancer is directly related to the radiation dose which would in turn result in improved biochemical control, disease-free survival and increased overall survival [5]. Various dose escalation methods are available including three-dimensional conformal radiotherapy (3D-CRT) or intensity-modulated radiotherapy (IMRT) with or without low-dose rate (LDR), high-dose rate (HDR) or particle beam boost [6–9].
Health related quality of life (HRQoL) is a subjective measure of a patient's perception of well-being. HRQoL concerns are important for patients with prostate cancer for selecting between different treatments options which may result in physical and psychological sequelae that would affect their daily lives. Evaluation of the quality of life (QoL) among cancer patients who had received radiation using different radiotherapeutic techniques certainly helps both patients and physicians to make a more informed decision on their treatment.
The main objective of this study was to compare prospectively HRQoL at one year after treatment in prostate cancer patients treated with either EBRT alone or a combination of EBRT and iridium HDRBT.
Patients and methods
Patient characteristics
This is a prospective study carried out among patients with localized prostate cancer during the period January 2000 to December 2002, in the department of Radiation Oncology at the Allan Blair Cancer Center (ABCC), in Regina, Canada. One of the standard treatment options for these patients during this period was EBRT alone. We started the prostate HDRBT program at the ABCC in 1999. Since then, HDRBT was used as an alternative method of dose escalation in patients with locally advanced prostate cancer who have received EBRT.
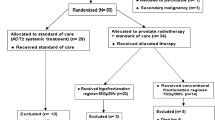
Patients in our study (Table 1) belonged to the intermediate or high risk groups with the following features: histological diagnosis of adenocarcinomas of the prostate, pretreatment PSA ≤ 20 ng/ml (mean), clinical stage T1c -T3a, prostate volume ≤ 60 cc, no evidence of lymphadenopathy on the pelvic CT scan, and a negative bone scan. During the above time period, 117 patients met the above criteria were treated at our institution with either EBRT alone or a combination of EBRT plus HDRBT.
Radiotherapy details
All the patients who received EBRT were treated by using 3D-CRT with a 4-field box technique using 10-MV or higher-energy photons. The EBRT alone group received a total dose of 66–70 Gy in 33 – 35 fractions (2-Gy per fraction) over six and half to seven weeks. This was the standard EBRT dose during that period (although considered to be low compared to current standards). EBRT was delivered in two phases. The planning target volume (PTV) for the initial phase included the prostate gland and seminal vesicles with a margin of 1–2 cm receiving a dose of 40 Gy in 20 fractions (2-Gy per fraction) over four weeks. The boost phase PTV for EBRT only group was defined as the prostate with a margin of 0.7–1 cm and received a dose of 26–30 Gy in 13–15 fractions (2-Gy per fraction) over two and half to three weeks at the discretion of the treating Radiation Oncologist. None of the patients received regional nodal radiation. Patients who were in the EBRT plus HDRBT treatment group received HDRBT initially followed by EBRT. Iridium-192 HDRBT was performed via a transperineal approach, delivering a total dose of 16.5 Gy in 3 fractions within 24 hours with a minimum gap of six hours between fractions. PTV for the brachytherapy treatment consists of the entire prostate gland and capsule with a margin of 2–3 mm. EBRT was given two weeks after HDRBT delivering a dose of 40 Gy at 2 Gy per fraction over 4 weeks.
Quality of life questionnaire
All one hundred and seventeen patients who underwent either EBRT alone or a combination of EBRT plus HDRBT were invited to participate in an institutional review board approved self-reported QoL survey at one year after completion of their radiation treatment. One hundred and eleven patients consented and participated in the survey. Eighty-eight patients of 111 received EBRT alone and 23 patients received combined EBRT and HDRBT. The survey was conducted using a modified version of the Functional Assessment of Cancer Therapy-Prostate (FACT-P) survey instrument (version 3). Results between the two treatment groups were compared using a paired t-test.
Results
Characteristics of the study population, according to treatment received, are shown in Table 1. Median age was identical between patients treated with EBRT alone and those treated with EBRT and HDRB. Approximately 2/3 of patients in both groups had stage T2 disease. There were no significant differences between the two groups with respect to the distribution of established risk factors (stage, Gleason score and PSA).
Table 2 shows modified FACT-P scores at one year for the two different treatment groups. There was no significant difference in overall QoL between the two groups (p = 0.668). For each component of the modified FACT-P survey, i.e. Physical Well-Being, Social/Family Well-Being, Emotional Well-Being, and Functional Well-Being, there was no statistically significant difference in the mean scores between the two groups.
Discussion
Patients with prostate cancer can live for many years regardless of the treatment they receive due to the long natural history. As a result, HRQoL has become an important outcome measure in patients with this disease. Different survey instruments are designed to assess HRQoL of patients with prostate cancer [3, 10, 11]. We have conducted our survey by using a modified version of FACT-P (version 3) survey tool [12, 13] The structure of FACT-P (version 3) survey instrument comprising a 47-item questionnaire, which is divided into four primary QoL domains: physical, social/family, emotional, and functional well-being, plus a 12-item prostate cancer subscale. These 12-items ask about symptoms and problems specific to prostate cancer. Higher total scores for the FACT-P scale indicate a better overall QoL. The modified survey instrument has a total of 50 questions and the only modification is in the prostate subscale for the purpose of accommodating symptoms related to radiation induced late toxicity (Table 3).
Sathya et al reported a randomized study in which patients with locally advanced prostate cancer were treated with EBRT alone or combination of EBRT and iridium HDRBT. The study showed no difference in the toxicity scores between the two arms at 18 months of follow up [9]. This study also provided evidence that higher doses of radiation delivered by the combination treatment resulted in better local as well as biochemical control in locally advanced prostate cancer. Other studies have also reported improved local control following dose escalation with 3D-CRT or IMRT [7, 8]. The risks of long-term morbidity, following dose escalation by various methods are incompletely understood yet and they could have a significant impact on post treatment QoL.
Various studies have demonstrated the significance of HRQoL assessment when considering different treatment options for prostate cancer and suggested that recommended treatment decisions should take into account HRQoL in addition to survival [12, 13]. Wei et al reported a comparative HRQoL outcome study for patients with localized prostate cancer who underwent brachytherapy, radical prostatectomy or EBRT [14]. Higher FACT-P scores were reported in patients treated with EBRT than with brachytherapy. The authors concluded that the HRQoL changes are likely to be treatment-specific. Welsh et al compared the baseline to six months post treatment QoL of 10 patients with prostate cancer treated with EBRT plus HDRBT [15]. They found that the median QoL scores were comparable to baseline values at six months and concluded that EBRT plus HDRBT is an acceptable treatment when QoL is considered.
Our study compared HRQoL among patients with localized prostate cancer who had undergone radical treatment using the two different radiation techniques. Our findings indicated that both groups had similar QoL outcomes at the end of one year of treatment. Vordermark D et al reported the results of a similar study among 84 prostate cancer patients treated with either EBRT alone or EBRT plus HDRBT [16]. The study showed comparable QoL data between the two groups at a median duration of 19 months post treatment. HRQoL differences may not become apparent at the end of one to two years of completion of treatment and hence a longer follow up might be helpful to see the difference. Wahlgren T et al reported the five year disease-specific HRQoL of patients with localized prostate cancer following combined treatment including EBRT, HDRBT and hormone therapy [17]. The long term data reported that only minor differences in general HRQoL compared with normative data. We are in the process of reviewing HRQoL of our patients at five years post treatment.
Our data may have significant implications. While offering curative radiation treatment, most of the patients are interested to know how the different treatments compare to one another in terms of survival, long term morbidity and HRQoL. Our study showed the significance of the evaluation of QoL which would help both patients and physicians to make more informed decisions between different treatment techniques.
A potential limitation of our study is that this is a single-institutional non-randomised study with a small sample size in the EBRT plus HDRBT arm. In addition the study lacks baseline HRQoL information. Radiation doses are also low by today's standards. However the study does help to minimise concerns of using combination treatment as an alternative for dose escalation when QoL is considered.
Conclusion
Our study showed that the impact of prostate cancer treatments such as EBRT alone vs. combination of EBRT and HDRBT on HRQoL was comparable at one year after completion of treatment. Prospective randomized studies are needed to confirm these findings. In addition, an understanding of the relative HRQoL would help clinicians and patients to make informed choices between different treatment options that may offer a similar chance of tumor control.
References
Canadian Cancer Society/National Cancer Institute of Canada: Canadian Cancer Statistics 2008. Toronto, Canada 2008.
Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, Thun MJ: Cancer statistics 2006. CA Cancer J Clin 2006, 56: 106-130.
Joly F, Brune D, Couette JE, Lesaunier F, Heron JF, Peny J, Henry-Amar M: Health-related quality of life and sequelae in patients treated with brachytherapy and external beam irradiation for localized prostate cancer. Ann Oncol 1998, 9: 751-757. 10.1023/A:1008276632623
Hsu IC, Cabrera AR, Weinberg V, Speight J, Gottschalk AR, Roach M 3rd, Shinohara K: Combined modality treatment with high-dose-rate brachytherapy boost for locally advanced prostate cancer. Brachytherapy 2005, 4: 202-206. 10.1016/j.brachy.2005.03.005
Al-Salihi O, Mitra A, Payne H: Challenge of dose escalation in locally advanced unfavourable prostate cancer using HDR brachytherapy. Prostrate Cancer Prostatic Dis 2006, 9: 370-373. 10.1038/sj.pcan.4500893
Pinkawa M, Fischedick K, Treusacher P, Asadpour B, Gagel B, Piroth MD, Borchers H, Jakse G, Eble MJ: Dose-volume impact in high-dose-rate Iridium-192 brachytherapy as a boost to external beam radiotherapy for localized prostate cancer- a phase II study. Radiother Oncol 2006, 78: 41-46. 10.1016/j.radonc.2005.10.003
Dearnaley DP, Hall E, Lawrence D, Huddart RA, Eeles R, Nutting CM, Gadd J, Warrington A, Bidmead M, Horwich A: Phase III pilot study of dose escalation using conformal radiotherapy in prostate cancer: PSA control and side effects. Br J Cancer 2005, 92: 488-498. 10.1038/sj.bjc.6602624
Zelefsky MJ, Fuks Z, Hunt M, Lee HJ, Lombardi D, Ling CC, Reuter VE, Venkatraman ES, Leibel SA: High dose radiation delivered by intensity modulated conformal radiotherapy improves the outcome of localized prostate cancer. J Urol 2001, 166: 876-881. 10.1016/S0022-5347(05)65855-7
Sathya JR, Davis IR, Julian JA, Guo Q, Daya D, Dayes IS, Lukka HR, Levine M: Randomized trial comparing iridium implant plus external-beam radiation therapy with external-beam radiation therapy alone in nodenegative locally advanced cancer of the prostate. Clin Oncol 2005, 23: 1192-9. 10.1200/JCO.2005.06.154
Esper P, Mo F, Chodak G, Sinner M, Cella D, Pienta KJ: Measuring quality of life in men with prostate cancer using the functional assessment of cancer therapy-prostate instrument. Urology 1997, 50: 920-928. 10.1016/S0090-4295(97)00459-7
Ferrer M, Suárez JF, Guedea F, Fernández P, Macías V, Mariño A, Hervas A, Herruzo I, Ortiz MJ, Villavicencio H, Craven-Bratle J, Garin O, Aguiló F: Multicentric Spanish Group of Clinically Localized Prostate Cancer.Health-Related Quality of Life 2 Years After Treatment with Radical Prostatectomy, Prostate Brachytherapy, or External Beam Radiotherapy in Patients with Clinically Localized Prostate Cancer. Int J Radiat Oncol Biol Phys 2008 Mar 4
DF Cella, DS Tulsky, G Gray, B Sarafian, E Linn, A Bonomi, M Silberman, SB Yellen, P Winicour, J Brannon: The Functional Assessment of Cancer Therapy (FACT) scale: development and validation of the general measure. J Clin Oncol 1993, 11: 570-579.
Wang H, Huang E, Dale W, Campbell T, Ignacio L, Kopnick M, Ray P, Vijayakumar S: Self-assessed health-related quality of life in men who have completed radiotherapy for prostate cancer: instrument validation and its relation to patient-assessed bother of symptoms. Int J Cancer 2000, 90: 163-172. 10.1002/1097-0215(20000620)90:3<163::AID-IJC7>3.0.CO;2-Q
Wei JT, Dunn RL, Sandler HM, McLaughlin PW, Montie JE, Litwin MS, Nyquist L, Sanda MG: Comprehensive comparison of health-related quality of life after contemporary therapies for localized prostate cancer. J Clin Oncol 2002, 20: 557-566. 10.1200/JCO.20.2.557
Welsh L, Lydon A, Ingham D: Pilot Study to Assess the Quality of Life and Toxicity in Patients with Carcinoma of the Prostate undergoing External Beam Radiotherapy Plus High Dose Rate Brachytherapy Boost. Clin Oncol 2007, 19: S49. 10.1016/j.clon.2007.01.431
Vordermark D, Wulf J, Markert K, Baier K, Kölbl O, Beckmann G, Bratengeier K, Noe M, Schön G, Flentje M: 3-D conformal treatment of prostate cancer to 74 Gy vs. high-dose-rate brachytherapy boost: a cross-sectional quality-of-life survey. Acta Oncol 2006, 45: 708-16. 10.1080/02841860600710913
Wahlgren T, Nilsson S, Lennernäs B, Brandberg Y: Promising long-term health-related quality of life after high-dose-rate brachytherapy boost for localized prostate cancer. Int J Radiat Oncol Biol Phys 2007, 69: 662-70.
Acknowledgements
Authors thank Dr.A Firth who has initiated the study
Authors thank Dr.MC Ambrose for helping for preparation of manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
KJJ wrote the manuscript and supported with data analysis. RA collected the data, enrolled patients and performed the statistical analysis. DS critically reviewed the manuscript. JT critically reviewed the manuscript. NP critically reviewed the manuscript. CS critically reviewed the manuscript. PT supported the data collection, enrolled patients and critically reviewed the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Joseph, K.J., Alvi, R., Skarsgard, D. et al. Analysis of health related quality of life (HRQoL) of patients with clinically localized prostate cancer, one year after treatment with external beam radiotherapy (EBRT) alone versus EBRT and high dose rate brachytherapy (HDRBT). Radiat Oncol 3, 20 (2008). https://doi.org/10.1186/1748-717X-3-20
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1748-717X-3-20