Abstract
Murine models have highlighted the importance of T-cells and TH2 cytokines in development of allergen-induced airway disease. In contrast, the role of mast cells for the development of allergic airway disease has been controversial. Recent studies in murine models demonstrate a significant contribution of mast cells during the development of airway hyperresponsiveness and airway inflammation. Furthermore these models have allowed identifying certain mast cell-produced mediators (e.g. histamine and leukotriene B4) to be involved in the recruitment of effector T-cells into the lung. Additionally, mast cell-produced TNF can directly activate TH2 cells and contribute to the development of allergic airway disease. These new findings demonstrate a complex role of mast cells and their mediators, not only as effector cells, but also during sensitization and development of allergic airway disease. Therefore mast cells and certain mast cell-produced mediators might be an interesting target for the prevention and treatment of allergic asthma.
Similar content being viewed by others
Introduction
For decades mast cells have been known as important effector cells for adaptive immune responses. Functions of mast cells include both IgE-dependent mucosal immunity to parasites but also dysregulated allergic responses to environmental antigens. In patients with allergic asthma, allergen-specific activation of mast cells through IgE bound to the high-affinity IgE receptor (FcΕRI) induces early airway responses following allergen exposure. Also increased numbers of mast cells are found in close proximity to airway smooth muscle in patients with allergic asthma, suggesting their potential role in the development and maintenance of allergic airway disease [1].
Murine models have helped to gain insights into the pathogenesis of airway inflammation and airway responsiveness [2]. These models have highlighted the importance of T-cells and T-cell mediated cytokines for the development of the disease. Mast cell-deficient mice can be utilized to investigate the role of mast cells in these models. Most commonly two mast cell-deficient mouse strains, the WBBF1-KitW/KitW-v and more recently the C57BL/6-KitW-sh/KitW-sh are used [3]. Both strains are mast cells-deficient but also lack melanocytes. Additionally, the WBBF1-KitW/KitW-v mice are sterile, anaemic, and lack intestinal cells of Cajal, whereas the C57BL/6-KitW-sh/KitW-sh are not sterile or anaemic [3].
Mast cells contribute to the development of allergic airway disease
The role of mast cells for the development of allergic airway disease in murine models is critically dependent on the sensitization and allergen exposure protocol. In studies using systemic sensitization with adjuvant hyperresponsiveness (AHR) and airway inflammation are similar in mast cell- or IgE-deficient mice compared to wild-type mice [4–6]. However, in models with less potent sensitization protocols, a role of mast cells for the induction of non-allergic [7] but also allergen-induced airway disease [8–10] can be demonstrated. In these models the presence of mast cells in already sensitized animals is essential for the initiation of airway inflammation and AHR. Further studies, using mast cell reconstitution protocols, revealed that the expression of the Fc receptor γ chain in mast cells [10], necessary for the surface expression of the Fcγ receptors I and III and the FcεRI receptor is pivotal for the induction of most features of allergen-induced lung pathology. In studies using an inhalation allergen exposure, development of increased airway reactivity was associated with the expression of FcεRI on mast cells [11]. These results underscore that mast cells are involved in the development of an allergic airway disease in already sensitized hosts.
Mast cells not only play an important role during the effector phase of allergic airway disease but also could be involved during sensitization to an allergen. Intranasal exposure with allergen alone does not induce a specific T-cell response. In contrast, exposure with allergen in combination with a low dose of bacterial lipopolysaccharides (LPS) induces a specific T-cell response [12] and consecutive challenge with the allergen then leads to eosinophilic airway inflammation. Interestingly, mast cell-deficient mice exposed intranasally with allergen and low dose LPS do not develop eosinophilic airway inflammation following rechallenge. However, mast cell-deficient mice reconstituted with wild-type mast cells developed airway inflammation similar to wild-type animals, suggesting an involvement of mast cells during the sensitization process [13]. Indeed, mast cells express several Toll like receptors (TLR) including TLR-4 on their surface and release cytokines and chemokines following exposure to TLR-ligands [14] and mast cell-deficient mice reconstituted with TLR-4 deficient mast cells, did not develop airway eosinophilia following allergen exposure [13]. These findings suggest that IgE-independent mast cell activation through TLR-4 is necessary for sensitization to an allergen administered directly into the lung, further extending the function and role of mast cells in the development of allergic diseases.
Mast cell-produced mediators
Mast cells, following activation, degranulate and produce a plethora of lipid mediators, cytokines, and chemokines [3]. Several of these mediators might contribute through different mechanisms to the development of AHR. One potential mechanism could be the secretion of cytokines and especially IL-13 [15]. IL-13 is capable to directly induce AHR and blockade of IL-13 has been shown to be an effective treatment approach in acute [16, 17] and chronic [18] models of allergic airway disease. However, IL-13 deficient mast cells, when transferred into FcεRI-receptor deficient mice, where still able to induce increased airway reactivity. This finding suggests that IL-13 production from mast cells does not play a primary role in the development of allergic airway disease [11].
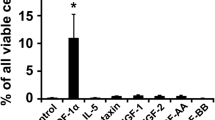
Other mechanisms could be the secretion of chemo-attractants and chemokines, which lead to the recruitment of other cell populations, such as effector T-cell into the lung and airways. Recently an interaction with mast cells has been described for allergen specific CD8-positive T-effector cells. These in vitro studies have shown that migration of CD8-positive T-effector cells can be initiated by mast cell activation. Furthermore T-cell migration was regulated by leukotriene B4 (LTB4) produced by mast cells and the expression of the receptor 1 (BLT-1) on the T-cells [19]. CD8-positive T-cells [20, 21] and especially allergen experienced CD8-positive T effector cells (Teff) are critical for the development of AHR and airway inflammation [22]. Following sensitization and challenge increased migration of these cells into the lung can be demonstrated [22] and this migration is dependent on LTB4 [23]. The contribution of mast cell produced LTB4 for Teff cell recruitment was assessed in a previously described model of passive sensitization [24]. Mice were passively sensitized with OVA-specific IgE. Mast cell-, FcεRI- and CD8-deficient mice showed only low airway reactivity following passive sensitization compared to passively sensitized wild-type mice. Increased airway reactivity could be reconstituted in CD8-deficient mice by adoptive transfer of allergen-specific Teff cells. Only transferred BLT-1 expressing Teff migrated effectively to the lung and reconstituted AHR whereas BLT-1 deficient Teff failed to do so [25]. A potential contribution of basophils in this response can not be excluded as basophils express the FcΕRI in the mouse [26].
Also other mast cell-produced mediators are of interest. Histamine receptor 1 has recently been shown to be important for the development of allergic airway disease and also for T-cell trafficking [27]. Another important mast cell-produced mediator is Tumor Necrosis Factor (TNF). In other disease models mast cell-derived TNF is important for the induction and promotion of initial inflammatory events [28–33]. Several studies have also demonstrated a contribution of TNF to the induction of allergic airway diseases [34–36]. Sensitized mast cell-deficient mice express lower levels of TNF in BAL fluid compared to sensitized and challenged wild-type mice and reconstitution with bone marrow-derived mast cells restored BAL fluid levels of TNF and AHR [37]. In a recent study Nakae et al. directly evaluated the role of mast cell-produced TNF for the induction of allergic airway disease using a mast cell reconstitution model. Similar to previous studies, mast cell-deficient animals fail to develop allergic airway disease whereas mice reconstituted with mast cells derived from wild-type mice developed allergic airway disease. In contrast, mice reconstituted with mast cells derived from TNF-deficient donors have less airway inflammation and AHR, demonstrating that mast cell-produced TNF is pivotal for the induction of allergic airway disease [38]. Furthermore the authors point out an enhanced proliferation of TH2 cells induced by mast cell-produced TNF, suggesting that mast cells induce activation of allergen specific T-cells in the sites of inflammation. These findings are of clinical interest as recent studies in patients with moderate [39] and also more severe asthma [40, 41] described beneficial effects of treatment with TNF neutralizing antibodies on lung function and airway reactivity.
Conclusion
Recent studies have outlined a critical role of mast cells for the development of acute allergic airway disease, especially in sensitization protocols without an adjuvant. Furthermore there is evidence that mast cells are also involved during the sensitization to inhaled allergens by IgE-independent activation through TLR. Still little is known about the role of the different mediators produced and secreted by mast cells. Several mast cell-produced mediators like LTB4, histamine and TNF have been identified to contribute to the development of allergic airway disease. Further research is needed as increasing knowledge about these pathways might allow a more targeted therapy of allergic asthma.
References
Brightling CE, Bradding P, Symon FA, Holgate ST, Wardlaw AJ, Pavord ID: Mast-cell infiltration of airway smooth muscle in asthma. N Engl J Med 2002, 346: 1699–705. 10.1056/NEJMoa012705
Taube C, Dakhama A, Gelfand EW: Insights into the pathogenesis of asthma utilizing murine models. Int Arch Allergy Immunol 2004, 135: 173–186. 10.1159/000080899
Galli SJ, Nakae S, Tsai M: Mast cells in the development of adaptive immune responses. Nat Immunol 2005, 6: 135–142. 10.1038/ni1158
Mehlhop PD, van de Rijn M, Goldberg AB, Brewer JP, Kurup VP, Martin TR, Oettgen HC: Allergen-induced bronchial hyperreactivity and eosinophilic inflammation occur in the absence of IgE in a mouse model of asthma. Proc Natl Acad Sci USA 1997, 94: 1344–9. 10.1073/pnas.94.4.1344
Nogami M, Suko M, Okudaira H, Miyamoto T, Shiga J, Ito M, Kasuya S: Experimental pulmonary eosinophilia in mice by Ascaris suum extract. Am Rev Respir Dis 1990, 141: 1289–95.
Takeda K, Hamelmann E, Joetham A, Shultz LD, Larsen GL, Irvin CG, Gelfand EW: Development of eosinophilic airway inflammation and airway hyperresponsiveness in mast cell-deficient mice. J Exp Med 1997, 186: 449–54. 10.1084/jem.186.3.449
Kraneveld AD, van der Kleij HP, Kool M, van Houwelingen AH, Weitenberg AC, Redegeld FA, Nijkamp FP: Key role for mast cells in nonatopic asthma. J Immunol 2002, 169: 2044–53.
Ogawa K, Kaminuma O, Kikkawa H, Kameda R, Ikezawa K, Suko M, Okudaira H, Akiyama K, Mori A: Primary role of CD4+ T cells and supplemental role of mast cells in allergic pulmonary eosinophilia. Int Arch Allergy Immunol 1999,120(Suppl 1):15–8. 10.1159/000053586
Williams CM, Galli SJ: Mast cells can amplify airway reactivity and features of chronic inflammation in an asthma model in mice. J Exp Med 2000, 192: 455–62. 10.1084/jem.192.3.455
Yu M, Tsai M, Tam SY, Jones C, Zehnder J, Galli SJ: Mast cells can promote the development of multiple features of chronic asthma in mice. J Clin Invest 2006, 116: 1633–1641. 10.1172/JCI25702
Taube C, Wei X, Swasey CH, Joetham A, Zarini S, Lively T, Takeda K, Loader J, Miyahara N, Kodama T, et al.: Mast cells FcepsilonRI, and IL-13 are required for development of airway hyperresponsiveness after aerosolized allergen exposure in the absence of adjuvant. J Immunol 2004, 172: 6398–406.
Eisenbarth SC, Piggott DA, Huleatt JW, Visintin I, Herrick CA, Bottomly K: Lipopolysaccharide-enhanced, toll-like receptor 4-dependent T helper cell type 2 responses to inhaled antigen. J Exp Med 2002, 196: 1645–1651. 10.1084/jem.20021340
Nigo YI, Yamashita M, Hirahara K, Shinnakasu R, Inami M, Kimura M, Hasegawa A, Kohno Y, Nakayama T: Regulation of allergic airway inflammation through Toll-like receptor 4-mediated modification of mast cell function. Proc Natl Acad Sci USA 2006, 103: 2286–2291. 10.1073/pnas.0510685103
Stassen M, Hultner L, Schmitt E: Classical and alternative pathways of mast cell activation. Crit Rev Immunol 2002, 22: 115–140.
Burd PR, Thompson WC, Max EE, Mills FC: Activated mast cells produce interleukin 13. J Exp Med 1995, 181: 1373–80. 10.1084/jem.181.4.1373
Grunig G, Warnock M, Wakil AE, Venkayya R, Brombacher F, Rennick DM, Sheppard D, Mohrs M, Donaldson DD, Locksley RM, et al.: Requirement for IL-13 independently of IL-4 in experimental asthma. Science 1998, 282: 2261–3. 10.1126/science.282.5397.2261
Wills-Karp M, Luyimbazi J, Xu X, Schofield B, Neben TY, Karp CL, Donaldson DD: Interleukin-13: central mediator of allergic asthma. Science 1998, 282: 2258–61. 10.1126/science.282.5397.2258
Taube C, Duez C, Cui ZH, Takeda K, Rha YH, Park JW, Balhorn A, Donaldson DD, Dakhama A, Gelfand EW: The role of IL-13 in established allergic airway disease. J Immunol 2002, 169: 6482–9.
Ott VL, Cambier JC, Kappler J, Marrack P, Swanson BJ: Mast cell-dependent migration of effector CD8+ T cells through production of leukotriene B4. Nat Immunol 2003, 4: 974–81. 10.1038/ni971
Hamelmann E, Oshiba A, Paluh J, Bradley K, Loader J, Potter TA, Larsen GL, Gelfand EW: Requirement for CD8+ T cells in the development of airway hyperresponsiveness in a murine model of airway sensitization. J Exp Med 1996, 183: 1719–29. 10.1084/jem.183.4.1719
Miyahara N, Takeda K, Kodama T, Joetham A, Taube C, Park JW, Miyahara S, Balhorn A, Dakhama A, Gelfand EW: Contribution of antigen-primed CD8+ T cells to the development of airway hyperresponsiveness and inflammation is associated with IL-13. J Immunol 2004, 172: 2549–2558.
Miyahara N, Swanson BJ, Takeda K, Taube C, Miyahara S, Kodama T, Dakhama A, Ott VL, Gelfand EW: Effector CD8+ T cells mediate inflammation and airway hyper-responsiveness. Nat Med 2004, 10: 865–869. 10.1038/nm1081
Miyahara N, Takeda K, Miyahara S, Taube C, Joetham A, Koya T, Matsubara S, Dakhama A, Tager AM, Luster AD, et al.: Leukotriene B4 receptor-1 is essential for allergen-mediated recruitment of CD8+ T cells and airway hyperresponsiveness. J Immunol 2005, 174: 4979–4984.
Oshiba A, Hamelmann E, Takeda K, Bradley KL, Loader JE, Larsen GL, Gelfand EW: Passive transfer of immediate hypersensitivity and airway hyperresponsiveness by allergen-specific immunoglobulin (Ig) E and IgG1 in mice. J Clin Invest 1996, 97: 1398–408.
Taube C, Miyahara N, Ott V, Swanson B, Takeda K, Loader J, Shultz LD, Tager AM, Luster AD, Dakhama A, et al.: The leukotriene B4 receptor (BLT1) is required for effector CD8+ T cell-mediated, mast cell-dependent airway hyperresponsiveness. J Immunol 2006, 176: 3157–3164.
Kinet JP: The high-affinity IgE receptor (Fc epsilon RI): from physiology to pathology. Annu Rev Immunol 1999, 17: 931–72. 10.1146/annurev.immunol.17.1.931
Bryce PJ, Mathias CB, Harrison KL, Watanabe T, Geha RS, Oettgen HC: The H1 histamine receptor regulates allergic lung responses. J Clin Invest 2006, 116: 1624–1632. 10.1172/JCI26150
Echtenacher B, Mannel DN, Hultner L: Critical protective role of mast cells in a model of acute septic peritonitis. Nature 1996, 381: 75–77. 10.1038/381075a0
von Stebut E, Metz M, Milon G, Knop J, Maurer M: Early macrophage influx to sites of cutaneous granuloma formation is dependent on MIP-1alpha /beta released from neutrophils recruited by mast cell-derived TNFalpha. Blood 2003, 101: 210–215. 10.1182/blood-2002-03-0921
Rijnierse A, Koster AS, Nijkamp FP, Kraneveld AD: TNF-alpha is crucial for the development of mast cell-dependent colitis in mice. Am J Physiol Gastrointest Liver Physiol 2006, 291: G969-G976. 10.1152/ajpgi.00146.2006
Biedermann T, Kneilling M, Mailhammer R, Maier K, Sander CA, Kollias G, Kunkel SL, Hultner L, Rocken M: Mast cells control neutrophil recruitment during T cell-mediated delayed-type hypersensitivity reactions through tumor necrosis factor and macrophage inflammatory protein 2. J Exp Med 2000, 192: 1441–1452. 10.1084/jem.192.10.1441
van Houwelingen AH, Kool M, de Jager SC, Redegeld FA, van Heuven-Nolsen D, Kraneveld AD, Nijkamp FP: Mast cell-derived TNF-alpha primes sensory nerve endings in a pulmonary hypersensitivity reaction. J Immunol 2002, 168: 5297–302.
Heib V, Becker M, Warger T, Rechtsteiner G, Tertilt C, Klein M, Bopp T, Taube C, Schild H, Schmitt E, et al.: Mast cells are crucial for early inflammation migration of Langerhans cells and CTL responses following topical application of TLR7 ligand in mice. Blood 2007, 110: 946–953. 10.1182/blood-2006-07-036889
Busse PJ, Zhang TF, Srivastava K, Lin BP, Schofield B, Sealfon SC, Li XM: Chronic exposure to TNF-alpha increases airway mucus gene expression in vivo. J Allergy Clin Immunol 2005, 116: 1256–1263. 10.1016/j.jaci.2005.08.059
Choi IW, Sun K, Kim YS, Ko HM, Im SY, Kim JH, You HJ, Lee YC, Lee JH, Park YM, et al.: TNF-alpha induces the late-phase airway hyperresponsiveness and airway inflammation through cytosolic phospholipase A(2) activation. J Allergy Clin Immunol 2005, 116: 537–543. 10.1016/j.jaci.2005.05.034
Kim J, McKinley L, Natarajan S, Bolgos GL, Siddiqui J, Copeland S, Remick DG: Anti-tumor necrosis factor-alpha antibody treatment reduces pulmonary inflammation and methacholine hyper-responsiveness in a murine asthma model induced by house dust. Clin Exp Allergy 2006, 36: 122–132. 10.1111/j.1365-2222.2005.02407.x
Kim YS, Ko HM, Kang NI, Song CH, Zhang X, Chung WC, Kim JH, Choi IH, Park YM, Kim GY, et al.: Mast cells play a key role in the development of late airway hyperresponsiveness through TNF-alpha in a murine model of asthma. Eur J Immunol 2007, 37: 1107–1115. 10.1002/eji.200636612
Nakae S, Ho LH, Yu M, Monteforte R, Iikura M, Suto H, Galli SJ: Mast cell-derived TNF contributes to airway hyperreactivity inflammation, and T(H)2 cytokine production in an asthma model in mice. J Allergy Clin Immunol 2007, 120: 48–55. 10.1016/j.jaci.2007.02.046
Erin EM, Leaker BR, Nicholson GC, Tan AJ, Green LM, Neighbour H, Zacharasiewicz AS, Turner J, Barnathan ES, Kon OM, et al.: The effects of a monoclonal antibody directed against tumor necrosis factor-alpha in asthma. Am J Respir Crit Care Med 2006, 174: 753–762. 10.1164/rccm.200601-072OC
Berry MA, Hargadon B, Shelley M, Parker D, Shaw DE, Green RH, Bradding P, Brightling CE, Wardlaw AJ, Pavord ID: Evidence of a role of tumor necrosis factor alpha in refractory asthma. N Engl J Med 2006, 354: 697–708. 10.1056/NEJMoa050580
Howarth PH, Babu KS, Arshad HS, Lau L, Buckley M, McConnell W, Beckett P, Al AM, Chauhan A, Wilson SJ, et al.: Tumour necrosis factor (TNFalpha) as a novel therapeutic target in symptomatic corticosteroid dependent asthma. Thorax 2005, 60: 1012–1018. 10.1136/thx.2005.045260
Acknowledgements
Supported by Deutsche Forschungsgemeinschaft (SFB 548/A11)
This article has been published as part of Journal of Occupational Medicine and Toxicology Volume 3 Supplement 1, 2008: Proceedings of the 6th Workshop on Animal Models of Asthma. The full contents of the supplement are available online at http://www.occup-med.com/content/3/S1.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
S.R. designed and wrote the manuscript, C.T. designed and wrote the manuscript
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Reuter, S., Taube, C. Mast cells and the development of allergic airway disease. J Occup Med Toxicol 3 (Suppl 1), S2 (2008). https://doi.org/10.1186/1745-6673-3-S1-S2
Published:
DOI: https://doi.org/10.1186/1745-6673-3-S1-S2