Abstract
Background
Hypertension is the leading global risk factor for mortality. Hypertension treatment and control rates are low worldwide, and delays in seeking care are associated with increased mortality. Thus, a critical component of hypertension management is to optimize linkage and retention to care.
Methods/Design
This study investigates whether community health workers, equipped with a tailored behavioral communication strategy and smartphone technology, can increase linkage and retention of hypertensive individuals to a hypertension care program and significantly reduce blood pressure among them. The study will be conducted in the Kosirai and Turbo Divisions of western Kenya. An initial phase of qualitative inquiry will assess facilitators and barriers of linkage and retention to care using a modified Health Belief Model as a conceptual framework. Subsequently, we will conduct a cluster randomized controlled trial with three arms: 1) usual care (community health workers with the standard level of hypertension care training); 2) community health workers with an additional tailored behavioral communication strategy; and 3) community health workers with a tailored behavioral communication strategy who are also equipped with smartphone technology. The co-primary outcome measures are: 1) linkage to hypertension care, and 2) one-year change in systolic blood pressure among hypertensive individuals. Cost-effectiveness analysis will be conducted in terms of costs per unit decrease in blood pressure and costs per disability-adjusted life year gained.
Discussion
This study will provide evidence regarding the effectiveness and cost-effectiveness of strategies to optimize linkage and retention to hypertension care that can be applicable to non-communicable disease management in low- and middle-income countries.
Trial registration
This trial is registered with (NCT01844596) on 30 April 2013.
Similar content being viewed by others
Background
Cardiovascular disease (CVD) is the leading cause of mortality in the world, with 80% of CVD deaths occurring in low- and middle-income countries (LMICs) [1]. Hypertension, a major risk factor for ischemic heart disease, heart failure, and stroke [2], is the leading global risk for mortality [3]. The global cost of suboptimal blood pressure (BP) is estimated to reach nearly $1 trillion over the next decade [4]. Unless adequately controlled, hypertension will continue to be responsible for significant morbidity and mortality worldwide [5].
Rationale for a focus on linkage and retention to care
Hypertension awareness, treatment, and control rates are low worldwide [6]. In Kenya, hypertension treatment and control rates have been reported at below 15% and 5%, respectively [7–9]. Given that hypertension may be asymptomatic, linkage and retention to care and medication adherence are particularly difficult challenges [10]. Delays in seeking hypertension care have been shown to be associated with increased mortality [11]. Thus, early linkage to hypertension care and successful retention to clinical services are critical components of hypertension management.
Studies of hypertension programs in sub-Saharan Africa have suggested that addressing financial barriers, provider-patient communication, and education may improve linkage, retention, and medication adherence [12–14]. Although preliminary qualitative research in western Kenya has revealed that community members understand that hypertension can cause significant morbidity and mortality [15], there are few known specific strategies to optimize linkage and retention to hypertension care in this setting.
Components of the proposed intervention to optimize linkage and retention to care
Community health workers (CHWs) are members of a community who have received basic training to supply community members with access to health and social services, to educate individuals about various health issues, and to support overall community development [16]. CHWs have been utilized in communicable disease and maternal/child health programs [17]. However, they are only recently being deployed and evaluated in the context of non-communicable diseases [18], and the impact of CHWs on linkage and retention to hypertension care in Africa is relatively unknown.
Motivational interviewing and tailored communication-strategies intended to tailor interventions based on individual-specific behavioral assessments-have been shown to improve a variety of health behaviors [19, 20]. In addition, mobile technology-based tools have the potential to improve the scope and efficiency of CHWs, and have demonstrated benefit for communicable diseases [21, 22]. However, these strategies have not been rigorously evaluated in the context of hypertension management in LMICs. Thus, we plan to utilize a multidisciplinary implementation research approach [23] to develop and evaluate innovative community-based strategies, supported by mobile technology, to optimize linkage and retention to a hypertension management program in western Kenya.
Aims
The central hypothesis of this study is that CHWs equipped with a tailored behavioral communication strategy, with or without smartphone technology, can increase linkage and retention of hypertensive individuals to a hypertension care program and thereby significantly reduce BP among these patients, when compared to usual care. We further hypothesize that these interventions will be cost-effective. Thus, the aims of this study are threefold. First, we aim to identify the facilitators and barriers to linking and retaining individuals with high BP to a hypertension care delivery program, using qualitative research methods. With this information, we will develop a communication strategy and a smartphone-based tool linked to an electronic health record. Second, we aim to evaluate the incremental effectiveness of the communication strategy and the smartphone-based tool in improving linkage and reducing BP among hypertensive patients. This will be done by conducting a three-arm cluster randomized controlled trial comparing: 1) usual care (CHWs with standard training on recruitment of individuals with any chronic condition); 2) CHWs with a communication strategy; and 3) CHWs with the communication strategy and equipped with smartphone technology. The co-primary outcome measures will be: 1) documented linkage to care, and 2) one year change in systolic BP (SBP) among those with hypertension. Third, we aim to evaluate the incremental cost-effectiveness of each intervention arm of the cluster randomized controlled trial, in terms of costs per unit decrease in BP and costs per disability-adjusted life year (DALY) gained.
Methods/Design
Setting
The United States Agency for International Development-Academic Model Providing Access to Healthcare Partnership (AMPATH) was initiated in Kenya in 2001 and has established a HIV care system in western Kenya that serves over 100,000 patients [24]. Based on that foundation, and in partnership with the Government of Kenya, AMPATH is expanding its clinical scope of work to include hypertension [25]. This study will be conducted within the AMPATH infrastructure in western Kenya, in the Kosirai and Turbo Divisions (Figure 1). Each Division is geographically and administratively divided into Community Units of approximately 5,000 individuals, with 9 units in Kosirai and 15 units in Turbo. Each Division has one rural health center staffed primarily by non-physician clinical officers trained to deliver a range of clinical health services [26], decentralized rural dispensaries staffed by nurses, and CHWs who are assigned to specific units. There has been a longstanding and positive relationship among AMPATH, the healthcare providers, and these communities [24, 27, 28]. The protocol has been approved by the institutional review boards of all participating institutions (Additional file 1), and the study is a registered on http://www.clinicaltrials.gov (identifier NCT01844596). Informed consent will be obtained from all study participants using a written informed consent form. During the consent process, participants will have the opportunity to request information and pose questions or concerns about their participation in the study.
Conceptual framework
Many behavior change models have been developed that focus on various types of health-related behavior and disease entities. In this study, we use the Health Belief Model, modified by incorporating the additional impact of emotional and environmental factors on behavior (Figure 2) [29]. The Health Belief Model is primarily a cognitive model based on the domains of perceived risk, perceived benefits, perceived barriers, cues to action, and self-efficacy [30]. While the Health Belief Model has been successfully applied to hypertension-related research in a variety of settings and populations [31, 32], we have expanded the model to incorporate the complex interactions among cognition, emotion, environment, and behavior. Emotional factors include desires, aspirations, fears, and worries that may directly motivate action or serve as a powerful lens to weigh advantages and disadvantages of alternative actions [33]. Environmental factors include socioeconomic factors, costs, political constraints, and cultural norms, which may facilitate or constrain an individual’s behavior.
Facilitators and barriers to linkage and retention to hypertension care
We will use a combination of qualitative research methods, including traditional community assemblies (mabaraza) and focus group discussions (FGDs), to identify the facilitators and barriers to linkage and retention to hypertension care. In East Africa, the mabaraza are used to address a wide variety of situations, ranging from local disputes to exchange of information. This unique and novel qualitative research setting has been used as a form of participatory action research related to HIV care [34]. The mabaraza allow us to organize large and heterogeneous groups of individuals, which complement the purposive sampling inherent in FGDs.
For all qualitative sessions, we have developed moderator guides, which have been used by trained moderators fluent in the local languages. We have thus far conducted 6 mabaraza and 17 FGDs using purposive sampling by age, sex, occupation, and distance from nearest health facility. Participatory techniques have been used to elicit emotional elements and promote group interactions [35]. All sessions have been audio-recorded, transcribed, and translated into English. Content analysis of the transcripts will be performed using both deductive (a priori) and inductive (emerging) codes [36]. The coded items will be grouped together into distinct themes, and relationships among these themes will be formulated.
Using the data gathered in the formative qualitative sessions, we will use a participatory, iterative design process to develop a tailored behavioral communication strategy for CHWs to use as they interact with patients and their families [37]. CHWs will be trained to engage in practical, motivating, proactive problem-solving with patients around such issues as transportation, clinic scheduling, home responsibilities, stigma concerns, and other issues that may be uncovered by the qualitative research. We will develop both a hard copy version and a smartphone version to be used by CHWs.
The smartphone version will be linked to the electronic health record and will have two functionalities: 1) ability to provide each CHW with an automatically updated list of individuals requiring follow up; and 2) the ability to provide real-time decision support based on the communication strategy, using data collected by the CHW during a patient encounter. The decision support will use branching logic and decision trees based on specific motivational messages, as well as simple clinical care algorithms appropriate for CHWs. The smartphone technology will allow for alternative messaging modalities, such as images and recordings (both audio and visual).
Cluster randomized controlled trial
We will conduct a cluster randomized controlled trial with three intervention arms: 1) usual care - CHWs with standard training on recruitment of individuals with any chronic condition (‘UC’); 2) CHWs with a tailored behavioral communication strategy (‘TBCS’); and 3) CHWs with a communication strategy who are also equipped with smartphone technology (‘TBCS-ST’). The unit of randomization will be the community unit, since randomization by CHW or patient would be at risk for contamination, as all CHWs and nearly all patients within one community unit are affiliated with the same dispensary. Randomization will be stratified by division, so that the 9 units of Kosirai will be randomized separately from the 15 units of Turbo. The units will be randomly allocated to one of the three intervention arms. The randomization process will be conducted centrally by biostatisticians at Brown University (Providence, United States). We will compare key variables (such as age, sex, severity of initial SBP, different treatment regimens, previous history of hypertension treatment, socioeconomic status, body mass index, physical activity, alcohol consumption, and tobacco use) to ensure balance among the randomized groups, and make adjustments in our treatment effect estimates as needed using logistic regression adjustment.
Study participants
Home-based BP testing using automatic BP machines has been initiated by AMPATH in both the Kosirai and Turbo divisions, with a plan to cover one-third of each community unit’s adult population every year. Inclusion criteria for this study will be all adult individuals with elevated BP (SBP >140 or diastolic BP (DBP) >90) during home-based testing, who will be assigned a unique medical record number and referred to the local dispensary for further evaluation (Figure 3). Exclusion criteria will be individuals without elevated BP, those who are acutely ill and require immediate medical attention at the time of testing, and individuals who do not provide informed consent. Enrollment will occur for one year in each unit.
An individual who does not present to the dispensary within one month will be defined as ‘non-linked’ and will be identified by the dispensary nurse. At that point in time, a CHW will be assigned to visit that individual to encourage linkage to care. Those who do not link to care within one month of the second CHW visit will be considered ‘chronic non-linked’. Individuals who ultimately link to care will be characterized as ‘self-linked’ (linked on their own without CHW intervention) or ‘CHW-mediated linked’. At the dispensary, each individual who has linked will have a repeat BP measured, and those with repeat elevated BP will be entered into the hypertension management program as patients. Patients will be managed according to the AMPATH hypertension protocol that is derived from consensus guidelines for hypertension management, using drugs contained in the Kenyan national formulary [38–40]. Patients who miss a clinic appointment for more than one month will be considered ‘non-retained’. Patients who are retained in care will be defined as either ‘self-retained’ (retained on their own without CHW intervention) or ‘CHW-mediated retained’. An individual will be considered ‘lost to follow up’ if they does not return to the clinic for three months despite CHW visits. The 12-month follow up BP will be measured in the dispensary, in order to mimic real-world practice.
Intervention and control
In the UC arm, the CHW will first measure the individual’s BP. If it is elevated (SBP >140 or DBP >90), the CHW will refer the individual to the dispensary for further evaluation and management, as per the usual care protocol.
In the TBCS arm, the CHW will measure the individual’s BP and then will engage in behavioral, clinical, and environmental assessments. Based on the behavioral assessment, the CHW will employ the communication strategy consisting of tailored behavioral and motivational messages, as described above. Depending on the severity of the clinical assessment, the CHW will either refer or accompany high-risk patients to the dispensary. The environmental assessment will evaluate socioeconomic barriers to care-seeking, and the CHW will provide this information to the nurses in the dispensary.
In the TBCS-ST arm, the CHW will conduct all assessments described above; however, s/he will also be equipped with a smartphone that has real-time decision support and data entry that is linked to the electronic health record. Thus, the smartphone will provide the tailored messaging and specific recommendations based on inputs from the assessments. The smartphone technology would allow for alternative messaging modalities, such as images and recordings (audio and visual), to ensure its applicability to a population speaking diverse languages and with different literacy levels. If a patient does successfully go to the dispensary for the linkage visit, this visit will be entered into the electronic health record and we will program the system to immediately send a positive reinforcement message to the CHW.
Outcomes
The co-primary outcome measures will be: 1) documented linkage to care, defined as a confirmed dispensary visit within one month of either home-based testing (self-linked) or a CHW visit (CHW-mediated linked), and 2) one-year change in SBP among those with hypertension. Our ultimate goal is to implement an intention-to-treat comparison of change in SBP among confirmed hypertensive individuals. However, confirmation of hypertensive status requires at least two BP measurements, and this requires successful linkage to care (Figure 3). Hence, we have opted for the co-primary outcome approach. We will compare the proportion linked to care between the three study arms using conditional logistic regression. For the SBP outcome, we will implement an intention-to-treat comparison of change in SBP between the three study arms. For those who are not successfully linked to care, we will use imputed SBP values. Full details of our approach to imputation appear in Additional file 2.
Statistical power
The study is powered on the linkage-to-care outcome in order to preserve the properties of randomization at the community unit level and avoid bias due to differential selection into care by the linkage intervention. In light of AMPATH’s pilot experience with home-based testing and linkage to hypertension care [10], we anticipate that the usual care arm will have 40% linkage (self-linked plus CHW-mediated linked). The study is powered to detect an absolute difference of 20% in percent linkage to care between each of the three treatment arms (expected 60% linkage in the TBCS arm and 80% linkage in the TBCS-ST arm). It is expected that 226 people will be referred to the dispensary per community unit per year, based on the following: 1) each community unit has a population of approximately 5,000; 2) 45.3% of the population is above the age of 20 [41]; 3) one-third of the population will be screened during the year; and 4) approximately 30% of adults will have an elevated SBP at the home-based testing [10].
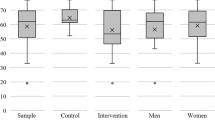
Our power calculations set overall Type I error rate at 5% (alpha = 0.05), and use a Bonferroni correction to permit all pairwise comparisons between treatment arms. To account for cluster effects, we consider scenarios where intraclass correlation (ICC) ranges from 0 to 0.15 [42]. Plots demonstrating power for each of the pairwise treatment arm comparisons across different values of ICC reveal that our pairwise comparisons have over 80% power over a large range of ICC values (Figure 4).
Power to detect differences in the proportion of patients linked to care over a realistic range of ICC coefficients. Horizontal line is at 80% power. CHWs, community health workers; ICC, intraclass correlation; TBCS, CHWs with a tailored behavioral communication strategy; TBCS-ST, CHWs with a communication strategy and also equipped with smartphone technology; UC, usual care.
Cost-effectiveness analysis
For each intervention arm, costs from the societal perspective will be captured using validated cost questionnaires and will include all relevant labor, materials, supplies, and contracted services costs for all activities required to deliver the interventions [43, 44]. Only incremental (variable and fixed) costs will be included in the analysis. We will also identify which activities drive the overall costs, and how costs would change if specific activities are added or eliminated. We will also identify potential cost offsets (reductions in health services utilization as a result of participation in a specific arm) using health service utilization data contained within the electronic health record and based on utilization and cost questionnaires that participants will take at baseline and 12 months. We will thus quantify the net costs of participation in each intervention arm.
Once costs and effectiveness are calculated for each intervention arm, we will then generate incremental cost-effectiveness ratios (ICERs) following the approach described in the literature [43]. First, costs and effectiveness measures will be tabulated for each strategy in order of increasing costs. After removing dominated interventions, we will present the final ICERs and provide comparisons to other CVD interventions and to other interventions targeting this population after first converting the results to international dollars using World Health Organization conversion rates [45]. Our results will also be presented in the form of cost-effectiveness acceptability curves [46], which will show the probability that each strategy is cost-effective for a range of monetary values that a decision-maker might be willing to pay for a unit change in effectiveness. In addition, we will perform one-way (and n-way) sensitivity analyses, in which we will examine the effect of changing one (or n) of the model parameters, holding all other parameters constant.
We will evaluate the incremental cost-effectiveness of each intervention arm, both in terms of costs per unit decrease in BP and in terms of costs per unit reduction in CVD risk by extrapolating one-year BP reductions to CVD risk reductions based on the QRISK™2-2011 CVD risk calculator (University of Nottingham, Nottingham, United Kingdom) specific for Black African populations [47]. We will then present costs per DALY saved by extrapolating these reductions to all-cause mortality, using an approach we have previously developed, with care to note all assumptions required [48].
Discussion
The global burden of hypertension and other non-communicable diseases is substantial and increasing, especially in LMICs. However, insufficient data exist regarding effective health care delivery practices in these settings. Each step in the implementation pathway, including linkage and retention to care, can benefit from evidence-based approaches. The LARK hypertension study has been designed with these objectives in mind, and offers several unique and innovative elements. First, we are expanding the traditional Health Belief Model to include emotional and environmental factors that influence health behavior. Second, we are utilizing the mabaraza form of qualitative inquiry and actively pursuing a participatory methodology throughout all phases of the research. Third, we are evaluating the use of mobile technology in a novel domain of non-communicable disease care delivery. Fourth, we are embedding the research within a foundational partnership of academic institutions, communities, and local government, to ensure that the program meets the needs of all stakeholder groups. Finally, we are working within the existing structure of primary care delivery that is established by the government.
We aim to demonstrate how the infrastructure and strategies that have been established for the control of communicable diseases-including community-based screening, task redistribution within teams, partnerships with local providers, and medical informatics- can serve as a foundation for an integrated delivery system approach to the control of non-communicable chronic conditions [49]. Thus, the results of this project can serve as a platform to be used for other non-communicable diseases, such as stroke, diabetes, respiratory disease, cancer, and mental illness. While this research is situated within a particular sociocultural and institutional context, we aim to produce generalizable methods and results that can be applied in other settings. We therefore hope that this project will provide a model for the evaluation of other new approaches to non-communicable disease management in LMICs.
Trial status
The cluster randomized controlled trial portion of this study has not yet begun. The qualitative portion of the study is currently ongoing.
Abbreviations
- AMPATH:
-
academic model providing access to healthcare partnership
- BP:
-
blood pressure
- CHW:
-
community health worker
- CVD:
-
cardiovascular disease
- DALY:
-
disability-adjusted life year
- DBP:
-
diastolic blood pressure
- FGD:
-
focus group discussion
- ICC:
-
intraclass correlation
- ICER:
-
incremental cost-effectiveness ratio
- LMICs:
-
low- and middle- income countries
- SBP:
-
systolic blood pressure
- TBCS:
-
tailored behavioral communication strategy
- TBCS-ST:
-
tailored behavioral communication strategy with smartphone technology
- UC:
-
usual care.
References
Fuster V, Kelly BB: Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. 2010, Washington, DC: National Academies Press
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R: Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002, 360 (9349): 1903-1913.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C: A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012, 380 (9859): 2224-2260. 10.1016/S0140-6736(12)61766-8.
Gaziano TA, Bitton A, Anand S, Weinstein MC: The global cost of nonoptimal blood pressure. J Hypertens. 2009, 27 (7): 1472-1477. 10.1097/HJH.0b013e32832a9ba3.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J: Global burden of hypertension: analysis of worldwide data. Lancet. 2005, 365 (9455): 217-223. 10.1016/S0140-6736(05)17741-1.
Pereira M, Lunet N, Azevedo A, Barros H: Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009, 27 (5): 963-975. 10.1097/HJH.0b013e3283282f65.
Hendriks ME, Wit FW, Roos MT, Brewster LM, Akande TM, de Beer IH, Mfinanga SG, Kahwa AM, Gatongi P, Van Rooy G, Janssens W, Lammers J, Kramer B, Bonfrer I, Gaeb E, van der Gaag J, de Wit TF R, Lange JM, Schultsz C: Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PLoS One. 2012, 7 (3): e32638-10.1371/journal.pone.0032638.
van de Vijver SJ, Oti SO, Agyemang C, Gomez GB, Kyobutungi C: Prevalence, awareness, treatment and control of hypertension among slum dwellers in Nairobi Kenya. J Hypertens. 2013, 31 (5): 1018-1024. 10.1097/HJH.0b013e32835e3a56.
Mathenge W, Foster A, Kuper H: Urbanization, ethnicity and cardiovascular risk in a population in transition in Nakuru, Kenya: a population-based survey. BMC Public Health. 2010, 10: 569-10.1186/1471-2458-10-569.
Pastakia S, Ali SM, Kamano J, Akwanalo CO, Ndege SK, Buckwalter V, Vedanthan R, Bloomfield GS: Screening for diabetes and hypertension in a rural low income setting in western Kenya utilizing home-based and community-based strategies. Global Health. 2013, 9: 21-10.1186/1744-8603-9-21.
Moodley J: Maternal deaths associated with hypertension in South Africa: lessons to learn from the saving mothers report, 2005–2007. Cardiovasc J Afr. 2011, 22 (1): 31-35.
Labhardt ND, Balo JR, Ndam M, Manga E, Stoll B: Improved retention rates with low-cost interventions in hypertension and diabetes management in a rural African environment of nurse-led care: a cluster-randomised trial. Trop Med Int Health. 2011, 16: 1276-1284. 10.1111/j.1365-3156.2011.02827.x.
Ohene Buabeng K, Matowe L, Plange-Rhule J: Unaffordable drug prices: the major cause of non-compliance with hypertension medication in Ghana. J Pharm Pharm Sci. 2004, 7 (3): 350-352.
Magadza C, Radloff SE, Srinivas SC: The effect of an educational intervention on patients’ knowledge about hypertension, beliefs about medicines, and adherence. Res Social Adm Pharm. 2009, 5 (4): 363-375. 10.1016/j.sapharm.2009.01.004.
Naanyu V, Greene J, Mamlin JJ, Kimaiyo S: An exploration of the best location to refer Eldoret and Burnt Forest individuals newly diagnosed with hypertension or diabetes. USAID-Academic Model Providing Access to Healthcare (AMPATH) Program Report. 2010, Eldoret, Kenya: AMPATH
Prasad B, Muraleedharan V: Community health workers: a review of concepts, practice and policy concerns. 2007, London: Consortium for Research on Equitable Health Systems
Jokhio AH, Winter HR, Cheng KK: An intervention involving traditional birth attendants and perinatal and maternal mortality in Pakistan. N Engl J Med. 2005, 352 (20): 2091-2099. 10.1056/NEJMsa042830.
Jafar TH, Hatcher J, Poulter N, Islam M, Hashmi S, Qadri Z, Bux R, Khan A, Jafary FH, Hameed A, Khan A, Badruddin SH, Chaturvedi N, Hypertension Research Group: Community-based interventions to promote blood pressure control in a developing country: a cluster randomized trial. Ann Intern Med. 2009, 151 (9): 593-601. 10.7326/0003-4819-151-9-200911030-00004.
Rimer BK, Kreuter MW: Advancing tailored health communication: a persuasion and message effects perspective. J Commun. 2006, 56: S184-S201. 10.1111/j.1460-2466.2006.00289.x.
Ogedegbe G, Chaplin W, Schoenthaler A, Statman D, Berger D, Richardson T, Phillips E, Spencer J, Allegrante JP: A practice-based trial of motivational interviewing and adherence in hypertensive African Americans. Am J Hypertens. 2008, 21 (10): 1137-1143. 10.1038/ajh.2008.240.
Braitstein P, Einterz RM, Sidle JE, Kimaiyo S, Tierney W: “Talkin’ about a revolution”: How electronic health records can facilitate the scale-up of HIV care and treatment and catalyze primary care in resource-constrained settings. J Acquir Immune Defic Syndr. 2009, 52 (Suppl 1): S54-S57.
Noormohammad SF, Mamlin BW, Biondich PG, McKown B, Kimaiyo SN, Were MC: Changing course to make clinical decision support work in an HIV clinic in Kenya. Int J Med Inform. 2010, 79 (3): 204-210. 10.1016/j.ijmedinf.2010.01.002.
Vedanthan R: Global health delivery and implementation research: a new frontier for global health. Mt Sinai J Med. 2011, 78 (3): 303-305. 10.1002/msj.20250.
Einterz RM, Kimaiyo S, Mengech HN, Khwa-Otsyula BO, Esamai F, Quigley F, Mamlin JJ: Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med. 2007, 82 (8): 812-818. 10.1097/ACM.0b013e3180cc29f1.
Bloomfield GS, Kimaiyo S, Carter EJ, Binanay C, Corey GR, Einterz RM, Tierney WM, Velazquez EJ: Chronic noncommunicable cardiovascular and pulmonary disease in sub-Saharan Africa: an academic model for countering the epidemic. Am Heart J. 2011, 161 (5): 842-847. 10.1016/j.ahj.2010.12.020.
Mullan F, Frehywot S: Non-physician clinicians in 47 sub-Saharan African countries. Lancet. 2007, 370 (9605): 2158-2163. 10.1016/S0140-6736(07)60785-5.
Kamano JH, Vedanthan R, Mutua E, Pastakia S, Fuster V, Horowitz C, Mamlin JJ, Kimaiyo S: Partnerships among academia, government and community to optimize delivery of care for non-communicable diseases in western Kenya. 2012, Washington, DC: Presented at Science of Eliminating Health Disparities Summit
Inui TS, Nyandiko WM, Kimaiyo SN, Frankel RM, Muriuki T, Mamlin JJ, Einterz RM, Sidle JE: AMPATH: living proof that no one has to die from HIV. J Gen Intern Med. 2007, 22 (12): 1745-1750. 10.1007/s11606-007-0437-4. Epub 2007 Oct 31. PubMed PMID: 17972138
Bandura A: The self system in reciprocal determinism. Am Psychol. 1978, 33 (4): 344-344.
Becker MH: The Health Belief Model And Personal Health Behavior. 1974, San Francisco: Society for Public Health Education
Newell M, Modeste N, Marshak HH, Wilson C: Health beliefs and the prevention of hypertension in a black population living in London. Ethn Dis. 2009, 19 (1): 35-41.
Thalacker KM: Hypertension and the hmong community: using the health belief model for health promotion. Health Promot Pract. 2011, 12 (4): 538-543. 10.1177/1524839909353735.
Baumeister RF, Vohs KD, Nathan DeWall C, Zhang L: How emotion shapes behavior: feedback, anticipation, and reflection, rather than direct causation. Pers Soc Psychol Rev. 2007, 11 (2): 167-203. 10.1177/1088868307301033.
Naanyu V, Sidle JE, Frankel RM, Ayuku D, Nyandiko WM, Inui TS: Rooting inquiry in tradition: the health baraza as a tool for social research in Kenya. Qual Health Res. 2011, 21 (1): 14-26. 10.1177/1049732310367498.
Scrimshaw NS, Gleason GR: Rapid assessment procedures: qualitative methodologies for planning and evaluation of health related programmes. 1992, Boston: International Nutrition Foundation for Developing Countries
Neuendorf KA: The Content Analysis Guidebook. 2002, Thousand Oaks, CA: Sage Publications
Carter JA, Molyneux CS, Mbuba CK, Jenkins J, Newton CR, Hartley SD: The reasons for the epilepsy treatment gap in Kilifi, Kenya: using formative research to identify interventions to improve adherence to antiepileptic drugs. Epilepsy Behav. 2012, 25 (4): 614-621. 10.1016/j.yebeh.2012.07.009.
Whitworth JA: 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003, 21 (11): 1983-1992.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ, National High Blood Pressure Education Program Coordinating Committee: The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003, 289 (19): 2560-2572. 10.1001/jama.289.19.2560.
Crouch M: Clinical Management and Referral Guidelines, Volume III. 2010, Nairobi: Kenyan Ministry of Medical Services and Ministry of Public Health and Sanitation
Kenya National Bureau of Statistics (KNBS) and ICF Macro: Kenya Demographic and Health Survey 2008–09. 2010, Calverton, MD: KNBS and ICF Macro
Littenberg B, MacLean CD: Intra-cluster correlation coefficients in adults with diabetes in primary care practices: the vermont diabetes information system field survey. BMC Med Res Methodol. 2006, 6: 20-10.1186/1471-2288-6-20.
Gold MR, Siegel JE, Russell LB, Weinstein MC: Cost-effectiveness in health and medicine. 1996, New York: Oxford University Press
Finkelstein EA, Wittenborn JS, Farris RP: Evaluation of public health demonstration programs: the effectiveness and cost-effectiveness of WISEWOMAN. J Womens Health. 2004, 13 (5): 625-633. 10.1089/1540999041281043.
Purchasing power parity conversion factor, GDP. [http://data.worldbank.org/indicator/PA.NUS.PPP]
Fenwick E, Claxton K, Sculpher M: Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ. 2001, 10: 779-787. 10.1002/hec.635.
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, Brindle P: Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008, 336 (7659): 1475-1482. 10.1136/bmj.39609.449676.25.
Finkelstein EA, Khavjou O, Will JC: Cost-effectiveness of WISEWOMAN, a program aimed at reducing heart disease risk among low-income women. J Womens Health. 2006, 15 (4): 379-389. 10.1089/jwh.2006.15.379.
Rabkin M, El-Sadr WM: Why reinvent the wheel? Leveraging the lessons of HIV scale-up to confront non-communicable diseases. Glob Public Hlth. 2011, 6 (3): 247-256. 10.1080/17441692.2011.552068.
Acknowledgements
The authors would like to thank the LARK research team - Claire Hutchinson, Peninah Kiptoo, Kennedy Lagat, and Jackson Rotich - for their assistance with all aspects of the project. We would like to thank Vishal Marwah for assistance with preparation of the figures. We also thank Jadry Gruen for editorial assistance. Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number 1U01HL114200, United States, under The Global Alliance for Chronic Diseases programme RV receives salary support from the Fogarty International Center of the National Institutes of Health under Award Number K01 TW 009218 - 03.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
VF is the principal investigator of the study, was responsible for and conceived the concept and design of the overall study, had ultimate oversight over the study design and conduct of the study, and reviewed the manuscript critically for content. RV contributed to the content and design of the overall study and drafted the manuscript. JHK contributed to the content and design of the overall study and reviewed the manuscript critically for content. VN led the design of the qualitative portion of the study and reviewed the manuscript critically for content. AKD contributed to the randomization protocol and statistical analysis plan and reviewed the manuscript critically for content. MCW led the design of the information technology component of the study and reviewed the manuscript critically for content. EAF designed the cost-effectiveness analysis and reviewed the manuscript critically for content. DM contributed to the design of the community health worker intervention and reviewed the manuscript critically for content. COA contributed to the overall protocol development and reviewed the manuscript critically for content. GSB contributed to the content and design of the study and reviewed the manuscript critically for content. CAB contributed to the overall protocol development and reviewed the manuscript critically for content. EJV contributed to the content and design of the study and reviewed the manuscript critically for content. JWH led the design of the randomization protocol and statistical analysis plan and reviewed the manuscript critically for content. CRH contributed to the content and design of the study and reviewed the manuscript critically for content. TSI contributed to the content and design of the study and reviewed the manuscript critically for content. SK contributed to the content and design of the study and reviewed the manuscript critically for content. All authors read and approved the final manuscript.
Electronic supplementary material
13063_2013_2028_MOESM2_ESM.zip
Additional file 2: Figure S1: Schematic illustrating the strategy for estimating intention-to-treat effect on change in SBP among those diagnosed with hypertension. Light gray boxes represent individuals with suspected hypertension at time 0; white boxes represent patients with hypertension; dark gray boxes represent those without hypertension. Abbreviations as in the Appendix; FU = follow-up. (ZIP 289 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Vedanthan, R., Kamano, J.H., Naanyu, V. et al. Optimizing linkage and retention to hypertension care in rural Kenya (LARK hypertension study): study protocol for a randomized controlled trial. Trials 15, 143 (2014). https://doi.org/10.1186/1745-6215-15-143
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1745-6215-15-143