Abstract
Background
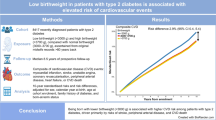
To investigate whether low birth weight increases the risk of myocardial infarction later in life in women.
Methods
Nationwide population-based case-control study. Patients and controls: 152 patients with a first myocardial infarction before the age of 50 years in the Netherlands. 568 control women who had not had a myocardial infarction stratified for age, calendar year of the index event, and area of residence.
Results
Birth weight in the patient group was significantly lower than in control women (3214 vs. 3370 gram, mean difference -156.3 gram (95%CI -9.5 to -303.1). The odds ratio for myocardial infarction, associated with a birth weight lower than 3000 gram (20th percentile in controls) compared to higher than 3000 gram was 1.7 (95%CI 1.1–2.7), while the odds ratio for myocardial infarction for children with a low birth weight (< 2000 g) compared to a birth weight ≥ 2000 g was 2.4 (95%CI 1.0 – 5.8). Both figures did not change after adjustment for putative confounders (age, education level, body mass index, waist-hip ratio, hypertension, diabetes, hypercholesterolemia, smoking, and family history of cardiovascular disease).
Conclusions
Low birth weight is associated with an increased risk of myocardial infarction before age of 50 in Dutch women.
Similar content being viewed by others
Background
Intrauterine malnutrition, as reflected by birth weight and abnormal thinness at birth, has been associated with an increased incidence of risk factors for arterial disease, i.e. hypertension, impaired glucose tolerance, diabetes and to a lesser extent hyperlipidemia and body fat distribution in adulthood [1–10]. This observation has become known as the 'fetal origins of adult disease' or 'Barker hypothesis', which suggests that several of the major diseases of later life, including coronary heart disease, stroke and cardiovascular death, originate in impaired intrauterine growth and development [11, 12]. In cohort studies, Barker [13–15] in England and Finland, Rich-Edwards et al. [16] as part of the Nurses' Health Study in the USA and Leon et al. [17] from Uppsala in Sweden showed an inverse relationship between birth weight and the clinical endpoint ischemic heart disease. Leon et al. [17] found a significant relationship only among male singletons and adjusted their results for gestational age and socioeconomic confounding. The association was not found in a cohort study from Gothenburg [18].
Our aim was to investigate the association in a case control study among Dutch women.
Methods
The RATIO (Risk of Arterial Thrombosis In relation to Oral contraceptives) study is a population-based case-control study on myocardial infarction in relation to oral contraceptive use among women aged 18 to 49 years in the Netherlands [19]. An additional standardized questionnaire was sent to all 218 patients and 769 controls from whom also blood samples had been taken for determination of metabolic risk factors (diabetes and hypercholesterolemia). Questions elicited information on birth weight, waist and hip circumference and data on the menstrual cycle. For 13 women no current address could be found (12 patients, 1 control). Four women had died since the index date (2 patients, 2 controls), which was the date of the first myocardial infarction for the patients and the midyear for the controls. One hundred and fifty two patients (71%) and 568 controls (75%) responded to the questionnaire and women were asked to measure their waist and hip circumference. Body mass index (BMI) was calculated as body weight (kg) divided by height squared (m2). Waist-hip-ratio was calculated as waist circumference divided by hip circumference.
Multiple linear and unconditional logistic regression were used to analyze the data. Odds ratios for the relationship between birth weight and myocardial infarction were calculated and 95% confidence intervals (95%CI) were derived from the models. Birth weights were categorized according to quintiles in control women in order to investigate an association between birth weight and the risk of myocardial infarction later in life. These were <3000 g, 3000 to 3199 g, 3200 to 3499 g, 3500 to 3883 g, and >3884 g, respectively. To determine whether women with a lower birth weight had a higher risk for a myocardial infarction, patients were divided in a group with a birth weight equally or higher than 2000 g and a group with a birth weight lower 2000 g [20]. Odds ratios were adjusted for age, education level, body mass index, waist-hip ratio, hypertension, diabetes, hypercholesterolemia, smoking, and family history of cardiovascular disease, when appropriate. Interaction between low birth weight and low education level was investigated by computing a dummy variable.
Results
The characteristics of 152 women with myocardial infarction and 568 control women at the index date are shown in Table 1. At the moment of completing the questionnaire, patients were aged 32–59 years (mean 50), and control women 25–60 years (mean 47). The mean body mass index was 25.1 kg/m2 for the patients and 23.4 kg/m2 for control women, mean difference 1.76 kg/m2 (95%CI 1.05–2.47), p < 0.001. Ninety-seven patients (64%) and 415 (73%) controls could give their birth weight. Compared with control women, patients had a significantly lower mean birth weight (3214 vs. 3370 g, mean difference -156.3 g (95%CI -9.5 to -303.1). The odds ratio for myocardial infarction for children with a low birth weight (< 2000 g) compared to a birth weight ≥ 2000 g was 2.4 (95%CI 1.0 to 5.8). After adjustment for putative confounders (age, education level, body mass index, waist-hip ratio, hypertension, diabetes, hypercholesterolemia, smoking, and family history of cardiovascular disease) the odds ratio did not change. Odds ratios for myocardial infarction in different categories of birth weight as compared to the reference category (birth weight higher than 3884 g) were 1.3 (95%CI 0.5–3.3) for a birth weight 3500 to 3883 g, 1.4 (95%CI 0.6–3.4) for a birth weight 3200 to 3499 g, 1.7 (95%CI 0.6–5.1) for a birth weight 3000 to 3199 g, and 2.3 (95%CI 1.0–5.4) for a birth weight lower than 3000 g (Table 2). The risk of myocardial infarction was 6.2 fold increased (95%CI 2.7–13.9) among women with low birth weight and a low educational level compared to women with a high birth weight and a high educational level (reference category).
Discussion
In this case control study we have found that women with a low birth weight had a higher risk of myocardial infarction than women with a higher birth weight. The data confirm the association found in cohort studies [13–17] and as such support the 'fetal origins of adult disease' or 'Barker hypothesis'.
A limitation of the study is that we have no information on gestational age. However, recently it has been demonstrated that both children who had been born prematurely and children who are small for gestational age had a reduction in insulin resistance [21, 22]. The self-report of birth weights as well as the rather high percentage of missing values for birth weight may also limit the study, but the random events among cases and controls cannot explain our results. Socio-economic factors associated with low birth weight are also associated to risk factors for arterial disease later in life. As pointed out by several others, it will be nearly impossible to disentangle these effects [16, 17].
In the present study we confirmed an interactive effect between low birth weight and a low educational level on the risk of myocardial infarction in women. However, when we adjusted for age, education level, body mass index, waist-hip ratio, hypertension, diabetes, hypercholesterolemia, smoking, and family history of cardiovascular disease, factors of which some may partly been seen as (the result of) socio-economic/environmental and genetic factors, we still observed an association between low birth weight and a higher risk of myocardial infarction. This is in agreement with others who also found that genetic and socio-economic circumstances at birth and in adult life can not completely explain the association between low birth weight and disease late in life [10, 16, 17, 23–25].
Among the proposed underlying biological mechanisms to explain the association is impaired endothelial development. Already at very young age, individuals with low birth weight exhibit endothelial dysfunction that persists into childhood and adult life, suggesting that endothelial dysfunction precedes the development of vascular related diseases later in life and represents the link between low birth weight and these diseases [26–32]. Furthermore, Smith et al. [33] found that mothers, who once gave birth to thin babies, have a higher risk of developing ischemic heart disease later in life. Therefore, these mothers seem to have, just as their children, an impaired endothelial function. If the impaired endothelial function is already manifest during the process of implantation, it might lead to inadequate development of the vasculature in the maternal part of the placenta, which enfeebles the function of the placenta resulting in low birth weight.
Conclusions
In conclusion, our study shows that a low birth weight (<2000 g) is associated with a 2.4 fold higher risk of myocardial infarction before the age of 50 as compared with a birth weight ≥ 2000 g. Because the risk of cardiovascular disease is known to increase with an increasing number of risk factors, women with a low birth weight should try to avoid acquired risk factors, like smoking and obesity. In addition, extra attention should be given in detecting diabetes or hypertension at a later stage in life and in detecting exaggerated growth during childhood, as these individuals seem most prone to develop disease later on in life [[34–36]].
References
Barker DJ, Osmond C, Golding J, Kuh D, Wadsworth ME: Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ. 1989, 298: 564-567.
Barker DJ, Bull AR, Osmond C, Simmonds SJ: Fetal and placental size and risk of hypertension in adult life. BMJ. 1990, 301: 259-262.
Hales CN, Barker DJ, Clark PM, Cox LJ, Fall C, Osmond C, Winter PD: Fetal and infant growth and impaired glucose tolerance at age 64. BMJ. 1991, 303: 1019-1022.
Barker DJ, Meade TW, Fall CH, Lee A, Osmond C, Phipps K, Stirling Y: Relation of fetal and infant growth to plasma fibrinogen and factor VII concentrations in adult life. BMJ. 1992, 304: 148-152.
Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM: Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia. 1993, 36: 62-67. 10.1007/BF00399095.
Valdez R, Athens MA, Thompson GH, Bradshaw BS, Stern MP: Birthweight and adult health outcomes in a biethnic population in the USA. Diabetologia. 1994, 37: 624-631.
McCance DR, Pettitt DJ, Hanson RL, Jacobsson LT, Knowler WC, Bennett PH: Birth weight and non-insulin dependent diabetes: thrifty genotype, thrifty phenotype, or surviving small baby genotype?. BMJ. 1994, 308: 942-945.
Whincup P, Cook D, Papacosta O, Walker M: Birth weight and blood pressure: cross sectional and longitudinal relations in childhood. BMJ. 1995, 311: 773-776.
Stein CE, Fall CH, Kumaran K, Osmond C, Cox V, Barker DJ: Fetal growth and coronary heart disease in south India. Lancet. 1996, 348: 1269-1273. 10.1016/S0140-6736(96)04547-3.
Frankel S, Elwood P, Sweetnam P, Yarnell J, Smith GD: Birthweight, body-mass index in middle age, and incident coronary heart disease. Lancet. 1996, 348: 1478-1480. 10.1016/S0140-6736(96)03482-4.
Barker DJ: Fetal origins of coronary heart disease. BMJ. 1995, 311: 171-174.
Paneth N, Susser M: Early origin of coronary heart disease (the "Barker hypothesis"). BMJ. 1995, 310: 411-412.
Barker DJ, Winter PD, Osmond C, Margetts B, Simmonds SJ: Weight in infancy and death from ischaemic heart disease. Lancet. 1989, 2: 577-580. 10.1016/S0140-6736(89)90710-1.
Osmond C, Barker DJ, Winter PD, Fall CH, Simmonds SJ: Early growth and death from cardiovascular disease in women. BMJ. 1993, 307: 1519-1524.
Eriksson JG, Forsen T, Tuomilehto J, Winter PD, Osmond C, Barker DJ: Catch-up growth in childhood and death from coronary heart disease: longitudinal study. BMJ. 1999, 318: 427-431.
Rich-Edwards JW, Stampfer MJ, Manson JE, Rosner B, Hankinson SE, Colditz GA, Willett WC, Hennekens CN: Birth weight and risk of cardiovascular disease in a cohort of women followed up since 1976. BMJ. 1997, 315: 396-400.
Leon DA, Lithell HO, Vagero D, Koupilova I, Mohsen R, Berglund L, Lithell UB, McKeigue PM: Reduced fetal growth rate and increased risk of death from ischaemic heart disease: cohort study of 15 000 Swedish men and women born 1915–29. BMJ. 1998, 317: 241-245.
Eriksson M, Tibblin G, Cnattingius S: Low birthweight and ischaemic heart disease. Lancet. 1994, 343: 731-10.1016/S0140-6736(94)91610-1.
Tanis BC, Van Den Bosch MA, Kemmeren JM, Cats VM, Helmerhorst FM, Algra A, Van Der Graaf Y, Rosendaal FR: Oral contraceptives and the risk of myocardial infarction. N Engl J Med. 2001, 345: 1787-1793. 10.1056/NEJMoa003216.
World Health Organization: Low birth weight. A tabulation of available information. WHO Geneva. 1992
Bazaes RA, Alegria A, Pittaluga E, Avila A, Iniguez G, Mericq V: Determinants of insulin sensitivity and secretion in very-low-birth-weight children. J Clin Endocrinol Metab. 2004, 89: 267-272. 10.1210/jc.2003-031239.
Hofman PL, Regan F, Jackson WE, Jefferies C, Knight DB, Robinson EM, Cutfield WS: Premature birth and later insulin resistance. N Engl J Med. 2004, 351: 2179-2186. 10.1056/NEJMoa042275.
Frankel S, Elwood P, Sweetnam P, Yarnell J, Smith GD: Birthweight, adult risk factors and incident coronary heart disease: the Caerphilly Study. Public Health. 1996, 110: 139-143. 10.1016/S0033-3506(96)80066-7.
Barker DJ, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS: Fetal nutrition and cardiovascular disease in adult life. Lancet. 1993, 341: 938-941. 10.1016/0140-6736(93)91224-A.
Poulter NR: Birthweights, maternal cardiovascular events, and Barker hypothesis. Lancet. 2001, 357: 1990-1991. 10.1016/S0140-6736(00)05131-X.
Martin H, Gazelius B, Norman M: Impaired acetylcholine-induced vascular relaxation in low birth weight infants: implications for adult hypertension?. Pediatr Res. 2000, 47: 457-462.
Goh KL, Shore AC, Quinn M, Tooke JE: Impaired microvascular vasodilatory function in 3-month-old infants of low birth weight. Diabetes Care. 2001, 24: 1102-1107.
Leeson CP, Whincup PH, Cook DG, Donald AE, Papacosta O, Lucas A, Deanfield JE: Flow-mediated dilation in 9- to 11-year-old children: the influence of intrauterine and childhood factors. Circulation. 1997, 96: 2233-2238.
Martin H, Hu J, Gennser G, Norman M: Impaired endothelial function and increased carotid stiffness in 9-year-old children with low birthweight. Circulation. 2000, 102: 2739-2744.
Leeson CP, Kattenhorn M, Morley R, Lucas A, Deanfield JE: Impact of low birth weight and cardiovascular risk factors on endothelial function in early adult life. Circulation. 2001, 103: 1264-1268.
Goodfellow J, Bellamy MF, Gorman ST, Brownlee M, Ramsey MW, Lewis MJ, Davies DP, Henderson AH: Endothelial function is impaired in fit young adults of low birth weight. Cardiovasc Res. 1998, 40: 600-606. 10.1016/S0008-6363(98)00197-7.
McAllister AS, Atkinson AB, Johnston GD, McCance DR: Relationship of endothelial function to birth weight in humans. Diabetes Care. 1999, 22: 2061-2066.
Smith GC, Pell JP, Walsh D: Pregnancy complications and maternal risk of ischaemic heart disease: a retrospective cohort study of 129,290 births. Lancet. 2001, 357: 2002-2006. 10.1016/S0140-6736(00)05112-6.
Oren A, Vos LE, Uiterwaal CS, Gorissen WH, Grobbee DE, Bots ML: Birth weight and carotid intima-media thickness: new perspectives from the atherosclerosis risk in young adults (ARYA) study. Ann Epidemiol. 2004, 14: 8-16. 10.1016/S1047-2797(03)00068-1.
Forsen T, Eriksson J, Tuomilehto J, Reunanen A, Osmond C, Barker DJ: The fetal and childhood growth of persons who develop type 2 diabetes. Ann Intern Med. 2000, 133: 176-182.
Yajnik C: Interactions of perturbations in intrauterine growth and growth during childhood on the risk of adult-onset disease. Proc Nutr Soc. 2000, 59: 257-265.
Acknowledgements
This work was supported by the Netherlands Heart Foundation (97-063).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
BT participated in the design, execution and analysis of the RATIO- study and drafted the manuscript.
KK analyzed the data and drafted the manuscript.
RH collected the data and performed statistical analyses.
FR initiated the study and helped to draft the manuscript.
FH participated in the design of the study and the writing of the paper.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Tanis, B.C., Kapiteijn, K., Hage, R.M. et al. Dutch women with a low birth weight have an increased risk of myocardial infarction later in life: a case control study. Reprod Health 2, 1 (2005). https://doi.org/10.1186/1742-4755-2-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1742-4755-2-1