Abstract
Background
Mucopolysaccharidosis type I (MPS I) is an autosomal storage disease resulting from defective activity of the enzyme α-L-iduronidase (IDUA). This glycosidase is involved in the degradation of heparan sulfate and dermatan sulfate. MPS I has severe and milder phenotypic subtypes.
Aim of study: This study was carried out on six newly collected MPS I patients recruited from many regions of Tunisia.
Patients and methods: Mutational analysis of the IDUA gene in unrelated MPS I families was performed by sequencing the exons and intron-exon junctions of IDUA gene.
Results
Two novel IDUA mutations, p.L530fs (1587_1588 insGC) in exon 11 and p.F177S in exon 5 and two previously reported mutations p.P533R and p.Y581X were detected. The patient in family 1 who has the Hurler phenotype was homozygous for the previously described nonsense mutation p.Y581X.
The patient in family 2 who also has the Hurler phenotype was homozygous for the novel missense mutation p.F177S. The three patients in families 3, 5 and 6 were homozygous for the p.P533R mutation. The patient in family 4 was homozygous for the novel small insertion 1587_1588 insGC. In addition, eighteen known and one unknown IDUA polymorphisms were identified.
Conclusion
The identification of these mutations should facilitate prenatal diagnosis and counseling for MPS I in Tunisia.
Background
Mucopolysaccharidosis type I (MPS I) is an autosomal recessive lysosomal storage disorder caused by the deficient activity of the enzyme of α-L-iduronidase (IDUA, EC 3.2.1.76). This glycosidase is involved in the degradation of heparan sulfate and dermatan sulfate. The clinical phenotype of MPS I ranges from the very severe in Hurler syndrome (MPS IH) to the relatively benign in Scheie syndrome (MPS IS), with an intermediate phenotype designated Hurler/Scheie (MPS IH/S) [1]. Isolation of complementary and genomic DNAs encoding human α -L- iduronidase [2, 3] have enable the identification of mutations underlying the enzyme defect and resulting in MPS I clinical phenotype. More than 100 mutations have been reported in patients with the MPS I subtypes (Human Gene Mutation Database; http://www.hgmd.org). High prevalence of the common mutations p.W402X and p.Q70X has been described; both of them in the severe clinical forms [4, 5]. A high prevalence of common mutation p.P533R has also been described in MPS I patients with various phenotypes [5, 6]. In addition, rare mutations including single base substitution, deletion, insertion and splicing site mutation have been identified [7], indicating a high degree of allelic heterogeneity in IDUA gene.
Here, we described two novel IDUA mutations in MPS I Tunisian patients. These lesions were homoallelic in all the patients of the six families investigated as consanguineous marriages are still frequent in Tunisia [8].
Similar content being viewed by others
Patients and Methods
Patients
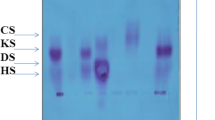
Six Tunisian unrelated families with MPS I were investigated. The MPS I patients were diagnosed in paediatric clinics of hospital of northern and southern Tunisia (Figure 1). The patients were all offspring of consanguineous marriages between first, second or third cousins. This study was approved by the Ethics committees of the Tunisian hospitals, and all families gave informed consent. Blood samples were collected from the six patients, their parents, and unaffected siblings and relatives. The clinical diagnoses were confirmed by enzymatic assays (Table 1).
IDUA activity
IDUA activity was determined in sonicated leukocyte pellets as described using the artificial substrate 4-methylumbellifery-α-L-iduronide [9].
IDUA mutation analysis
Genomic DNA was isolated from venous blood by the phenol/chloroform procedure. Each of the 14 exons and flanking intron-exon junctions of the IDUA gene were amplified from genomic DNAs from the patients and their parents as described previously [10].
Polymerase chain reaction (PCR) was carried out in a volume of 50 μl containing 100 ng genomic DNA, 0.2 mmol/L dNTPs, 0.4 μM of each primer, 1.5 mmol/L Mgcl2, 10% (v/v) DMSO, and 0.15 μl (0.75 units) of Taq Qbiogen (Promega).
Results
The affected probands in the six families had the typical Hurler phenotype. Two novel mutations, p.L530fs (1587_1588 inGC) in exon 11, and p.F177S in exon 5, and two previously reported mutations, p.P533R and p.Y581X, were detected in the affected patients and their respective parents from the six MPS I families (Table 2). The proband of family 1 with the Hurler phenotype was homozygous for the previously reported p.Y581X nonsense mutation (Figure 2a). The affected MPS IH patient in family 2 was homozygous for the novel p.F177S missense mutation. This mutation was due to a thymine -to- cytosine transversion in codon 177, resulting in the substitution of a polar phenylalanine to an uncharged polar serine residue (Figure 2b). The three affected siblings in families 3, 5 and 6 were homozygous for the previously reported p.P533R missense mutation (Figure 2c). The proband of family 4 was homozygous for a novel small insertion mutation 1587_1588 inGC (Figure 2d). This novel framshift (Leu530fs) in exon 11 changed codon 530 for leucine (CTG) to a premature termination codon (TGA), 30 amino acids downstream from the termination codon of the enzyme glycopeptide. In addition to these mutations, eighteen previously identified and one novel polymorphisms were identified in the Tunisian MPS I alleles (Table 2) [2, 7, 11, 12].
Direct sequencing of IDUA gene in Tunisian MPS I patients. 2a: Patient 1 (family 1): p.Y581X point mutation. 2b: Patient 2 (family 2): p.F177S point mutation. 2c: Patients 3, 5 and 6 (families 3, 5 and 6): p.P533R point mutation. 2d: Patient 4 (family 4): p.L530fs frame shift mutation. (w): mutant sequence, (w+): wild -type sequence.
The previously reported polymorphisms were detected in families 4 and 6, including: p.A8A (c.24 A > C), p.A20A (c.60G > A); p.H33Q (c.99 T > G), p.Q433Q (c.99T > G), IVS2-44 (c.300-44C > T); p.R105Q (c.314G > A); p.N181N (c.543 T > C), IVS5-45 (c.590-45G > C); IVS5-8 (c.590-8C > T); p.A314A (c.942G > C); IVS7+48 (c.972+48A > G), IVS7-45 (c.973-45 G > C; p.A361 (c.1081G > A; p.T388T (c.116 G > C); p.V454I (c.1360G > A); IVS9+36 (c.1402+36T > C), p.R489R (c.1467C > T), IVS12+72 (c.1727T > G), and one previously unreported polymorphism, 3'UTR+44 (c.1962+44G > C).
Discussion
MPS I is the most common mucopolysaccharidosis worldwide, with an average incidence of about 1.7 in 100.000 live births for the severe and mild forms [13]. The incidence of MPS I in Tunisia is also high, estimated at 0.63 in 100.000 live births [14], owing to the high rate of consanguinity [15].
To date, over 100 mutations in the IDUA gene have been described in patients with the MPS I subtypes (Human Gen Database, http://www.hgmd.org).
The molecular analysis of the six newly collected patients in Tunisian families allowed the identification of four mutations including a small insertion (1587_1588 inGC), a novel missense mutation (p.F177S) and two previously reported mutations, p.P533R and p.Y581X (Table 2). Of note, the common Caucasian IDUA mutations, p.Q70X and p.W402X, were not present [7].
Patient 1 from family 1 was homozygous for the previously reported p.Y581X mutation in exon 13 of the IDUA gene. The p.Y518X mutation was first described in one patient of Croatian origin. This patient was heteroallelic for the p.Y581X mutation and the Ile583delC mutation [16].
A patient 2 from family 2 was homozygous for the novel p.F177S mutation. This mutation causes a sever instability or loss of IDUA protein function, since the 177 residue was predicted to form the strands of the β barrel with the catalytic residues perched on the C terminal ends of the β strands [17]. The predicted IDUA active site showed different residues, among which the residue Glu178 which is near the Phe177. This mutation presumably resulted from slipped mispairing and repairing during replication. Our study identified the p.177S mutation in patient which had the severe phenotype and undetectable IDUA activity. This concept is consistent with the fact that the phenylalanine at IDUA residue 177 is highly conserved in evolution.
A patient four from family four was homozygous for the novel 1587_1588 inGC mutation that leads to the lack of 30 aminoacid at the amino terminus of the IDUA protein (p.Leu530fs).
The insertion (GC) occurred between two direct repeats (GC) that were separated by only three bases (CCC). The patient 4 did not have detectable IDUA activity and presented with the severe Hurler phenotype.
Patients 3, 5 and 6 from families 3, 5 and 6 respectively were homozygous for the p.P533R mutation. These patients had undectable IDUA activity and the typical Hurler phenotype. The p.P533R missense mutation in exon 11 resulted in a non conservative substitution of a neutral proline for a basic arginine.
The IDUA model begins at residue 36 of the linear sequence and terminates at residue 522, as this is the longest section that can be reliably predicted on the basis of the crystal structure of of the β-D-xylosidase from Thermoanaerobacterium saccharolyticum (XyTS, EC 3.2.1.37) [18]. As a result, residues 523-653 do not appear in the IDUA model, consistent with the finding that a proline residue in codon 533 is incapable of forming the main chain hydrogen bonds. A non conservative substitution of a neutral proline for a basic arginie could be predicted to drastically change the orientation of the secondary structure in IDUA protein leading to a severe disease phenotype.
The basis of such regional distribution of p.P533R mutation is not clear. This mutation has been identified in 92% of mutant alleles in 13 MPS I patients from Marroco [6], in 11% of mutant alleles of 27 MPS I patients from Sicily [19], in 62.5% of mutant alleles in 10 MPS I patients from Tunisia [20] and not identified in 3 MPS I patients from Egypt [21], suggesting that the p.P5323R allele possibly originated from a common founder from the Islamic occupation of Sicily [22].
A large number of polymorphisms and non pathogenic sequence variants have been described in the IDUA gene [7, 23, 24] (Table 2). The effect of these sequences variants on the IDUA activity has not been clearly defined especially when they are associated with specific mutations causing the Hurler/Scheie and Scheie phenotypes [7]. The effect of the noncoding [IVS2-44 (c.300-44C > T);IVS5-45 (c.590-45G > C); IVS5-8 (c.590-8C > T);IVS7+48 (c.972+48A > G), IVS7-45 (c.973-45 G > C; IVS9+36 (c.1402+36T > C), IVS12+72 (c.1727T > G),3'UTR+44 (c.1962+44G > C)] and coding [p.A8A (c.24 A > C), p.A20A (c.60G > A); p.H33Q (c.99 T > G), p.Q433Q (c.99T > G), p.R105Q (c.314G > A); p.N181N (c.543 T > C); p.A314A (c.942G > C); p.A361 (Tc.1081G > A; p.T388T (c.116 G > C); p.V454I (c.1360G > A); p.R489R (c.1467C > T)] polymorphisms/sequence variants on IDUA expression in the Hurler patients from the Tunisian families is unknown [25].
Our study showed a heterogeneous pattern of mutations and polymorphisms among MPS I Tunisian patients.
The results of recent studies support the evidence of mutational heterogeneity of the IDUA, IDS and GALNS genes in patients with MPS I [25], MPS II [26] and MPS IVA [27] respectively. These MPS patients have different clinical presentation ranging from severe to mild. Since most patients have unique mutations, a comprehensive genotype-phenotype correlation is not feasible. At any rate, even in presence of recurrent mutations, a correlation has proved inapplicable. For example, the missense p.P533R mutation was usually reported associated with a severe phenotype [5], whereas this lesion identified on the contrary in our patients was found associated with mild and severe forms of the disease. This type of observation implicates others modifying or non genetic factor in the clinical presentation of disease.
A more comprehensive analysis of MPS I patients is essential. This must comprise not only a molecular screening for other known mutations, but also a complete screening for new mutations. In addition, a comprehensive clinical and epidemiological investigation could help assign the ethnic background of these patients.
Conclusion
In summary, two novel mutations were identified in six MPS I patients from six Tunisian families. The severe missense mutation p.F177S was detected in one family and presumably resulted in misfolding and degradation of the mutant glycopepide. The other lesion was a severe small insertion 1587_1588 insGC that predicts premature termination of the IDUA protein. The identification of these mutations could provide genotype/phenotype correlations for the severe MPS I subtypes, accurate carrier detection, and prenatal diagnosis for MPS I families.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
- MPS I:
-
Mucopolysaccharidosis I
- IDUA:
-
Alpha L iduronidase
- PCR:
-
polymerase chain reaction
- MPS II:
-
Mucopolysaccharidosis II
- MPS IVA:
-
mucopolysaccharidosis IVA
- IDS:
-
Iduronate -2-sulfatase
- GALNS:
-
N-acetylgalactosamine-6-sulfate-sulfatase.
References
Neufeld EF, Muenzer J: The mucopolysaccharidoses. The Metabolic and Molecular Bases of Inherited Disease. Edited by: Scriver CR, Beaudet AL, Sly WS, Valle D. 2002, McGraw-Hill, New York, 2421-3452. 8
Scott HS, Anson DS, Orsborn AM, Nelson PV, Clements PR, Morris CP, Hopwood JJ: Human alpha-L-iduronidase: cDNA isolation and expression. Proc Natl Acad Sci USA. 1991, 88: 9695-9699. 10.1073/pnas.88.21.9695.
Scott HS, Guo XH, Hopwood JJ, Morris CP: Structure and sequence of the human alpha-L-iduronidase gene. Genomics. 1992, 13: 1311-1313. 10.1016/0888-7543(92)90053-U.
Scott HS, Litjens T, Hopwood JJ, Morris CP: A common mutation for mucopolysaccharidosis type I associated with a severe Hurler syndrome phenotype. Hum Mutat. 1992, 1: 103-108. 10.1002/humu.1380010204.
Scott HS, Litjens T, Nelson PV, Brooks DA, Hopwood JJ, Morris CP: alpha-L-iduronidase mutations (Q70X and P533R) associate with a severe Hurler phenotype. Hum Mutat. 1992, 1: 333-339. 10.1002/humu.1380010412.
Alif N, Hess K, Straczek J, Sebbar S, N'Bou A, Nabet P, Dousset B: Mucopolysaccharidosis type I: characterization of a common mutation that causes Hurler syndrome in Moroccan subjects. Ann Hum Genet. 1999, 63: 9-16. 10.1046/j.1469-1809.1999.6310009.x.
Scott HS, Bunge S, Gal A, Clarke LA, Morris CP, Hopwood JJ: Molecular genetics of mucopolysaccharidosis type I: diagnostic, clinical, and biological implications. Hum Mutat. 1995, 6: 288-302. 10.1002/humu.1380060403.
BenM'rad L: Le choix matrimonial en Tunisie est-il transmissible?. Antropo 7. 2004, 31-37.
Hopwood JJ, Muller V, Smithson A, Baggett N: A fluorometric assay using 4- methylumbelliferyl alpha-L-iduronide for the estimation of alpha-L-iduronidase activity and the detection of Hurler and Scheie syndromes. Clin Chim Acta. 1979, 92: 257-65. 10.1016/0009-8981(79)90121-9.
Beesley CE, Meaney CA, Greenland G, Adams V, Vellodi A, Young EP, Winchester BG: Mutational analysis of 85 mucopolysaccharidosis type I families: frequency of known mutations, identification of 17 novel mutations and in vitro expression of missense mutations. Hum Genet. 2001, 109: 503-11. 10.1007/s004390100606.
Bunge S, Kleijer WJ, Steglich C, Beck M, Zuther C, Morris CP, Schwinger E, Schinzel A, Hopwood JJ, Gal A: Mucopolysaccharidosis type I: identification of 8 novel mutations and determination of the frequency of the two common alpha-L-iduronidase mutations (W402X and Q70X) among European patients. Hum Mol Genet. 1994, 3: 861-866. 10.1093/hmg/3.6.861.
Scott HS, Nelson PV, Litjens T, Hopwood JJ, Morris CP: Multiple polymorphisms within the alpha-L-iduronidase gene (IDUA): implications for a role in modification of MPS-I disease phenotype. Hum Mol Genet. 1993, 2: 1471-1473. 10.1093/hmg/2.9.1471.
Nelson J: Incidence of the mucopolysaccharidoses in Northern Irland. Hum Genet. 1997, 101: 255-258. 10.1007/s004390050626.
Ben Turkia H, Tebib N, Azzouz H, Abdelmoula MS, Ben Chehida A, Chemli J, Monastiri K, Chaabouni M, Sanhagi H, Zouari B, Kaabachi N, Ben Dridi MF: Incidence of mucopolysaccharidoses in Tunisia. Tunis Med. 2009, 87: 782-785.
Laradi S, Monastiri K, Ferchichi S, Nabli N, Aouini Rea P, Ben Limam H, Ben Mansour R, Bousoffara R, Yacoub M, Froissart R, Miled A, Maire I: Clinico-biologic and molecular study of mucopolysaccharidosis in central and southern Tunisia. Ann Biol Clin. 2001, 100-4.
Petkovć (Tokć) Višnja, Barišć Ingeborg, Huzjak Nevenka, Petkovć Giorgie, Fumć Ksenija: First results of enzyme replacement therapy in two patients with mucopolysaccharidosis IH. Paediatria Croatica. 2005, 49: 181-187.
Rempel BP, Clarke LA, Withers SG: A homology model for human alpha-L-iduronidase: insights into human disease. Mol Genet Metab. 2005, 85: 28-37. 10.1016/j.ymgme.2004.12.006.
Yang JK, Yoon HJ, Ahn HJ, Lee BI, Pedelacq JD, Liong EC, Berendzen J, Laivenieks M, Vieille C, Zeikus GJ, Vocadlo DJ, Withers SG, Suh SW: Crystal structure of β-D-xylosidase from Thermoanaerobacterium saccharolyticum, a family 39 glycoside hydrolase. J Mol Biol. 2004, 335: 155-165. 10.1016/j.jmb.2003.10.026.
Gatti R, DiNatale P, Villani GR, Filocamo M, Muller V, Guo XH, Nelson PV, Scott HS, Hopwood JJ: Mutations among Italian mucopolysaccharidosis type I patients. J Inherit Metab Dis. 1997, 20: 803-806. 10.1023/A:1005323918923.
Chkioua L, Khedhiri S, Jaidane Z, Ferchichi S, Habib S, Froissart R, Bonnet V, Chaabouni M, Dandana A, Jrad T, Limem H, Maire I, Abdelhedi M, Laradi S: Mucopolysaccharidosis type I: identification of alpha-L-iduronidase mutations in Tunisian families. Arch Pediatr. 2007, 14: 1183-9. 10.1016/j.arcped.2007.06.018.
Amr K, Katoury A, Abdel-Hamid M, Bassiouni R, Ibrahim M, Faten E: Mutational Analysis of the alpha-L-iduronidase gene in three Egyptian families: identification of three novel mutations and five novel polymorphisms. Genet Test Mol Biomarkers. 2009, 13: 761-764. 10.1089/gtmb.2009.0057.
Laradi S, Tukel T, Erazo M, Shabbeer J, Chkioua L, Khedhiri S, Ferchichi S, Chaabouni M, Miled A, Desnick RJ: Mucopolysaccharidosis type I: identification of 13 novel mutations of the alpha-Liduronidase gene. J Inherit Metab Dis. 2005, 28: 1019-1026. 10.1007/s10545-005-0197-4.
Bunge S, Kleijer WJ, Steglich C, Beck M, Schwinger E, Gal A: Mucopolysaccharidosis type I: identification of 13 novel mutations of the alpha-Liduronidase gene. Hum Mutat. 1995, 6: 91-94. 10.1002/humu.1380060119.
Venturi N, Rovelli A, Parini R, Menni F, Brambillasca F, Bertagnolio F, Uziel G, Gatti R, Filocamo M, Donati MA, Biondi A, Goldwurm S: Molecular analysis of 30 mucopolysaccharidosis type I patients: evaluation of the mutational spectrum in Italian population and identification of 13 novel mutations. Hum Mutat. 2002, 20: 231-23.
Chkioua L, Khedhiri S, Kassab A, Bibi A, Ferchichi S, Froissart R, Vianey-Saban C, Laradi S, Miled A: Molecular analysis of mucopolysaccharidosis type I in Tunisia: identification of novel mutation and eight Novel polymorphisms. Diagn Pathol. 2011, 6: 39-10.1186/1746-1596-6-39.
Chkioua L, Khedhiri S, Ferchichi S, Tcheng R, Froissart R, Chehed H, Vianey-Saban C, Laradi S, Miled A: Molecular analysis of iduronate -2- sulfatase gene in Tunisian patients with mucopolysaccharidosis type II. Diagn Pathol.
Khedhiri S, Chkioua L, Ferchichi S, Miled A, Laradi S: Polymorphisms in Tunisian patients with N-acetylgalactosamine-6-sulfate sulfatase gene deficiency: Implication in Morquio A disease. Diagn Pathol. 2011, 6: 11-10.1186/1746-1596-6-11.
Acknowledgements
We grateful acknowledge the patients and their families for participation in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
LC wrote the manuscript LC, SK and RT performed all the work (PCR, sequencing...) in the laboratory. HC, HB and MF analysed of the results RF and ChVS participated in data analysis. SF, SL and AM revised the manuscript and save final approval of the version to be published.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chkioua, L., Khedhiri, S., Turkia, H.B. et al. Mucopolysaccharidosis type I: molecular characteristics of two novel alpha-L-iduronidase mutations in Tunisian patients. Diagn Pathol 6, 47 (2011). https://doi.org/10.1186/1746-1596-6-47
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1746-1596-6-47