Abstract
Background
Hydrogen sulphide (H2S) is a gaseous neuro-mediator that exerts analgesic effects in rodent models of visceral pain by activating KATP channels. A body of evidence support the notion that KATP channels interact with endogenous opioids. Whether H2S-induced analgesia involves opioid receptors is unknown.
Methods
The perception of painful sensation induced by colorectal distension (CRD) in conscious rats was measured by assessing the abdominal withdrawal reflex. The contribution of opioid receptors to H2S-induced analgesia was investigated by administering rats with selective μ, κ and δ opioid receptor antagonists and antisenses. To investigate whether H2S causes μ opioid receptor (MOR) transactivation, the neuronal like cells SKNMCs were challenged with H2S in the presence of MOR agonist (DAMGO) or antagonist (CTAP). MOR activation and phosphorylation, its association to β arrestin and internalization were measured.
Results
H2S exerted a potent analgesic effects on CRD-induced pain. H2S-induced analgesia required the activation of the opioid system. By pharmacological and molecular analyses, a robust inhibition of H2S-induced analgesia was observed in response to central administration of CTAP and MOR antisense, while κ and δ receptors were less involved. H2S caused MOR transactivation and internalization in SKNMCs by a mechanism that required AKT phosphorylation. MOR transactivation was inhibited by LY294002, a PI3K inhibitor, and glibenclamide, a KATP channels blocker.
Conclusions
This study provides pharmacological and molecular evidence that antinociception exerted by H2S in a rodent model of visceral pain is modulated by the transactivation of MOR. This observation provides support for development of new pharmacological approaches to visceral pain.
Similar content being viewed by others
Introduction
Visceral pain is the most common sign of acute and chronic gastrointestinal, pelvic and genitourinary diseases. As one of the most common causes of persistent disability, visceral pain represents a frequent reason for patients to seek medical treatment. Despite multiple therapeutic approaches, the treatment of visceral pain remains a significant challenge.
A complex network of signaling molecules mediates perception of visceral pain [1]. Hydrogen sulphide (H2S) is a gaseous neuromodulator generated from L-cysteine by the activity of two pyrodoxal-5'-phosphate-dependent enzymes, the cystathionine γ-lyase (CSE) and the cystathionine β-synthase (CBS) [2–5], that exerts regulatory activities in the gastrointestinal tract [1, 4]. In the central nervous system H2S mediates the induction of hippocampal long-term potentiation [6–8] and the release of the corticotropin releasing hormone from the hypothalamus [9], enhances NMDA receptor-mediated responses [8] and protects against peroxynitrite-induced neuronal toxicity [10]. ATP-sensitive potassium (KATP) channels have been identified as important mediators of several effects exerted by H2S [2, 3, 10]. Thus, glibenclamide, a KATP channels blocker, attenuates analgesic effect of H2S in a model of visceral pain induced by colorectal distension (CRD) in healthy and post-colitis, allodynic rats [11, 12].
Opioid receptors are G protein-coupled receptors (GPCRs) and the main receptors involved in the modulation of pain in mammals [13, 14]. The principal opioid receptor subtypes, μ (MOR), δ (DOR) and κ (KOR), are all expressed in the spinal cord and in the brain contributing to the modulation of nociceptive transmission. In addition, the μ and κ opioid receptors are also expressed in the enteric nervous system. MOR is the preferred receptor for potent analgesics with high potential for abuse, such as morphine [14]. Endogenous opioids, including enkephalins, endorphins and opiates like etorphine, induce rapid μ receptor endocytosis in neurons and transfected cells [15, 16], a process called internalization that is widely used as a marker of MOR activation [17, 18].
Opioid receptors and KATP channels converge in regulating release of neurotransmitters, smooth muscle contractions and neuronal excitability with both signaling pathways being effective in attenuating perception of visceral painful sensations in animal models and patients [19, 20]. Whether H2S signaling integrates with the opioid system, however, is still unknown.
In the present study we provide evidence that antinociception exerted by H2S in a rodent model of visceral pain is selectively modulated by the intervention of μ opioid receptors. By in vitro studies we demonstrated that a previously unrecognized neuronal circuit with H2S-activated KATP channels transactivating the μ opioid receptor supports the analgesic activities of H2S. These results identify new pharmacological targets in the treatment of chronic visceral pain.
Results
H2S inhibits CRD-induced nociception
In all experimental settings two sequential distension-effect curves were constructed. The first distension-effect curve was used as a control, while the second was constructed in response to saline or specified drug. In all experiments animals were awake and no changes in the consciousness state were produced by Na2S administration.
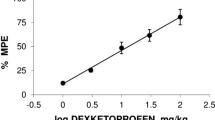
CRD (0.4-1.6 ml water) elicited a volume-dependent increase of the AWR scores which was rapid in onset, persisted for the duration of the distension period (Figure 1, panel A) and returned to the baseline immediately after the distension was stopped. In the fed animals CRD elicited a similar pattern of response (Figure 1, panel B). Injected intraperitoneally (i.p.) at the dose of 100 μMol/kg, Na2S decreased the AWR score (Figure 1, panel C, p < 0.05 versus CRD alone) and determined a significant increase of colorectal compliance (data not shown) indicating that H2S induced a myorelaxant action on colonic smooth muscle cells. The antinociceptive effect of Na2S was confirmed by analysis of spinal cFos mRNA expression. Thus, Na2S administration abrogated cFos mRNA expression induced in the spinal cord by CRD (Figure 1, panel D, p < 0.05 versus control).
Na 2 S induces antinociception. CRD induces a volume-dependent increase of the AWR score in both fasting and fed rats (panels A and B respectively) and Na2S (100 μMol/kg i.p.) causes a significant reduction of visceral sensitivity and pain (panel C). Data are mean ± SEM of 5 rats. *p < 0.05 versus CRD. CRD induces the increase of spinal cFos expression that is downregulated by Na2S (panel D). Data are mean ± SEM of 5 rats. *p < 0.05 versus control.
μ opioid receptors antagonism inhibits the H2S-induced antinociception
The antinociceptive effect of Na2S on CRD-induced pain was studied by pre-treating animals with selective opioid receptor antagonists. As illustrated in Figure 2, while the DOR antagonist NTI, and the KOR antagonist GNTI injected intracerebroventricularly (i.c.v.) had no effect on Na2S-induced antinociception (Figure 2, panels A and B respectively, p < 0.05 versus CRD), the selective MOR antagonist CTAP injected i.c.v. reverted analgesia induced by Na2S (Figure 2, panel C) without interfering with its myorelaxant activity (data not shown). Administering rats with NTI, GNTI and CTAP alone had no effect on CRD-induced nociception (data not shown). To confirm the above mentioned results by another method, we injected rats i.c.v. with oligodeoxynucleotide antisenses directed against each specific opioid receptor subtype. While pre-treating rats with mismatched antisenses failed to modulate Na2S-induced analgesia (Figure 3, panel A, p < 0.05 versus CRD), the analgesic activity of H2S on CRD-induced pain was abrogated by pre-treating animals with δ and μ opioid receptor antisenses (Figures 3, panels B and D respectively). In contrast, no effect was observed with the κ opioid receptor antisense (Figure 3, panel C, p < 0.05 versus CRD). All antisenses had no effect on colonic myorelaxation induced by Na2S (data not shown). Finally, administering rats with antisenses alone had no effect on nociception induced by CRD (data not shown).
CTAP reverses the Na 2 S-induced antinociception. Pre-treating rats with the selective μ opioid receptor antagonist CTAP (0.09 mg/kg i.c.v. thirty minutes before Na2S; panel C) abrogates the antinociceptive effect of Na2S (100 μMol/kg i.p.). In contrast, the selective δ opioid receptor antagonist NTI (4 μg/kg i.c.v. five minutes before Na2S, panel A) and the selective κ opioid receptor antagonist GNTI (0.08 μmg/kg i.c.v. three days before Na2S, panel B) do not inhibit the analgesic effect of Na2S, indicating that δ and κ opioid receptors have no effects on Na2S-induced antinociception. Data are mean ± SEM of 5 rats. *p < 0.05 versus CRD.
The selective antisense oligodeoxynucleotide probes against DOR and MOR reverse the Na 2 S-induced antinociception. Pre-treating rats with both the mismatched antisense oligodeoxynucleotides (panel A) and the κ opioid receptor antisense oligodeoxynucleotides (panel C) does not modify the H2S-induced decrease of the AWR score, confirming that KOR does not cause any change on the Na2S-induced analgesia. In contrast, oligodeoxynucleotide probes against DOR and MOR reverse the antinociception caused by Na2S (panel B and D respectively). Data are mean ± SEM of 5 rats. *p < 0.05 versus CRD.
To determine whether the analgesic effect of Na2S was modulated by KATP channels, we performed an experiment by using the KATP channel antagonist glibenclamide. The antinociceptive effect of Na2S (Figure 4, panel A) was reverted by blocking the KATP channels with glibenclamide (Figure 4, panel B), while treating rats with glibenclamide alone failed to modulate nociception induced by CRD (data not shown).
Glibenclamide reverses the Na 2 S-induced antinociception. In a different experiment we have analyzed the role of the KATP channels on the H2S-induced analgesia (panel A). Pre-treating rats with the KATP channels selective blocker glibenclamide (2.8 μmol/kg i.v.) completely reverses the Na2S-induced analgesia (panel B) without any effects on the change of the colonic compliance induced by Na2S. Data are mean ± SEM of 5 rats. *p < 0.05 versus CRD.
H2S induces MOR activation and internalization
To investigate the mechanisms by which Na2S activates MOR, experiments were carried out in SKNMC cells, a neuron-like cell line that expresses functional μ opiod receptors. Agonist-induced activation of MOR results in conformational changes of the extracellular portion of the receptor that unmasks a specific epitope near to the N-terminus. By using a specific antibody that target this epitope, we have investigated whether Na2S causes MOR activation. As illustrated in Figure 5, panels A and B, MOR activation was detected in cells exposed to either the μ receptor-selective enkephalin analog DAMGO and Na2S, indicating that exposure to Na2S induced an activity-dependent conformational change of the N-terminal region of the MOR. Further, exposure of SKNMCs to Na2S caused the direct phosphorylation of MOR in the Ser(377) (Figure 5, panel C), a measure of the receptor activation, and exposure of cells to DAMGO also caused a robust induction of MOR phosphorylation in the serine residue, thought that the kinetic of the two effects was different (Figure 5, panel C). As expression of total MOR protein did not change (Figure 5, panel D), these results demonstrated that exposure of SKNMCs to Na2S induced a rapid and persistent phosphorylation of the μ opioid receptor in a site that is functionally linked to its activation.
Na 2 S induces MOR activation and phosphorylation, the recruitment of β arrestin and MOR internalization. Both DAMGO (1 μM) and Na2S (50 μM) induce MOR activation (panel A and B respectively). Treating SKNMCs with both DAMGO and Na2S results in MOR phosphorylation that is time-dependent. DAMGO induces MOR phosphorylation at Ser(377) that is maximal at 30 minutes and, similarly, H2S induces MOR phosphorylation that peaks at 3-6 minutes and persists until 30 minutes (panel C). The total DAMGO-induced and H2S-induced MOR phosphorylation is unchanged within the duration of the experiment (panel D). Co-immunoprecipitation experiments demonstrate that DAMGO induces the rapid complex between MOR and β arrestin with the peak at 5-15 minutes and, similarly, H2S induces the co-immunoprecipitation of MOR and β arrestin that peaked at 30 minutes (panel E), indicating that H2S induces the interaction between β arrestin and MOR. At the cell membrane fractioning experiments, DAMGO (1 μM) causes the disappearance of MOR from the plasma membrane fraction at 5 minutes and this effect is maximal at 60 minutes. At the same time there is a progressive increment of MOR presence in the cytoplasmatic fraction (panel F). After Na2S (50 μM), MOR disappears from the plasma membrane fraction at 30 minutes with the maximal effect at 60 minutes and, in contemporary, it passes into the cytoplasmatic fraction (panel G). At the confocal microscopy SKNMCs exhibit MOR immunoreactivity predominantly localized at the cell surface in nonstimulated condition (panel H) and it translocates to cytoplasm after activation with DAMGO (panel I), which is known to induce MOR internalization. Na2S induces a massive translocation of MOR from plasma membrane into the cytoplasm in most neurons (panel L). Data are representative of at least 3 experiments. *p < 0.05 vs control.
Following its activation, MOR is rapidly internalized after its recruitment into a multiprotein complex with β arrestin. By co-immunoprecipitation experiments (Figure 5, panel E) we found that exposure of SKNMCs to DAMGO and Na2S caused a robust induction of MOR association with β arrestin. By membrane fraction technique we found that DAMGO caused MOR internalization as shown by its disappearance from the plasma membrane and relocation into the cytosol fraction as early as 5 minutes of exposure (Figure 5, panel F). A similar pattern was observed in response to Na2S, thought the time course was slightly different (Figure 5, panel G). These findings were confirmed by confocal microscopy analysis (Figure 5, panels H-L). Thus, while resting SKNMCs exhibited MOR immunoreactivity predominantly at the cell surface (Figure 5, panel H), a massive translocation of receptor to the cytosol occurred in cells exposed to DAMGO (Figure 5, panel I) and Na2S (Figure 5, panel L).
To further investigate whether activation of MOR by Na2S occurs by direct receptor activation or is mediated by receptor transactivation, we challenged SKNMCs with the highly selective μ receptor antagonist CTAP. Results from these experiments demonstrate that while MOR activation induced by DAMGO was abrogated by CTAP, the antagonist had no effects on MOR activation induced by Na2S (Figure 6, panel A). Similarly, CTAP was effective in preventing MOR internalization induced by DAMGO but only partially prevented cytosolic MOR translocation induced by Na2S treatment (Figure 6, panel B).
CTAP only partially inhibits the Na 2 S-induced MOR internalization. SKNMCs are stimulated with DAMGO (1 μM) or Na2S (50 μM) in presence or in absence of CTAP (1 μM) and the effects on MOR activation and internalization are detected. CTAP inhibits the MOR activation induced by DAMGO while it has no effect on that induced by Na2S (panel A). CTAP blocks the DAMGO-induced MOR internalization but, in contrast, it only partially inhibits the Na2S-induced MOR internalization (panel B). Data are representative of at least 3 experiments. *p < 0.05 vs control, **p < 0.05 vs DAMGO alone.
H2S induces PI3K/AKT activation
Because H2S induces AKT phosphorylation [21] and AKT is also activated in response to MOR activation by DAMGO [22], we have investigated whether Na2S induces AKT phosphorylation in SKNMCs. Results of these experiments demonstrated that both DAMGO and Na2S caused a long-lasting phosphorylation of AKT in Threonine 308 (Thre308), a marker of AKT activation (Figure 7, panel A). The induction of AKT phosphorylation by Na2S was time dependent as further confirmed by an immunoassay that specifically detects AKT phosphorylation on Serine 473 (Ser473) (Figure 7, panel B). AKT phosphorylation induced by DAMGO was reversed by CTAP (Figure 7C). However, CTAP failed to inhibit AKT phosphorylation induced by Na2S (Figure 7, panel C and D, p < 0.05 versus control).
Na 2 S induces AKT phosphorylation. Exposure to both DAMGO (1 μM) and Na2S (50 μM) causes AKT phosphorylation on Threonine 308 as detected by Western blot analysis (panel A). Moreover, Na2S induces AKT phosphorylation on Ser(473) as detected by phospho AKT assay (panel B). CTAP inhibits the DAMGO-induced AKT phosphorylation on Thre(308) (panel C), while it does not prevent that induced by Na2S on Thre(308) and Ser(473) (panels C and D). Data are representative of at least 3 experiments. Data on AKT phosphorylation are mean ± SE of 5 experiments. *p < 0.05 vs control.
To investigate the role of the PI3K/AKT pathway in Na2S-induced MOR internalization, SKNMCs were pre-treated with the selective PI3K inhibitor LY294002 (50 μM). LY294002 had no effect on DAMGO-induced MOR internalization (Figure 8, panel A), but prevented MOR internalization induced by Na2S (Figure 8, panel B). Moreover, LY294002 abrogated AKT phosphorylation induced by Na2S (Figure 8, panel C).
LY294002 inhibits the Na 2 S-induced MOR internalization and AKT phosphorylation. The selective PI3K inhibitor LY294002 has no effects on DAMGO-induced MOR internalization (panel A), while it blocks that induced by Na2S (panel B). Furthermore, LY294002 inhibits the AKT phosphorylation induced by Na2S on Ser(473) (panel C). Data are representative of at least 3 experiments. Data on AKT phosphorylation are mean ± SE of 5 experiments. *p < 0.05 vs control.
SKNMCs express KATP channels subunits: glibenclamide inhibits MOR activation and AKT phosphorylation
Because glibenclamide abrogates analgesia induced by Na2S suggesting the involvement of KATP channels, we have investigated whether SKNMCs express functional KATP channels. By RT-PCR we found that both the Kir6.2 and SUR1 subunits were expressed in the SKNMCs (Figure 9, panels A and B respectively) and by antagonism experiments we demonstrated that these channels were functionally active because glibenclamide (1 μM) inhibited MOR activation (Figure 9, panel C), MOR internalization (Figure 9, panel D) and AKT phosphorylation (Figure 9, panel E) induced by Na2S.
Glibenclamide inhibits Na 2 S-induced MOR activation and internalization and AKT phosphorylation. Qualitative PCR (panel A) and Quantitative Real-Time PCR (panel B) showing the expression of Kir6.2 and SUR1 in HepG2 (positive control) demonstrate that SKNMCs express both the KATP channels subunits Kir6.2 and SUR1. SKNMCs are stimulated with Na2S (50 μM) in presence or in absence of glibenclamide (1 μM) for 60 minutes. Glibenclamide prevents the Na2S-induced MOR activation (panel C) and internalization (panel D), while it has no effect on MOR internalization induced by DAMGO (panel D). Finally, glibenclamide inhibits AKT phosphorylation induced by Na2S, as assessed by phospho-immunoassay (panel F). Data are representative of at least 3 experiments. Data on AKT phosphorylation are mean ± SE of 5 experiments. *p < 0.05 vs control; **p < 0.05 vs DAMGO or Na2S alone.
Discussion
In this study we have demonstrated that H2S induces μ opioid-dependent analgesia in a rodent models of visceral pain. Moreover, in a supplementary experiment, we have demonstrated that, in contrast to what previously reported on the effect of meal on visceral perception in humans [23–25], CRD induces a similar painful response in both fasting and fed animals, indicating that meal has no influence on visceral perception in this experimental setting. However, more experiments are needed to clarify this particular issue.
Several mechanisms might explain the antinociceptive effect of H2S. First, a bluntness of sensorial functions that mimics a pain-free condition is unlikely because we did not observe any change in the consciousness of the rats during these studies. Second, as H2S causes a relaxation of smooth muscle cells, H2S could simply act as myorelaxant agent. However, this explanation seems unlikely, given that we have previously demonstrated that H2S inhibited CRD-induced nociception at doses that did not modify the colorectal compliance [11]. A third, more likely explanation would be that the antinociceptive effect of H2S is mediated by a direct inhibitory activity on colorectal afferent pathways. Consistent with this view, we found that administration of H2S decreased spinal cord expression of cFos mRNA.
The widespread occurrence of the opioid receptors indicates that opioids have the potential for affecting multiple systems, including nervous, hormonal and immunological systems. Opioid receptors have specific pharmacological profiles and physiological functions, maintain a certain degree of selectivity for various opioid ligands, and display unique patterns of expression in the nervous system, even though there is overlap in their binding affinity, distribution and function [26, 27]. Agonists of μ opioid receptors produce analgesia, affect mood and rewarding behavior and alter respiratory, cardiovascular, gastrointestinal and neuroendocrine functions [27]. While the actions of μ opioid agonists are invariably analgesic, those of κ agonists can be either analgesic or antianalgesic, the last effect being mediated by a functional antagonism on the action of μ receptor agonists. δ opioid receptor agonists also are potent analgesics in animals and, in isolated cases, have proved useful in human beings [27]. The main barrier to the clinical use of δ agonists is that the most available agents are peptides that do not cross the blood-brain barrier, thus requiring intraspinal administration. The ability to elucidate the roles of opioid receptor subtypes in the mediation of analgesia was first enhanced by the development of selective opioid receptor subtype antagonists direct against μ, κ and δ receptors and subsequently by the use of antisense probes to establish the relationship of the cloned receptors to opioid actions using sequences complementary to regions of specific exons of mRNA to down-regulate opioid receptor proteins.
In the present study we described for the first time that the analgesic effects of H2S is reverted by central opioid antagonism. In particular, the selective μ antagonist CTAP, centrally administered, inhibits the H2S-induced analgesia while the selective κ and δ receptor antagonists have no effect. Moreover, when the selective, centrally administered antisense olygodeoxynucleotides have been used, the antisense oligodeoxynucleotides direct against μ receptors confirm the pharmacological data, suggesting that the μ opioid receptors are primarily involved in the mediation of H2S-induced analgesia. In contrast, our pharmacological and antisense oligodeoxynucleotides studies converge onto the indication that κ opioids receptors do not alter the H2S-mediated effects on visceral sensitivity and pain. Previous pharmacological data indicating that activation of δ opioid receptors attenuates responses to noxious stimuli [28–31] were confirmed by studies conducted by using olygodeoxynucleotide probes direct against δ opioids receptors [32–34]. In our study, the selective δ opioid receptor antagonist NTI has no effect on the H2S-induced analgesia, while the oligodeoxynucleotide probes against DOR cause the reversion of the analgesic effect exerted by H2S, suggesting a relatively minor contribution of δ opioid receptors to pain modulation by H2S. However, the discrepancy between pharmacological and antisense data about the modulation of H2S-induced analgesia by δ opioid receptors needs to be clarified by further studies.
Although hundreds of studies performed by using both pharmacological approaches and antisense probes focused on the different ability of the opioid receptors to cause analgesia, our data fit with the notion that MOR is identified as the most important opioid receptor linked with pain system so that the selective μ endogenous or exogenous agonists are invariably analgesic while selective μ opioid antagonists induce or exacerbate pain by blocking the effects of μ agonists in several experimental conditions. Because antisenses are highly selective and specific in downregulating one opioid receptor without interfering with the activity of other subtypes [35], these pharmacological and antisense studies converge in the indication that μ opioid receptors mediate H2S-induced analgesia.
In the present study we have provided evidence that the analgesic activity of H2S is mediated by the recruitment of μ opioid receptor. In addition to specific pharmacological antagonism exerted in vivo by CTAP and MOR antisense on antinociceptive activity of H2S, results from in vitro pharmacological dissection of signaling pathways activated by H2S are consistent in supporting the view that H2S transactivates the μ opioid receptor. Exposure of SKNMCs to H2S causes conformational changes of the extracellular tail of MOR that are known to be associated with an activated state of the receptor. These conformational changes of the N-terminus unmasks a specific epitope that can be detected by an activation-state specific antibody [36, 37]. Results of experiments carried out using this approach have revealed that exposure of SKNMCs to H2S causes a change in the conformational status of MOR similar to that induced by the enkephalin analog DAMGO, a potent agonist of MOR. Further, and similarly to DAMGO, H2S causes a robust, time- and concentration-dependent phosphorylation of MOR in Ser(377), a site that is specifically required to induce receptor activation and internalization by DAMGO. Previous studies have shown that among the 12° potential phosphorylation sites present in the C-tail of MOR, only Ser(363), Thre(370) and Ser(375) are involved in MOR phosphorylation and linked to receptor activation [38]. DAMGO-induced MOR phosphorylation occurs at Thre (370) and Ser(375) [Ser(377) in human receptor] but only mutation of Ser(375) is reported to attenuate the rate and extent of receptor internalization [38].
One important observation we made is that phosphorylation of MOR's Ser(377) induced by H2S is rapidly reversible. Because prolonged activation of μ opioid receptors leads to their phosphorylation, internalization, desensitization and down-regulation and represents one the main biochemical substrates of morphine tolerance, the fact that H2S causes a short-lasting receptor phosphorylation and that rapid receptor phosphorylation (min) does not directly correlate with the relatively slow rate of desensitization (h) of MOR induced by morphine [27], suggests that this mediator is unlikely to play a role in long term desensitization of MOR and could still be a pharmacological target in situation of MOR desensitization
Mutational analysis has demonstrated that phosphorylation of Ser (375) or Ser(377) in the human receptor is critical for DAMGO-induced MOR internalization [38]. In the present study we have shown that exposure of SKNMCs to H2S not only results in Ser(377) phosphorylation but also in MOR internalization. Similarly to DAMGO, H2S induces a loss of cell surface expression of MOR as monitored by confocal microscopy and cell membrane fractioning technique. MOR internalization induced by H2S is mediated by its recruitment to a protein-protein complex with β arrestin [18]. Previous studies have shown that once phosphoryled, the opioid receptor binds to β arrestin and is trafficked to clathrin-coated pits where it can subsequently be internalized into endosomes. Once internalized, endosomes containing receptors can be fused with lysosomes where receptors are proteolytically degraded or, alternatively, the receptors are dephosphoryled, resensitized and recycled back to membrane [39]. One of the main findings of the present study is that H2S reproduces the same effects of DAMGO in terms of MOR phosphorylation, association with β arrestin and internalization. However, H2S induces a slower β arrestin recruitment and MOR internalization than DAMGO, providing evidence that it does not behave as a direct MOR agonist.
Results form mechanistic studies aimed at dissecting intracellular signals activated by H2S in SKNMCs have shown that H2S activates the PI3K/AKT pathway and induces AKT phosphorylation [21]. PI3K is a lipid kinase acting as a membrane-embedded second messenger [40] and AKT is a downstream target of the PI3K [41]. Activation of MOR by DAMGO induces AKT phosphorylation [42]. Our study confirms these observations and extend this effect to H2S. However, while CTAP reverses AKT phosphorylation induced by DAMGO, it fails to inhibit the effects exerted by H2S on AKT, indicating that, despite MOR trans-activation, H2S-induced AKT phosphorylation is due to a direct effect of the gas on the PI3K/AKT pathway. The fact that inhibition of AKT phosphorylation by the PI3K inhibitor LY294002 prevents MOR internalization induced by H2S but not by DAMGO, indicates that H2S directly activates the PI3K/AKT pathway and that activation of this pathway is hierarchically higher in the mechanism that leads to MOR activation by H2S. These findings are consistent with the observation that activation and internalization of a GPCR can be regulated by activation of the PI3K/AKT pathway [43].
The mechanism through which H2S targets the PI3K/AKT pathway involves KATP channels. Thus not only SKNMCs express SUR1 and Kir6.2, but blocking these channels with glibenclamide abrogates AKT phosphorylation and MOR activation and internalization induced by H2S. This suggest a hierarchic order in the observed effects with H2S acting as a KATP channels opener leading to activation of PI3K/AKT pathway and MOR activation and phosphorylation (Figure 10). Similar transactivation of opioid receptors by epidermal growth factor receptor has been recently described [44], however this is the first evidence of transactivation of MOR by activation of KATP channels.
Schematic representation of H 2 S and opioid receptor interaction. The selective μ opioid receptor enkephalin analog DAMGO acts as a direct agonist of MOR leading to its activation, phosphorylation on Ser(377), co-immunoprecipitation with β arrestin and internalization (panel A and B). The selective MOR antagonist CTAP blocks the effects induced by DAMGO, while it only partially inhibits those induces by H2S. In contrast, H2S opens the KATP channels that activate the PI3K/AKT pathway leading to MOR activation, phosphorylation, co-immunoprecipitation with β arrestin and internalization, as the selective KATP channels blocker glibenclamide and the selective PI3K inhibitor LY294002 inhibit these effects (panel C and D).
Conclusion
This study demonstrates that, in a rodent model of visceral pain, H2S-induced analgesia is mediated by μ opioids receptor activation as, in vivo, the selective antagonism of MOR by i.c.v. administration of both CTAP and antisenses direct against MOR reverses the analgesic effects of H2S. Moreover, pre-treating rats with the KATP channels selective blocker glibenclamide reverses the H2S-induced analgesia. The in vitro studies performed comparing the effect of the μ receptor-selective enkephalin analog DAMGO and H2S confirm these data demonstrating that, in the neuronal-cell line SKNMC, both DAMGO and H2S induce MOR activation and phosphorylation leading to interaction between MOR and β arrestin and MOR internalization. CTAP completely blocks MOR internalization induced by DAMGO while, in contrast, it partially inhibits MOR internalization induced by hydrogen sulphide. In addition, exposure to hydrogen sulphide causes the PI3K/AKT pathway activation and induces AKT phosphorylation. The selective PI3K inhibitor LY294002 does not interfere with the DAMGO-induced MOR internalization, while it causes the inhibition of the translocation process of MOR from the plasma membrane to the cytoplasm induced by hydrogen sulphide as well as AKT phosphorylation induced by hydrogen sulphide. As glibenclamide reverted the analgesia induced by hydrogen sulphide, we hypothize that the ATP potassium channels could modulate MOR activation induced by hydrogen sulphide. First we have demonstrated that SKNMCs express the ATP potassium channels subunits Kir6.2 and SUR1. Moreover, glibenclamide inhibits both MOR and AKT phosphorylation induced by hydrogen sulphide, demonstrating that activation of ATP potassium channels by hydrogen sulphide is a key process of these effects. On these basis we can speculate that hydrogen sulphide acts on the ATP potassium channels that induce the PI3K/AKT pathway that, on turn causes MOR activation and internalization (Figure 10). This study provides the first evidence for a cross-talk between H2S and the μ opioid receptors and paves the way to development of new therapeutic approaches to visceral pain.
Methods
Materials
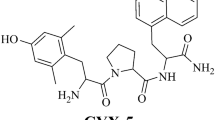
Sodium sulphide (Na2S) was used as donor of hydrogen sulphide and was from Sigma-Aldrich (S. Louis, MO, USA). Methylene blue, glibenclamide, naltrindole (NTI) 5'-guanidinonaltrindole (GNTI),D-Phe-Cys-Tyr-D-Trp-Arg-Thr-Pen-Thr-NH2 (CTAP), mismatched and specific antisense olygodeoxynucleotide probes for opioid receptors, [D-Ala 2,N-Me-Phe 4,Gly 5-o1]enkephalin (DAMGO), ascorbic acid, salicylic acid, potassium hydroxide, trichloroacetic acid, pyridoxal-5'-phosphate and calmodulin were from Sigma-Aldrich (S. Louis, MO, USA). Tissue Protein Extraction Reagent (T-PER) was obtained by Pierce Biotechnology (Rockford, IL, USA).
In vivo experiments
Animals
Male, Wistar rats (200-250 g, Charles River, Monza, Italy) were housed in plastic cages and maintained under controlled conditions with 12-hour light/dark cycles (lights on at 07.00). Tap water and standard laboratory chow were freely available (Additional file 1). It has been demonstrated that the nutrients induce an enhancement of the colorectal sensitivity in both healthy subjects [23] and IBS patients [24, 25]. To avoid the influence of the meal on colorectal perception and pain, food was withdrawn 12 hours before surgical procedures and CRD recordings in all in vivo experiments [11, 12]. However, to verify whether meal could influence the perception of CRD-induced visceral pain, we performed a supplementary experiment on fed rats (n = 5). Experimental procedures were approved by our institutional animal research committees and were in accordance with nationally approved guidelines for the treatment of laboratory animals.
Surgical procedure
Rat were anesthetized by an i.p. injection of 70 mg/kg penthotal and were then mounted in a stereotaxic instrument. To perform the i.c.v. injection, a guide cannula (Alzet Brain Infusion Kit II, 3-5 mm) was inserted stereotaxically into the right lateral cerebral ventricle. The stereotaxic coordinates were 1,6 mm right laterally and 0,8 mm dorsoventrally from the bregma and 3,5 mm below the dura. Drugs dissolved in 10 μl saline were injected into the cerebral ventricle by insertion of an injection cannula (28 gauge stainless steel tube) connected to a catheter tube into the guide cannula which was connected to a syringe. In each injection 10 μl of vehicle or drugs were delivered manually into the ventricle over 3 min. At the end of each experiment, methylene blue solution was injected through the injection cannula to verify its correct placement in the right lateral ventricle. Rats exhibiting motor deficits after the surgical procedure were not used in the subsequent experiments.
CRD and behavioral testing
All experiments began 1 week after the surgical procedure. Distending procedure were performed as previously described (Additional file 2). The behavioral response to CRD was assessed by measuring the abdominal withdrawal reflex (AWR) as previously described [45, 46] (Additional file 2).
Effects of H2S on colonic nociception
The control group (n = 5) consisted of fasting rats that underwent surgical procedures but not CRD, while the CRD group consisted of fasting rats that underwent surgical procedures and two sets of CRD, the first acting as control. To investigate whether H2S administration modulates sensitivity and pain induced by CRD, rats were treated i.p. with vehicle (CRD group) or Na2S, an H2S donor, at the dose of 100 μMol/kg five minutes before CRD.
Effects of the opioid and KATP channels inhibitors
The role of the δ, κ and μ opioid receptors in the H2S-induced antinociception was investigated by pre-treating rats with selective opioid receptor antagonists administered at final volume of 10 μl i.c.v.: NTI, a δ opioid receptor antagonist (4 μg/kg), was injected 5 minutes before Na2S [47]; GNTI, a κ opioid receptor antagonist (0.08 mg/kg), was administered three days before Na2S [48]; CTAP, a μ opioid receptor antagonist (0.09 mg/kg), was administered 30 minutes before Na2S [49]. Control experiments were performed by injecting rats with NTI, GNTI and CTAP alone (n = 5 rats/group).
For antisense experiments rats were pretreated with antisense oligodeoxynucleotides direct against specific exons of DOR, KOR and MOR. A mismatched antisense was used as control (Table 1). All antisense olygodeoxynucleotides were administered i.c.v. in dose of 10 μg in 10 μl volume saline [50, 52, 53]. Treatment with antisenses was performed on day 1, 3 and 5 and the behavioral test was performed at day 6 [51] (Additional file 3).
The involvement of KATP channels in the analgesic effects of H2S was assessed by pre-treating rats with glibenclamide, a selective KATP channel blocker, at a dose of 2.8 μmol/kg injected intravenously (i.v.) for 20 minutes before Na2S administration [11, 12] (Additional file 4).
At the end of the CRD procedures, rats were sacrificed and spinal cords (L1-L5) collected for RT-PCR analysis of cFOS [54] (additional file 5) using the following sense and antisense primers: gtctggttccttctatgcag and taggtagtgcagctgggagt.
In vitro experiments
The immortalized human neuronal SKNMCs were used for in vitro studies. Cells were grown in Minimum Essential Medium with Earl's salts supplemented with 10% FBS, L-glutamine, penicillin and streptomycin, and regularly passaged to maintain exponential growth.
For in vitro studies DAMGO was used at the dose of 1 μM and Na2S at the dose of 50 μM. To determine whether H2S induces MOR activation, SKNMCs were stimulated with DAMGO or Na2S and MOR activation detected by Western blot analysis using a specific antibody raised against a specific epitope in the N-terminus of the receptor that becomes exposed in response to conformational changes induced by receptor activation [55]. This activation-state specific antibody exhibits enhanced recognition of activated receptor [36, 37]. In addition, activation of MOR by H2S was detected by Western blot analysis of receptor phosphorylation on Serine (Ser) (377). Finally, because MOR activation results in receptor recruitment to β arrestin, co-immunoprecipitation experiments were performed to investigate whether H2S induces the formation of a protein-protein complex between MOR and β arrestin (Additional file 6).
Effect of H2S on MOR internalization
To investigate whether exposure of SKNMCs to H2S induces MOR internalization, cells were treated with the μ receptor-selective enkephalin analog DAMGO [15, 16] and Na2S alone or in combination with the MOR antagonist CTAP. Internalization of the receptor was assessed by Western blot analysis by measuring its translocation from the cell membrane fraction to the cytosol and by confocal microscopy (Nikon) using a specific anti-MOR immunofluorescent antibody (Additional file 7).
Effect of H2S on AKT phosphorylation
SKNMCs were exposed to DAMGO and Na2S up to 60 minutes and Western blot analysis performed on whole cell lysates using a specific antibody that detected the phosphorylated form of AKT on Thre(308). AKT phosphorylation was also detected by measuring the AKT phosphorylated form on Ser(473) (phospho-AKT ELISA KIT, Biosource).
Activation of the PI3K/AKT pathway was tested by exposing SKNMCs to the selective PI3K inhibitor LY294002 (50 μM) in the presence of DAMGO or Na2S (Additional file 8).
Effect of KATP channels blockade
Expression of KATP channels in SKNMCs was evaluated by assessing the expression of Kir6.2 and SUR1 sub-units (Additional file 9). Qualitative and quantitative PCR were performed by using the following sense and antisense primers: hGAPDH: gaaggtgaaggtcggagt and catgggtggaatcatattggaa; hSUR.1: gtccagatcatgggaggcta and cagaagacagcccctgagac; hKir6.2: gtcaccagcatccactcctt and ggggacttcaaatgttgcat. The effects of glibenclamide (1 μM) on AKT phosphorylation and MOR activation and internalization were determined (Additional file 9).
Densitometric analysis
All the densitometric analysis have been performed by using the Image J software.
Statistical analysis
Behavioral data are presented as mean ± SE, with sample sizes of at least 5 rats per group. Statistical comparisons of unpaired data were performed by the Mann-Whitney test, while statistical comparisons of paired data were performed by the Wilcoxon signed rank test. Densitometric data have been analyzed with Turkey's multiple comparison test. Data on AKT phosphorylation are presented as mean ± SE, with sample sizes of at least 5 experiments per group. An associated probability (p value) of less that 5% was considered significant.
References
Fiorucci S, Distrutti E, Cirino G, Wallace JL: The emerging roles of hydrogen sulfide in the gastrointestinal tract and liver. Gastroenterology 2006, 131: 259–271. 10.1053/j.gastro.2006.02.033
Wang R: Two's company three's a crowd: can H 2 S be the third endogenous gaseous transmitter? FASEB J 2002, 16: 1792–1798. 10.1096/fj.02-0211hyp
Boehning D, Snyder SH: Novel neural modulators. Annu Rev Neurosci 2003, 26: 105–131. 10.1146/annurev.neuro.26.041002.131047
Schemann M, Grundy D: >Role of hydrogen sulfide in visceral nociception. Gut 2009, 58: 744–747. 10.1136/gut.2008.167858
Zhao W, Zhang J, Lu Y, Wang R: The vasorelaxant effect of H 2 S as a novel endogenous gaseous K ATP channel opener. EMBO J 2001, 20: 6008–6016. 10.1093/emboj/20.21.6008
Abe K, Kimura H: The possible role of hydrogen sulfide as an endogenous neuromodulator. J Neurosci 1996, 16: 1066–1071.
Eto K, Ogasawara M, Umemura K, Nagai Y, Kimura H: Hydrogen sulfide is produced in response to neuronal excitation. J Neurosci 2002, 22: 3386–3391.
Kimura H: Hydrogen sulfide induces cyclic AMP and modulates the NMDA receptors. Biochem Biophys Res Commun 2000, 267: 129–133. 10.1006/bbrc.1999.1915
Dello Russo C, Tringali G, Ragazzoni E, Maggiano N, Menini E, Vairano M, Preziosi P, Navarra P: Evidence that hydrogen sulphide can modulate hypothalamo-pituitary-adrenal axis function: in vitro and in vivo studies in the rat. J Neuroendocrinol 2000, 12: 225–233. 10.1046/j.1365-2826.2000.00441.x
Whiteman M, Armstrong JS, Chu SH, Jia-Ling S, Wong BS, Cheung NS, Halliwell B, Moore PK: The novel neuromodulator hydrogen sulfide: an endogenous peroxynitrite 'scavenger'? J Neurochem 2004, 90: 765–768. 10.1111/j.1471-4159.2004.02617.x
Distrutti E, Sediari L, Mencarelli A, Renga B, Orlandi S, Antonelli E, Roviezzo F, Morelli A, Cirino G, Wallace JL, Fiorucci S: Evidence that hydrogen sulfide exerts antinociceptive effects in the gastrointestinal tract by activating K ATP channels. J Pharmacol Exp Ther 2006, 316: 325–335. 10.1124/jpet.105.091595
Distrutti E, Sediari L, Mencarelli A, Renga B, Orlandi S, Russo G, Caliendo G, Santagada V, Cirino G, Wallace JL, Fiorucci S: 5-Amino-2-hydroxybenzoic acid 4-(5-thioxo-5H-[1, 2]dithiol-3yl)-phenyl ester (ATB-429), a hydrogen sulfide-releasing derivative of mesalamine exerts antinociceptive effects in a model of postinflammatory hypersensitivity. J Pharmacol Exp Ther 2006, 319: 447–458. 10.1124/jpet.106.106435
Uhl GR, Childers S, Pasternak G: An opiate-receptor gene family reunion. Trend Neurosci 1994, 17: 89–93. 10.1016/0166-2236(94)90110-4
Reisine T, Bell GI: Molecular biology of opioid receptors. Trends Neurosci 1993, 16: 506–510. 10.1016/0166-2236(93)90194-Q
Sternini C, Brecha NC, Minnis J, D'Agostino G, Balestra B, Fiori E, Tonini M: Role of agonist-dependent receptor internalization in the regulation of μ opioid receptors. Neuroscience 2000, 98: 233–241. 10.1016/S0306-4522(00)00118-4
Sternini C, Spann M, Anton B, Keith DE Jr, Bunnett NW, von Zastrow M, Evans C, Brecha NC: Agonist-selective endocytosis of μ-opioid receptor by neurons in vivo. Proc Natl Acad Sci 1996, 93: 9241–9246. 10.1073/pnas.93.17.9241
Mantyh PW, DeMaster E, Malhotra A, Ghilardi JR, Rogers SD, Mantyh CR, Liu H, Basbaum AI, Vigna SR, Maggio JE: Receptor endocytosis and dendrite reshaping in spinal neurons after somatosensory stimulation. Science 1995, 268: 1629–1632. 10.1126/science.7539937
Ferguson SS, Zhang J, Barak LS, Caron MG: Role of beta-arrestins in the intracellular trafficking of G-protein-coupled receptors. Adv Pharmacol 1998, 42: 420–424. full_text
Rodrigues ARA, Duarte IDG: The peripheral antinociceptive effect induced by morphine is associated with ATP-sensitive K + channels. Br J Pharmacol 2000, 129: 110–114. 10.1038/sj.bjp.0703038
Ocaña M, Cendán CM, Cobos EJ, Entrena JM, Baeyens JM: Potassium channels and pain: present realities and future opportunities. Eur J Pharmacol 2004, 500: 203–219. 10.1016/j.ejphar.2004.07.026
Yong QC, Lee SW, Foo CS, Neo KL, Chen X, Bian JS: Endogenous hydrogen sulphide mediates the cardioprotection induced by ischemic postconditioning. Am J Physiol Hearth Circ Physiol 2008, 295: H1330-H1340. 10.1152/ajpheart.00244.2008
Polakiewicz RD, Schieferl SM, Gingras AC, Sonenberg N, Comb MJ: μ-Opioid receptor activates signalling pathways implicated in cell survival and translational control. J Biol Chem 1998, 273: 23534–23541. 10.1074/jbc.273.36.23534
Musial F, Crowell MD, Kalveram KT, Enck P: Nutrient ingestion increases rectal sensitivity in humans. Physiol Behav 1994, 55: 953–956. 10.1016/0031-9384(94)90085-X
Distrutti E, Hauer SK, Fiorucci S, Pensi MO, Morelli A: Intraduodenal lipids increase perception of rectal distension in IBS patients. Gastroenterology 2000,118(4, suppl 2):A138.
Simrén M, Agerforz P, Björnsson ES, Abrahamsson H: Nutrient-dependent enhancement of rectal sensitivity in irritable bowel syndrome (IBS). Neurogastroenterol Motil 2007, 19: 20–29. 10.1111/j.1365-2982.2006.00849.x
Raynor K, Kong H, Chen Y, Yasuda K, Yu L, Bell GI, Reisine T: Pharmacological characterization of the clones kappa delta and mu opioid receptor. Mol Pharmacol 1994, 45: 330–334.
Gutstein HB, Akil H: Opioid analgesics. In Goodman and Gilman's The pharmacological basis of therapeutics.. Edited by: Hardman JGL, Limbird LE. New York: McGraw-Hill; 2001:569–619.
Danzebrink RM, Green SA, Gebhart GF: Spinal mu and delta but not kappa opioid-receptor agonists attenuate responses to noxious colorectal distension in the rat. Pain 1995, 63: 39–47. 10.1016/0304-3959(94)00275-J
Marker CL, Lujan R, Loh HH, Wickman K: Spinal G-protein-gated potassium channels contribute in a dose-dependent manner to the analgesic effect of μ- and δ- but not κ-opioids. J Neurosci 2005, 25: 3551–3559. 10.1523/JNEUROSCI.4899-04.2005
Pacheco DF, Reis GM, Francischi JN, Castro MS, Perez AC, Duarte ID: Delta-opioid receptor agonist SNC80 elicits peripheral antinociception via delta (1) and delta (2) receptors and activation of the l-arginine/nitric oxide/cyclic GMP pathway. Life Sci 2005, 78: 54–60. 10.1016/j.lfs.2005.04.032
Gendron L, Pintar JE, Chavkin C: Essential role of mu opioids receptor in the regulation of delta opioids receptor-mediated antihyperalgesia. Neurosci 2007, 150: 807–817. 10.1016/j.neuroscience.2007.09.060
Bilsky EJ, Wang T, Lai J, Porreca F: Selective blockade of peripheral delta opioids agonist induced antinociception by intrathecal administration of delta receptor antisense oligodeoxynucleotide. Neurosci Lett 1996, 220: 155–158. 10.1016/S0304-3940(96)13262-6
Fraser GL, Pradhan AA, Clarke PB, Wahlestedt C: Supraspinal antinociceptive response to [D-Pen(2,5)]-enkephalin (DPDPE) is pharmacologically distinct from that to other delta-agonists in the rat. J Pharmacol Exp Ther 2000, 295: 1135–1141.
Lohmann AB, Welch SP: Antisense to opioids receptors attenuate ATP-gated K+ channel opener-induced antinociception. Eur J Pharmacol 1999, 384: 147–152. 10.1016/S0014-2999(99)00698-6
Pasternak GW, Standifer KM: Mapping of opioid receptors using antisense oligodeoxynucleotides: correlating their molecular biology and pharmacology. Trend Pharmacol Sci 1995, 16: 344–350. 10.1016/S0165-6147(00)89068-9
Gupta A, Décaillot FM, Gomes I, Tkalych O, Heimann AS, Ferro ES, Devi LA: Conformation state-sensitive antibodies to G-protein-coupled receptors. J Biol Chem 2007, 282: 5116–5124. 10.1074/jbc.M609254200
Gupta A, Rozenfeld R, Gomes I, Raehal KM, Décaillot FM, Bohn LM, Devi LA: Post-activation-mediated changes in opioid receptors detected by N-terminal antibodies. J Biol Chem 2008, 283: 10735–10744. 10.1074/jbc.M709454200
El Kouhen R, Burd AL, Erickson-Herbrandson LJ, Chang CY, Law PY, Loh HH: Phosphorylation of Ser 363 , Thr 370 and Ser 375 residues within the carboxyl tail differentially regulates μ-opioid receptor internalization. J Biol Chem 2001, 276: 12774–12780. 10.1074/jbc.M009571200
Ferguson SS: Evolving concepts in G protein-coupled receptor endocytosis: the role in receptor desensitization and signaling. Pharmacol Rev 2001, 53: 1–24.
Whitman M, Downes CP, Keeler M, Keller T, Cantley L: Type I phosphatidylinositol kinase makes a novel inositol phospholipids phosphatidylinositol-3-phosphate. Nature 1988, 332: 644–646. 10.1038/332644a0
Chan TO, Rittenhouse SE, Tsichlis PN: AKT/PKB and other D3 phosphoinositide-regulated kinases: activation by phosphoinositide-dependent phosphorylation. Annu Rev Biochem 1999, 68: 965–914. 10.1146/annurev.biochem.68.1.965
Iglesias M, Segura MF, Comella JX, Olmos G: Mu-opioid receptor activation prevents apoptosis following serum withdrawal in differentiated SH-SY5Y cells and cortical neurons via phosphatidylinositol 3-kinase. Neuropharmacology 2003, 44: 482–492. 10.1016/S0028-3908(03)00024-8
Gavi S, Shumay E, Wang H-y, Malbon CC: G-protein-coupled receptors and tyrosin kinases: crossroads in cell signalling and regulation. Trends Endocrinol Met 2006, 17: 46–52.
Chen Y, Long H, Wu Z, Jiang X, Ma L: EGF transregulates opioid receptors through EGFR-mediated GRK2 phosphorylation and activation. Mol Biol Cell 2008, 19: 2973–2983. 10.1091/mbc.E07-10-1058
Al-Chaer ED, Kawasaki M, Pasricha PJ: A new model of chronic visceral hypersensitivity in adult rats induced by colon irritation during postnatal development. Gastroenterology 2000, 119: 1276–1285. 10.1053/gast.2000.19576
Ness TJ, Gebhart GF: Visceral pain: a review of experimental studies. Pain 1990, 41: 167–234. 10.1016/0304-3959(90)90021-5
Calcagnetti DJ, Holtzman SG: Delta Opioid antagonist naltrindole, selectively blocks analgesia induced by DPDPE but not DAMGO or morphine. Pharmacol Biochem Behav 1991, 38: 185–190. 10.1016/0091-3057(91)90608-5
Jewett DC, Grace MK, Jones RM, Billington CJ, Portoghese PS, Levine AS: The kappa-opioid antagonist GNTI reduces U50,488-, DAMGO-, and deprivation-induced feeding but not butorphanol- and neuropeptide Y-induced feeding in rats. Brain Res 2001, 909: 75–80. 10.1016/S0006-8993(01)02624-5
Sterious SN, Walker EA: Potency differences for D-Phe-Cys-Tyr-D-Trp-Arg-Thr-Pen-Thr-NH2 as an antagonist of peptide and alkaloid micro-agonists in an antinociception assay. J Pharmacol Exp Ther 2003, 304: 301–309. 10.1124/jpet.102.042093
Rossi GC, Pan Y-X, Brown GP, Pasternak GW: Antisense mapping the MOR-1 opioid receptor: evidence of alternative splicing and a novel morphine-6β-glucuronide receptor. FEBS Letters 1995, 369: 192–196. 10.1016/0014-5793(95)00757-Z
Rossi GC, Leventhal L, Pan YX, Cole J, Su W, Bodnar RJ, Pasternak GW: Antisense mapping of MOR-1 in rats: distinguishing between morphine and morphine-6β-glucoronide antinociception. J Pharmacol Exp Ther 1997, 281: 109–114.
Silva RM, Grossman HC, Hadjimarkou MM, Rossi GC, Pasternak GW, Bodnar RJ: Dynorphin A 1–17- -induced feeding: pharmacological characterization using selective opioid antagonists and antisense probes in rats. J Pharmacol Exp Ther 2002, 301: 513–518. 10.1124/jpet.301.2.513
Israel Y, Kandov Y, Khaimova E, Kest A, Lewis SR, Pasternak GW, Pan YX, Rossi GC, Bodnar RJ: NPY-induced feeding: pharmacological characterization using selective opioid antagonists and antisense probes in rats. Peptides 2005, 26: 1167–1175. 10.1016/j.peptides.2005.01.017
Bonaz B, Rivière PJ, Sinniger V, Pascaud X, Junien JL, Fournet J, Feuerstein C: Fedotozine, a kappa-opioid agonist prevents spinal and supra-spinal Fos expression induced by a noxious visceral stimulus in the rat. Neurogastroenterol Motil 2000, 2: 135–147. 10.1046/j.1365-2982.2000.00188.x
Gomes I, Gupta A, Singh SP, Sharma SK: Monoclonal antibody to the delta opioid receptor acts as an agonist in dual regulation of adenylate cyclase in NG 108–15 cells. FEBS Lett 1999, 456: 126–130. 10.1016/S0014-5793(99)00878-9
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
ED and SF conceived the study and wrote the manuscript. S Cianetti wrote the manuscript. S Cipriani and AM carried out the in vivo studies and helped to draft the manuscript (Methods section). BR and MM carried out the in vitro studies and helped to draft the manuscript (Methods section). All authors read and approved the final manuscript.
Electronic supplementary material
12990_2009_295_MOESM2_ESM.DOC
Additional file 2: CRD and behavioral testing. This file describes the behavioral testing used in the in vivo studies. (DOC 28 KB)
12990_2009_295_MOESM3_ESM.DOC
Additional file 3: Effects of the opioid receptors antagonism. This file describes the methods used for blocking the opioid receptors. (DOC 30 KB)
12990_2009_295_MOESM4_ESM.DOC
Additional file 4: Effects of K ATP channels. This file describes the method used for blocking the KATP channels. (DOC 24 KB)
12990_2009_295_MOESM5_ESM.DOC
Additional file 5: Spinal cFOS expression. This file describes the method used for determining spinal cFos expression. (DOC 27 KB)
12990_2009_295_MOESM7_ESM.DOC
Additional file 7: Effect of H 2 S on MOR internalization. This file describes the methods used to detect MOR internalization. (DOC 28 KB)
12990_2009_295_MOESM8_ESM.DOC
Additional file 8: Effect of H 2 S on AKT phosphorylation. This file describes the methods used to determine AKT phosphorylation. (DOC 27 KB)
12990_2009_295_MOESM9_ESM.DOC
Additional file 9: Effects of glibenclamide. This file describes the methods used to determine the effects of KATP channels blockade. (DOC 30 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Distrutti, E., Cipriani, S., Renga, B. et al. Hydrogen sulphide induces μ opioid receptor-dependent analgesia in a rodent model of visceral pain. Mol Pain 6, 36 (2010). https://doi.org/10.1186/1744-8069-6-36
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1744-8069-6-36