Abstract
Background
Reliability of quantitative gait assessment while dual-tasking (walking while doing a secondary task such as talking) in people with cognitive impairment is unknown. Dual-tasking gait assessment is becoming highly important for mobility research with older adults since better reflects their performance in the basic activities of daily living. Our purpose was to establish the test-retest reliability of assessing quantitative gait variables using an electronic walkway in older adults with mild cognitive impairment (MCI) under single and dual-task conditions.
Methods
The gait performance of 11 elderly individuals with MCI was evaluated using an electronic walkway (GAITRite® System) in two sessions, one week apart. Six gait parameters (gait velocity, step length, stride length, step time, stride time, and double support time) were assessed under two conditions: single-task (sG: usual walking) and dual-task (dG: counting backwards from 100 while walking). Test-retest reliability was determined using intra-class correlation coefficient (ICC). Gait variability was measured using coefficient of variation (CoV).
Results
Eleven participants (average age = 76.6 years, SD = 7.3) were assessed. They were high functioning (Clinical Dementia Rating Score = 0.5) with a mean Mini-Mental Status Exam (MMSE) score of 28 (SD = 1.56), and a mean Montreal Cognitive Assessment (MoCA) score of 22.8 (SD = 1.23). Under dual-task conditions, mean gait velocity (GV) decreased significantly (sGV = 119.11 ± 20.20 cm/s; dGV = 110.88 ± 19.76 cm/s; p = 0.005). Additionally, under dual-task conditions, higher gait variability was found on stride time, step time, and double support time. Test-retest reliability was high (ICC>0.85) for the six parameters evaluated under both conditions.
Conclusion
In older people with MCI, variability of time-related gait parameters increased with dual-tasking suggesting cognitive control of gait performance. Assessment of quantitative gait variables using an electronic walkway is highly reliable under single and dual-task conditions. The presence of cognitive impairment did not preclude performance of dual-tasking in our sample supporting that this methodology can be reliably used in cognitive impaired older individuals.
Similar content being viewed by others
Background
A large body of research has demonstrated an important interdependence between gait and cognition in elderly people noting that slow motor performance is associated with cognitive impairment and dementia [1–5]. Walking is a complex learned task that becomes automatic for most people from early childhood onwards. However, there is evidence that cognitive control of gait becomes increasingly important in older adults[6, 7]. Since a seminal study demonstrated that the inability to maintain a conversation while walking is a marker for future falls in older adults[8], walking while performing a secondary task (dual-task paradigm) has become a classic way to assess the relationship between cognition and gait Because the dual-task paradigm is a realistic proxy for daily living activities that seniors may perform at home, it is growing in interest and application in clinical research settings.
Although previous studies have reported good test-retest reliability using electronic walkways while assessing gait in older people without performing a secondary task [9–11], the reliability of quantitative gait assessment under dual-task conditions among those with cognitive problems has not been established. One of the challenges faced when assessing cognitively impaired older adults is their potential inability to perform dual-tasking properly, thereby increasing measurement error. Therefore, our objective was to determine the reliability of quantitative gait assessment under both single and dual-task conditions in people with mild cognitive impairment (MCI) using a one-week space between assessments. This timeframe is appropriate for research purposes in this population, since gait variables are stable over short intervals. Establishing the reliability of quantitative gait assessment under dual-task conditions among those with cognitive problems is an important first step in validating this methodology for future longitudinal studies.
Methods
Subjects
Thirteen subjects were recruited from the Aging Brain and Memory Clinic (ABMC) at Parkwood Hospital, St. Joseph's Health Care, London, Ontario. Inclusion criteria were age 65 years and older, a diagnosis of MCI, and ability to communicate in English. Participants were diagnosed with MCI if they[12]: did not have dementia.[13], had objective memory impairment, experienced subjective memory symptoms corroborated by an informant, and had preserved activities of daily living (defined in our study as being able to perform basic and instrumental activities of daily living as evaluated by Lawton Brody Scale[14]). An additional MCI criterion was to have a Clinical Dementia Rating Scale (CDR) of 0.5[15].
Exclusion criteria included any objective gait disorder due to Parkinson's disease, previous stroke, clinical osteoarthritis in lower limbs joints, myopathy, or neuropathy as verified by a formal clinical examination. The presence of depressive symptoms, defined as a score ≥ 5/15 on the Geriatric Depression Scale[16], was also an exclusion criterion since depression may affect gait performance[16]. The Health Sciences Research Ethics Board at The University of Western Ontario approved the study. Subjects who consented to participate underwent a comprehensive medical examination by experienced geriatricians. Co morbidities, medications, falls in the previous 12 months, and fear of falling were recorded. Global cognitive status was assessed using the Mini Mental Status Exam (MMSE; scored 0-30)[17] and the Montreal Cognitive Assessment (MoCA; scored 0-30), a validated tool that was originally created to assist in the diagnosis of MCI[18]. A pattern of a low MoCA score (<26) with a normal MMSE score (>26) is associated with having MCI[18].
Procedures
Each participant's gait performance was assessed using an electronic walkway system (GAITRite®) under a single (three trails) and a dual-task (three trails) condition per session over two sessions, spaced one week apart. Three trials per condition was found in the power analysis to be the optimum number of trials needed to obtain enough number of strides to be able to compute reliability assessment for the quantitative gait variables of interests[19]
The GAITRite® system includes a portable electronic walkway mat (600 cm in length and 64 cm in width) for the automated measurement of spatiotemporal gait parameters. As participants walk along the mat, imbedded sensors are activated by the foot pressure and is deactivated when the pressure is released. A computer processed the footsteps, providing data for both spatial and temporal parameters. The following six gait variables were selected based on their clinical relevance and their reported association with cognitive function in previous aging studies[5, 16, 20, 21]: gait velocity (cm/s), step length (cm), stride length (cm), step time (sec), stride time (sec), and double support time (sec). Gait parameters were recorded using only the footprint of the participants, thereby eliminating the need for external sensors attached to the body or lower limbs that may interfere with the gait performance.
GAITRite® system resolution is in milliseconds for time parameters and in millimeters for distances and lengths parameters. The mat was located in a well-lit, 10-meter long hallway with starting and ending limits marked one meter from the mat to avoid recording acceleration and deceleration phases.
Gait assessments
Prior to the trials, participants were giving standardized instructions and a visual demonstration. Then, participants were asked to perform three single-task trials and three dual-task trials. The single task trials consisted of walking the length of the mat at self-selected pace (sG). For the dual-task trials, participants walked the length of the mat while counting backward from one hundred by one aloud (dG). This dual-task condition was selected based on previous research which demonstrated that counting backwards requires both working memory and attention[22]. There was no instruction to prioritize either gait or cognitive task; however, if a participant stopped either task during the trial they were prompted to continue. Allowing both aspects to vary, gait and cognitive task, has previously been shown to better represent the dynamics of daily living tasks of older adults[23, 24].
Data acquisition of the quantitative gait variables
GAITRite software Version 3.8 was used to process the footstep data using the settings for light and short footsteps as individuals with MCI may be more likely to slow down or hesitate while dual-tasking. If a participant's first or last footstep did not fall completely within the active area of the walkway these footstep were manually removed from the recorded walk. Further, to minimize environmental variability, evaluations were conducted on the same weekday (± 1 day) and at the same time of day, with participants instructed to wear the same pair of shoes for both sessions.
Statistical analysis
Baseline characteristics and gait parameters were summarized using either means and standard deviations, or frequencies and percentages, as appropriate. For each gait parameter and for both conditions, the mean of the three trials was used in the analysis. Three trials was found to be the optimum number of trials needed to obtain enough number of strides to be able to compute reliability assessment for the quantitative gait variables of interests[19]. Comparisons between means obtained during sG and dG conditions were performed using a paired t-test. To quantify gait variability under both single and dual-task conditions, the coefficient of variation[25] (CoV = SD/mean*100) of each gait variable was calculated at each time point.
The Intraclass Correlation Coefficient (ICC), based on a two-way random effects analysis of variance, was used to quantify test-retest reliability. To interpret ICC values we used bench marks suggested by Cicchetti (if ICC<0.40, the level of clinical significance is "poor;" between 0.40 and 0.59 is "fair;" between 0.60 and 0.74 is "good;" and between 0.75 and 1.00 the level of clinical significance is "excellent."[26]). We preferred ICC to evaluate test-retest reliability over a standard correlation analysis because ICC accounts for differences between data sets by using analysis of variance. The level of statistical significance was set at 0.05 and analyses were conducted using SPSS version 15.0 (SPSS Inc., Chicago IL).
Results
Of the 13 individuals recruited from the ABMC, 2 were excluded due to gait-affecting comorbidities yielding a final study group of 11 participants. Demographic and medical characteristics are summarized in Table 1. In brief, they were five males and six females, with a mean age of 76.6 years (SD = 7.3). They were high functioning in terms of instrumental activities of daily living with a mean Lawton-Brody = 7.18 out of 8 (SD = 1.06) with higher scores indicating better functionality Four participants had experienced a fall in the preceding 12 months. Global cognitive functioning pattern was consistent with the diagnosis of MCI[18].
At baseline assessment (week 1), mean gait velocity under single-task conditions (sG) was significantly faster than the gait velocity under dual-task conditions (dG) (sG = 119.11 vs. dG = 110.88 cm/s, p = 0.005, Table 2). This mean decrement of 8.23 cm/s, a seven-percent change, is considered a clinically significant change in gait velocity[6, 27]. At Week 2, although gait velocity decreased under dG conditions, the difference in velocity was not statistically significant (sG: 113.18 vs. dG: 111.84 cm/s, p = 0.579).
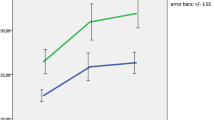
Gait variability results are expressed as CoV in Table 2. Of the six parameters analyzed, only step and stride time have significantly increased during dual-task condition and with considerable stride-to-stride variability. In fact, the CoV for stride time increased from 6.36 on sG to 11.02 on dG in week-one assessment. As shown in Figure 1, under dual task conditions, there was an increase in the CoV for the variables related to time: step, stride, and double support time. For these time-related variables, the CoV increased by 63.13%, 73.27%, and 36.82% respectively from sG to dG conditions, while the CoV for the remaining gait variables increased by less than 6%.
Reliability results are shown in Table 2. Under single task conditions, re-test reliability was excellent with the ICCs for six gait variables being 0.83 or higher with the exception of double support time, which was 0.80. Reliability results under dual-task conditions were also excellent with ICCs for the six gait measures were 0.93 or higher.
Discussion
This study established the test-retest reliability of gait assessment under single and dual-task conditions in older adults with MCI. There is excellent reliability in both conditions over a one-week time span. Reliability of gait assessment in older adults has been reported previously[11, 20, 28]; however, to our knowledge, this is the first report which determined the reliability under dual-task conditions in mildly cognitively impaired older people. Due to the growing importance of dual-task paradigm in current research of cognitive decline, falls, and dementia [29–31], our results are of particular relevance since the presence of cognitive impairment in our population did not preclude performance of dual-tasking while gait assessment.
The ICCs for the six variables analyzed under single and dual-task were higher than 0.75, showing excellent clinical reliability for the assessment of these spatial and temporal gait parameters.
One interesting finding of our study is that the time required to perform steps and strides significantly increased under the dual-task condition. This is consistent with previous studies, which have demonstrated that these parameters have a greater dependence on brain cortical control than other gait parameters[25, 31]. In addition, step and stride time showed a greater variability under dual-task conditions when compared with the other parameters analyzed (Table 2, Figure 1). This finding is particularly relevant given that gait variability under dual-tasking has been demonstrated to be an early predictor of future falls[8] In our sample of people with Mild Cognitive Impairment, gait variability significantly increased under dual-task conditions. While gait variability is minimal under dual-task conditions for the general population, high gait variability is associated with Parkinson disease, Alzheimer's disease and other dementias, a variety of types of dementias and is a predictor of future falls[25, 30, 31]. Since our results confirm the reliability of this assessment in persons with MCI, this type of assessment may be an effective early measure of detecting individuals with MCI who are at higher risk of future falls. Increased gait variability represents a more unstable walking pattern with less rhythmicity. We postulate that this altered gait pattern is a type of "arrhythmia" of the gait and may correlate to other health outcomes such as future dementias, falls or other comorbidities.
Particularly, our results provide support to apply this methodology in people with cognitive problems. Although gait has long been considered as primarily an automatic motor task, emerging evidence suggests that this view may be overly simplistic[32]. Cortical brain control may play a key role in the regulation of even routine walking, specifically through attention. Attention is a necessary cognitive resource for maintaining normal walking and attentional deficits are independently associated with postural instability, impairment in performing daily living activities, and future falls[24]. Specifically, dual-tasking cost has been traditionally related to the prefrontal cortical regions[33]. These brain regions are crucially involved in the mediation of the division of attention and executive function. Functional neuroimaging studies showed correlations between dual-task performance with increase activity in prefrontal areas, cingulate, parietal and premotor areas[34, 35]. Therefore, we postulate that those regions may have a control on gait in older individuals. In line with previous studies, our results support the hypothesis that occupying these areas with concurrent cognitive processing (dual-tasking) may result in a brain resource limitation that affects gait in people with MCI.
Strengths of our study include the use of a well-defined population that met strict criteria for MCI, and the use of established and validated measures of cognition using a sophisticated quantitative gait assessment. The small sample size of our study, however, is a potential limitation, as it may not represent the full spectrum of MCI population. Despite these limitations, this study provides evidence that quantitative gait analysis while dual-tasking among older adults with MCI is a reliable methodology.
Conclusion
In older adults with MCI, assessment of quantitative gait variables using an electronic walkway was highly reliable under single and dual-task conditions. In line with previous studies conducted in elderly with normal cognition, variability of time-related gait parameters increased while dual-tasking in our sample. The presence of cognitive impairment did not preclude performance of dual-tasking gait assessment in our sample; therefore, this methodology can be reliably used in older people with MCI.
References
Camicioli R, Howieson D, Oken B, Sexton G, Kaye J: Motor slowing precedes cognitive impairment in the oldest old. Neurology 1998, 50: 1496-1498.
Allan LM, Ballard CG, Burn DJ, Kenny RA: Prevalence and severity of gait disorders in Alzheimer's and non-Alzheimer's dementias. J Am Geriatr Soc 2005, 53: 1681-1687.
Holtzer R, Verghese J, Xue X, Lipton RB: Cognitive processes related to gait velocity: results from the Einstein Aging Study. Neuropsychology 2006, 20: 215-223. 10.1037/0894-4105.20.2.215
Pettersson AF, Olsson E, Wahlund LO: Motor function in subjects with mild cognitive impairment and early Alzheimer's disease. Dement Geriatr Cogn Disord 2005, 19: 299-304. 10.1159/000084555
van Iersel MB, Hoefsloot W, Munneke M, Bloem BR, Olde Rikkert MG: Systematic review of quantitative clinical gait analysis in patients with dementia. Z Gerontol Geriatr 2004, 37: 27-32. 10.1007/s00391-004-0176-7
Alexander NB: Gait disorders in older adults. J Am Geriatr Soc 1996, 44: 434-451.
Woollacott M, Shumway-Cook A: Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture 2002, 16: 1-14. 10.1016/S0966-6362(01)00156-4
Lundin-Olsson L, Nyberg L, Gustafson Y: "Stops walking when talking" as a predictor of falls in elderly people. Lancet 1997, 349: 617. 10.1016/S0140-6736(97)24009-2
Bilney B, Morris M, Webster K: Concurrent related validity of the GAITRite walkway system for quantification of the spatial and temporal parameters of gait. Gait Posture 2003, 17: 68-74. 10.1016/S0966-6362(02)00053-X
Cutlip RG, Mancinelli C, Huber F, DiPasquale J: Evaluation of an instrumented walkway for measurement of the kinematic parameters of gait. Gait Posture 2000, 12: 134-138. 10.1016/S0966-6362(00)00062-X
Menz HB, Latt MD, Tiedemann A, Mun SK, Lord SR: Reliability of the GAITRite walkway system for the quantification of temporo-spatial parameters of gait in young and older people. Gait Posture 2004, 20: 20-25. 10.1016/S0966-6362(03)00068-7
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E: Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 1999, 56: 303-308. 10.1001/archneur.56.3.303
American Psychiatric, Association: Diagnostic and Statistical Manual of Mental Disorders (Text Revision; [DSV-IV-TR]). Washington, DC 4th edition. 2000.
Lawton MP, Brody EM: Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9: 179-186.
Morris JC: The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 1993, 43: 2412-2414. 10.1111/j.1532-5415.2005.53433_4.x
van Iersel MB, Haitsma A, Olde Rikkert MG, Benraad CE: Quantitative gait analysis to detect gait disorders in geriatric patients with depression. J Am Geriatr Soc 2005, 53: 1441-1442. 10.1016/0022-3956(75)90026-6
Folstein MF, Folstein SE, McHugh PR: "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975, 12: 189-198. 10.1111/j.1532-5415.2005.53221.x
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al.: The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005, 53: 695-699. 10.1002/sim.4780060404
Donner A, Eliasziw M: Sample size requirements for reliability studies. Stat Med 1987, 6: 441-448. 10.1111/j.1532-5415.2007.01130.x
van Iersel MB, Benraad CE, Rikkert MG: Validity and reliability of quantitative gait analysis in geriatric patients with and without dementia. J Am Geriatr Soc 2007, 55: 632-634. 10.1136/jnnp.2006.106914
Verghese J, Wang C, Lipton RB, Holtzer R, Xue X: Quantitative gait dysfunction and risk of cognitive decline and dementia. J Neurol Neurosurg Psychiatry 2007, 78: 929-935. 10.1093/brain/117.4.715
Hittmair-Delazer M, Semenza C, Denes G: Concepts and facts in calculation. Brain 1994,117(Pt 4):715-728. 10.1016/j.apmr.2006.10.007
Verghese J, Kuslansky G, Holtzer R, Katz M, Xue X, Buschke H, et al.: Walking while talking: effect of task prioritization in the elderly. Arch Phys Med Rehabil 2007, 88: 50-53. 10.1002/mds.21720
Yogev-Seligmann G, Hausdorff JM, Giladi N: The role of executive function and attention in gait. Mov Disord 2008, 23: 329-342. 10.1186/1743-0003-2-19
Hausdorff JM: Gait variability: methods, modeling and meaning. J Neuroengineering Rehabil 2005, 2: 19. 10.1037/1040-3590.6.4.284
Cicchetti DV: Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment 1994, 6: 284-290. 10.1093/ageing/18.5.327
Bendall MJ, Bassey EJ, Pearson MB: Factors affecting walking speed of elderly people. Age Ageing 1989, 18: 327-332. 10.1186/1471-2474-5-13
van Uden CJ, Besser MP: Test-retest reliability of temporal and spatial gait characteristics measured with an instrumented walkway system (GAITRite). BMC Musculoskelet Disord 2004, 5: 13. 10.1046/j.1532-5415.2003.51468.x
Bootsma-van der Wiel A, Gussekloo J, de Craen AJ, van Exel E, Bloem BR, Westendorp RG: Walking and talking as predictors of falls in the general population: the Leiden 85-Plus Study. J Am Geriatr Soc 2003, 51: 1466-1471. 10.1046/j.1532-5415.2003.51516.x
Sheridan PL, Solomont J, Kowall N, Hausdorff JM: Influence of executive function on locomotor function: divided attention increases gait variability in Alzheimer's disease. J Am Geriatr Soc 2003, 51: 1633-1637. 10.1002/mds.20848
Springer S, Giladi N, Peretz C, Yogev G, Simon ES, Hausdorff JM: Dual-tasking effects on gait variability: the role of aging, falls, and executive function. Mov Disord 2006, 21: 950-957. 10.1007/s00221-005-2280-3
Hausdorff JM, Yogev G, Springer S, Simon ES, Giladi N: Walking is more like catching than tapping: gait in the elderly as a complex cognitive task. Exp Brain Res 2005, 164: 541-548. 10.1093/cercor/7.1.63
Chao LL, Knight RT: Prefrontal deficits in attention and inhibitory control with aging. Cereb Cortex 1997, 7: 63-69. 10.1093/cercor/7.5.465
Klingberg T, O'Sullivan BT, Roland PE: Bilateral activation of fronto-parietal networks by incrementing demand in a working memory task. Cereb Cortex 1997, 7: 465-471. full_text
Klingberg T: Limitations in information processing in the human brain: neuroimaging of dual task performance and working memory tasks. Prog Brain Res 2000, 126: 95-102.
Acknowledgements
We are grateful for the thoughtful review of the manuscript from Dr. Denise Goens, Clinical Research Office at University of Western Ontario. This paper was presented at 2008 American Geriatric Society Meeting (Washington, DC), 2008 Canadian Geriatric Society Meeting (Montreal, QC). This study was funded by a research grant from the Glenn E Pratt Endowment Fund and the Lawson Health Research Institute at London, ON, Canada. Dr. Montero-Odasso is recipient of the Schulich Clinician-Scientist Award (2008-2011).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
Study concept and design (MMO and MB), acquisition of subjects and data (MMO, AC, MB, JW, PB), data analysis (MMO, KTH, IG), preparation of the manuscript (MMO, KTH), and critical review of the manuscript (MMO, KTH, AC, MB, JW, IG). All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Montero-Odasso, M., Casas, A., Hansen, K.T. et al. Quantitative gait analysis under dual-task in older people with mild cognitive impairment: a reliability study. J NeuroEngineering Rehabil 6, 35 (2009). https://doi.org/10.1186/1743-0003-6-35
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1743-0003-6-35