Abstract
Background
Methicillin-resistant coagulase-negative staphylococci (MR-CNS) are of increasing importance to animal and public health. In veterinary medicine and along the meat and milk production line, only limited data were so far available on MR-CNS characteristics. The aim of the present study was to evaluate the prevalence of MR-CNS, to identify the detected staphylococci to species level, and to assess the antibiotic resistance profiles of isolated MR-CNS strains.
Results
After two-step enrichment and growth on chromogenic agar, MR-CNS were detected in 48.2% of samples from livestock and chicken carcasses, 46.4% of samples from bulk tank milk and minced meat, and 49.3% of human samples. Using matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS), 414 selected MR-CNS strains belonged to seven different species (S. sciuri, 32.6%; S. fleurettii, 25.1%; S. haemolyticus, 17.4%; S. epidermidis, 14.5%, S. lentus, 9.2%; S. warneri, 0.7%; S. cohnii, 0.5%). S. sciuri and S. fleurettii thereby predominated in livestock, BTM and minced meat samples, whereas S. epidermidis and S. haemolyticus predominated in human samples. In addition to beta-lactam resistance, 33-49% of all 414 strains were resistant to certain non-beta-lactam antibiotics (ciproflaxacin, clindamycin, erythromycin, tetracycline).
Conclusions
A high prevalence of MR-CNS was found in livestock production. This is of concern in view of potential spread of mecA to S. aureus (MRSA). Multiresistant CNS strains might become an emerging problem for veterinary medicine. For species identification of MR-CNS isolated from different origins, MALDI-TOF MS proved to be a fast and reliable tool and is suitable for screening of large sample amounts.
Similar content being viewed by others
Background
It is assumed that methicillin-resistance genes had evolved in coagulase-negative staphylococci (CNS) and were then horizontally transferred among staphylococci [1, 2]. Particularly S. sciuri [3] and S. fleurettii [4] are discussed as natural reservoir of the methicillin-resistance gene mecA. The mecA gene is located on a mobile genetic element called staphylococcal cassette chromosome (SCC) and confers resistance to methicillin by encoding an altered penicillin-binding protein (PBP2α), which shows limited affinity to beta-lactam antibiotics. The mecA gene is now distributed among both coagulase-positive and -negative staphylococcal species.
In recent years, the isolation of methicillin-resistant CNS (MR-CNS) from diverse sources was reported. Dakic et al. [5] detected MR-CNS on medical devices, Silva et al. [6] in healthy humans, de Mattos et al. [7] and Ruppe et al. [8] in ambulatory patients, and Diekema et al. [9] in human bloodstream infections. According to Kloos and Bannerman [10], S. epidermidis and S. haemolyticus are the principal pathogens involved in foreign body infections. Miragaia et al. [11] discussed S. epidermidis as one of the most important causes for hospital-acquired bacteremia and found many isolates from hospitalized patients to be methicillin-resistant. Recently, several authors reported MR-CNS also in healthy animals. The existence of MR-CNS in animals was first described by Kawano et al. [12], who detected MR-CNS in chicken. Worldwide, MR-CNS were isolated from horses [13–15], dogs [15], cattle [16, 17], as well as from sheep, goats, and pigs [17]. However, MR-CNS were also found in animals with clinical infections. Van Duijkeren et al. [18] detected methicillin-resistant S. haemolyticus from cats with cystitis and rhinitis, from dogs with bronchitis and pyoderma, and from a horse with vaginitis. Moreover, Fessler et al. [19] reported different MR-CNS species in association with bovine mastitis.
However, comprehensive data on MR-CNS along the meat and milk production line were so far missing. The present work is a subsequent study of a previously published study on the prevalence of MRSA in Switzerland. The aim of the present study was to evaluate the occurrence of MR-CNS in livestock (cows, calves, pigs) and chicken carcasses, bulk tank milk (BTM) and minced meat, as well as people in contact with farm animals (veterinarians, pig farmers, and employees of a chicken and a pig and cattle abattoir), to identify the occurring CNS species, and to assess antibiotic resistance profiles of isolated strains.
Results
MR-CNS occurrence
Using the described procedure, MR-CNS were detected in 1'013 (48.3%) of the 2'099 analyzed samples from livestock and chicken carcasses, BTM and minced meat, and humans (Table 1). Amongst the 1'428 samples from livestock and chicken carcasses, MR-CNS were found in 48.2% of samples. Thereby, the proportion of positive samples ranged from 36.3% in pigs to 72.0% in calves. Analysis of the 211 samples from BTM and minced meat yielded an average MR-CNS occurrence of 46.4% (32.4% in meat and 62.0% in BTM). Of the 460 human samples, 49.3% turned out to test positive for MR-CNS (from 26.3% in slaughterhouse employees to 67.6% in pig farmers).
Species identification
A total of 414 strains were selected and subjected to species identification using MALDI-TOF MS. Amongst samples, seven different CNS species were detected (Table 2). Sequencing of sodA from a subset of 25 strains (5 S. sciuri; 5 S. fleurettii; 5 S. haemolyticus; 5 S. epidermidis; 3 S. lentus; 1 S. cohnii; 1 S. warneri) confirmed the results obtained by MALDI-TOF MS. Overall, S. sciuri (32.6%) and S. fleurettii (25.1%) were most frequently found, followed by S. haemolyticus (17.4%), S. epidermidis (14.5%), and S. lentus (9.2%). Moreover, S. cohnii and S. warneri were only rarely identified (<1.0%).
Within the 191 selected MR-CNS strains of animal origin, the majority of strains was identified as S. sciuri (63.4% of strains), followed by S. fleurettii (17.8%), S. lentus (15.7%), S. haemolyticus (1.6%), S. epidermidis (1.0%), and S. warneri (0.5%). Thirty of the 38 S. lentus strains isolated originated from chicken. Of the 51 strains isolated from calves, 50 were identified as S. sciuri. The 52 strains from pigs were identified as S. sciuri (55.8%) and S. fleurettii (44.2%). The 50 MR-CNS strains isolated from cows also mainly consisted of S. sciuri (72.0%) and S. fleurettii (22.0%).
Of the 84 MR-CNS strains isolated from BTM and minced meat samples, 76.2% of strains were identified as S. fleurettii, followed by 15.5% of strains identified as S. sciuri. The remaining seven strains belonged to S. haemolyticus (n = 3), S. epidermidis (n = 2), S. cohnii (n = 1), and S. warneri (n = 1).
Of the 139 MR-CNS strains isolated from humans, S. haemolyticus (47.5%) and S. epidermidis (40.3%) accounted for the great majority. S. lentus were only isolated from eight employees of a poultry slaughterhouse, whereas S. fleurettii was found in a veterinarian, two pig farmers, and three slaughterhouse employees. The remaining three MR-CNS strains isolated from two veterinarians and a slaughterhouse employee were identified as S. cohnii, S. warneri and S. sciuri.
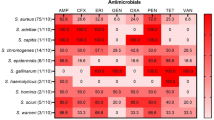
Antimicrobial susceptibility testing
The results of the phenotypic antibiotic resistance testing of the 414 MR-CNS strains are shown in Tables 3, 4 and 5. Although all characterized strains harbored the mecA gene, phenotypic resistance to beta-lactam antibiotics (ampicillin, cefoxitin, oxacillin, penicillin) varied between 63.5% (cefoxitin) and 97.8% (oxacillin). Resistance to ciprofloxacin, clindamycin, erythromycin, gentamicin, sulphamethoxazole/trimethoprim, and tetracycline varied between 14.7% and 49.0%. On the other hand, resistance to rifampin and vancomycin was only detected in 0.7% and 0.2% of strains, respectively. Table 5 shows the species-specific situation of MR-CNS strains to cefoxitin.
With regard to resistance rates of individual MR-CNS species (Table 3), more than 87% of the S. sciuri and S. haemolyticus strains showed phenotypical resistance to beta-lactam antibiotics. On the other hand, of the S. epidermidis, S. fleurettii, and S. lentus strains only 60% to 80% were resistant to beta-lactam antibiotics. Apart from one exception, more than 54% of strains from cows, calves, veterinarians and pig farmers were resistant to ciprofloxacin, clindamycin, erythromycin, and tetracycline (Table 4). In contrast, apart from two exceptions, less than 27% of strains isolated from BTM, minced meat, pigs and slaughterhouse employees, were resistant to the four antibiotics mentioned above. No strains from BTM, minced meat, and chicken were resistant to sulphamethoxazole/trimethoprim (SxT), whereas 40.0% of strains from pig farmers and 64.0% of strains from veterinarians showed resistance to SxT. None of the strains isolated from BTM and minced meat samples were resistant to rifampin or vancomycin.
Discussion
Methicillin-resistant staphylococci are a major concern to public and animal health. In veterinary medicine and along the meat and milk production line only very limited data were available on characteristics of MR-CNS. The present study provides an overview on the MR-CNS situation in Swiss livestock, chicken carcasses, BTM, minced meat, and persons in contact with farm animals. Since data of studies with comparable procedures are lacking, direct comparison of results is not possible. Therefore, we discussed our results in comparison to data that we considered most appropriate and as close to our own results as possible. In our study, MR-CNS were detected at an average of 48.3% in 2'099 samples. The occurrence varied thereby from 26.3% in slaughterhouse employees to 72.0% in calves. The MR-CNS occurrence rates mentioned above are in contrast to the low MRSA prevalence in Switzerland [20].
In the present study, 48.2% of all samples from livestock (pigs, cows, calves) and chicken carcasses tested positive for MR-CNS. MR-CNS were also found in cows and pigs by Zhang et al. [17]. In contrast, Bagcigil et al. [15] did not detect any MR-CNS in pigs and cattle. The species most frequently detected in animal samples of the present study were S. sciuri (63.4%), followed by S. fleurettii (17.8%), and S. lentus (15.7%). In calves, 98.0% of MR-CNS strains were identified as S. sciuri, whereas in cows only 72.0% belonged to this species. The strains from pigs were divided about half-and-half in S. sciuri and S. fleurettii. The high percentage of S. sciuri in pigs is especially relevant, since this CNS species is also reported to cause fatal exudative epidermitis in piglets [21], which is normally caused by exfoliative toxin producing S. hyicus. Interestingly, methicillin-resistant S. sciuri were also found to predominate in horses [22, 23]. Furthermore, the MR-CNS strains isolated from chicken in our study were mainly (78.9%) of S. lentus, whereas Kawano et al. [12] did not detect methicillin-resistant S. lentus in their samples. Methicillin-resistant S. lentus have also been described in other animal species such as horses [14, 22, 24], pigs, cattle, sheep, and goats [17]. Other data on species-specific identification of MR-CNS from livestock are limited.
In the BTM and minced meat samples of the present study, MR-CNS were detected in 32.4% of minced meat and in 62.0% of BTM samples. Respective data on MR-CNS from these sample categories are hardly found. The species predominantly found in BTM and minced meat samples of the present study, were S. fleurettii accounting for 76.2% of all analyzed strains, followed by S. sciuri comprising 15.5% of strains. In bovine quarter milk samples, Gillespie et al. [25] found mainly CNS of S. chromogenes, S. hyicus, S. epidermidis, and S. simulans. In a subsequent study, Sawant et al. [26] found 11 of 37 S. epidermidis strains to harbor the mecA gene and show phenotypic resistance to ampicillin and oxacillin. On the other hand, CNS are also frequently isolated from clinical and in particular subclinical intramammary infections in cattle [27] and small ruminants [28–30]. CNS found in this context generally showed a species distribution different from that present in our samples.
In the 460 nasal swabs from humans in contact with farm animals, MR-CNS were detected in 49.3% of samples. In view of contact persons, two studies found the prevalence of MR-CNS in horse personnel to be 37% and 63% [22, 23]. Moreover, a study among healthy humans without association to hospital or animals found an MR-CNS prevalence of 24% [6]. In human samples of the present study, the most frequently isolated species were S. haemolyticus (47.5%) and S. epidermidis (40.3%). MR-CNS of species S. haemolyticus [23] and S. epidermidis [22] were also frequently isolated from horse personnel. These two predominant species are also of importance for human infections. As discussed above, S. epidermidis and S. haemolyticus are frequently isolated CNS species involved in clinical cases of humans.
There are not much data available on the antimicrobial susceptibility of MR-CNS isolated from colonized livestock and humans, or from BTM and minced meat. In the present study, MR-CNS strains from BTM, minced meat, and chicken were only in limited numbers resistant to antibiotics other than beta-lactams. In view of MR-CNS as food contaminants and potential vectors of antibiotic resistance, these results suggest a favorable situation. In contrast, strains isolated from calves, cows, pig farmers, and veterinarians showed multi-resistance to a great extent. This situation may also be caused by frequent direct contact of these individuals with antibiotics. Interestingly, resistance rates of strains from pigs and slaughterhouse employees were in-between the groups mentioned above. Furthermore, it is noteworthy that in our MR-CNS strains, phenotypic resistance to oxacillin was by far a better indicator for the presence of the mecA gene than resistance to cefoxitin. Interestingly, for indication of mecA in MR-CNS using MIC, both cefoxitin and oxacillin are discussed as valuable approaches [31].
Conclusion
In conclusion, the results obtained indicate a high MR-CNS prevalence (on average 48.3%) in samples from livestock, chicken carcasses, BTM and minced meat, as well as persons in contact with livestock. The occurrence thereby ranged from 26.3% in slaughterhouse employees to 72.0% in calves. This is the first study detecting MR-CNS in a large collection of samples taken along the meat and milk production line. For species identification of MR-CNS isolated from different origins, MALDI TOF MS proved to be a fast and reliable tool and is therefore suitable for screening of large sample amounts. Furthermore, based on the present data, the occurrence of methicillin-resistant staphylococci should be continuously evaluated in surveillance programs within the scope of veterinary public health aspects. Otherwise, further studies are required to investigate the impact of the high MR-CNS prevalence on human and animal health.
Methods
Bacterial strains
From March through September 2009, we collected a total of 2'099 samples from livestock and chicken carcasses, BTM and minced meat, as well as humans in contact with farm animals. Livestock was sampled at slaughter. Thereby, swabs were collected from the nasal cavity of pigs (n = 716), calves (n = 300), cows (n = 340). From chicken carcasses herd-wise pooled neck skin samples (n = 72) were collected, each herd originating from a different farm. Sampled animals (including chicken) originated from more than 800 farms in 10 different cantons distributed throughout Switzerland. Furthermore, 100 BTM and 111 minced meat (pork and beef) samples were tested. Moreover, we analyzed nasal swabs from 148 pig farmers attending two meetings on swine breeding, 133 veterinarians participating in a course on castration of piglets, and 179 slaughterhouse employees working in two different abattoirs (a poultry and a pig and cattle slaughterhouse). All human nasal swabs samples were taken by the persons themselves. They gave us their consent that the samples can be used for this study.
For isolation of MR-CNS strains, a two-step enrichment procedure in Mueller-Hinton broth supplemented with 6.5% NaCl (24 h at 37°C) and in phenolred mannitol broth supplemented with 75 mg/L aztreonam and 5 mg/L cefoxitin (24 h at 37°C) was used. Samples were then plated onto Oxoid Brilliance™ MRSA Agar (Oxoid Ltd., Hampshire, UK) and incubated for 24 h at 37°C. Of presumptive MR-CNS colonies of beige or white color, one colony (and for some samples with different colony morphologies at most two colonies) was picked, gram-stained, and tested for catalase-activity. All gram-positive, catalase-positive cocci grown beige or white on Oxoid Brilliance™ MRSA Agar were considered MR-CNS. Thereafter, a random selection of 414 strains (34 to 52 isolates per sample origin) was confirmed as genetically methicillin-resistant by detection of the mecA gene [32] and then further characterized.
Species identification
MR-CNS species identification was performed by matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS). MALDI-TOF MS was recently described as an effective and powerful tool for reliable identification of staphylococci [33] and CNS in particular [34]. Briefly, of the 414 randomly selected strains, one or two colonies of a fresh overnight culture grown on TSA were suspended in 20 μL formic acid (25%). Thereafter, 20 μL of a saturated solution of sinapinic acid (49508, Sigma-Aldrich, Buchs, Switzerland) in 60% acetonitril (154601, Sigma-Aldrich, Buchs, Switzerland), 0.3% trifluoracetic acid (T6508, Sigma-Aldrich, Buchs, Switzerland) was added. Of this mixture 1 μl was spotted in duplicates on a steel target plate and air dried at room temperature. Spectra were acquired using a Axima™ confidence (Shimadzu-Biotech Corp., Kyoto, Japan) MALDI-TOF massspectrometer, in the linear positive mode, at a laser frequency of 50 Hz and within a mass range from 2000-30000 Da. Acceleration voltage was 20 kV, and the extraction delay time was 200 ns. A minimum of 10 lasershots per sample was used to generate each ion spectrum. For each bacterial sample, a total of 100 ion spectra were averaged and processed using the Launchpad™ v.2.8 Software (Shimadzu-Biotech Corp., Kyoto, Japan). Peaks lists were in ASCII format imported into the SARAMIS™ (Spectral Archive And Microbial Identification System, AnagnosTec, Potsdam-Golm, Germany) for automated species identification.
For additional confirmation of species identification, 56 randomly chosen strains were identified by sequencing an internal fragment of the sodA gene following a protocol of Poyart et al. [35] with slight modifications. DNA sequence-based species identification is currently the most accurate identification method available for CNS [36]. The partial sodA gene was amplified by PCR using primers d1 (5'-CCITAYICITAYGAYGCIYTIGARCC-3') and d2 (5'-ARRTARTAIGCRTGYTCCCAIACRTC-3'). PCRs were performed in a T3000 thermocycler (Biometra, Goettingen, Germany) in a final volume of 50 μL containing a minimum of 150 ng of DNA, 2 μM of each primer, 200 μM of each deoxynucleoside triphosphate, and 2 U of FastStart High Fidelity polymerase (Roche, Basel, Switzerland) in a 10× reaction buffer (with 18 mM MgCl2, included in kit). PCR mixtures were denatured (3 min, 95°C) and then subjected to 30 cycles of amplification (60 s of annealing at 39°C, 45 s of elongation at 72°C, and 30 s of denaturation at 95°C). The product was then sequenced and the results were compared to the GenBank database using the BLAST program (http://blast.ncbi.nlm.nih.gov/Blast.cgi).
Antimicrobial susceptibility testing
To evaluate the phenotypic antibiotic resistance of the selected 414 strains, the disk diffusion method was used in accordance with the guidelines of the Clinical and Laboratory Standards Institute [37] using the following disks (BD BBL Sensi-Disc; Becton, Dickinson and Company, Sparks, MD, USA): ampicillin (10 μg), cefoxitin (30 μg), ciprofloxacin (5 μg), clindamycin (2 μg), erythromycin (15 μg), gentamicin (10 μg), oxacillin (1 μg), penicillin (10 units), rifampin (5 μg), sulphamethoxazole/trimethoprim (23.75/1.25 μg), tetracycline (30 μg), and vancomycin (30 μg). Results were interpreted according to the CLSI guidelines, whereby intermediate results were considered resistant.
References
Barbier F, Ruppe E, Hernandez D, Lebeaux D, Francois P, Felix B, Desprez A, Maiga A, Woerther PL, Gaillard K, et al: Methicillin-resistant coagulase-negative staphylococci in the community: high homology of SCCmec IVa between Staphylococcus epidermidis and major clones of methicillin-resistant Staphylococcus aureus. J Infect Dis. 2010, 202: 270-281. 10.1086/653483.
Archer GL, Niemeyer DM, Thanassi JA, Pucci MJ: Dissemination among staphylococci of DNA sequences associated with methicillin resistance. Antimicrob Agents Chemother. 1994, 38: 447-454.
Kloos WE, Ballard DN, Webster JA, Hubner RJ, Tomasz A, Couto I, Sloan GL, Dehart HP, Fiedler F, Schubert K, et al: Ribotype delineation and description of Staphylococcus sciuri subspecies and their potential as reservoirs of methicillin resistance and staphylolytic enzyme genes. Int J Syst Bacteriol. 1997, 47: 313-323. 10.1099/00207713-47-2-313.
Tsubakishita S, Kuwahara-Arai K, Sasaki T, Hiramatsu K: Origin and molecular evolution of the determinant of methicillin resistance in staphylococci. Antimicrob Agents Chemother. 2010, 54: 4352-4359. 10.1128/AAC.00356-10.
Dakic I, Morrison D, Vukovic D, Savic B, Shittu A, Jezek P, Hauschild T, Stepanovic S: Isolation and molecular characterization of Staphylococcus sciuri in the hospital environment. J Clin Microbiol. 2005, 43: 2782-2785. 10.1128/JCM.43.6.2782-2785.2005.
Silva FR, Mattos EM, Coimbra MV, Ferreira-Carvalho BT, Figueiredo AM: Isolation and molecular characterization of methicillin-resistant coagulase-negative staphylococci from nasal flora of healthy humans at three community institutions in Rio de Janeiro City. Epidemiol Infect. 2001, 127: 57-62. 10.1017/S095026880100574X.
de Mattos EM, Teixeira LA, Alves VM, Rezendae Resende CA, da Silva Coimbra MV, da Silva-Carvalho MC, Ferreira-Carvalho BT, Figueiredo AM: Isolation of methicillin-resistant coagulase-negative staphylococci from patients undergoing continuous ambulatory peritoneal dialysis (CAPD) and comparison of different molecular techniques for discriminating isolates of Staphylococcus epidermidis. Diagn Microbiol Infect Dis. 2003, 45: 13-22. 10.1016/S0732-8893(02)00477-7.
Ruppe E, Barbier F, Mesli Y, Maiga A, Cojocaru R, Benkhalfat M, Benchouk S, Hassaine H, Maiga I, Diallo A, et al: Diversity of staphylococcal cassette chromosome mec structures in methicillin-resistant Staphylococcus epidermidis and Staphylococcus haemolyticus strains among outpatients from four countries. Antimicrob Agents Chemother. 2009, 53: 442-449. 10.1128/AAC.00724-08.
Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN, Beach M: Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997-1999. Clin Infect Dis. 2001, 32 (Suppl 2): S114-132. 10.1086/320184.
Kloos WE, Bannerman TL: Update on clinical significance of coagulase-negative staphylococci. Clin Microbiol Rev. 1994, 7: 117-140.
Miragaia M, Couto I, Pereira SF, Kristinsson KG, Westh H, Jarlov JO, Carrico J, Almeida J, Santos-Sanches I, de Lencastre H: Molecular characterization of methicillin-resistant Staphylococcus epidermidis clones: evidence of geographic dissemination. J Clin Microbiol. 2002, 40: 430-438. 10.1128/JCM.40.2.430-438.2002.
Kawano J, Shimizu A, Saitoh Y, Yagi M, Saito T, Okamoto R: Isolation of methicillin-resistant coagulase-negative staphylococci from chickens. J Clin Microbiol. 1996, 34: 2072-2077.
Yasuda R, Kawano J, Matsuo E, Masuda T, Shimizu A, Anzai T, Hashikura S: Distribution of mecA-harboring staphylococci in healthy mares. J Vet Med Sci. 2002, 64: 821-827. 10.1292/jvms.64.821.
De Martino L, Lucido M, Mallardo K, Facello B, Mallardo M, Iovane G, Pagnini U, Tufano MA, Catalanotti P: Methicillin-resistant staphylococci isolated from healthy horses and horse personnel in Italy. J Vet Diagn Invest. 2010, 22: 77-82.
Bagcigil FA, Moodley A, Baptiste KE, Jensen VF, Guardabassi L: Occurrence, species distribution, antimicrobial resistance and clonality of methicillin- and erythromycin-resistant staphylococci in the nasal cavity of domestic animals. Vet Microbiol. 2007, 121: 307-315. 10.1016/j.vetmic.2006.12.007.
Jaglic Z, Michu E, Holasova M, Vlkova H, Babak V, Kolar M, Bardon J, Schlegelova J: Epidemiology and characterization of Staphylococcus epidermidis isolates from humans, raw bovine milk and a dairy plant. Epidemiol Infect. 2010, 138: 772-782. 10.1017/S0950268809991002.
Zhang Y, Agidi S, LeJeune JT: Diversity of staphylococcal cassette chromosome in coagulase-negative staphylococci from animal sources. J Appl Microbiol. 2009, 107: 1375-1383. 10.1111/j.1365-2672.2009.04322.x.
van Duijkeren E, Box AT, Heck ME, Wannet WJ, Fluit AC: Methicillin-resistant staphylococci isolated from animals. Vet Microbiol. 2004, 103: 91-97. 10.1016/j.vetmic.2004.07.014.
Fessler AT, Billerbeck C, Kadlec K, Schwarz S: Identification and characterization of methicillin-resistant coagulase-negative staphylococci from bovine mastitis. J Antimicrob Chemother. 2010, 65: 1576-1582. 10.1093/jac/dkq172.
Huber H, Koller S, Giezendanner N, Stephan R, Zweifel C: Prevalence and characteristics of meticillin-resistant Staphylococcus aureus in humans in contact with farm animals, in livestock, and in food of animal origin, Switzerland, 2009. Euro Surveill. 2010, 15:
Chen S, Wang Y, Chen F, Yang H, Gan M, Zheng SJ: A highly pathogenic strain of Staphylococcus sciuri caused fatal exudative epidermitis in piglets. PLoS One. 2007, 2: e147-10.1371/journal.pone.0000147.
Busscher JF, van Duijkeren E, Sloet van Oldruitenborgh-Oosterbaan MM: The prevalence of methicillin-resistant staphylococci in healthy horses in the Netherlands. Vet Microbiol. 2006, 113: 131-136. 10.1016/j.vetmic.2005.10.028.
Moodley A, Guardabassi L: Clonal spread of methicillin-resistant coagulase-negative staphylococci among horses, personnel and environmental sites at equine facilities. Vet Microbiol. 2009, 137: 397-401. 10.1016/j.vetmic.2009.01.034.
Corrente M, D'Abramo M, Latronico F, Greco MF, Bellacicco AL, Greco G, Martella V, Buonavoglia D: Methicillin-resistant coagulase negative staphylococci isolated from horses. New Microbiol. 2009, 32: 311-314.
Gillespie BE, Headrick SI, Boonyayatra S, Oliver SP: Prevalence and persistence of coagulase-negative Staphylococcus species in three dairy research herds. Vet Microbiol. 2009, 134: 65-72. 10.1016/j.vetmic.2008.09.007.
Sawant AA, Gillespie BE, Oliver SP: Antimicrobial susceptibility of coagulase-negative Staphylococcus species isolated from bovine milk. Vet Microbiol. 2009, 134: 73-81. 10.1016/j.vetmic.2008.09.006.
Rajala-Schultz PJ, Smith KL, Hogan JS, Love BC: Antimicrobial susceptibility of mastitis pathogens from first lactation and older cows. Vet Microbiol. 2004, 102: 33-42. 10.1016/j.vetmic.2004.04.010.
Kunz F, Corti S, Giezendanner N, Stephan R, Wittenbrink MM, Zweifel C: Antibiotikaresistenz von Staphylococcus aureus und Koagulase-negativen Staphylokokken isoliert aus Mastitismilchproben von Schafen und Ziegen. Schweiz Arch Tierheilk. 2010, 153: 63-69.
Virdis S, Scarano C, Cossu F, Spanu V, Spanu C, De Santis EP: Antibiotic Resistance in Staphylococcus aureus and Coagulase Negative Staphylococci Isolated from Goats with Subclinical Mastitis. Vet Med Int. 2010, 2010: 517060-
Contreras A, Luengo C, Sanchez A, Corrales JC: The role of intramammary pathogens in dairy goats. Livestock Production Science. 2003, 79: 273-283. 10.1016/S0301-6226(02)00172-0.
Swenson JM, Brasso WB, Ferraro MJ, Hardy DJ, Knapp CC, Lonsway D, McAllister S, Reller LB, Sader HS, Shortridge D, et al: Correlation of cefoxitin MICs with the presence of mecA in Staphylococcus spp. J Clin Microbiol. 2009, 47: 1902-1905. 10.1128/JCM.02304-08.
Mehrotra M, Wang G, Johnson WM: Multiplex PCR for detection of genes for Staphylococcus aureus enterotoxins, exfoliative toxins, toxic shock syndrome toxin 1, and methicillin resistance. J Clin Microbiol. 2000, 38: 1032-1035.
Carbonnelle E, Beretti JL, Cottyn S, Quesne G, Berche P, Nassif X, Ferroni A: Rapid identification of Staphylococci isolated in clinical microbiology laboratories by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2007, 45: 2156-2161. 10.1128/JCM.02405-06.
Dubois D, Leyssene D, Chacornac JP, Kostrzewa M, Schmit PO, Talon R, Bonnet R, Delmas J: Identification of a variety of Staphylococcus species by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2010, 48: 941-945. 10.1128/JCM.00413-09.
Poyart C, Quesne G, Boumaila C, Trieu-Cuot P: Rapid and accurate species-level identification of coagulase-negative staphylococci by using the sodA gene as a target. J Clin Microbiol. 2001, 39: 4296-4301. 10.1128/JCM.39.12.4296-4301.2001.
Zadoks RN, Watts JL: Species identification of coagulase-negative staphylococci: genotyping is superior to phenotyping. Vet Microbiol. 2009, 134: 20-28. 10.1016/j.vetmic.2008.09.012.
CLSI: Performance standards for antimicrobial susceptibility testing; 18th informational supplement. CLSI document M100-S18. Clinical and Laboratory Standards Institute, Wayne, PA, USA. 2008.
Acknowledgements
We thank the staff of the slaughterhouses involved in this study for facilitating access to their operation and for assistance with the collection of data, Selina Koller for her great effort in taking samples in the slaughterhouses, and Xaver Sidler for his help in making sampling of veterinarians and pig farmers possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
HH was responsible for isolation and characterization of strains and drafted the manuscript. DZ, VP, and GV performed MALDI-TOF MS analysis and evaluated respective data. CZ and RS designed the study and edited the manuscript. All authors read, commented on, and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Huber, H., Ziegler, D., Pflüger, V. et al. Prevalence and characteristics of methicillin-resistant coagulase-negative staphylococci from livestock, chicken carcasses, bulk tank milk, minced meat, and contact persons. BMC Vet Res 7, 6 (2011). https://doi.org/10.1186/1746-6148-7-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1746-6148-7-6