Abstract
Insulin and insulin-like growth factors (IGFs) maintain vital neuronal functions. Absolute or functional deficiencies of insulin or IGF-I may contribute to neuronal and vascular complications associated with diabetes. Vanilloid receptor 1 (also called TRPV1) is an ion channel that mediates inflammatory thermal nociception and is present on sensory neurons. Here we demonstrate that both insulin and IGF-I enhance TRPV1-mediated membrane currents in heterologous expression systems and cultured dorsal root ganglion neurons. Enhancement of membrane current results from both increased sensitivity of the receptor and translocation of TRPV1 from cytosol to plasma membrane. Receptor tyrosine kinases trigger a signaling cascade leading to activation of phosphatidylinositol 3-kinase (PI(3)K) and protein kinase C (PKC)-mediated phosphorylation of TRPV1, which is found to be essential for the potentiation. These findings establish a link between the insulin family of trophic factors and vanilloid receptors.
Similar content being viewed by others
Introduction
TRPV1 is a Ca2+ permeable nonspecific cation channel, located on peripheral sensory neurons, that serves as a molecular detector for heat, capsaicin, protons, and endovanilloids [1–4]. Moreover, its role as a heat sensor (activation threshold of ~43°C), its influence from trophic/inflammatory agents (i.e. nerve growth factor, bradykinin, prostaglandins, etc.) and its vasodilatory effect on small vessels (by releasing CGRP) make TRPV1 an essential component of the pain pathway [3, 5–11].
In peripheral nerves, insulin does not promote its typical metabolic effects of glucose and amino acid uptake [12]. However, physiologic concentrations can act as neurotrophic factors, in combination with nerve growth factor (NGF), to stimulate neurite outgrowth and survival of both sensory and sympathetic neurons [13–15]. Furthermore, it has been proposed that insulin and IGFs exert trophic influences on the same neurons that are responsive to NGF by sharing common signaling pathways [13].
Though it is widely believed these neural disturbances are secondary to hyperglycemia [16], this remains controversial. Results from the Diabetes Control and Complications Trial show that intensive glycemic control for 5 years reduced the incidence of neuropathy by 60% in Type I patients [17]. However, the fact that strict glucose regulation does not completely prevent diabetic peripheral neuropathy suggests additional mechanisms as a result of insulin deficiency may be involved.
Experiments in humans show that non-diabetic, normoglycemic subjects have heat thresholds that correlate positively with insulin sensitivity [18]. Furthermore, circulating levels of IGFs and NGF are reduced in diabetes and to a greater degree in patients with thermal sensory deficits characteristic of neuropathy [19–21]. Growth factor replacement therapy improves neuronal regeneration [22, 23] and insulin, under conditions of rapid infusion, can restore decreased neurogenic vasodilation [24, 25]. Taken together, these studies suggest that insulin and trophic factor deficiencies may alter sensory nerve function [26].
In this study we demonstrate that insulin and IGF-I enhance TRPV1-mediated membrane currents by enhancing receptor sensitivity and translocation from cytosol to plasma membrane in heterologous expression systems and cultured dorsal root ganglion (DRG) neurons in a PKC-dependent manner. Preliminary results of this study have been published elsewhere in an abstract form [27].
Materials and Methods
Oocyte Electrophysiology
Oocytes were isolated from tricaine-anesthetized Xenopus laevis and separated from the follicular layer after incubation with collagenase (1–2 mg/ml). 3–7 days following cRNA injections (50–70 nl, 1 μg/μl), oocytes were stored at 18°C and used for experiments. Double electrode voltage clamp (-60 mV) was performed using a Warner amplifier (Warner Instruments, OC725C, Hamden, CT, USA) with 100% d.c. gain, digitized and stored on video tape. Experiments were performed at 21–23°C. Oocytes were placed in a Perspex chamber superfused (5–10 ml min-1) with Ca2+-free Ringer solution containing (in mM): 100 NaCl, 2.5 KCl, 5 HEPES, pH 7.35. Within figures, current traces were shown as initial response to agonist juxtaposed on currents recorded following incubation with insulin, IGF-I and various inhibitors. Time course experiments consisted of current recording during capsaicin application in the presence of either control (first 20 min) or insulin (last 15 min) containing solutions. In all experiments, fold increase was calculated as agonist induced current amplitude in the presence of trophic factors and inhibitors divided by the agonist induced initial current amplitude under control conditions before their bath application. I-V relationships were measured using 500-ms voltage ramps from -80 mV to +80 mV.
DRG Culture and Electrophysiology
Dorsal root ganglia were isolated from embryonic day 18 (E18) rats, triturated and cultured for 5–7 d in Neurobasal/B-27 (Life Technologies; Grand Island, NY) + 10% fetal bovine serum (FBS) on poly-D-lysine-coated glass coverslips. For perforated patch recording, the bath solution contained (in mM): 140 NaGlu, 2.5 KCl, 10 HEPES, 2 MgCl2, 1 EGTA, pH 7.35 and the pipette solution contained (in mM): 130 NaGlu, 10 NaCl, 2.5 KCl, 10 HEPES, 1 MgCl2, 0.2 EGTA, and amphotericin B (240 μg/ml). For cell-attached recording, the bath solution contained (in mM): 140 Kglu, 10 NaCl, 10 HEPES, 1 EGTA, 2 MgCl2, pH 7.35 and the pipette contained (in mM): 140 NaGlu, 2.5 KCl, 10 HEPES, 2 MgCl2, pH 7.35. Currents were recorded using a WPC 100 patch clamp amplifier (E. S. F. Electronic, Goettingan, Germany) or Axopatch 200B (Axon Instruments, Union City, CA). Data were digitized (VR-10B, Instrutech Corp.; Great Neck, NY) and stored on video tape.
For analysis, data were filtered at 2.5 kHz (-3db frequency with an 8-pole low-pass Bessel filter, Warner Instruments, LPF-8) and digitized at 5 kHz. Data analyses were performed on continuous stretches greater than 20 s from patches that contained one or two channels. Single channel current amplitude and Po were calculated from all point amplitude histograms fitted with Gaussian functions (Microcal Origin; Northampton, MA).
Ca2+ Imaging
Cells were grown on glass coverslips, then incubated with 5 μM Fluo-4AM (Molecular Probes; Eugene, OR) for 20 min at 37°C, washed with physiological buffer [(in mM): 140 NaCl, 5 HEPES, 2 CaCl2, 1 MgCl2, 2.5 KCl, pH 7.35], and treated with 500 nM capsaicin +/- 1 μM insulin immediately prior to analysis by confocal microscopy (Fluoview, Olympus; Mellville, NY). Data for each cell was quantified as the fluorescence after treatment (F) divided by initial fluorescence (Fo) at t = 0 (Fluoview software).
Transfection of Cells and Cell Culture
HEK 293 cells, which endogenously express IGF-I receptors [29] were cultured in Dulbecco's modified Eagle's medium (high glucose) supplemented with 10% fetal bovine serum, 50 units/ml penicillin, and 50 μg/ml streptomycin (Invitrogen; Carlsbad, CA) and maintained under 95% air/ 5% CO2 at 37°C. Cells were transiently transfected with wild type TRPV1, TRPV1eGFP, TRPV1 S502/S800A mutant (gifted by D. Julius, N. Kadei, M. Tominaga, respectively), or TRPV1-V5-His tagged plasmid using Lipofectamine2000 reagent (Invitrogen) according to manufacturer's protocol. TRPV1-V5-His tagged plasmid was constructed in pcDNA3.1 vector using Topo Cloning kit (Invitrogen). To determine the membrane translocation of TRPV1, confocal images (1 μm sections) of GFP-tagged TRPV1 fluorescence was obtained. The intensity of the brightest membrane fluorescence was selected and quantified using MCID imaging software (Imaging Research Inc; St. Catherines, ONT)
Determination of Surface TRPV1
After 36 h of TRPV1 transfection, the cells (grown on 100 mm tissue culture plate) were insulin-treated and biotinylated with membrane impermeable NHS-LC-biotin (1.5 mg/ml in PBS; Pierce, Rockford, IL) as per manufacturer's protocol. Labeled cells were lysed in RIPA buffer and immunoprecipitated overnight with 10 μl of goat anti-VR1 polyclonal antibody/ Protein A/G Plus-agarose (Santa Cruz Biotechnology, Santa Cruz, CA) following manufacturer's protocol. Immunoprecipitates were eluted with 2X SDS sample buffer, separated on 7.5% SDS-PAGE, and transferred to PVDF membrane. To detect total TRPV1, blots were probed with rabbit anti-VR1 polyclonal antibody (1:1000; Affinity Bioreagents, Golden, CO). Specific antibody binding was detected using HRP-conjugated anti-rabbit secondary antibody (1:20,000; Jackson Immunoresearch, West Grove, PA) and Super Signal reagent (Pierce). To detect surface TRPV1, blots were stripped and probed with neutravidin-HRP (1:20,000; Pierce). Chemiluminescence was captured in Hitachi CCD Bio Genetic Systems after exposing the blot to Super Signal reagent (Pierce). Data were quantitated using LabWorks analysis software (UVP Inc., Upland, CA) and surface TRPV1 was normalized using total TRPV1. TRPV1-V5-His transfected cells were biotinylated as above and purified using Ni-NTA agarose (Qiagen, Valencia, CA) as per manufacturer's protocol.
Immunohistochemistry
Cells were plated on glass coverslips coated with 40 μg ml-1 poly-L-lysine, treated with insulin/IGF/PDBu after 36 h of transfection, and fixed with 4% paraformaldehyde for 1 h. The cells were probed with rabbit anti-VR1 antibody (1:10,000; Affinity Bioreagents) followed by rhodamine red-X conjugated anti-rabbit secondary antibody (1:50; Jackson Immuno Research) following method described by Santa Cruz Biotechnology. Confocal images (1 μm sections) were captured using 570 nm laser. The brightest membrane fluorescence was selected from control and treated cells and quantified using MCID imaging software (Imaging Research Inc.).
Unless otherwise stated, all chemicals were obtained by Sigma (St. Louis, MO). Data are given as mean ± s.e.m. and statistical significance (set at P < .05) was evaluated using Student's t-test or one-way ANOVA.
Results
Insulin and IGF-I potentiate TRPV1 current in oocytes
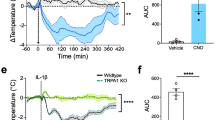
First, we tested whether insulin and/or IGFs influence TRPV1-mediated membrane currents. The effect of insulin and IGF-I on cloned TRPV1 was characterized through dual-electrode voltage clamp (Vm = -60 mV) of Xenopus oocytes injected with TRPV1 cRNA. Insulin (1 μM) significantly potentiated the response to capsaicin (500 nM) greater than 2 fold (Fig. 1a). The time course of insulin-induced potentiation of capsaicin response shows a significant increase in current amplitude for 5, 10 and 15 minute incubation periods compared to initial levels (Fig. 1b). Dose response curves of capsaicin show that both the sensitivity (EC50 shifted from 0.9 to 0.6 μM) and the maximal response (normalized to 1 μM capsaicin induced current before insulin application) increased (from 1.8 to 2.4) after incubation of oocytes with insulin (circles) for 5 min (Fig. 1c). A representative current-voltage relationship (I-V curve) confirms the outward rectification characteristic of TRPV1 current and shows that, in the presence of insulin, amplitude is increased at both positive and negative potentials (Fig. 1d). In addition, current potentiation was also seen with heat evoked responses (Fig. 1e) and protons (Fig. 1f), an endogenous TRPV1 agonist. These experiments show that insulin is increasing TRPV1-mediated currents and making the receptor more responsive to exogenous and endogenous activators.
Insulin and IGF-I potentiate TRPV1 currents in Xenopus Oocytes. a, A representative dual-electrode whole-oocyte experiment showing potentiation of capsaicin induced TRPV1 currents following 15 min incubation of insulin (see Methods). b, Time course for capsaicin induced current (■: 500 nM capsaicin, 30 sec application) before and after insulin exposure at 5 (P < .05), 10 (P < .01), and 15 min (P < .01) incubation times (n = 7). c, Dose response curve of capsaicin before (squares) and after 5 μM insulin (circles) application, the currents were normalized to 1 μM capsaicin before insulin application (n = 2 to 4, before and after insulin). Both the sensitivity (EC50 shifted from 0.9 to 0.6 μM) and maximal response increased (1.8 to 2.4). d, Representative I-V relationships (1 s, 1 mV step ramp from -80 to +80 mV) before and after insulin treatment that demonstrates the outward rectification typical of TRPV1 channels. e, Potentiation of heat-induced currents by insulin. f, Potentiation of pH induced currents by insulin. g, Potentiation of pH induced currents by IGF-I. h, Tyrphostin A47, an IR / IGFR antagonist, blocked insulin potentiation. i, Summary graph showing fold increase in TRPV1 currents following 10 min incubation with control, insulin (cap: n = 5, P < .01; pH: n = 4, P < .01), IGF-I (n = 3, P < .01), and insulin + tyrophostin A47 (n = 3, P < .01). Results are expressed as increase in current amplitude relative to initial capsaicin or pH response.
Oocytes endogenously express insulin-like growth factor receptors (IGFR) rather than insulin receptors (IR) [30]. Insulin binds to IGFR with 100–1000 times lower affinity than IR. On the other hand, IGF-I binds to IGFR with much higher affinity, so we tested whether lower concentrations of IGF-I could potentiate TRPV1. Indeed, 20 nM IGF-I potentiated pH currents to a similar degree as 1 μM insulin (Fig. 1g). Potentiation was dramatically reduced by the addition of tyrphostin A47 (100 μM; 10 min), a selective inhibitor for the insulin family of receptor tyrosine kinases (Fig. 1h). Together these data suggest that in oocytes, insulin and IGF-I are acting through IGFR to potentiate TRPV1 (Fig. 1i).
Insulin and IGF-I potentiate native TRPV1 current in DRG neurons
Since insulin and IGF-I functions vary with cell type, it was important to establish that current potentiation also occurred in sensory neurons that express native TRPV1 [15, 21]. Therefore, we determined the effect of insulin and IGF-I on capsaicin-induced TRPV1 responses using cultured DRG neurons. For whole cell recordings, the perforated patch technique was used to prevent desensitization and tachyphylaxis, minimize intracellular disruption, and maintain intact signaling cascades. In this setting, insulin (1 μM) induced a potentiation of the capsaicin (100 nM) response (Fig. 2a), which returned to control levels 20 minutes after its removal (Fig. 2b, inset). Like oocytes, similar results were seen with IGF-I, signifying that insulin was binding IGFR in DRG neurons (Fig. 2c).
Insulin and IGF-I potentiate native TRPV1 currents in DRG neurons. a, Capsaicin (100 nM, applied at 2 min intervals) response was enhanced by insulin (1 μM) under perforated patch conditions. b, Time course of insulin induced potentiation of capsaicin currents (■: 500 nM capsaicin, 20 sec application) (n = 4, P < .01 at 5, 10, and 15 min incubation times). Inset shows the time course for experiment in Fig. 2a. c, Summary graph showing fold increase in TRPV1 currents following 10 min treatment with control (n = 15), insulin (1 μM; n = 11, P < .01) and IGF-I (20 nM; n = 4, P < .01). d, Under confocal microscopy, insulin (1 μM, 2 min) potentiated intracellular Ca2+ rise in response to 500 nM capsaicin (n = 10, P < .05). e, Capsaicin induced single channel current activity recorded at +60 mV was increased by exposure of cell to insulin (1 μM). f, Mean capsaicin induced open probability (Po) in the absence and presence of insulin (n = 5, P < .05). g, Mean current amplitude observed from single channel recordings (n = 5).
To confirm electrophysiological experiments, measurements of Ca2+-uptake were performed using confocal microscopy (Fig. 2d). In DRG neurons, capsaicin (500 nM) produced a Ca2+ influx that was increased in the presence of insulin. This shows that insulin elevated TRPV1-regulated Ca2+ mobilization. Together this data, confirm that the potentiation seen with cloned TRPV1 in oocytes is present in native TRPV1 expressing peripheral sensory neurons as well.
Insulin increases single channel activity
To understand the underlying molecular mechanism responsible for whole-cell potentiation, single channel currents were recorded in cell-attached patches from DRG neurons. Under this configuration, extracellular insulin would require receptor mediated signal transduction to facilitate changes in TRPV1 channel function recorded within the patch area (Fig. 2e). Channel open probability (Po), a measure of the time the channel spends in the open state, induced by capsaicin (10 nM) increased following bath-application of insulin (1 μM), outside the patch area (Fig. 2e, lower graphs). Po significantly changed from 0.15 ± 0.05 in control conditions to 0.43 ± 0.14 after insulin (Fig. 2f), without altering the single channel amplitude (Fig. 2g). Since insulin application was outside the patch, these data support intracellular signaling, as opposed to direct binding to TRPV1 as a mechanism for insulin-mediated potentiation.
Signaling cascades utilized by Insulin and IGF-I
IR and IGFR produce their effects via an overlapping set of downstream enzymes [29], so we sought to identify signaling pathways involved in TRPV1 modulation. First, receptor tyrosine kinase (RTK) involvement was assessed by pretreating oocytes with membrane permeable inhibitors before and during insulin application (Fig. 3a). The nonspecific RTK blockers genistein (50 μM, 60 min) and lavendustin A (100 μM, 60 min) significantly reduced IGF-I (20 nM, 10 min) potentiation. Second, wortmannin (100 nM, 15 min), a specific phosphatidylinositol 3-kinase (PI(3)K) inhibitor, reduced potentiation as well. Thus, we reasoned that insulin and IGF-I utilize receptor tyrosine kinases to activate PI(3)K and prompt a signaling cascade that leads to TRPV1 current potentiation.
Singnaling cascades utilized by Insulin and IGF-I. a, Summary graph showing fold increase of current in the presence of IGF-I and the inhibitors: genistein (50 μM, n = 6, P < .05), lavendustin A (100 μM, n = 7, P < .05), wortmannin (100 nM, n = 5, P < .05) and BIM (200 nM, n = 5, P < .05). b, A PKC phosphorylation site TRPV1 mutant (S502A/S800A) (n = 6, P < .01, upper trace) and cytochalasin D (1 μM, n = 4, P < .01, lower trace) completely blocked insulin potentiation.
PI(3)K mediates some of its effects through various isoforms of protein kinase C (PKC) [29]. Therefore, we tested in oocytes expressing TRPV1 whether insulin and IGF-I could activate PKC, an enzyme known to potentiate TRPV1 through channel phosphorylation [8, 31]. Bisindoylmaleimide (BIM; 200 nM, 60 min), a nonspecific PKC inhibitor, significantly decreased IGF-I potentiation (Fig. 3a). The importance of PKC was further demonstrated using a mutant TRPV1 (S502A/S800A), which lacks residues acting as substrates for PKC phosphorylation (31) (Fig. 3b, upper trace). Two consequences of these mutations were apparent. First, insulin/IGF-I potentiation was abolished. Second, current amplitude was smaller in oocytes injected with mutant TRPV1 compared to wild type, suggesting that phosphorylation might have an intrinsic effect on basal channel function. Thus, it appears that RTK, PI(3)K and PKC activation are required for current potentiation by insulin.
Insulin and IGF-I translocate TRPV1 to the plasma membrane
In a number of systems, insulin and/or IGF-I can increase surface content of effector molecules [32–34]. We have used five different approaches to examine whether TRPV1 translocation occurs in response to insulin or IGF-I. First, we used cytochalasin D (1 μM, 60 min) to inhibit actin polymerization and decrease vesicular fusion to the plasma membrane in oocytes (Fig. 3b, lower traces). Cytochalasin D almost completely blocked TRPV1 current potentiation by insulin, implicating involvement of protein trafficking affecting translocation of both TRPV1 and PKC. Second, insulin and PDBu not only increased the potency but also the efficacy of capsaicin induced currents. In DRG neurons, at saturating concentrations of capsaicin (20 μM) (Fig. 4a i ) the current amplitude increased (>50%) following exposure (2–5 min) to insulin (1 μM) (Fig. 4a ii ) or PDBu (1 μM) (Fig. 4a iii ) suggesting recruitment of new channels into the plasma membrane or activation of previously silent channels (see also Fig. 1c). Third, Western blot analysis of cell-surface biotinylated TRPV1 expressed in HEK cells was carried out to test whether TRPV1 itself was being translocated to the plasma membrane (Fig. 4b). Analysis of band densities indicates that insulin (10 μM, 15 min) doubled surface TRPV1 expression levels relative to controls. Fourth, relative surface to cytosol optical intensities were quantified by immunofluorescence microscopy (Fig. 4c). These results, obtained with antibodies specific for TRPV1, show that IGF-I (20 nM, 15 min), insulin (10 μM, 15 min) and PDBu (10 μM, 15 min), all significantly increased surface TRPV1 expressed in HEK cells (Fig. 4c). Fifth, similar results were seen in HEK cells transiently transfected with green fluorescence protein (GFP)-tagged TRPV1. Exposure of IGF-I (50 nM) significantly increased the fluorescence intensity of the membrane within five minutes, indicating the accumulation of TRPV1 on the membrane (Fig. 4d). Together, these data suggest the involvement of receptor translocation in TRPV1 current potentiation and show that, in the presence of insulin, TRPV1 is mobilized to the plasma membrane from the cytosol.
Insulin and IGF-I translocate TRPV1 to the plasma membrane. a, Potentiation of saturating concentrations of capsaicin response by insulin and PDBu. Application of 5, 10 and 20 μM capsaicin shows saturation of current response (a i ), exposure (2–5 min) of insulin (a ii ) or PDBu (a iii ) caused a 50% increase in current amplitude induced by 20 μM capsaicin (a iv ) (insulin n = 4 P < .01; PDBu n = 5 P > .01). b, Representative Western blot of surface protein and total TRPV1 from control and insulin-treated (10 μM, 15 min) HEK293 cells expressing TRPV1 (probed with anti-TRPV1 antibody). Surface represents fraction of biotinylated TRPV1 and total represents total amount of TRPV1 in immunoprecipitate. Quantitative analysis of insulin's effect on surface expression, with mean densities of surface bands normalized to control values for samples run on the same gel (n = 4, P < .01). c, Immunohistochemistry performed TRPV1 transfected HEK cells that were exposed to IGF-I (20 nM, 15 min), insulin (10 μM, 15 min) and PKC agonist, PDBu (10 μM, 15 min). Quantification of relative optical intensities (ROI, normalized as surface/cytosol for each cell): (control: n = 5; IGF-I: n = 7, P < .05; insulin: n = 3 P < .01; and PDBu: n = 7, P < .01). d, Confocal image showing a significant increase (3.17 ± 0.52 fold, n = 9; P < .01) in fluorescence intensity at the membrane 5 min after exposure to IGF-1 (50 nM) in HEK cells heterologously expressing GFP-TRPV1 fusion protein as compared to before IGF-1 application.
Discussion
From these results, we propose that insulin and its related growth factors provide both trophic and sensory support to peripheral nerve endings. Insulin and IGF-I can directly influence nociceptive ion channel function through phosphorylation and receptor translocation. In the presence of these modulators, TRPV1 is more responsive to painful stimuli (capsaicin, pH and heat) by increasing sensitivity and lowering thresholds. Based on this evidence, we conclude that insulin/IGF levels maintain TRPV1 function and their deficiency or resistance leads to deficits in inflammatory thermal sensation. The role of TRPV1 in animal models of diabetes has been suggested [27, 35–37]. The intriguing aspect is that insulin deficiency results in thermal hyperalgesia in streptozotocin induced diabetes. Sensitization of TRPV1 by phosphorylation could account for the hyperalgesic phenotype seen in this animal model of diabetes [35]. The exact mechanism of sensitization of TRPV1 is not clear, but could be due to over compensation by other tropic factors, such as NGF in response to insulin deficiency or elevated PKC activity in diabetes [38].
Using multiple methods, we elucidate molecular mechanism(s) by which insulin/IGF-I potentiate TRPV1 current (Fig. 3 and 4). These neurotrophic factors, operating through RTKs, trigger a signaling cascade leading to PI(3)K and PKC activation [27, 28, 35]. PKC, an enzyme known to sensitize TRPV1 through phosphorylation [5, 8, 31], increases channel activity and receptor translocation to the cell surface [39]. Activation of a similar pathway to insulin by NGF via PI(3)K has been shown to robustly potentiate TRPV1 current [40]. Since insulin/IGF-I levels and PKC activity are altered in diabetes, we speculate that abnormalities in TRPV1 function may contribute to neuropathy in diabetes.
In DRG sensory neurons, diminished growth factor levels are some of the earliest changes noticed with diabetic neuropathy [11, 20, 21]. One explanation for diabetic neuropathy states that it is, in essence, a microvascular disturbance [41]. Peripheral C fibers (which express TRPV1) release vasoactive substances like CGRP, causing small vessel dilation to increase cutaneous circulation and nerve terminal viability. Activation of TRPV1 has been shown to induce and enhance the release of CGRP (7). This neural component of microcirculatory control is decreased in diabetic neuropathy, and the consequent reduction in local blood flow contributes to peripheral vascular complications [41, 42]. With regards to growth factor deficiency, insulin has a vasodilatory effect that is dependent on CGRP release, which is compromised in diabetes [43, 44]. Our findings illustrates insulin/IGFs can cause vasodilation via their influence on TRPV1.
A concept is emerging where signals emanating from IR and/or IGFR can activate kinases with the potential to control ion channel phosphorylation, subcellular localization and overall expression. Our work elucidates the mechanism insulin/IGF-I use for TRPV1 sensitization (i.e. RTK→PI(3)K→PKC), but the transduction pathway regulating expression has not been identified. Previously, it was suggested that insulin exerts influences on the same neurons that are responsive to NGF by sharing common pathways [13]. Recent reports demonstrate that NGF and glial cell line-derived neurotrophic factor (GDNF) upregulate TRPV1 expression on DRG neurons using transduction mechanisms common to insulin/IGF-I (i.e. MAPKs, PI(3)K, Ras, etc.) [11, 40, 45, 46]. Taken together, these studies set precedence for growth factor influence on nociceptor levels and implicate signaling cascades, which may be compromised by the absence of insulin/IGF.
Insulin potentiates both whole cell and single channel currents mediated by NMDA receptors in Xenopus oocytes in a PKC-dependent manner [47]. Moreover, this effect was found to be due to membrane translocation involving both PI(3)K and PKC [33, 34, 38]. In DRG neurons insulin increased capsaicin induced cobalt uptake [48]. Along these same lines, insulin can potentiate currents in HEK293 cells through recruitment of GABAA receptors to postsynaptic domains [32]. In cultured cerebellar granular cells, IGF-I potentiates kinate receptors through a PI(3)K dependent mechanism [49].
Furthermore, vanilloid receptors (VRs) are present throughout the body, widely believed to have functions other than temperature sensation. TRPV1 expressed in the central terminals of the sensory neurons robustly modify synaptic transmission [50, 51]. TRPV1 could be detected using RT-PCR technique throughout the neuroaxis [52] and identification of specific ligands such as NADA in certain brain regions confirms a role in the CNS [53]. The nature of the receptors involved in this response and their role in the CNS are not clearly understood, but suggestive of a direct or indirect role in modifying neurotransmitter release [54]. TRPV1 is also located in vasculature, bronchi and urinary bladder [7, 55, 56]. Modulation of these receptors by lack of insulin and IGF-I may contribute to CNS disturbances, cardiovascular, respiratory and urinary complications resulting from diabetes.
Lastly, these findings emphasize the importance of maintaining proper insulin levels and suggest a potential benefit of IGF-I administration in the treatment and prevention of diabetic complications. We propose that insulin and IGF-I therapy, partially working through TRPV1, can improve complications associated with diabetes mellitus.
References
Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, Julius D: The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 1997, 389: 816–824. 10.1038/39807
Baumann TK, Martenson ME: Extracellular protons both increase the activity and reduce the conductance of capsaicin- gated channels. J Neurosci 2000, 20: RC80.
Julius D, Basbaum AI: Molecular mechanisms of nociception. Nature 2001, 413: 203–210. 10.1038/35093019
Di Marzo V, Blumberg PM, Szallasi A: Endovanilloid signaling in pain. Curr Opin Neurobiol 2002, 12: 372–379. 10.1016/S0959-4388(02)00340-9
Cesare P, McNaughton P: A novel heat-activated current in nociceptive neurons and its sensitization by bradykinin. Proc Natl Acad Sci USA 1996, 93: 15435–15439. 10.1073/pnas.93.26.15435
Lopshire JC, Nicol GD: The cAMP transduction cascade mediates the prostaglandin E2 enhancement of the capsaicin-elicited current in rat sensory neurons, whole-cell and single-channel studies. J Neurosci 1998, 18: 6081–6092.
Zygmunt PM, Petersson J, Andersson DA, Chuang H, Sorgard M, Di Marzo V, Julius D, Hogestatt ED: Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature 1999, 400: 452–457. 10.1038/22761
Premkumar LS, Ahern GP: Induction of vanilloid receptor channel activity by protein kinase C. Nature 2000, 408: 985–990. 10.1038/35050121
De Petrocellis L, Harrison S, Bisogno T, Tognetto M, Brandi I, Smith GD, Creminon C, Davis JB, Geppetti P, Di Marzo V: The vanilloid receptor (VR1)-mediated effects of anandamide are potently enhanced by the cAMP-dependent protein kinase. J Neurochem 2001, 77: 1660–1663. 10.1046/j.1471-4159.2001.00406.x
Chuang HH, Prescott ED, Kong H, Shields S, Jordt SE, Basbaum AI, Chao MV, Julius D: Bradykinin and nerve growth factor release the capsaicin receptor from PtdIns(4,5)P2-mediated inhibition. Nature 2001, 411: 957–962. 10.1038/35082088
Ji R, Samad TA, Jin S, Schomll R, Woolf CJ: p38 MAPK activation by NGF in primary sensory neurons after inflammation increases TRPV1 levels and maintains heat hyperalgesia. Neuron 2002, 36: 57–68. 10.1016/S0896-6273(02)00908-X
Patel NJ, Llewelyn JG, Wright DW, Thomas PK: Glucose and leucine uptake by rat dorsal root ganglia is not insulin sensitive. J Neurol Sci 1994, 121: 159–162. 10.1016/0022-510X(94)90345-X
Recio-Pinto E, Rechler MM, Ishii DN: Effects of insulin, insulin-like growth factor-II, and nerve growth factor on neurite formation and survival in cultured sympathetic and sensory neurons. J Neurosci 1986, 6: 1211–1219.
Fernyhough P, Willars GB, Lindsay RM, Tomlinson DR: Insulin and insulin-like growth factor I enhance regeneration in cultured adult rat sensory neurons. Brain Res 1993, 607: 117–124. 10.1016/0006-8993(93)91496-F
Sugimoto K, Murakawa Y, Sima AF: Expression and localization of insulin receptor in rat dorsal root ganglion and spinal cord. J Per Ner Sys 2002, 7: 44–53. 10.1046/j.1529-8027.2002.02005.x
Sheetz MJ, King GL: Molecular understanding of hyperglycemia's adverse effects for diabetic complications. JAMA 2002, 288: 2579–2588. 10.1001/jama.288.20.2579
The Diabetes Control and Complications Trial Research Group: The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993, 329: 977–986. 10.1056/NEJM199309303291401
Delaney CA, Mouser JV, Westerman RA: Insulin sensitivity and sensory nerve function. Clin Exp Neurol 1994, 31: 19–37.
Ishii DN, Lupien SB: Insulin-like growth factors protect against diabetic neuropathy: effects on sensory nerve regeneration in rats. J Neurosci Res 1995, 40: 138–144. 10.1002/jnr.490400116
Migdalis IN, Kalogeropoulou K, Kalantzis L, Nounopoulos C, Bouloukos A, Samartzis M: Insulin-like growth factor-I and IGF-I receptors in diabetic patients with neuropathy. Diabet Med 1995, 12: 823–827.
Craner MJ, Klein JP, Black JA, Waxman SG: Preferential expression of IGF-I in small DRG neurons and down-regulation following injury. Neuroreport 2002, 13: 1649–1652. 10.1097/00001756-200209160-00016
Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S, Kojima Y, Furuyoshi N, Shichiri M: Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract 1995, 28: 103–117. 10.1016/0168-8227(95)01064-K
Apfel SC, Kessler JA, Adornato BT, Litchy WJ, Sanders C, Rask CA: Recombinant human nerve growth factor in the treatment of diabetic polyneuropathy. Neurology 1998, 51: 695–702.
Delaney CA, Murchie KJ, Westerman RA, de Courten MP: Rapid actions of insulin on sensory nerve function. Neuroreport 1998, 9: 2775–2779.
Forst T, Pohlmann T, Kunt T, Goitom K, Schulz G, Lobig M, Engelbach M, Beyer J, Pfutzner A: The influence of local capsaicin treatment on small nerve fibre function and neurovascular control in symptomatic diabetic neuropathy. Acta Diabetol 2002, 39: 1–6. 10.1007/s005920200005
Pierson CR, Zhang W, Murakawa Y, Sima AF: Insulin deficiency rather than hyperglycemia accounts for impaired neurotrophic responses and nerve fiber regeneration in type 1 diabetic neuropathy. J Neuropathol Exp Neurol 2003, 62: 260–271.
Premkumar LS, Van Buren J, Bhat S, Rotello R, Smith S, Puntambekar P, Ramkumar V, Pauza ME: Functional impairment of TRPV1 in diabetic peripheral neuropathy. Neurosci Abst 2003, 381.9.
Karas M, Koval AP, Zick Y, Leroith D: The insulin-like growth factor I receptor-induced interaction of insulin receptor substrate-4 and Crk-II. Endocrinology 2001, 142: 1835–1840. 10.1210/en.142.5.1835
De Meyts P, Wallach B, Christoffersen CT, Urso B, Gronskov K, Latus LJ, Yakushiji F, Ilondo MM, Shymko RM: The insulin-like growth factor-I receptor. Structure, ligand-binding mechanism and signal transduction. Horm Res 1994, 42: 152–169.
Zhu L, Ohan N, Agazie Y, Cummings C, Farah S, Liu XJ: Molecular cloning and characterization of Xenopus insulin-like growth factor-1 receptor: its role in mediating insulin-induced Xenopus oocyte maturation and expression during embryogenesis. Endocrinology 1998, 139: 949–954. 10.1210/en.139.3.949
Numazaki M, Tominaga T, Toyooka H, Tominaga M: Direct phosphorylation of capsaicin receptor VR1 by protein kinase C epsilon and identification of two target serine residues. J Biol Chem 2002, 277: 13375–13378. 10.1074/jbc.C200104200
Wan Q, Xiong ZG, Man HY, Ackerley CA, Braunton J, Lu WY, Becker LE, MacDonald JF, Wang YT: Recruitment of functional GABA(A) receptors to postsynaptic domains by insulin. Nature 1997, 388: 686–690. 10.1038/41792
Kanzaki M, Zhang YQ, Mashima H, Li L, Shibata H, Kojima I: Translocation of a calcium-permeable cation channel induced by insulin-like growth factor-I. Nat Cell Biol 1999, 1: 165–170. 10.1038/11086
Skeberdis VA, Lan J, Zheng X, Zukin RS, Bennett MV: Insulin promotes rapid delivery of N-methyl-D-aspartate receptors to the cell surface by exocytosis. Proc Natl Acad Sci USA 2001, 98: 3561–3566. 10.1073/pnas.051634698
Hong S, Wiley JW: Early painful diabetic neuropathy is associated with differential changes in the expression and function of vanilloid receptor 1. J Biol Chem 2005, 280: 618–627. 10.1074/jbc.M413753200
Kamei J, Zushida K, Morita K, Sasaki M, Tanaka S: Role of vanilloid VR1 receptor in thermal allodynia and hyperalgesia in diabetic mice. Eur J Pharmacol 2001, 422: 83–86. 10.1016/S0014-2999(01)01059-7
Rashid MH, Inoue M, Kondo S, Kawashima T, Bakoshi S, Ueda H: Novel expression of vanilloid receptor 1 on capsaicin-insensitive fibers accounts for the analgesic effect of capsaicin cream in neuropathic pain. J Pharmacol Exp Ther 2003, 304: 940–948. 10.1124/jpet.102.046250
Eichberg J: Protein kinase C changes in diabetes: is the concept relevant to neuropathy? Int Rev Neurobiol 2002, 50: 61–82.
Morenilla-Palao C, Planells-Cases R, Garcia-Sanz N, Ferrer-Montiel A: Regulated exocytosis contributes to protein kinase C potentiation of vanilloid receptor activity. J Biol Chem 2004, 279: 25665–25672. 10.1074/jbc.M311515200
Zhuang ZY, Xu H, Clapham DE, Ji RR: Phosphatidylinositol 3-kinase activates ERK in primary sensory neurons and mediates inflammatory heat hyperalgesia through TRPV1 sensitization. J Neurosci 2004, 24: 8300–8309. 10.1523/JNEUROSCI.2893-04.2004
Way KJ, Katai N, King GL: Protein kinase C and the development of diabetic vascular complications. Diabet Med 2001, 18: 945–959. 10.1046/j.0742-3071.2001.00638.x
Kilo S, Berghoff M, Hilz M, Freeman R: Neural and endothelial control of the microcirculation in diabetic peripheral neuropathy. Neurology 2000, 54: 1246–1252.
Parkhouse N, Le Quesne PM: Impaired neurogenic vascular response in patients with diabetes and neuropathic foot lesions. N Engl J Med 1988, 318: 1306–1309.
Salem N, Dunbar JC: The insulin-mediated vascular and blood pressure responses are suppressed in CGRP-deficient normal and diabetic rats. Diabetes Metab Res Rev 2002, 18: 238–244. 10.1002/dmrr.293
Cheng HL, Feldman EL: Bidirectional regulation of p38 kinase and c-Jun N-terminal protein kinase by insulin-like growth factor-I. J Biol Chem 1998, 273: 14560–14565. 10.1074/jbc.273.23.14560
Kimpinski K, Mearow K: Neurite growth promotion by nerve growth factor and insulin-like growth factor-I in cultured adult sensory neurons: role of phospoinositide 3-kinase and mitogen activated protein kinase. J Neurosci Res 2001, 63: 486–499. 10.1002/jnr.1043
Liao GY, Leonard JP: Insulin modulation of cloned mouse NMDA receptor currents in Xenopus oocytes. J Neurochem 1999, 73: 1510–1519. 10.1046/j.1471-4159.1999.0731510.x
Sathianathan V, Avelino A, Charrua A, Santha P, Matesz K, Cruz F, Nagy I: Insulin induces cobalt uptake in a subpopulation of rat cultured primary sensory neurons. Eur J Neurosci 2003, 18: 2477–2486. 10.1046/j.1460-9568.2003.03004.x
Gonzalez de la Vega A, Buno W, Pons S, Garcia-Calderat MS, Garcia-Galloway E, Torres-Aleman I: Insulin-like growth factor I potentiates kainate receptors through a phosphatidylinositol 3-kinase dependent pathway. Neuroreport 2001, 12: 1293–1296. 10.1097/00001756-200105080-00047
Tognetto M, Amadesi S, Harrison S, Creminon C, Trevisani M, Carreras M, Matera M, Geppetti P, Bianchi A: Anandamide excites central terminals of dorsal root ganglion neurons via vanilloid receptor-1 activation. J Neurosci 2001, 21: 1104–1109.
Baccei ML, Bardoni R, Fitzgerald M: Development of nociceptive synaptic inputs to the neonatal rat dorsal horn: glutamate release by capsaicin and menthol. J Physiol 2003, 549: 231–242. 10.1113/jphysiol.2003.040451
Mezey E, Toth ZE, Cortright DN, Arzubi MK, Krause JE, Elde R, Guo A, Blumberg PM, Szallasi A: Distribution of mRNA for vanilloid receptor subtype 1 (VR1), and VR1-like immunoreactivity, in the central nervous system of the rat and human. Proc Natl Acad Sci USA 2000, 97: 3655–3660. 10.1073/pnas.060496197
Huang SM, Bisogno T, Trevisani M, Al-Hayani A, De Petrocellis L, Fezza F, Tognetto M, Petros TJ, Krey JF, Chu CJ, Miller JD, Davies SN, Geppetti P, Walker JM, Di Marzo V: An endogenous capsaicin-like substance with high potency at recombinant and native vanilloid VR1 receptors. Proc Natl Acad Sci USA 2002, 99: 8400–8405. 10.1073/pnas.122196999
Marinelli S, Di Marzo V, Berretta N, Matias I, Maccarrone M, Bernardi G, Mercuri NB: Presynaptic facilitation of glutamatergic synapses to dopaminergic neurons of the rat substantia nigra by endogenous stimulation of vanilloid receptors. J Neurosci 2003, 23: 3136–3144.
Manzini S: Bronchodilatation by tachykinins and capsaicin in the mouse main bronchus. Br J Pharmacol 1992, 105: 968–972.
Birder LA, Kanai AJ, de Groat WC, Kiss S, Nealen ML, Burke NE, Dineley KE, Watkins S, Reynolds IJ, Caterina MJ: Vanilloid receptor expression suggests a sensory role for urinary bladder epithelial cells. Proc Natl Acad Sci USA 2001, 98: 13396–13401. 10.1073/pnas.231243698
Acknowledgements
We thank R. Khardori for critical reading of the manuscript. cDNA clones were gifts from D. Julius, M. Tominaga and N. Kadei. This work was supported with a grant from NIH (DK065742, NSO42296 to L.S.P) and SIU Excellence in Academic Medicine (M.E.P. and L.S.P).
Author information
Authors and Affiliations
Corresponding author
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Van Buren, J.J., Bhat, S., Rotello, R. et al. Sensitization and translocation of TRPV1 by insulin and IGF-I. Mol Pain 1, 17 (2005). https://doi.org/10.1186/1744-8069-1-17
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1744-8069-1-17