Abstract
With the continuing march of the AIDS epidemic and little hope for an effective vaccine in the near future, work to develop a topical strategy to prevent HIV infection is increasingly important. This stated, the track record of large scale "microbicide" trials has been disappointing with nonspecific inhibitors either failing to protect women from infection or even increasing HIV acquisition. Newer strategies that target directly the elements needed for viral entry into cells have shown promise in non-human primate models of HIV transmission and as these agents have not yet been broadly introduced in regions of highest HIV prevalence, they are particularly attractive for prophylaxis. We review here the agents that can block HIV cellular entry and that show promise as topical strategies or "virustats" to prevent mucosal transmission of HIV infection
Similar content being viewed by others
Introduction: the compelling need for prevention of HIV infection
As the pandemic spread of HIV infection and AIDS continues, there is increasing need to develop strategies for its containment. Since sexual transmission of HIV infection is the most important route of transmission throughout the world [1], approaches to limit transmission by this route are especially needed. To date, there is reason to believe that three prevention strategies work in this arena, but there are limits to their implementation. First it is a tautology that avoidance of sex will result in a decrease in sexual transmission of HIV. Despite innumerable campaigns encouraging abstinence or monogamy and some indications that some of these campaigns might have had limited effect [2], we haven't yet figured out a way to convince ourselves that avoidance of sex is better than having it when the opportunity arises. Likewise, while there is strong evidence that regular use of condoms will decrease the risk of HIV transmission by at least 80% [3], there is often resistance to their use for reasons that may relate to perceptions of pleasure, perceptions of trust and fidelity, social norms, and of access and opportunity [4]. Finally while there is strong evidence that male circumcision will decrease the risk of HIV acquisition by half or more [5–7], broad "roll-out" of circumcision has not yet been implemented. Though this is likely to be remedied soon and should have measureable impact on HIV spread, protection is not complete and additional methods of prevention will surely be needed
While a vaccine that is capable of providing sterilizing immunity to HIV is rightly the goal of intensive research, vaccine candidates plausibly capable of inducing such protection are not nearly within reach and in fact there is only limited insight into what it will take to design such candidates [8, 9]. Thus there is compelling need to develop additional effective strategies for the prevention of sexual transmission of HIV.
We should no longer develop "Microbicides" for the prevention of HIV infection
The term "microbicide" has been used to describe agents that can be applied topically to mucosal surfaces in order to prevent HIV transmission. We think that the term is both inaccurate and misleading and should not be used in polite company (at least not when discussing HIV prevention). We outline below why we would like to see this word take its rightful place beside "impact" (the verb) and the thoughtless "gerundification" of perfectly proper nouns such as "text" and "parent".
First, the most promising topical strategies to prevent HIV transmission are not microbicidal in so far as they do not kill microbes (or viruses for that matter). They achieve their effect by blocking HIV replication through interference with either a viral or a host element that is necessary for viral propagation. Second (and this is where even words can be dangerous), those agents that were in fact microbicidal (i.e., they destroyed viruses and other microbes in the test tube) have been disastrous failures in the clinic, in large part because they were broadly "microbicidal". There was early hope that topical application of a single agent might kill or otherwise render non-infectious HIV as well as a variety of other sexually transmissible pathogens. Unfortunately, the agents that had this broad killing activity were primarily soaps or detergents that dissolved the microbial cell wall or membrane. This activity was predictably toxic to human cells as the lipid membrane that surrounds the HIV capsid is always derived from the human cell in which the virions were produced. This hazard turned out to be significant in the clinic as topical application of the detergent N-9 not only failed to protect against HIV acquisition, but also likely increased infection risk as a result of toxicity to the vaginal mucosal surface [10]. A further trial of another microbicide detergent -SAVVY- nearly doubled the risk of HIV acquisition among recipients (hazard ratio 1.7), but with few events, these differences were not significant (CI = 0.9–3.5) [11]. Despite these predictably discouraging results, other detergents are still being studied with the aim of preventing HIV transmission. Such studies make us very anxious.
We would propose, therefore, that the term "microbicide" not be used when discussing HIV prevention. Instead, perhaps, a complex but more accurate phrase could be "topical prevention strategies," or even the simpler term "virustats," since the most promising agents effectively block HIV from replicating but do not "kill" it. This proposal may be a losing battle as there is something to be gained from branding a term and acknowledging its wide recognition by both the scientific and the lay communities. Nonetheless, one of the major advantages to writing a review article (and there are many downsides) is that you can pick your own battles and hope that others might see it your way.
What topical prevention strategies might be implemented to prevent sexual transmission of HIV?
The viral replication cycle offers a number of opportunities for intervention to prevent HIV acquisition [12–15]. We will focus this piece on strategies that block HIV entry into cells, strategies that to us are among the most attractive for prevention. Strategies targeting later points in the viral replication cycle also are quite plausible but with some limitations as will be discussed below.
HIV entry into host cells
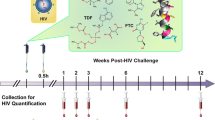
HIV cellular invasion is a complicated process coordinated by the sequential binding of the viral envelope to cellular receptors (Figure 1). The responsible viral component, Env, is a heavily glycosylated, trimeric protein composed of two subunits, gp120 and gp41. Initial cellular capture of the virus is achieved through Env glycans that bind cellular lectins (DC-Sign and related C-type lectins)[16]. For some special antigen-presenting cells (mucosal dendritic cells), captured virions can be conveyed to a protected cellular compartment, enabling infectious HIV to be transported in situ to adjacent lymphoid tissue containing an abundance of infectable target cells [17]. On susceptible target cells, the Env-lectin interactions keep the virus close to the membrane, facilitating the binding of gp120 to its primary receptor, CD4[18]. This event induces a structural change in gp120 that exposes new surfaces capable of binding 7-transmembrane G-protein-coupled chemokine receptors (referred to as HIV coreceptors). In humans, the key coreceptors utilized by HIV are CCR5 and CXCR4, even though numerous other chemokine receptors appear to support infection in vitro. Interestingly, almost all cases of acute infection involve CCR5-using HIV. Consequently, individuals lacking cell surface-expressed CCR5 (owing to a 32-base pair deletion in the open reading frame of both alleles) are almost completely protected from acquiring HIV infection [19, 20]. In the rare instances in which these individuals have been found to be HIV positive, the viruses were shown to utilize CXCR4 for cellular entry [21–32].
HIV entry and its inhibition. In the native conformation of Env, a canopy of three gp120 molecules (green) covers gp41, holding the trimer in a metastable conformation. Binding to cellular lectins (black) keeps Env close to the cellular membrane, facilitating subsequent interactions with CD4 (orange) and a chemokine receptor (CoR, purple). These gp120/receptor interactions trigger gp41 to extend and insert its N-terminal fusion peptide segment (red) into the target cell membrane. Ultimately, the exposed heptad repeat segments in the N- and C-terminal regions of the gp41 ectodomain [labeled N (gray) and C (blue)] associate to form the trimer-of-hairpins structure, juxtaposing viral and cellular membranes in a manner crucial for membrane fusion. HIV entry inhibitors investigated as potential topical prevention strategies are listed in red below each modeled transition.
The interactions between gp120 and cellular receptors trigger a series of conformational transitions in gp41 that ultimately lead to the fusion of viral and cellular membranes. Initially, gp41 extends to insert its N-terminal "fusion peptide" segment into the target cell membrane [33]. Because gp41 already contains a transmembrane region embedded in the viral envelope, this high energy, extended conformation essentially bridges the space between target cell and virus. Driven by the tight association of heptad-repeat (HR) segments in its N- and C-terminal regions, the gp41 ectodomain eventually collapses into a compact structure known as a trimer-of-hairpins[34]. Formation of the gp41 trimer-of-hairpins brings the fusion peptide, the transmembrane region and their associated membranes into the close proximity required for the fusion process. Although evidence supports the gp120-CD4 interaction initiating gp41 structural changes, the precise role of gp120-coreceptor interaction in promoting formation of the gp41 trimer-of-hairpins remains a mystery [35, 36].
Strategies to block HIV entry into cells
Blocking the entry of HIV into target cells should be an effective mechanism to neutralize HIV infectivity since cellular infection and use of cellular machinery are necessary for production of new viruses. Entry can be blocked by targeting either the viral envelope glycoprotein, or host elements such as CD4 or CCR5.
Inhibition of HIV replication by targeting the HIV envelope
Polyanions
A variety of negatively charged polyanions such as cellulose sulfate, dextran sulfate, carageenan and PRO-2000 are capable of binding to the HIV envelope and preventing cellular infection. In part because these agents are inexpensive to make and showed some in vitro activity, a number of them were accelerated into development as topical prevention strategies. Unfortunately, these agents tend to be far more active against the more positively charged CXCR4-using (X4-tropic) viruses than they are against the CCR5-using (R5-tropic) viruses that are responsible for most instance of HIV transmission [37, 38]. In fact both dextran sulfate and cellulose sulfate can actually increase HIV infectivity in vitro [39, 40], and plasma levels of HIV were increased in persons receiving treatment with dextran sulfate in vivo [41]. Thus, it is not surprising that several large placebo-controlled trials of these agents have failed to demonstrate protection against HIV infection [40]. In some instances, HIV transmission may even have been increased in persons receiving cellulose sulfate. Although one arm of a polyanion (PRO-2000) trial is still ongoing and we do not know yet whether this approach will prove useful, the poor track record of trials with other anions and the recent termination of the higher dose arm of this same PRO-2000 trial for futility tempers enthusiasm for this approach. On the other hand, the relationship between in vitro enhancement of infection and in vivo protection remains unclear. A recent study confirmed in vitro enhancement of infection by the polyanion carageenan but showed significant protection from SHIV vaginal challenge in rhesus macaques [42]. At the same time, this agent failed to protect women from HIV infection in a large randomized controlled clinical trial [43]. How much of this relates to the activity of the agent, the durability of its protection or the consistency of its application in the clinical trial remains to be determined. SPL 7013 is a polylysine based polyanionic dendrimer with naphthalene disulfonic acid surface groups that when formulated as a 5% gel protected 6 of 6 pigtailed macaques from infection with the predominantly CXCR4 tropic SHIV 89.6 [44]. Similar in vitro antiviral activity was reported against both SHIV 89.6 and the R5 tropic SHIV 163P3 [44] but to date, no in vivo challenge studies using an R5 tropic virus have been reported.
Lectins
Cyanovirin and griffithisin are small lectins that demonstrate potent in vitro activity against HIV replication [45, 46]. They appear to bind Env glycans and interfere with cellular entry, most likely by blocking viral capture through cellular C-type lectins and/or interfering with gp120 binding to cellular CD4 and coreceptor. Cyanovirin is a 101 amino-acid protein produced by the cyanobacterium Nostoc ellipsosporum. Its gene has been inserted into lactobacilli that are common residents among the vaginal microbiota [47]. Sustained expression of cyanovirin by these bacteria within the vagina may provide some protection against vaginal acquisition of HIV infection, but this observation remains to be shown in a relevant animal model. Griffithisin is a 121 amino-acid protein derived from the algae Griffithsia and is currently being explored as a candidate for topical prevention of HIV transmission [48]. Immunogenicity is a potential issue for these foreign proteins after repeated topical application. Moreover, there is the additional risk that these lectins will bind to and crosslink glycoproteins present on immune cell surfaces, potentially activating these cells nonspecifically and stimulating mitogenic activity [49]. How much of a problem these concerns will be remains to be determined.
Monoclonal antibodies
In many viral infections, antibodies that can neutralize infectivity have the ability to provide sterilizing immunity against infection. Although neutralizing antibodies are readily demonstrable in the plasmas of persons who acquire HIV infection, these antibodies are typically type-specific and virus escapes rapidly from neutralizing activity [50, 51]. A small number of human or "humanized" broadly neutralizing monoclonal antibodies (mAb) have been developed that bind to limited regions of the HIV envelope [52]. Of these, mAb b12, which recognizes the CD4 binding domain of HIV gp120, provided partial protection (9 of 12 animals protected) in the rhesus vaginal challenge model [53]. Two others, mAbs 2F5 (which targets the C-terminal region of the gp41 ectodomain) and 2G12 (which recognizes sugar moieties on gp120) also provided partial protection when co-administered systemically in combination with polyclonal anti-HIV immunoglobulin [54]. The virus utilized in these studies, however, was SHIV 89.6, which predominantly uses CXCR4 for entry. (It should be noted that in these latter studies, the antibodies were not applied topically). Such antibodies are costly to produce in large scale because they must be generated in mammalian cells capable of post-translational modification. Nonetheless, their activity in vivo demonstrates that targeting these regions of the viral envelope might provide a plausible topical protection strategy for a product that is simpler to make. In addition, as newer technologies are being developed to express biologically active antibodies or their fragments (see for example [55, 56]), these approaches may become increasingly affordable and practicable.
BMS 377806
This small molecule binds to gp120 and interferes with cellular receptor interactions, thereby blocking infectivity [57]. While there is still some uncertainty as to the precise mechanism of activity of this agent, it provides substantial protection (6 of 8 animals protected) when used alone and, when used in combination with other entry inhibitors, can provide complete protection [58].
Inhibitors of gp41
Agents that disrupt gp41 conformational changes required for HIV membrane fusion effectively inhibit viral entry[34]. The best characterized are linear peptides originally derived from the C-terminal heptad repeat segment (C-HR) and adjacent membrane-proximal region of the gp41 ectodomain [59, 60]. These so-called C-peptides bind the gp41 N-terminal heptad repeat segment (N-HR) exposed in the extended, prehairpin intermediate conformation of the ectodomain [34]. Once bound, they block association of N-HR and C-HR segments, thereby disrupting trimer-of-hairpins formation and inhibiting viral membrane fusion. While C-peptides are only effective during a short kinetic window between CD4-gp120 binding and trimer-of-hairpins formation, they can possess potent (low nanomolar) antiviral activity in vitro. With parenteral administration of 90 to 180 mg/day, the 36-mer C-peptide enfuvirtide (T-20) can effectively suppress HIV replication in humans and is currently used as a salvage therapy for HIV-1 infected individuals [61] Surprisingly, the effectiveness of enfuvirtide as a topical protective agent against mucosal HIV transmission has not been reported. However, the second generation agent T-1249 and an extended C-peptide C52L have been shown to effectively reduce HIV mucosal transmission in macaque studies [62, 63]. As a monotherapy, T-1249 completely protected against infection following vaginal SHIV challenge, but only at concentrations in excess of 100 μM. For C52L, concentrations as high as 1.5 mM only afforded protection in 60% of challenged animals. However, the activity of C52L is enhanced in combination with other antiviral agents (especially inhibitors of coreceptor binding), consistent with the synergistic activity between C-peptides and different HIV entry inhibitors observed in vitro [64, 65]. As with cyanovirin, mucosal bacteria secreting C-peptides have been generated, but whether colonization with these microorganisms can protect against HIV transmission remains to be tested [66].
The 5 order-of-magnitude disparity in C-peptide potencies determined from in vitro infectivity experiments and from vaginal challenge studies is disconcerting, and its cause unknown. Similar differences are also observed for entry inhibitors of different classes, leading many investigators to speculate that these observations reflect some intrinsic difficulty in delivering inhibitors to sites where they need to act [67]. Two aspects of C-peptide inhibition compound this problem. First, C-peptides target an intermediate state during the entry process and, thus, must be present at high levels at the site of viral infection[34]. They do not bind the Env native state prior to CD4 interaction, and they do not work on target cells. Where in the vaginal mucosa HIV first encounters and infects target cells remains unknown, but such events are likely to take place in the deep epithelium or submucosa. Hence, to effectively block all mucosal transmission, C-peptides must passively diffuse a significant distance through the vaginal epithelium and surrounding tissue. Second, C-peptides are unstructured in solution and readily susceptible to proteolysis [68]. The vaginal milieu and surrounding tissues are full of proteases that can potentially limit the bioavailability these antiviral agents. To date, the search for non-peptide, small molecule gp41 inhibitors has not yielded compounds with sufficient antiviral potency. Recently, however, protease-insensitive peptides composed of d-amino acids (D-peptides) have been developed that target a small region of the N-terminal HR segment [69, 70]. Crosslinked versions of these D-peptides show potent, broad-spectrum inhibitory activity and represent promising candidates for a future topical antiviral strategy.
Inhibition of HIV replication by targeting host cell surface receptors
Blockade of CD4
In principal, blockade of CD4 by targeting the envelope binding domain of the HIV receptor should decrease HIV infectivity and one humanized monoclonal antibody, TNX-355 (Ibalizumab) has demonstrated antiretroviral activity in HIV infected persons after systemic administration [71], however there do not appear to be plans to develop this reagent as a topical prevention strategy.
Blockade of CCR5
Since the original discovery that CCR5 and CXCR4 are critical to HIV entry [72–78], major effort has been devoted to developing reagents that target these coreceptors and disrupt their interactions with gp120 [13, 79]. To date, efforts to develop CCR5 inhibitors have been much more successful than strategies targeting CXCR4. From the standpoint of a topical prevention strategy, CCR5 inhibition appears to be much more important as almost all cases of new infection are caused by R5-tropic viruses. This point is underscored by the rarity of HIV infected individuals who lack surface-expressed CCR5. Nonetheless, there was no certainty that mucosal blockade of CCR5 would be sufficient to provide protection against HIV transmission. Viruses captured by DC-SIGN (or related C-type lectins) on certain submucosal dendritic cells might be transported and presented for trans-infection to CD4+ CCR5+ immune cells found deeper within the body. Thus it was important to learn that topical blockade of CCR5 was sufficient to provide very high level [58] or complete [80] protection against vaginal transmission of the R5 tropic SHIV 16P3.
There are now three strategies to block HIV replication by targeting CCR5. Humanized monoclonal antibodies have been developed that bind to CCR5 and block its interaction with the HIV envelope. Both HGS 004 and PRO 140 have been given systemically to persons with HIV infection and have demonstrable antiretroviral activity in vivo [81, 82]. Neither is being developed for topical application. A number of small molecule allosteric inhibitors of CCR5 have been developed for systemic administration; one of these, maraviroc, has been approved for treatment of HIV infection, and another, vicriviroc, has demonstrated in vivo efficacy [83, 84]. A third small molecule CCR5 inhibitor, CMPD 167 (Merck), is not being developed for systemic administration but has shown protective activity in the rhesus vaginal challenge model [58]. The advantages to developing these small molecule CCR5 inhibitors as topical agents to prevent HIV infection include 1) the rigorous safety testing that they have undergone during trials of systemic administration, 2) the fact that they are relatively inexpensive to produce and 3) their lack of agonist activity on the chemokine receptor. In fact, these molecules block the agonist activity of natural chemokine ligands and, thus, are expected to be anti-inflammatory. Conceivably, this property might protect the vaginal mucosa from the inflammation caused by concurrent bacterial vaginosis [85] or sexually transmissible infections [86] that have been linked to enhanced risk for HIV acquisition.
A third mechanism by which CCR5 can be targeted to block mucosal HIV transmission is by application of their natural or modified chemokine ligands. By experimental modification of the amino terminus of RANTES, Robin Offord and Oliver Hartley have developed a series of RANTES analogues with substantially greater antiretroviral activity than the native molecule [87]. The first lead molecule to be tested in the non-human primate vaginal challenge model, PSC-RANTES, has several non-natural amino acid residues of the amino terminus which are responsible for its antiretroviral activity at sub-nanomolar concentrations. PSC-RANTES is an agonist of CCR5 and induces durable (at least 24 hrs) internalization of CCR5, rendering the coreceptor inaccessible to the viral envelope [87]. When tested in the rhesus vaginal challenge model, PSC-RANTES completely protected 12 of 12 animals from infection with SHIV 162P3 ([80] and Veazey, unpublished). Because the amino terminus of PSC- RANTES comprised non-natural amino acids, the molecule cannot be produced completely by biosynthesis, rendering cost of chemical synthesis an insurmountable obstacle for large scale production. For this reason, a novel phage display selection method was applied to develop recombinant RANTES variants with high level potency [88]. The selection strategy successfully identified two fully recombinant molecules, 5P12 and 6P4 RANTES, with the comparable in vitro antiviral potency to that of PSC-RANTES [89]. Morevoer, both fully recombinant molecules completely protected 5 of 5 challenged monkeys from SHIV 162P3 infection in the rhesus vaginal challenge model [90]. These new molecules are stable at high temperatures and are resistant to loss of biologic activity after exposure to vaginal and seminal fluids [91]. Because they are fully recombinant, it should be possible to produce them in sufficient bulk and affordably for distribution in the developing world where these agents are needed most. Interestingly, while having equipotent antiviral activity in vitro and in vivo, these two new molecules have distinctly different mechanisms of action. Similar to PSC-RANTES, 6P4-RANTES is a CCR5 agonist that activates cell signaling cascades and receptor internalization after binding. By contrast, 5P12-RANTES binding fails to properly activate the receptor (no observed changes in intracellular calcium levels) and does not promote CCR5 internalization. It remains to be seen whether simple receptor occupancy without cellular activation will prove a better topical prevention strategy than durable coreceptor internalization with induced cellular activation. Perhaps the ideal strategy will be one that promotes durable receptor internalization without signal transduction, and development of such a molecule may be achievable. Other G-protein-coupled receptors can be internalized by internalized by certain ligands without demonstrable agonist activation [92–95]. Already, one chemokine analog, 5P14-RANTES [96], has been identified that is as potent as PSC-RANTES, does not stimulate Ca2+ flux, but induces the sequestration of CCR5 with approximately half the efficiency of PSC-RANTES and 6P4-RANTES.
Combination strategies
Combination antiretroviral therapies have proven enormously successful in the treatment of established HIV infection. In fact, single agent strategies have invariably failed, in large part due to the predictable emergence of viruses that contain mutations conferring resistance to the antiviral drug. Though the principles are not exactly the same, there are solid rationales to the development of combination strategies for the topical prevention of HIV mucosal transmission. First, while emergence of resistance is unlikely to occur upon HIV exposure during sex with an infected partner, the increasing transmission of drug resistant viruses among newly infected persons [97, 98] may render some topical prevention strategies less effective (see below). Thus combinations of agents that disrupt different elements of the HIV life cycle may also provide a broader safety net of protection. Second, additive or synergistic activities might enhance the level of protection against the establishment of infection. Using SHIV 162P3 in a macaque vaginal challenge model, Veazey et al. have shown that combinations of agents that block viral entry provide better levels of protection than any single agent used alone [58]. While CMPD 167, C52L, BMS 378806 failed to completely protect challenged animals alone, combinations of two and all three of these agents proved fully protective. Unfortunately, before a single agent is proven to be safe and effective, there are practical (e.g. formulation) and registrational hurdles to the development of combinations of active agents as topical prevention strategies. We do not believe these hurdles to be insurmountable. Formulations compatible with multiple active agents can be developed and agencies charged with oversight of drug development can work closely with investigators to design and accelerate the pace of studies designed to test the safety and activity of plausible combination prevention strategies.
Additional comments
As has been stated by nearly every researcher in the field, a successful "microbicide" or topical prevention strategy must be safe, effective and affordable. There are currently a good number of promising candidates under development, including inhibitors of entry as well as inhibitors of other elements of the viral life cycle[12]. Unfortunately, the field (and public perceptions of the field) has been considerably damaged by a number of widely publicized dramatic failures of large test of efficacy studies, some of which have actually increased the risk of HIV transmission (reviewed in [99]). While the urgent need to halt the spread of the epidemic is real, the field needs to be more selective about which agents to bring forward into large efficacy studies. Candidates for topical prevention strategies must have a plausible chance for succeeding. Thus, they must be effective in preclinical studies that include protection of non-human primates from infection with an R5 tropic virus. The agents must be safe. Thus, they must be well tolerated after multiple applications in women who are at low risk for HIV infection and must not induce the inflammation that has been linked to an increased risk for HIV transmission. Ideally, they should not perturb the normal vaginal microbiota, nor increase risks for acquisition of other sexually transmissible infections. Finally, these drugs should have durable activity. Analyses from a failed prevention trial suggest that agents requiring application just prior to coitus are not likely to be used often enough to provide sufficient protection [100]. Thus, only strategies that provide substantial protection from infection for at least a full day or even longer are likely to prove effective in clinical settings. It remains to be seen whether durable protection can be provided by formulation in slow release gels or films or by application using vaginal rings that have been used for slow release of contraceptives[101, 102].
It may be problematic to apply a strategy for topical prevention in a community that is using the same strategy for treatment. First, the predictable emergence of resistance during therapy may render that strategy less effective when applied to prevent the initial acquisition of infection. Second, topical application of an antiviral drug by persons who are unknowingly infected may provide sufficient selection pressure systemically or even at mucosal and peri-mucosal sites of HIV replication to induce emergence of resistance, rendering subsequent treatment less effective. How much of an issue these concerns will be remains to be seen, but they provide some rationale for the need to develop different strategies for treatment and for prevention. Lastly, a major rate limiting step to the implementation of a topical HIV prevention strategy is the cost of development. The cost can be measured both in real dollars and in expertise. Most scientists engaged in this new area of prevention research are not experts in drug development. Those with the managerial and scientific expertise to bring a new drug to the clinic are found in the pharmaceutical industry, which, for the most part, has steered clear of topical HIV prevention strategies for market reasons. Getting these companies engaged in a substantive way might help accelerate the process.
References
AIDS U: AIDS Epidemic Update. UN AIDS. 2002, Geneva, Switzerland
Hattori MK, Dodoo FN: Cohabitation, marriage, and 'sexual monogamy' in Nairobi's slums. Soc Sci Med. 2007, 64: 1067-1078. 10.1016/j.socscimed.2006.10.005.
Weller S, Davis K: Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev. 2002, CD003255-
Pool R, Hart G, Green G, Harrison S, Nyanzi S, Whitworth J: Men's attitudes to condoms and female controlled means of protection against HIV and STDs in south-western Uganda. Cult Health Sex. 2000, 2: 197-211. 10.1080/136910500300804.
Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A: Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005, 2: e298-10.1371/journal.pmed.0020298.
Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, Williams CF, Campbell RT, Ndinya-Achola JO: Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007, 369: 643-656. 10.1016/S0140-6736(07)60312-2.
Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, Kiwanuka N, Moulton LH, Chaudhary MA, Chen MZ, et al: Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007, 369: 657-666. 10.1016/S0140-6736(07)60313-4.
Johnston MI, Fauci AS: An HIV Vaccine – Challenges and Prospects. N Engl J Med. 2008, 359: 888-890. 10.1056/NEJMp0806162.
Burton DR, Desrosiers RC, Doms RW, Feinberg MB, Gallo RC, Hahn B, Hoxie JA, Hunter E, Korber B, Landay A, et al: Public health. A sound rationale needed for phase III HIV-1 vaccine trials. Science. 2004, 303: 316-10.1126/science.1094620.
Hillier SL, Moench T, Shattock R, Black R, Reichelderfer P, Veronese F: In vitro and in vivo: the story of nonoxynol 9. J Acquir Immune Defic Syndr. 2005, 39: 1-8. 10.1097/01.qai.0000159671.25950.74.
Feldblum PJ, Adeiga A, Bakare R, Wevill S, Lendvay A, Obadaki F, Olayemi MO, Wang L, Nanda K, Rountree W: SAVVY vaginal gel (C31G) for prevention of HIV infection: a randomized controlled trial in Nigeria. PLoS ONE. 2008, 3: e1474-10.1371/journal.pone.0001474.
Klasse PJ, Shattock R, Moore JP: Antiretroviral drug-based microbicides to prevent HIV-1 sexual transmission. Annu Rev Med. 2008, 59: 455-471. 10.1146/annurev.med.59.061206.112737.
Kuhmann SE, Hartley O: Targeting chemokine receptors in HIV: a status report. Annu Rev Pharmacol Toxicol. 2008, 48: 425-461. 10.1146/annurev.pharmtox.48.113006.094847.
Lederman MM, Offord RE, Hartley O: Microbicides and other topical strategies to prevent vaginal transmission of HIV. Nat Rev Immunol. 2006, 6: 371-382. 10.1038/nri1848.
Shattock R: Microbicide development: multiple targets, multiple mechanisms. Retrovirology. 2006, 3 (Suppl 1): S49-10.1186/1742-4690-3-S1-S49.
Geijtenbeek TB, Kwon DS, Torensma R, van Vliet SJ, van Duijnhoven GC, Middel J, Cornelissen IL, Nottet HS, KewalRamani VN, Littman DR, et al: DC-SIGN, a dendritic cell-specific HIV-1-binding protein that enhances trans-infection of T cells. Cell. 2000, 100: 587-597. 10.1016/S0092-8674(00)80694-7.
Kwon DS, Gregorio G, Bitton N, Hendrickson WA, Littman DR: DC-SIGN-mediated internalization of HIV is required for trans-enhancement of T cell infection. Immunity. 2002, 16: 135-144. 10.1016/S1074-7613(02)00259-5.
McDonald D, Wu L, Bohks SM, KewalRamani VN, Unutmaz D, Hope TJ: Recruitment of HIV and its receptors to dendritic cell-T cell junctions. Science. 2003, 300: 1295-1297. 10.1126/science.1084238.
Margolis L, Shattock R: Selective transmission of CCR5-utilizing HIV-1: the 'gatekeeper' problem resolved?. Nat Rev Microbiol. 2006, 4: 312-317. 10.1038/nrmicro1387.
Moore JP, Kitchen SG, Pugach P, Zack JA: The CCR5 and CXCR4 coreceptors – central to understanding the transmission and pathogenesis of human immunodeficiency virus type 1 infection. AIDS Res Hum Retroviruses. 2004, 20: 111-126. 10.1089/088922204322749567.
Oh D-Y, Jessen H, Kücherer C, Neumann K, Oh N, Poggensee G, Bartmeyer B, Jessen A, Pruss A, Schumann RR, Hamouda O: CCR5Œî32 Genotypes in a German HIV-1 Seroconverter Cohort and Report of HIV-1 Infection in a CCR5Œî32 Homozygous Individual. PLoS ONE. 2008, 3: e2747-10.1371/journal.pone.0002747.
Sheppard HW, Celum C, Michael NL, O'Brien S, Dean M, Carrington M, Dondero D, Buchbinder SP: HIV-1 infection in individuals with the CCR5-Delta32/Delta32 genotype: acquisition of syncytium-inducing virus at seroconversion. J Acquir Immune Defic Syndr. 2002, 29: 307-313.
Iversen AK, Christiansen CB, Attermann J, Eugen-Olsen J, Schulman S, Berntorp E, Ingerslev J, Fugger L, Scheibel E, Tengborn L, et al: Limited protective effect of the CCR5Delta32/CCR5Delta32 genotype on human immunodeficiency virus infection incidence in a cohort of patients with hemophilia and selection for genotypic X4 virus. J Infect Dis. 2003, 187: 215-225. 10.1086/345881.
Michael NL, Nelson JA, KewalRamani VN, Chang G, O'Brien SJ, Mascola JR, Volsky B, Louder M, White GC, Littman DR, et al: Exclusive and persistent use of the entry coreceptor CXCR4 by human immunodeficiency virus type 1 from a subject homozygous for CCR5 delta32. J Virol. 1998, 72: 6040-6047.
Gray L, Churchill MJ, Keane N, Sterjovski J, Ellett AM, Purcell DF, Poumbourios P, Kol C, Wang B, Saksena NK, et al: Genetic and functional analysis of R5X4 human immunodeficiency virus type 1 envelope glycoproteins derived from two individuals homozygous for the CCR5delta32 allele. J Virol. 2006, 80: 3684-3691. 10.1128/JVI.80.7.3684-3691.2006.
O'Brien TR, Winkler C, Dean M, Nelson JA, Carrington M, Michael NL, White GC: HIV-1 infection in a man homozygous for CCR5 delta 32. Lancet. 1997, 349: 1219-10.1016/S0140-6736(97)24017-1.
Theodorou I, Meyer L, Magierowska M, Katlama C, Rouzioux C: HIV-1 infection in an individual homozygous for CCR5 delta 32. Seroco Study Group. Lancet. 1997, 349: 1219-1220. 10.1016/S0140-6736(05)62411-7.
Kuipers H, Workman C, Dyer W, Geczy A, Sullivan J, Oelrichs R: An HIV-1-infected individual homozygous for the CCR-5 delta32 allele and the SDF-1 3'A allele. AIDS. 1999, 13: 433-434. 10.1097/00002030-199902250-00025.
Heiken H, Becker S, Bastisch I, Schmidt RE: HIV-1 infection in a heterosexual man homozygous for CCR-5 delta32. AIDS. 1999, 13: 529-530. 10.1097/00002030-199903110-00017.
Gorry PR, Zhang C, Wu S, Kunstman K, Trachtenberg E, Phair J, Wolinsky S, Gabuzda D: Persistence of dual-tropic HIV-1 in an individual homozygous for the CCR5 Delta 32 allele. Lancet. 2002, 359: 1832-1834. 10.1016/S0140-6736(02)08681-6.
Biti R, Ffrench R, Young J, Bennetts B, Stewart G, Liang T: HIV-1 infection in an individual homozygous for the CCR5 deletion allele. Nat Med. 1997, 3: 252-253. 10.1038/nm0397-252.
Balotta C, Bagnarelli P, Violin M, Ridolfo AL, Zhou D, Berlusconi A, Corvasce S, Corbellino M, Clementi M, Clerici M, et al: Homozygous delta 32 deletion of the CCR-5 chemokine receptor gene in an HIV-1-infected patient. AIDS. 1997, 11: F67-71. 10.1097/00002030-199710000-00001.
Moore JP, Doms RW: The entry of entry inhibitors: a fusion of science and medicine. Proc Natl Acad Sci USA. 2003, 100: 10598-10602. 10.1073/pnas.1932511100.
Root MJ, Hamer DH: Targeting therapeutics to an exposed and conserved binding element of the HIV-1 fusion protein. Proc Natl Acad Sci USA. 2003, 100: 5016-5021. 10.1073/pnas.0936926100.
Markosyan RM, Cohen FS, Melikyan GB: HIV-1 envelope proteins complete their folding into six-helix bundles immediately after fusion pore formation. Mol Biol Cell. 2003, 14: 926-938. 10.1091/mbc.E02-09-0573.
Mkrtchyan SR, Markosyan RM, Eadon MT, Moore JP, Melikyan GB, Cohen FS: Ternary complex formation of human immunodeficiency virus type 1 Env, CD4, and chemokine receptor captured as an intermediate of membrane fusion. J Virol. 2005, 79: 11161-11169. 10.1128/JVI.79.17.11161-11169.2005.
Moulard M, Lortat-Jacob H, Mondor I, Roca G, Wyatt R, Sodroski J, Zhao L, Olson W, Kwong PD, Sattentau QJ: Selective interactions of polyanions with basic surfaces on human immunodeficiency virus type 1 gp120. J Virol. 2000, 74: 1948-1960. 10.1128/JVI.74.4.1948-1960.2000.
Shattock RJ, Doms RW: AIDS models: microbicides could learn from vaccines. Nat Med. 2002, 8: 425-10.1038/nm0502-425.
Meylan PR, Kornbluth RS, Zbinden I, Richman DD: Influence of host cell type and V3 loop of the surface glycoprotein on susceptibility of human immunodeficiency virus type 1 to polyanion compounds. Antimicrob Agents Chemother. 1994, 38: 2910-2916.
Tao W, Richards C, Hamer D: Enhancement of HIV infection by cellulose sulfate. AIDS Res Hum Retroviruses. 2008, 24: 925-929. 10.1089/aid.2008.0043.
Flexner C, Barditch-Crovo PA, Kornhauser DM, Farzadegan H, Nerhood LJ, Chaisson RE, Bell KM, Lorentsen KJ, Hendrix CW, Petty BG, et al: Pharmacokinetics, toxicity, and activity of intravenous dextran sulfate in human immunodeficiency virus infection. Antimicrob Agents Chemother. 1991, 35: 2544-2550.
Turville SG, Aravantinou M, Miller T, Kenney J, Teitelbaum A, Hu L, Chudolij A, Zydowsky TM, Piatak M, Bess JW, et al: Efficacy of Carraguard-based microbicides in vivo despite variable in vitro activity. PLoS ONE. 2008, 3: e3162-10.1371/journal.pone.0003162.
Skoler S, Ramjee G, Ahmed K, Altini L, Govender S, et al: Efficacy of Carraguard for prevention of HIV infection among women in South Africa: a randomized, placebo-controlled trial. (In preparation). 2008
Jiang YH, Emau P, Cairns JS, Flanary L, Morton WR, McCarthy TD, Tsai CC: SPL7013 gel as a topical microbicide for prevention of vaginal transmission of SHIV89.6P in macaques. AIDS Res Hum Retroviruses. 2005, 21: 207-213. 10.1089/aid.2005.21.207.
Boyd MR, Gustafson KR, McMahon JB, Shoemaker RH, O'Keefe BR, Mori T, Gulakowski RJ, Wu L, Rivera MI, Laurencot CM, et al: Discovery of cyanovirin-N, a novel human immunodeficiency virus-inactivating protein that binds viral surface envelope glycoprotein gp120: potential applications to microbicide development. Antimicrob Agents Chemother. 1997, 41: 1521-1530.
Mori T, O'Keefe BR, Sowder RC, Bringans S, Gardella R, Berg S, Cochran P, Turpin JA, Buckheit RW, McMahon JB, Boyd MR: Isolation and characterization of griffithsin, a novel HIV-inactivating protein, from the red alga Griffithsia sp. J Biol Chem. 2005, 280: 9345-9353. 10.1074/jbc.M411122200.
Liu X, Lagenaur LA, Simpson DA, Essenmacher KP, Frazier-Parker CL, Liu Y, Tsai D, Rao SS, Hamer DH, Parks TP, et al: Engineered vaginal lactobacillus strain for mucosal delivery of the human immunodeficiency virus inhibitor cyanovirin-N. Antimicrob Agents Chemother. 2006, 50: 3250-3259. 10.1128/AAC.00493-06.
Emau P, Tian B, O'Keefe BR, Mori T, McMahon JB, Palmer KE, Jiang Y, Bekele G, Tsai CC: Griffithsin, a potent HIV entry inhibitor, is an excellent candidate for anti-HIV microbicide. J Med Primatol. 2007, 36: 244-253. 10.1111/j.1600-0684.2007.00242.x.
Huskens D, Vermeire K, Vandemeulebroucke E, Balzarini J, Schols D: Safety concerns for the potential use of cyanovirin-N as a microbicidal anti-HIV agent. Int J Biochem Cell Biol. 2008, 40: 2802-2814. 10.1016/j.biocel.2008.05.023.
Richman DD, Wrin T, Little SJ, Petropoulos CJ: Rapid evolution of the neutralizing antibody response to HIV type 1 infection. Proc Natl Acad Sci USA. 2003, 100: 4144-4149. 10.1073/pnas.0630530100.
Wei X, Decker JM, Wang S, Hui H, Kappes JC, Wu X, Salazar-Gonzalez JF, Salazar MG, Kilby JM, Saag MS, et al: Antibody neutralization and escape by HIV-1. Nature. 2003, 422: 307-312. 10.1038/nature01470.
Burton DR, Desrosiers RC, Doms RW, Koff WC, Kwong PD, Moore JP, Nabel GJ, Sodroski J, Wilson IA, Wyatt RT: HIV vaccine design and the neutralizing antibody problem. Nat Immunol. 2004, 5: 233-236. 10.1038/ni0304-233.
Veazey RS, Shattock RJ, Pope M, Kirijan JC, Jones J, Hu Q, Ketas T, Marx PA, Klasse PJ, Burton DR, Moore JP: Prevention of virus transmission to macaque monkeys by a vaginally applied monoclonal antibody to HIV-1 gp120. Nat Med. 2003, 9: 343-346. 10.1038/nm833.
Mascola JR, Stiegler G, VanCott TC, Katinger H, Carpenter CB, Hanson CE, Beary H, Hayes D, Frankel SS, Birx DL, Lewis MG: Protection of macaques against vaginal transmission of a pathogenic HIV-1/SIV chimeric virus by passive infusion of neutralizing antibodies. Nat Med. 2000, 6: 207-210. 10.1038/72318.
Rademacher T, Sack M, Arcalis E, Stadlmann J, Balzer S, Altmann F, Quendler H, Stiegler G, Kunert R, Fischer R, Stoger E: Recombinant antibody 2G12 produced in maize endosperm efficiently neutralizes HIV-1 and contains predominantly single-GlcNAc N-glycans. Plant Biotechnol J. 2008, 6: 189-201. 10.1111/j.1467-7652.2007.00306.x.
Floss DM, Sack M, Stadlmann J, Rademacher T, Scheller J, Stoger E, Fischer R, Conrad U: Biochemical and functional characterization of anti-HIV antibody-ELP fusion proteins from transgenic plants. Plant Biotechnol J. 2008, 6: 379-391. 10.1111/j.1467-7652.2008.00326.x.
Lin PF, Blair W, Wang T, Spicer T, Guo Q, Zhou N, Gong YF, Wang HG, Rose R, Yamanaka G, et al: A small molecule HIV-1 inhibitor that targets the HIV-1 envelope and inhibits CD4 receptor binding. Proc Natl Acad Sci USA. 2003, 100: 11013-11018. 10.1073/pnas.1832214100.
Veazey RS, Klasse PJ, Schader SM, Hu Q, Ketas TJ, Lu M, Marx PA, Dufour J, Colonno RJ, Shattock RJ, et al: Protection of macaques from vaginal SHIV challenge by vaginally delivered inhibitors of virus-cell fusion. Nature. 2005, 438: 99-102. 10.1038/nature04055.
Jiang S, Lin K, Strick N, Neurath AR: HIV-1 inhibition by a peptide. Nature. 1993, 365: 113-10.1038/365113a0.
Wild CT, Shugars DC, Greenwell TK, McDanal CB, Matthews TJ: Peptides corresponding to a predictive alpha-helical domain of human immunodeficiency virus type 1 gp41 are potent inhibitors of virus infection. Proc Natl Acad Sci USA. 1994, 91: 9770-9774. 10.1073/pnas.91.21.9770.
Lazzarin A, Clotet B, Cooper D, Reynes J, Arasteh K, Nelson M, Katlama C, Stellbrink HJ, Delfraissy JF, Lange J, et al: Efficacy of enfuvirtide in patients infected with drug-resistant HIV-1 in Europe and Australia. N Engl J Med. 2003, 348: 2186-2195. 10.1056/NEJMoa035211.
Veazey RS, Ketas TA, Klasse PJ, Davison DK, Singletary M, Green LC, Greenberg ML, Moore JP: Tropism-independent protection of macaques against vaginal transmission of three SHIVs by the HIV-1 fusion inhibitor T-1249. Proc Natl Acad Sci USA. 2008, 105: 10531-10536. 10.1073/pnas.0802666105.
Veazey RS, Klasse PJ, Schader SM, Hu Q, Ketas TJ, Lu M, Marx PA, Dufour J, Colonno RJ, Shattock RJ, et al: Protection of macaques from vaginal SHIV challenge by vaginally delivered inhibitors of virus-cell fusion. Nature. 2005
Jin H, Siwak EB, Smith R, Liwang PJ: Very strong synergy between modified RANTES and gp41 binding peptides leads to potent anti-HIV-1 activity. Antimicrob Agents Chemother. 2008
Tremblay CL, Giguel F, Kollmann C, Guan Y, Chou TC, Baroudy BM, Hirsch MS: Anti-human immunodeficiency virus interactions of SCH-C (SCH 351125), a CCR5 antagonist, with other antiretroviral agents in vitro. Antimicrob Agents Chemother. 2002, 46: 1336-1339. 10.1128/AAC.46.5.1336-1339.2002.
Rao S, Hu S, McHugh L, Lueders K, Henry K, Zhao Q, Fekete RA, Kar S, Adhya S, Hamer DH: Toward a live microbial microbicide for HIV: commensal bacteria secreting an HIV fusion inhibitor peptide. Proc Natl Acad Sci USA. 2005, 102: 11993-11998. 10.1073/pnas.0504881102.
Klasse PJ, Shattock RJ, Moore JP: Which topical microbicides for blocking HIV-1 transmission will work in the real world?. PLoS Med. 2006, 3: e351-10.1371/journal.pmed.0030351.
Sia SK, Kim PS: Protein grafting of an HIV-1-inhibiting epitope. Proc Natl Acad Sci USA. 2003, 100: 9756-9761. 10.1073/pnas.1733910100.
Eckert DM, Malashkevich VN, Hong LH, Carr PA, Kim PS: Inhibiting HIV-1 entry: discovery of D-peptide inhibitors that target the gp41 coiled-coil pocket. Cell. 1999, 99: 103-115. 10.1016/S0092-8674(00)80066-5.
Welch BD, Van Demark AP, Heroux A, Hill CP, Kay MS: Potent D-peptide inhibitors of HIV-1 entry. Proc Natl Acad Sci USA. 2007, 104: 16828-16833. 10.1073/pnas.0708109104.
Kuritzkes DR, Jacobson J, Powderly WG, Godofsky E, DeJesus E, Haas F, Reimann KA, Larson JL, Yarbough PO, Curt V, Shanahan WR: Antiretroviral activity of the anti-CD4 monoclonal antibody TNX-355 in patients infected with HIV type 1. J Infect Dis. 2004, 189: 286-291. 10.1086/380802.
Feng Y, Broder CC, Kennedy PE, Berger EA: HIV-1 entry cofactor: functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science. 1996, 272: 872-877. 10.1126/science.272.5263.872.
Dragic T, Litwin V, Allaway GP, Martin SR, Huang Y, Nagashima KA, Cayanan C, Maddon PJ, Koup RA, Moore JP, Paxton WA: HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC- CKR-5. Nature. 1996, 381: 667-673. 10.1038/381667a0.
Deng H, Liu R, Ellmeier W, Choe S, Unutmaz D, Burkhart M, Di MP, Marmon S, Sutton RE, Hill CM, et al: Identification of a major co-receptor for primary isolates of HIV-1. Nature. 1996, 381: 661-666. 10.1038/381661a0.
Choe H, Farzan M, Sun Y, Sullivan N, Rollins B, Ponath PD, Wu L, Mackay CR, LaRosa G, Newman W, et al: The beta-chemokine receptors CCR3 and CCR5 facilitate infection by primary HIV-1 isolates. Cell. 1996, 85: 1135-1148. 10.1016/S0092-8674(00)81313-6.
Bleul CC, Farzan M, Choe H, Parolin C, Clark-Lewis I, Sodroski J, Springer TA: The lymphocyte chemoattractant SDF-1 is a ligand for LESTR/fusin and blocks HIV-1 entry. Nature. 1996, 382: 829-833. 10.1038/382829a0.
Arenzana-Seisdedos F, Virelizier JL, Rousset D, Clark-Lewis I, Loetscher P, Moser B, Baggiolini M: HIV blocked by chemokine antagonist. Nature. 1996, 383: 400-10.1038/383400a0.
Alkhatib G, Combadiere C, Broder CC, Feng Y, Kennedy PE, Murphy PM, Berger EA: CC CKR5: a RANTES, MIP-1alpha, MIP-1beta receptor as a fusion cofactor for macrophage-tropic HIV-1. Science. 1996, 272: 1955-1958. 10.1126/science.272.5270.1955.
Tsibris AM, Kuritzkes DR: Chemokine antagonists as therapeutics: focus on HIV-1. Annu Rev Med. 2007, 58: 445-459. 10.1146/annurev.med.58.080105.102908.
Lederman MM, Veazey RS, Offord R, Mosier DE, Dufour J, Mefford M, Piatak M, Lifson JD, Salkowitz JR, Rodriguez B, et al: Prevention of vaginal SHIV transmission in rhesus macaques through inhibition of CCR5. Science. 2004, 306: 485-487. 10.1126/science.1099288.
Lalezari J, Yadavalli GK, Para M, Richmond G, Dejesus E, Brown SJ, Cai W, Chen C, Zhong J, Novello LA, et al: Safety, pharmacokinetics, and antiviral activity of HGS004, a novel fully human IgG4 monoclonal antibody against CCR5, in HIV-1-infected patients. J Infect Dis. 2008, 197: 721-727. 10.1086/527327.
Jacobson JM, Saag MS, Thompson MA, Fischl MA, Liporace R, Reichman RC, Redfield RR, Fichtenbaum CJ, Zingman BS, Patel MC, et al: Antiviral Activity of Single-Dose PRO 140, a CCR5 Monoclonal Antibody, in HIV-Infected Adults. J Infect Dis. 2008, 198 (9): 1345-1352. 10.1086/592169.
Gulick RM, Su Z, Flexner C, Hughes MD, Skolnik PR, Wilkin TJ, Gross R, Krambrink A, Coakley E, Greaves WL, et al: Phase 2 study of the safety and efficacy of vicriviroc, a CCR5 inhibitor, in HIV-1-Infected, treatment-experienced patients: AIDS clinical trials group 5211. J Infect Dis. 2007, 196: 304-312. 10.1086/518797.
Landovitz RJ, Angel JB, Hoffmann C, Horst H, Opravil M, Long J, Greaves W, Fatkenheuer G: Phase II Study of Vicriviroc versus Efavirenz (both with Zidovudine/Lamivudine) in Treatment-Naive Subjects with HIV-1 Infection. J Infect Dis. 2008
St John E, Mares D, Spear GT: Bacterial vaginosis and host immunity. Curr HIV/AIDS Rep. 2007, 4: 22-28. 10.1007/s11904-007-0004-y.
Galvin SR, Cohen MS: The role of sexually transmitted diseases in HIV transmission. Nat Rev Microbiol. 2004, 2: 33-42. 10.1038/nrmicro794.
Hartley O, Gaertner H, Wilken J, Thompson D, Fish R, Ramos A, Pastore C, Dufour B, Cerini F, Melotti A, et al: Medicinal chemistry applied to a synthetic protein: development of highly potent HIV entry inhibitors. Proc Natl Acad Sci USA. 2004, 101: 16460-16465. 10.1073/pnas.0404802101.
Hartley O, Dorgham K, Perez-Bercoff D, Cerini F, Heimann A, Gaertner H, Offord RE, Pancino G, Debre P, Gorochov G: Human immunodeficiency virus type 1 entry inhibitors selected on living cells from a library of phage chemokines. J Virol. 2003, 77: 6637-6644. 10.1128/JVI.77.12.6637-6644.2003.
Gaertner H, Cerini F, Kuenzi G, Melotti A, Offord RE, Rossitto-Borlat I, Nedellec R, Salkowitz J, Gorochov G, Mosier DE, Hartley O: Highly Potent, Fully Recombinant anti-HIV chemokines: Re-engineering a low-cost microbicide.
Veazey RS, Ling B, Green L, Lifson JD, Piatak MLMM, Mosier DE, Offord RE, Hartley O: Recombinant chemokine analogues represent promising new candidate microbicides.
Cerini F, Landay A, Gichinga C, Lederman MM, Flyckt R, Starks D, Offord RE, Le Gal F, Hartley O: Chemokine analogues show suitable stability for development as microbicides. Journal of AIDS. 2008,
Bhatnagar A, Willins DL, Gray JA, Woods J, Benovic JL, Roth BL: The dynamin-dependent, arrestin-independent internalization of 5-hydroxytryptamine 2A (5-HT2A) serotonin receptors reveals differential sorting of arrestins and 5-HT2A receptors during endocytosis. J Biol Chem. 2001, 276: 8269-8277. 10.1074/jbc.M006968200.
Feng Z, Dubyak GR, Lederman MM, Weinberg A: Cutting edge: human beta defensin 3 – a novel antagonist of the HIV-1 coreceptor CXCR4. J Immunol. 2006, 177: 782-786.
Pheng LH, Dumont Y, Fournier A, Chabot JG, Beaudet A, Quirion R: Agonist- and antagonist-induced sequestration/internalization of neuropeptide Y Y1 receptors in HEK293 cells. Br J Pharmacol. 2003, 139: 695-704. 10.1038/sj.bjp.0705306.
Roettger BF, Ghanekar D, Rao R, Toledo C, Yingling J, Pinon D, Miller LJ: Antagonist-stimulated internalization of the G protein-coupled cholecystokinin receptor. Mol Pharmacol. 1997, 51: 357-362.
Gaetner H, Cerini F, Kuenzi G, Melotti A, Offord R, Rossitto-Borlatt I, Nedellec R, Salkowitz J, Gorochov G, Mosier D, Hartley O: Highly Potent, Fully Recombinant anti-HIV chemokines: Re-engineering a low-cost microbicide. ProcNatl Acad Sci (USA).
Barth RE, Wensing AM, Tempelman HA, Moraba R, Schuurman R, Hoepelman AI: Rapid accumulation of nonnucleoside reverse transcriptase inhibitor-associated resistance: evidence of transmitted resistance in rural South Africa. Aids. 2008, 22: 2210-2212. 10.1097/QAD.0b013e328313bf87.
Little SJ, Holte S, Routy JP, Daar ES, Markowitz M, Collier AC, Koup RA, Mellors JW, Connick E, Conway B, et al: Antiretroviral-drug resistance among patients recently infected with HIV. N Engl J Med. 2002, 347: 385-394. 10.1056/NEJMoa013552.
Grant RM, Hamer D, Hope T, Johnston R, Lange J, Lederman MM, Lieberman J, Miller CJ, Moore JP, Mosier DE, et al: Whither or wither microbicides?. Science. 2008, 321: 532-534. 10.1126/science.1160355.
Van Damme L, Govinden R, Mirembe FM, Guedou F, Solomon S, Becker ML, Pradeep BS, Krishnan AK, Alary M, Pande B, et al: Lack of effectiveness of cellulose sulfate gel for the prevention of vaginal HIV transmission. N Engl J Med. 2008, 359: 463-472. 10.1056/NEJMoa0707957.
Woolfson AD, Malcolm RK, Gallagher R: Drug delivery by the intravaginal route. Crit Rev Ther Drug Carrier Syst. 2000, 17: 509-555.
Klasse PJ, Shattock RJ, Moore JP: Which Topical Microbicides for Blocking HIV-1 Transmission Will Work in the Real World?. PLoS Med. 2006, 3 (9): e351-10.1371/journal.pmed.0030351.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MML, RJ, MR and SFS contributed to the original drafts of the manuscript. All authors critiqued drafts of the manuscript and all authors read and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lederman, M.M., Jump, R., Pilch-Cooper, H.A. et al. Topical application of entry inhibitors as "virustats" to prevent sexual transmission of HIV infection. Retrovirology 5, 116 (2008). https://doi.org/10.1186/1742-4690-5-116
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1742-4690-5-116