Abstract
Background
Caspase-1 is a cysteine protease responsible for the processing and secretion of IL-1β and IL-18, which are closely related to the induction of inflammation. However, limited evidence addresses the participation of caspase-1 in inflammatory pain. Here, we investigated the role of caspase-1 in inflammatory hypernociception (a decrease in the nociceptive threshold) using caspase-1 deficient mice (casp1-/-).
Results
Mechanical inflammatory hypernociception was evaluated using an electronic version of the von Frey test. The production of cytokines, PGE2 and neutrophil migration were evaluated by ELISA, radioimmunoassay and myeloperoxidase activity, respectively. The interleukin (IL)-1β and cyclooxygenase (COX)-2 protein expression were evaluated by western blotting. The mechanical hypernociception induced by intraplantar injection of carrageenin, tumour necrosis factor (TNF)α and CXCL1/KC was reduced in casp1-/- mice compared with WT mice. However, the hypernociception induced by IL-1β and PGE2 did not differ in WT and casp1-/- mice. Carrageenin-induced TNF-α and CXCL1/KC production and neutrophil recruitment in the paws of WT mice were not different from casp1-/- mice, while the maturation of IL-1β was reduced in casp1-/- mice. Furthermore, carrageenin induced an increase in the expression of COX-2 and PGE2 production in the paw of WT mice, but was reduced in casp1-/- mice.
Conclusion
These results suggest that caspase-1 plays a critical role in the cascade of events involved in the genesis of inflammatory hypernociception by promoting IL-1β maturation. Because caspase-1 is involved in the induction of COX-2 expression and PGE2 production, our data support the assertion that caspase-1 is a key target to control inflammatory pain.
Similar content being viewed by others
Background
Inflammatory hypernociception results mainly from the sensitisation of primary afferent neurons and is detected as a decrease of the nociceptive threshold in animal models [1]. It is induced by inflammatory mediators, such as prostaglandins and sympathetic amines, that directly sensitise peripheral nociceptive neurons [2–4]. The release of these direct-acting hyperalgesic mediators is generally preceded by a cascade of cytokines [5]. Recently, we demonstrated that inflammatory hypernociception in mice is mediated by a concomitant release of tumour necrosis factor alpha (TNFα) and keratinocyte-derived chemokine (CXCL1/KC). Both mediators stimulate the subsequent release of interleukin (IL)-1β that in turn induces prostanoid production [6]. CXCL1/KC also stimulates the sympathetic component of inflammatory hypernociception [6]. Another important event that mediates inflammatory hypernociception is neutrophil migration [7]. It has also been demonstrated that the hyperalgesic effect of cytokines depends on neutrophil recruitment that, in the last instance, seems to be important for the production of directly-acting hyperalgesic mediators such as prostaglandin E2 (PGE2) [7].
Caspase-1 (previously known as IL-1 converting enzyme -ICE) is a member of the caspase family of proteases and is responsible for the processing and secretion of IL-1β and IL-18, two cytokines that are critical for inflammation [8, 9]. For instance, caspase-1-deficient mice (casp1-/-) have a defect in the maturation of pro-IL-1β and pro-IL-18 and are resistant to LPS-induced endotoxic shock [10]. Furthermore, the treatment of mice with a selective inhibitor of caspase-1 had reduced collagen-induced arthritis [11]. In this context, caspase-1 was considered an important target to control inflammatory diseases.
Although the action of caspase-1 in the maturation of IL-1β and IL-18 is an important step in the cascade of inflammatory events, there have been limited studies that investigate its role in the genesis of inflammatory pain [12, 13]. For instance, a selective inhibitor of caspase-1 was found to inhibit yeast-induced hypernociception in rats [12]. Nonetheless, more conclusive evidence about the participation and the role of caspase-1 in inflammatory hypernociception is required. In the present study, we addressed the role of caspase-1 in carrageenin-induced mechanical inflammatory hypernociception using mice deficient in this enzyme. We focused mainly in the peripheral mechanisms involved in caspase-1 mediation of this inflammatory symptom. Our results indicate that caspase-1 plays a crucial role in genesis of inflammatory pain by promoting IL-1β maturation in the site of inflammation.
Results
Caspase-1-/- mice show reduced mechanical inflammatory hypernociception
In the first set of experiments we evaluated the mechanical nociceptive threshold of WT and casp1-/- mice. Mechanical nociceptive thresholds of casp1-/- mice did not differ from WT littermates (Figure 1A). On the other hand, carrageenin-induced mechanical hypernociception was reduced in casp1-/- mice compared with WT mice. These differences were observed 3 and 5 h after stimuli injection (Figure 1B). The reduction in inflammatory hypernociception in casp1-/- mice was not accompanied by a reduction in carrageenin-induced paw oedema (WT/Saline 0.01 ± 0.003 mm3; WT/carrageenin 0,075 ± 0,007 mm3 casp1-/-Saline 0,01 ± 0,004 mm3; casp1-/-/carrageenin 0,06 ± 0,005 mm3).
The involvement of caspase-1 in mechanical inflammatory hypernociception. (A) Mechanical nociceptive threshold of wild type and casp1-/- mice using the electronic von Frey. (B) Wild type or casp1-/- mice received an intraplantar injection of carrageenin (100 μg/paw). Mechanical hypernociception was evaluated 3 and 5 h after carrageenin injection. (C) Mice were pretreated with a caspase-1 inhibitor (YVAD-CMK, 1-9 mg/kg s.c. 30 min before) followed by intraplantar injection of carrageenin (100 μg/paw). Mechanical hypernociception was evaluated 3 h after carrageenin injection. Data are expressed as the mean ± S.E.M. of 5 animals per group. * indicates statistical significance compared to the saline injected group; # statistical significance compared to wild type or vehicle-treated group. P < 0.05, one-way ANOVA followed by the Bonferroni's test.
For a clinical perspective, we evaluated the effect of a selective inhibitor of caspase-1 (Ac-YVAD-CMK) on inflammatory hypernociception. It was observed that the pretreatment of mice with YVAD-CMK (1-9 mg/kg s.c.; 30 min before carrageenin injection), inhibited carrageenin-induced mechanical hypernociception in a dose-dependent manner (Figure 1C).
Neither neutrophil nor pro-nociceptive cytokines (TNFα and CXCL1/KC) are involved in caspase-1 mediation of inflammatory hypernociception
Next, it was evaluated whether the reduction of inflammatory hypernociception in casp1-/- mice was associated with a reduction in the production of pro-nociceptive cytokines (TNFα or chemokines CXCL1/KC) or associated with a reduction in neutrophil migration. It was observed that the increase in the production of TNFα and CXCL1/KC after intraplantar injection of carrageenin in WT mice was not different from casp-1-/- mice (Figure 2A and B, respectively). Carrageenin-induced neutrophil migration was also not reduced in casp1-/- mice compared with WT mice (Figure 2C). In agreement with these findings, the doses of YVAD-CMK that inhibited carrageenin-induced mechanical hypernociception did not alter carrageenin-induced neutrophil migration (data not shown).
Role of neutrophils and cytokines in caspase-1 mediation of inflammatory hypernociception. (A-B) Wild type and casp1-/- mice received an intraplantar injection of carrageenin or saline. After 3 h, plantar tissue samples were removed and the levels of TNF-α and CXCL1/KC were determined by ELISA. (C) At 3 h after carrageenin injection, the activity of MPO was determined in the mice paw skin of wild type and casp1-/- mice as an index of neutrophil migration. Data are expressed as the mean ± S.E.M. of 5 animals per group. * indicates statistical significance compared to the saline-injected group. P < 0.05, one-way ANOVA followed by the Bonferroni's test.
Caspase-1 mediates TNFα and CXCL1/KC-induced mechanical hypernociception but is not induced by IL-1β or PGE2
Mechanical hypernociception induced by intraplantar injection of TNFα or CXCL1/KC was reduced in casp1-/- mice compared with WT mice (Figure 3A). On the other hand, the mechanical hypernociception induced by IL-1β or by PGE2 was not different in casp1-/- mice compared with WT mice (Figure 3A and 3B).
Role of caspase-1 in the mechanical hypernociception induced by pro-nociceptive cytokines and PGE 2 . (A) Wild type or casp1-/- mice received an intraplantar injection of TNF-α (100 pg/paw), CXCL1/KC (10 ng/paw or IL-1β (1 ng/paw). Mechanical hypernociception was evaluated 3 h after cytokines injection. (B) Wild type or casp1-/- mice received and intraplantar injection of PGE2 (100 ng/paw). Mechanical hypernociception was evaluated 0.5, 1.0, and 1.5 h after PGE2 injection. Data are expressed as the mean ± S.E.M. of 5 animals per group. * indicates statistical significance compared to the saline-injected group; # indicates statistical significance compared to wild type group. P < 0.05, one-way ANOVA followed by the Bonferroni's test.
IL-1β maturation in the inflammatory site, but not maturation of IL-18, accounts for caspase-1 mediation of inflammatory hypernociception
In the next part of this study, we tested the hypothesis that caspase-1 mediates inflammatory hypernociception by its action on IL-1β or IL-18 processing. Although carrageenin-induced mechanical hypernociception was not reduced in IL-18 null mice compared with WT mice (Figure 4A), the treatment of mice with IL-1ra (3-90 mg/kg, i.v. 15 min before carrageenin injection) reduced carrageenin-induced hypernociception in a dose-dependent manner (Figure 4B).On the other hand, IL-1ra treatment did not alter carrageenin-induced neutrophil migration toward mice paws (Figure 4C). The implication of IL-1β processing in the role of caspase-1 in inflammatory hypernociception was supported by the fact that while the increase in the expression of mRNA for pro-IL-1β induced in the mice paw by carrageenin was similar in WT and casp1-/- (Figure 4D), the expression of mature IL-1β (~19 kDa) was reduced in casp1-/- (Figure 4E). Densitometric analyses of the bands are present in Figure 4F.
IL-1β maturation, but not maturation of IL-18, is involved in caspase-1 mediation of inflammatory hypernociception. (A) Wild type or IL-18-/- mice received an intraplantar injection of carrageenin (100 μg/paw). Mechanical hypernociception was evaluated 3 h after carrageenin injection. Mice were pretreated with IL-1ra (3-90 mg/kg, i.v. 15 min before carrageenin injection) followed by intraplantar injection of carrageenin (100 μg/paw). Mechanical hypernociception was evaluated 3 h after carrageenin injection. (C) After the determination of hypernociception, mice paw skins were removed and the activity of MPO was determined. (D) Wild type and casp1-/- mice received an intraplantar injection of carrageenin or saline. After 1.5 h, plantar tissue samples were removed and the level of pro-IL-1β mRNA was determined by real-time PCR. (D) Wild type and casp1-/- mice received an intraplantar injection of carrageenin or saline. After 3 h, plantar tissue samples were removed and the level of mature IL-1β (~19 kDa) was determined by western blot. The β-actin level was used as a control. Data are presented as representative blots. Densitometry of the pixel intensity of IL-1β bands relative to β-actin is present. Data are expressed as the mean ± S.E.M. of 5 animals per group. * indicates statistical significance compared to the saline-injected group; # indicates statistical significance compared to the vehicle-treated group or wild type mice group. P < 0.05, one-way ANOVA followed by the Bonferroni's test.
Peripheral COX-2 induction and PGE2 production depends on caspase-1
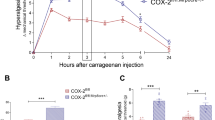
Because it was previously demonstrated that the induction of COX-2 expression and the production of the direct-acting hypernociceptive mediator, PGE2, during inflammatory hypernociception is mediated by IL-1β [6]; we evaluated the contribution of caspase-1 in these events. Western blot analyses revealed that the increase in the COX-2 expression induced by carrageenin in WT mice is reduced in casp1-/- mice (Figure 5A). Densitometric analyses of the bands are present in Figure 5B. The reduction in COX-2 expression was also associated with a decrease in the production of PGE2 in casp1-/- mice compared with WT mice (Figure 5C).
Role of caspase-1 in the induction of COX-2 and prostaglandin production during carrageenin-induced inflammation. (A) Wild type and casp1-/- mice received an intraplantar injection of carrageenin (100 μ/paw) or saline. After 3 h, plantar tissue samples were removed and the expression of COX-2 was determined by western blot. The β-actin level was used as a control. Data are presented as representative blots. (B) Densitometry of the pixel intensity of COX-2 bands relative to β-actin is present. (C) Wild type and casp1-/- mice received an intraplantar injection of carrageenin (100 μ/paw) or saline. After 3 h, plantar tissue samples were removed and the level of PGE2 was determined by RIA. Data are expressed as the mean ± S.E.M. of 5 animals per group. * indicates statistical significance compared to the saline-injected group; # indicates statistical significance compared to the wild type group. P < 0.05, one-way ANOVA followed by the Bonferroni's test.
Discussion
Caspase-1, originally described as interleukin converting enzyme, is an intracellular enzyme that plays a role in the maturation of two important mediators of inflammation, IL-1β and IL-18 [14–16]. Recently, it was suggested that caspase-1 also metabolises another inflammatory mediator, IL-33; however, contrary to IL-1β and IL-18, it seems that caspase-1 action upon IL-33 produces an inactive form of this cytokine [17]. In the present study, we demonstrated that caspase-1 plays a crucial role in the cascade of events involved in the genesis of inflammatory hypernociception. Indeed, caspase-1 null mice present a reduction in carrageenin-induced hypernociception, and a selective inhibitor of caspase-1 presents an antinociceptive effect in this mice model. Our present results corroborate a previous finding of Elford et al. (1995) that showed that the treatment of rats with a selective inhibitor of caspase-1 reduced mechanical hypernociception in a model of yeast-induced inflammation [12]. Extending these observations, it was recently shown that caspase-1 mediates the induction of a complex regional pain syndrome that developed after tibia fracture in rats [18].
It is well known that the release of cytokines in the inflammatory site is involved in the induction of inflammatory hypernociception. In addition, it seems that these pro-nociceptive cytokines are released sequentially [6]. In this cascade, TNFα and chemokines, such as CXCL1/KC, are released earlier [6]. Investigating whether caspase-1 might account for the release of these two cytokines, we detected that the levels of TNFα and CXCL1/KC in carrageenin-inflamed mice paws are similar in WT and casp1-/- mice, suggesting that the caspase-1 pro-nociceptive role is downstream of TNFα and CXCL1/KC. Our results also refute that the pro-nociceptive role of caspase-1 in carrageenin inflammation is dependent on its capacity to process IL-18. This conclusion is based in the fact that IL-18 null mice present similar hypernociception after carrageenin paw injection compared with WT mice. Nonetheless, the involvement of caspase-1 in complex regional pain syndrome triggered by tibia fracture seems to be dependent on IL-18 processing [18]. Moreover, IL-18 also plays a role in the genesis of hypernociception in a model of immune inflammation induced by ovalbumin in previously immunised mice, and in this model caspase-1 might be responsible for IL-18 processing [19]. We also recently showed that besides cytokines, the recruitment of neutrophils to inflammatory sites mediates carrageenin-induced hypernociception [7]. However, it is also seems that the caspase-1 pro-nociceptive role is not related to neutrophils, because neutrophil accumulation in the mice paws of casp1-/- is similar to WT mice.
TNFα and CXCL-1/KC hypernociceptive roles in carrageenin inflammation were demonstrated to be, at least in part, dependent on the production of IL-1β [6]. This fact, together with our present observation that casp1-/- mice present reduced hypernociception induced by TNF-α and CXCL1/KC but not by IL-1β and PGE2, is strongly suggestive that caspase-1 could be mediating inflammatory hypernociception through its product, mature IL-1β. Indeed, we detected that while the mRNA for pro-IL-1β increased at the same levels in casp1-/- and WT mice after carrageenin injection, there was a reduction in the mature form of IL-1β in casp-1-/- mice. This suggestion was supported by the observation that IL-1ra treatment reduced carrageenin-induced hypernociception. Corroborating the idea that IL-1β processing is the mechanism by which caspase-1 mediates inflammatory hypernociception, it was observed that IL-1ra treatment did not alter the neutrophil migration induced by carrageenin similarly observed in casp1-/- mice. It is somehow striking because IL-1β hypernociceptive effect is dependent on neutrophil migration [7]. At this moment, we have the hypothesis that that in carrageenin-induced inflammation neutrophils are recruited mainly by TNFα and CXCR2 ligands (CXCL1/KC in mice or CINC-1 in rats) and they are activated in the site of inflammation by IL-1β that in turn induced the expression of COX-2 and the production of PGE2.
Although casp1-/- mice present a reduction in the expression of the mature form of IL-1β during carrageenin-induced paw inflammation, these mice still present the residual production of active IL-1β, suggesting that alternative mechanisms might trigger the induction of mature IL-1β in this model. For instance, there is evidence that pro-IL-1β can be cleaved by other proteases in addition to caspase-1, including elastase, proteinase 3 matrix metalloprotease 9 (MMP9), which are produced by neutrophils recruited to sites of tissue damage [20–23]. In this context, we have recently shown that MMP9 mediates hypernociception that developed during antigen-induced arthritis, a model in which IL-1β also plays a role [24].
Besides peripheral participation in the development of inflammatory hypernociception, we could not disregard the fact that caspase-1 might be involved by playing a central role in the response. In fact, activation of caspase-1 in the spinal cord has been associated with an increase of central IL-1β production that promotes COX-2 dependent inflammatory hypernociception [13]. In the periphery, the pro-nociceptive effect of IL-1β was also mediated by cyclooxygenase-derived PGE2 because its effect was inhibited by treatment with indomethacin [6, 25]. Therefore, the observation that COX-2 expression and PGE2 production are reduced in casp1-/- mice challenged with carrageenin corroborates the importance of IL-1β in these processes. Contrary to these results, it was shown that although spinal glial-derived IL-1β is fundamental for the development of neuropathic pain after peripheral nerve injury, caspase-1 is not involved in this process [23]. It was clearly demonstrated that, in this model, MMP-9 and MMP-2 are the enzymes responsible for IL-1β maturation playing a central role in neuropathic pain induction [23].
One question that emerges from these results is how caspase-1 is activated during carrageenin-induced paw inflammation. Regarding the mechanisms that trigger caspase-1 activation in the inflammatory process, there is now a large body of recent evidence showing that they are dependent on the assembly of cytosolic multiprotein complexes known as inflammasomes [26, 27]. Inflammasomes are formed by self-oligomerising scaffold proteins belonging to the NOD-like receptor family. There are, at least, four different inflammasomes: NALP1/NLRP1, NALP3/NLRP3, IPAF/NLRC4 and the HIN-200 family member, AIM2 [26]. These molecules self-oligomerise after stimuli recognition and form high-molecular weight complexes that trigger caspase-1 autoactivation. Therefore, an interesting question is: which inflammasome is activated during carrageenin inflammation? In our knowledge, there is no study that addresses this issue. However, one can predict the involvement of the NALP3 inflammasome. This suggestion is based on the following indirect evidence: a) NALP3-containing inflammasomes that activate caspase-1 generally depend on stimulation of P2X7 [28]; b) P2X7 mediates carrageenin-induced inflammatory hypernociception [29, 30]; and c) P2X7 mediation of inflammatory hypernociception depends on stimulation of IL-1β because the antinociceptive effect of a selective P2X7 receptor antagonist is lost in IL-1 knockout mice [30]. Collectively, these data suggest that NALP3 is the inflammasome that triggers caspase-1 activation in the mediation of carrageenin-induced inflammatory hypernociception, yet other inflammasomes could be also involved. For instance, the NALP1 inflammasome is required for caspase-1 activation and mediates the complex regional pain syndrome that developed after tibia fracture in rats [18]. Therefore, additional studies using, for example, NALP3 null mice are required to solve this question.
In summary, the present study presents evidence that caspase-1 is involved in the genesis of inflammatory hypernociception. The participation of caspase-1 in this inflammatory symptom was not associated with the production of pro-inflammatory cytokines (TNFα, CXCL1/KC or IL-18) and recruitment of neutrophils, but was associated with the maturation of IL-1β in the inflammatory site. Caspase-1 seems to also be involved in the induction of COX-2 and consequently in the production of the directly-acting hypernociceptive mediator, PGE2. Together, these results added new information about the physiopathology of inflammatory pain. In conclusion, it is plausible to suggest that caspase-1 constitutes a real target to control inflammatory pain.
Methods
Animals
The experiments were performed on male C57BL/6 mice (wild type, WT, 20-25 g) and caspase-1 deficient mice (casp1-/-). Breeding pairs of mice with targeted disruption of the caspase-1 gene were back-crossed with C57BL/6 for 8 generations. BALB/C mice were used as a control when the experiment was conducted in IL-18 null mice (IL-18-/-). They were housed in the animal care facility of the School of Medicine of Ribeirao Preto and taken to the testing room at least one hour before the experiments. Food and water were available ad libitum. All behavioural tests were performed between 9:00 AM and 5:00 PM, and the animals were used only once. Animal care and handling procedures were in accordance with the guidelines of the International Association for the Study of Pain (IASP) on the use of animals in pain research. All efforts were made to minimise the number of animals used and their discomfort.
Drugs
The drugs used in this study were: prostaglandin E2 (PGE2) (from Sigma, St. Louis, MO), YVAD-CMK (Calbiochem, San Diego, CA, USA), TNFα, IL-1β and IL-1 receptor antagonist (IL-1ra) (NIBSC, South Mimms, Hertfordshire, U.K.), CXCL1/KC (PeproTech, Rocky Hill, NJ), and carrageenin (FMC, Philadelphia). A stock solution of PGE2 (1 μg/μL) was prepared in 10% ethanol, and dilutions were made in 0.9% NaCl (saline); the final concentration of ethanol was 1%. Other drugs were diluted in sterile saline.
Mechanical nociceptive paw test
Mechanical hypernociception was tested in mice as previously reported [31]. In a quiet room, mice were placed in acrylic cages (12 × 10 × 17 cm) with wire grid floors 15-30 min before the start of testing. The test consisted of evoking a hindpaw flexion reflex with a handheld force transducer (electronic aesthesiometer, IITC Life Science, Woodland Hills, CA) adapted with a 0.5 mm2 polypropylene tip. The investigator was trained to apply the tip perpendicularly to the central area of the plantar hindpaw with a gradual increase in pressure. The gradual increase in pressure was manually performed in blinded experiments. The upper limit pressure was 15 g. The end-point was characterised by the removal of the paw followed by clear flinching movements. After paw withdrawal, the intensity of the pressure was automatically recorded, and the final value for the response was obtained by averaging three measurements. The animals were tested before and after treatments. The results are expressed by the delta (Δ) withdrawal threshold (in g) calculated by subtracting the zero-time mean measurements from the mean measurements at the indicated times after drug or solvent (control) injections. The withdrawal threshold was 8.9 ± 0.2 g (mean ± S.E.M.; n = 30) before injection of the solvent or hypernociceptive agents.
Cytokine measurements
At indicated times after the injection of inflammatory stimuli, the animals were terminally anesthetised, and the skin tissues of the plantar region were removed from the injected and control paws (saline and naïve). The samples were triturated and homogenized in 500 μl of the appropriate buffer (phosphate-buffered saline containing 0.05% Tween 20, 0.1 mM phenylmethylsulphonyl fluoride, 0.1 mM benzethonium chloride, 10 mM EDTA and 20 kallikrein international units of aprotinin A) followed by a centrifugation of 10 min at 2000 g. The supernatants were used to determine the levels of TNF-α and CXCL1/KC as described previously [32] by enzyme-linked immunosorbent assays (ELISA). Briefly, microtiter plates were coated overnight at 4°C with an immunoaffinity-purified polyclonal sheep antibody against TNFα (2 μg/mL) or CXCL1/KC (1 μg/mL). After blocking the plates, recombinant murine TNFα or CXCL1/KC standards at various dilutions and the samples were added in duplicate and incubated overnight at 4°C. Rabbit biotinylated immunoaffinity-purified antibody anti- anti-TNFα (1:500) or CXCL1/KC (0.2 μg/mL) were added, followed by incubation at room temperature for 1 h. Finally, 50 μL of avidin-HRP (1:5000 dilution; DAKO A/S, Denmark) was added to each well, and after 30 min the plates were washed and the colour reagent OPD (200 μg/well; Sigma) was added. After 15 min, the reaction was stopped with 1 M H2SO4 and the optical density (O.D.) reading at 490 nm was taken. The results are expressed as picograms (pg) of each cytokine per paw.
Neutrophil migration to the plantar tissue
Neutrophil migration to the hind paw plantar tissues of mice was evaluated using a myeloperoxidase (MPO) kinetic-colorimetric assay as previously described [33, 34]. Samples of subcutaneous plantar tissue were collected in 50 mM K2HPO4 buffer (pH 6.0) containing 0.5% hexadecyltrimethylammonium bromide (HTAB) and kept at -80°C until use. Samples were homogenised using a Polytron (PT3100), centrifuged at 16,100 g for 4 min, and the resulting supernatant was assayed for MPO activity spectrophotometrically at 450 nm (Spectra max), with three readings in 1 min. The MPO activity of samples was compared to a standard curve of neutrophils. Briefly, 10 μL of sample was mixed with 200 μL of 50 mM phosphate buffer, pH 6.0, containing 0.167 mg/mL O-dianisidine dihydrochloride and 0.0005% hydrogen peroxide. The results are presented as MPO activity (number of neutrophils per mg of tissue).
RNA extraction and Real-Time PCR
At 1.5 h after intraplantar (i.pl.) injection of carrageenin or saline, mice were terminally anesthetised, and skin tissues were removed from the plantar region of paws. The samples were homogenised in 1 mL of TRIzol (Invitrogen, Carlsbad, CA) and total RNA was extracted following the manufacturer's instructions. The purity of total RNA was measured with a spectrophotometer and the wavelength absorption ratio (260/280 nm) was between 1.8 and 2.0 for all preparations. Reverse transcription of total RNA to cDNA was carried out with a reverse transcription reaction (Superscript II, Gibco Life Technologies, Grand Island, NY, USA). Real-time PCR was performed using primers specific for the mouse gene pro-IL-1β and for the mouse housekeeping gene hypoxanthine guanine phosphoribosyl transferase (Hprt). Reactions were conducted on the ABI Prism 7500 Sequence Detection System using the SYBR-green fluorescence system (Applied Biosystems, Warrington, UK). The data were analysed with the 2−ΔΔCt method as described previously [35] and they are expressed relative to samples collected in the saline group of animals. Primer pairs for mouse Hprt and pro-IL-1β were as follows:
pro-IL-1β fwd: 5'-GCTGCTTCCAAACCTTTGAC-3'
pro-IL-1β rev: 5'-AGCTTCTCCACAGCCACAAT-3'
Hprt fwd: 5'-GCCCCAAAATGGTTAAGGTT- 3'
Hprt rev: 5'-CAAGGGCATATCCAACAACA- 3'
Western blot analysis
At 3 h after i.pl. injection of carrageenin or saline, mice were terminally anesthetised, and skin tissues were removed from the plantar region of paws. The samples were homogenised and the expression of cyclooxygenase (COX-2; ~72 kDa) or the mature form of IL-1β (~19 kDa) were evaluated using western blot analyses. Briefly, samples were homogenised in a lysis buffer containing a mixture of proteinase inhibitors (Tris-HCl 50 mM, pH 7.4; NP-40 1%; Na-deoxycholate 0.25%; NaCl 150 mM; EDTA 1 mM; PMSF 1 mM; Aprotinin, leupeptin and pepstatin 1 μg/mL each). Proteins were separated by SDS-polyacrylamide gel electrophoresis (SDS-PAGE-12%) and transblotted onto nitrocellulose membranes (Amersham Pharmacia Biotech, Little Chalfont, UK). The membranes were blocked with 7% dry milk (overnight) and incubated overnight at 4°C with a rabbit polyclonal antibody against COX-2 (1:400; Cayman, Ann Arbor, Michigan, USA) or IL-1β (1:200, Santa Cruz, CA, USA). After these procedures, the membranes were washed and then incubated for 1 h at room temperature with an HRP-conjugated secondary antibody (1:20000; Jackson ImmunoResearch, PA, USA). The blots were visualised in ECL solution (Amersham Pharmacia Biotech) for 2 min and exposed onto sheets of Hyperfilm (Amersham Pharmacia Biotech) for 2-20 min. A β-actin (1:2000; AbCam, Cambridge, MA, USA) antibody was used for loading controls. A total of ten western blot runs were performed and transferred to eight nitrocellulose membranes with proteins of the saline group and carrageenin injection group in WT and casp-1-/- mice. Films were scanned into Image Quant 5.2 for analysis. A computer-based imaging system (Gel-Pro Analyzer) was used to measure the intensity of the optical density of the ~70 kDa and ~19 kDa bands that represent the molecular weight of COX-2 and the mature form of IL-1β proteins.
Measurement of PGE2 in paw skin
The plantar tissues were collected 3 h after intraplantar injection of carrageenin (100 μg/paw) or saline as described above. This time point is the peak of carrageenin-induced PGE2 production in the mice paw (data not shown). The paws were injected with indomethacin (50 μg/paw) 10 min before tissue retrieval to block PGE2 production during tissue processing. The PGE2 was extracted from plantar tissue and determined by radioimmunoassay [7]. Briefly, the plantar tissue samples were homogenized in a mixture of 3.0 ml of extraction solvent (isopropanol/ethyl acetate/0.1 N HCl, 3:3:1) and 3.0 ml of distilled water. Also, the solution contained 20 μg/ml of indomethacin. Homogenates were centrifuged at 1,500 g for 10 min at 4°C. The organic phase was aspirated and evaporated to dryness in a centrifugal evaporator. The pellet was reconstituted in 500 μl of 0.1 M phosphate buffer (pH 7.4) containing 0.8% sodium azide and 0.1% gelatin. Concentration of PGE2 in these samples was then measured by RIA by using a commercially available kit. The results are expressed as picograms of PGE2 per paw.
Paw oedema test
The volume of the mice paw was measured with a plesthismometer (Ugo Basil, Italy) before (Vo) the intraplantar stimulus with carrageenan and 3 h after (VT), as described previously [34]. The amount of paw swelling was determined for each mouse and the difference between VT and Vo was taken as the oedema value (oedema mm3/paw).
Statistical analysis
All results are presented as means ± S.E.M. The experiments were repeated at least twice. The "n" in the legends refers to the number of mice used in the experimental group of each experiment. The differences between the experimental groups were compared by ANOVA (one-way) and individual comparisons were subsequently made with Tukey's post hoc test. The level of significance was set at P < 0.05.
Abbreviations
- KC/CXCL1:
-
keratinocyte-derived chemokine
- TNF:
-
tumour necrosis factor
- TNFR:
-
tumour necrosis factor receptor
- PGE2 :
-
prostaglandin E2: IL, interleukin
- casp1-/-:
-
caspase-1-deficient mice
- i.pl.:
-
intraplantar
- MPO:
-
myeloperoxidase
- Hprt:
-
hypoxanthine guanine phosphoribosyl transferase
- WT:
-
wild type
- COX-2:
-
cyclooxygenase-2
- IL-1ra:
-
IL-1 receptor antagonist
- MMP:
-
matrix metalloprotease.
References
Cunha TM, Verri WA Jr, Poole S, Parada CA, Cunha FQ, Ferreira SH: Pain Facilitation by Proinflammatory Cytokine Actions at Peripheral Nerve Terminals. In Immune and Glial Regulation of Pain. Edited by: Sorkin L, DeLeo J, Watkins LR. Seattle: IASP PRESS; 2007:67–83.
Ferreira SH, Nakamura M: I - Prostaglandin hyperalgesia, a cAMP/Ca2+ dependent process. Prostaglandins 1979, 18: 179–190. 10.1016/0090-6980(79)90103-5
Khasar SG, Mccarter G, Levine JD: Epinephrine produces a beta-adrenergic receptor-mediated mechanical hyperalgesia and in vitro sensitization of rat nociceptors. J Neurophysiol 1999, 81: 1104–1112.
Nakamura M, Ferreira SH: A peripheral sympathetic component in inflammatory hyperalgesia. Eur J Pharmacol 1987, 135: 145–153.5. 10.1016/0014-2999(87)90606-6
Verri WA Jr, Cunha TM, Parada CA, Poole S, Cunha FQ, Ferreira SH: Hypernociceptive role of cytokines an d chemokines: targets for analgesic drug development? Pharmacol Ther 2006, 112: 116–38.6. 10.1016/j.pharmthera.2006.04.001
Cunha TM, Verri WA Jr, Silva JS, Poole S, Cunha FQ, Ferreira SH: A cascade of cytokines mediates mechanical inflammatory hypernociception in mice. Proc Natl Acad Sci USA 2005, 102: 1755–1760. 10.1073/pnas.0409225102
Cunha TM, Verri WA Jr, Schivo IR, Napimoga MH, Parada CA, Poole S, et al.: Crucial role of neutrophils in the development of mechanical inflammatory hypernociception. J Leukoc Biol 2008, 83: 824–832. 10.1189/jlb.0907654
Franchi L, Eigenbrod T, Munoz-Planillo R, Nunez G: The inflammasome: a caspase-1-activation platform that regulates immune responses and disease pathogenesis. Nat Immunol 2009, 10: 241–247. 10.1038/ni.1703
Kuida K, Lippke JA, Ku G, Harding MW, Livingston DJ, Su MS, et al.: Altered cytokine export and apoptosis in mice deficient in interleukin-1 beta converting enzyme. Science 1995, 267: 2000–2003. 10.1126/science.7535475
Li P, Allen H, Banerjee S, Seshadri T: Characterization of mice deficient in interleukin-1 beta converting enzyme. J Cell Biochem 1997, 64: 27–32. 10.1002/(SICI)1097-4644(199701)64:1<27::AID-JCB5>3.0.CO;2-1
Wannamaker W, Davies R, Namchuk M, Pollard J, Ford P, Ku G, et al.: (S)-1-((S)-2-{[1-(4 -amino- 3-chloro-phenyl)-methanoyl]-amino}-3,3-dimethyl- butanoyl)-pyrrolidine-2-carboxylic acid ((2R,3S)-2-ethoxy-5-oxo-tetrahydro-furan-3-yl)-amide (VX-765), an orally available selective interleukin (IL)-converting enzyme/caspase-1 inhibitor, exhibits potent anti-inflammatory activities by inhibiting the release of IL-1beta and IL-18. J Pharmacol Exp Ther 2007, 321: 509–16. 10.1124/jpet.106.111344
Elford PR, Heng R, Revesz L, Mackenzie AR: Reduction of inflammation and pyrexia in the rat by oral administration of SDZ 224–015, an inhibitor of the interleukin-1 beta converting enzyme. Br J Pharmacol 1995, 115: 601–606.
Lee KM, Kang BS, Lee HL, Son SJ, Hwang SH, Kim DS, et al.: Spinal NF-kB activation induces COX-2 upregulation and contributes to inflammatory pain hypersensitivity. Eur J Neurosci 2004, 19: 3375–3381. 10.1111/j.0953-816X.2004.03441.x
Ghayur T, Banerjee S, Hugunin M, Butler D, Herzog L, Carter A, et al.: Caspase-1 processes IFN-gamma-inducing factor and regulates LPS-induced IFN-gamma production. Nature 1997, 386: 619–623. 10.1038/386619a0
Dinarello CA: Interleukin-1 beta, interleukin-18, and the interleukin-1 beta converting enzyme. Ann N Y Acad Sci 1998, 856: 1–11. 10.1111/j.1749-6632.1998.tb08307.x
Fantuzzi G, Dinarello CA: Interleukin-18 and interleukin-1 beta: two cytokine substrates for ICE (caspase-1). J Clin Immunol 1999, 19: 1–11. 10.1023/A:1020506300324
Luthi AU, Cullen SP, Mcneela EA, Duriez PJ, Afonina IS, Sheridan C, et al.: Suppression of interleukin-33 bioactivity through proteolysis by apoptotic caspases. Immunity 2009, 31: 84–98. 10.1016/j.immuni.2009.05.007
Li WW, Guo TZ, Liang D, Shi X, Wei T, Kingery WS, et al.: The NALP1 inflammasome controls cytokine production and nociception in a rat fracture model of complex regional pain syndrome. Pain 2009, 147: 277–286. 10.1016/j.pain.2009.09.032
Verri WA Jr, Cunha TM, Parada CA, Poole S, Liew FY, Ferreira SH, et al.: Antigen-induced inflammatory mechanical hypernociception in mice is mediated by IL-18. Brain Behav Immun 2007, 21: 535–543. 10.1016/j.bbi.2006.11.005
Joosten LA, Netea MG, Fantuzzi G, Koenders MI, Helsen MM, Sparrer H, et al.: Inflammatory arthritis in caspase 1 gene-deficient mice: contribution of proteinase 3 to caspase 1-independent production of bioactive interleukin-1beta. Arthritis Rheum 2009, 60: 3651–3662. 10.1002/art.25006
Guma M, Ronacher L, Liu-Bryan R, Takai S, Karin M, Corr M: Caspase 1-independent activation of interleukin-1beta in neutrophil-predominant inflammation. Arthritis Rheum 2009, 60: 3642–3650. 10.1002/art.24959
Greten FR, Arkan MC, Bollrath J, Hsu LC, Goode J, Miething C, et al.: NF-kappaB is a negative regulator of IL-1beta secretion as revealed by genetic and pharmacological inhibition of IKKbeta. Cell 2007, 130: 918–931. 10.1016/j.cell.2007.07.009
Kawasaki Y, Xu ZZ, Wang X, Park JY, Zhuang ZY, Tan PH, et al.: Distinct roles of matrix metalloproteases in the early- and late-phase development of neuropathic pain. Nat Med 2008, 14: 331–336. 10.1038/nm1723
Pinto LG, Cunha TM, Vieira SM, Lemos HP, Verri WA, Cunha FQ, et al.: IL-17 mediates articular hypernociception in antigen-induced arthritis in mice. Pain 2010, 148: 247–256. 10.1016/j.pain.2009.11.006
Ferreira SH, Lorenzetti BB, Bristow AF, Poole S: Interleukin-1 beta as a potent hyperalgesic agent antagonized by a tripeptide analogue. Nature 1988, 334: 698–700. 10.1038/334698a0
Schroder K, Tschopp J: The inflammasomes. Cell 2010, 140: 821–32. 10.1016/j.cell.2010.01.040
Lamkanfi M, Dixit VM: The inflammasomes. PLoS Pathog 2009, 5: e1000510. 10.1371/journal.ppat.1000510
Mariathasan S, Weiss DS, Newton K, Mcbride J, O'Rourke K, Roose-Girma M, et al.: Cryopyrin activates the inflammasome in response to toxins and ATP. Nature 2006, 440: 228–232. 10.1038/nature04515
Broom DC, Matson DJ, Bradshaw E, Buck ME, Meade R, Coombs S, et al.: Characterization of N-(adamantan-1-ylmethyl)-5-[(3R-amino-pyrrolidin-1-yl)methyl]-2-chloro-ben zamide, a P2X7 antagonist in animal models of pain and inflammation. J Pharmacol Exp Ther 2008, 327: 620–633. 10.1124/jpet.108.141853
Honore P, Donnelly-Roberts D, Namovic MT, Hsieh G, Zhu CZ, Mikusa JP, et al.: A-740003 [N-(1-{[(cyanoimino)(5-quinolinylamino) methyl]amino}-2,2-dimethylpropyl)-2-(3,4-dimethoxyphenyl)acetamide], a novel and selective P2X7 receptor antagonist, dose-dependently reduces neuropathic pain in the rat. J Pharmacol Exp Ther 2006, 319: 1376–1385. 10.1124/jpet.106.111559
Cunha TM, Verri WA Jr, Vivancos GG, Moreira IF, Reis S, Parada CA, et al.: An electronic pressure-meter nociception paw test for mice. Braz J Med Biol Res 2004, 37: 401–407. 10.1590/S0100-879X2004000300018
Cunha TM, Verri WA Jr, Fukada SY, Guerrero AT, Santodomingo-Garzon T, Poole S, et al.: TNF-alpha and IL-1beta mediate inflammatory hypernociception in mice triggered by B1 but not B2 kinin receptor. Eur J Pharmacol 2007, 573: 221–229. 10.1016/j.ejphar.2007.07.007
Cunha TM, Dal-secco D, Verri WA Jr, Guerrero AT, Souza GR, Vieira SM, et al.: Dual role of hydrogen sulfide in mechanical inflammatory hypernociception. Eur J Pharmacol 2008, 590: 127–135. 10.1016/j.ejphar.2008.05.048
Valerio DA, Cunha TM, Arakawa NS, Lemos HP, DA Costa FB, Parada CA, et al.: Anti-inflammatory and analgesic effects of the sesquiterpene lactone budlein A in mice: inhibition of cytokine production-dependent mechanism. Eur J Pharmacol 2007, 562: 155–163. 10.1016/j.ejphar.2007.01.029
Livak KJ, Schmittgen TD: Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001, 25: 402–408. 10.1006/meth.2001.1262
Acknowledgements
The authors wish to express their appreciation to Ieda Regina dos Santos Schivo, Sérgio Roberto Rosa, Fabiola Mestriner and Giuliana Bertozi Francisco for excellent technical assistance. This work was supported by grants from FAPESP and CNPq.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
TMC, LGP, GRS, ATG and WAV carried out the behavioral studies, TMC, JT, SMV and FS carried out molecular and biochemical studies, TMC, DSZ, SHF and FQC conceived of and designed the study and TMC wrote the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Cunha, T.M., Talbot, J., Pinto, L.G. et al. Caspase-1 is involved in the genesis of inflammatory hypernociception by contributing to peripheral IL-1β maturation. Mol Pain 6, 63 (2010). https://doi.org/10.1186/1744-8069-6-63
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1744-8069-6-63