Abstract
Background
The viral and host factors involved in transmission of HIV through breastfeeding are largely unknown, and intervention strategies are urgently needed to protect at-risk populations. To evaluate the viral and immunological factors directly related to milk transmission of virus, we have evaluated the disease course of Simian Immunodeficiency Virus (SIV) in lactating rhesus macaques (Macaca mulatta) as a model of natural breast milk transmission of HIV.
Results
Fourteen lactating macaques were infected intravenously with SIV/DeltaB670, a pathogenic isolate of SIV and were pair-housed with their suckling infants throughout the disease course. Transmission was observed in 10 mother-infant pairs over a one-year period. Two mothers transmitted virus during the period of initial viremia 14–21 days post inoculation (p.i.) and were classified as early transmitters. Peak viral loads in milk and plasma of early transmitters were similar to other animals, however the early transmitters subsequently displayed a rapid progressor phenotype and failed to control virus expression as well as other animals at 56 days p.i. Eight mothers were classified as late transmitters, with infant infection detected at time points in the chronic stage of the maternal SIV disease course (81 to 360 days). Plasma viral loads, CD4+ T cell counts and SIV-specific antibody titers were similar in late transmitters and non-transmitters. Late breast milk transmission, however, was correlated with higher average milk viral loads and more persistent viral expression in milk 12 to 46 weeks p.i. as compared to non-transmitters. Four mothers failed to transmit virus, despite disease progression and continuous lactation.
Conclusion
These studies validate the SIV-infected rhesus macaque as a model for breast milk transmission of HIV. As observed in studies of HIV-infected women, transmission occurred at time points throughout the period of lactation. Transmission during the chronic stage of SIV-infection correlated with a threshold level of virus expression as well as more persistent shedding in milk. This model will be a valuable resource for deciphering viral and host factors responsible for transmission of HIV through breastfeeding.
Similar content being viewed by others
Background
Mother-to-infant transmission is the primary cause of HIV-1 infection in children worldwide, with an estimated 700,000 children infected in 2003 [1]. Transmission through breastfeeding accounts for at least one-third of these infections, however it is difficult to differentiate perinatal transmission from early milk transmission [2–4]. Meta-analysis of several cohorts has estimated that 14% of mothers chronically-infected with HIV transmit virus to their infant through breastfeeding, whereas 29% of women who acquire primary HIV infections during lactation transmit virus to their infants [5]. Since breastfeeding is unavoidable in many countries in which the HIV-1 epidemic is most severe, it is necessary to understand risk factors associated with breast milk transmission and the underlying viral and immunological mechanisms responsible for transmission.
Epidemiological studies of HIV-1 infected women and their infants have identified several risk factors for milk transmission of HIV, as recently reviewed by Read et al [6]. Reduced levels of innate immune factors including lactoferrin, lysozyme and secretory leukocyte protease inhibitor (SLPI), as well as insufficient secretory IgA responses have been associated with higher rates of HIV transmission through milk [7–10]. Conditions affecting the mucosal epithelium, such as mastitis, and oral candidiasis in the infant, have also been identified as risk factors for milk transmission of HIV [4, 11–13]. In addition, several studies have shown that longer durations of breastfeeding increase the cumulative risk of milk transmission [3, 4, 14–16].
One of the most consistently documented risk factors of mother-to-infant transmission through milk is advanced maternal disease as measured by higher plasma viral loads and lower CD4+ T cell counts [12, 17–19]. Although this risk factor has been identified in several cohorts, transmission occurs by mothers with a wide range of plasma viral loads and CD4+ T cell counts, and an absolute level of these markers has not been associated with transmission [20–22]. Longitudinal evaluations of HIV-infected women in a Nairobi clinical trial study have shown that transmission of HIV through milk is associated with higher levels of viral RNA in milk as well as with consistent shedding of virus in milk [23]. Although this study estimated that each log increase in milk viral load doubled the risk of transmission, they were unable to identify a milk viral threshold level required for transmission. The frequency of sampling and constant fluctuations in milk virus levels may explain these observations.
The epidemiological findings observed in humans have not been evaluated in an animal model that could allow the identification of viral and host factors directly responsible for transmission through breastfeeding. The SIV infected rhesus macaque has successfully been used as a model of HIV transmission and pathogenesis. Although disease progression is more rapid in macaques infected with SIV than in HIV infected humans, macaques exhibit a similar disease course and succumb to opportunistic infections much the same as infected humans [24]. We have previously reported breast milk transmission of SIV in experimentally infected rhesus macaques (Macaca mulatta) [25], and in this report, we expand our observations and examine the correlation between milk transmission of SIV and levels of virus in maternal plasma and milk samples, levels of peripheral CD4+ T cells, and titers of SIV-specific antibodies in milk and plasma from 14 lactating macaques.
Results
Outcome of SIV infection of lactating macaques
Fourteen lactating macaques were inoculated intravenously with a pathogenic SIV inoculum, SIV/DeltaB670 [26], to evaluate mother-to-infant transmission through breastfeeding. Each animal had a suckling infant at the time of inoculation and all mothers were PCR positive for SIV at 7 days post inoculation (p.i.). Mother-infant pairs were monitored daily for clinical signs of disease progression. Infant blood samples were collected weekly for 8 weeks for SIV PCR amplification, followed by biweekly and then monthly testing.
As summarized in Table 1, 10 of 14 infants became PCR positive for SIV over the course of the study. Two infants were rapidly infected as determined by PCR amplification of SIV sequences from infant PBMCs 14 and 21 days after inoculation of the mothers. The mothers, P173 and T243, were labeled as early transmitters. Two additional infants were identified as SIV-infected at 81 and 84 days post inoculation of the mothers, and six infants were SIV positive at time points ranging from 235–360 days post inoculation. Because these eight mothers transmitted virus at later times points in their disease course, they were labeled as late transmitters. Four infants were consistently SIV-negative by PCR amplification, despite progression of SIV disease and continued lactation in the non-transmitting mothers. Two of these infants repeatedly tested SIV-negative in PBMC for at least 1 year after removal from the dam. The other two of the four SIV-uninfected infants, monkeys CK56 and DP79, were euthanized at the same time point as their mother for reasons unrelated to SIV. PCR and RT-PCR analysis of PBMC, plasma, spleen, lymph node and thymus obtained at the time of necropsy were all negative for SIV.
The age of infants at the time point of maternal inoculation varied from 7 to 54 days (table 1). Although the ages varied at the time of maternal inoculation and the volume of milk ingested by each infant could not be controlled, associations between infant age, maturity of milk and the timing of transmission could not be identified. The two infants infected early were representative of the range of infant ages, at 7 and 43 days of age at the time of maternal inoculation. The four infants that remained uninfected despite disease progression displayed a similar age distribution at the start of the study at 8, 14, 26 and 54 days of age. Infants classified as late transmission ranged from 7–54 days of age at the start of the study. All females continued to lactate throughout the study period.
Disease course
Each of the 14 mothers developed clinical signs of SIV disease over the one-year study period, which included cachexia, weight loss, diarrhea, lymphadenopathy, and/or pneumonia. The two early transmitters progressed to end stage disease rapidly. Monkey P173 was euthanized 143 days p.i. with end stage disease caused by cytomegalovirus (CMV) infection, and monkey T243 was euthanized 132 days p.i. with interstitial pneumonia. Clinical signs of disease were evident in each of the late transmitting females near the time of transmission, but symptoms varied widely.
The time points of euthanization for late transmitters ranged from 143 to 373 days p.i. Each of the late transmitters was sacrificed with clinical signs of disease at the end of the study period, although end stage disease had not necessarily been reached in all of these monkeys at the time of euthanization. Three of the four non-transmitters progressed to end stage disease during the study period and were sacrificed due to opportunistic infections including disseminated CMV, cryptosporidium, or adenovirus. The fourth non-transmitter (monkey AA26) died suddenly while housed with her infant. Necropsy revealed the cause of death in monkey AA26 to be colitis, but lymphoid hyperplasia and loss of 6% body weight were also evident.
Analysis of CD4+, T cells
To evaluate the level of immunosupression in the mothers, CD4+ T cell counts were determined by flow cytometic evaluation of blood samples on the day of inoculation and at several time points over the course of disease (Figure 1), as previously described [27]. At the time of inoculation (day 0), a wide range of CD4+ T-cell counts were found in the females, varying from 600 to over 3000 cells/μl. Two weeks p.i., a decrease in the number of CD4+ T cells was observed in all animals. Cell counts remained at these low levels in the two early transmitters (yellow symbols), but rebounded to varying levels in the other 12 animals. No significant differences in cell counts were observed between non-transmitting and late transmitting mothers at any point in the disease course, with only a few animals dropping to CD4+ T cell counts below 400 cells/μl at any time point. The ratio of CD4+/CD8+ T cells was also compared in each of the monkeys; however, significant differences were not observed, between the transmission groups (data not shown).
CD4+ T Cell Counts in Lactating Macaques. CD3+, CD4+ cell counts in peripheral blood of lactating macaques at various time points post-inoculation with SIV. The day of inoculation is represented by the 0 time point. Cell counts for individual monkeys are shown and the means of each transmission group are represented in the line graph. Early transmitters are shown in yellow, late transmitters in red and non-transmitters in blue.
Viral load
Viral RNA levels in plasma and milk were determined by real-time quantitative RT-PCR at several time points throughout the one year study period to evaluate the relationship between viral load and transmission. As shown in Figure 2A, plasma viral RNA loads in each of the mothers peaked two weeks post-inoculation with levels ranging from 1 × 106 to 1 × 108 copies/ml. Average plasma viral loads at 14 days p.i. were similar for the transmitting and non-transmitting mothers (Figure 3). At 8 weeks p.i., plasma viral loads reached set point levels. The four non-transmitting mothers had average viral loads at set point, ranging from 4 × 105 to 6 × 106 copies/ml, and similar levels persisted until end stage disease. The eight late transmitters generally had lower plasma viral loads at 8 weeks p.i. than non-transmitters (p = 0.048) ranging from 1 × 104 to 2 × 106 copies/ml. Plasma viral loads in the late transmitters increased as disease progressed, reaching levels similar to non-transmitters.
Viral Load in Lactating Macaques. Viral RNA copies were measured by real-time RT-PCR from (A) peripheral blood plasma and (B) the cell-free fraction of milk samples obtained at indicated time points in each of fourteen lactating macaques. Milk samples that could be amplified by PCR, but had values calculated as ≤50 copies RNA/ml (amplifiable but not quantifiable) were indicated as having 50 copies. Samples from which viral RNA could not be amplified were indicated as having 1 copy. Early transmitters are shown in yellow, late transmitters in red and non-transmitters in blue.
Mean Plasma and Milk Viral Loads in Early, Late and Non-Transmitting Macaques. Viral RNA copies measured by real-time RT-PCR in cell-free fraction of milk samples obtained from lactating macaques. Samples that could be amplified by PCR, but had values calculated as having ≤50 copies RNA/ml (amplifiable but not quantifiable) were indicated as having 50 copies. Samples from which viral RNA could not be amplified were indicated as having 1 copy. Early transmitters are shown in yellow, late transmitters in red and non-transmitters in blue.
Milk viral loads, like plasma, were the highest at 2 weeks p.i. in all of the mothers, ranging from 2 × 103 to 4 × 105copies/ml (Figure 2B). Viral loads in early transmitters were not significantly higher than other animals at 14 days p.i. (Figure 3). Each mother displayed individual patterns of virus shedding in milk throughout the disease course, with many having low (≤50 copies/ml) or undetectable milk viral loads at some time points, while at other time points levels were as high as 1 × 104 copies/ml. To evaluate the levels and persistence of virus expression in milk at later time points during the disease course, we compared average milk viral loads as well as the highest milk viral load detected at any time point 12–46 weeks p.i. in each mother. As shown in Table 2, average and peak milk viral RNA levels in all non-transmitters were below 500 copies/ml during this time, with average viral loads ranging from <50 to 357 viral copies/ml. In contrast, late transmitters had at least one milk sample with more than 500 copies virus/ml and six of the eight late transmitters had milk samples with more than 1000 copies/ml over this time period. Peak milk virus levels observed 12–46 weeks p.i. were significantly higher in late transmitting animals than non-transmitters (p = 0.004). Over the same period of time, late transmitters had higher average milk viral loads than non-transmitters (p = 0.028), demonstrating more consistent shedding of virus in milk by late transmitters throughout the disease course.
SIV Specific Antibody
To evaluate humoral immune responses in SIV-infected females and determine their association with transmission, levels of SIV envelope specific IgG in plasma and milk were determined by ELISA. As shown in Table 3, peak SIV-specific plasma IgG titers ranging from 1:20,000 to 1:320,000 were found in late transmitter and non-transmitter females, whereas lower titers of ≤1: 5,000 were detected in the two early transmitters. Milk titers of env-specific IgG were 1–3 logs lower than plasma IgG titers in all monkeys, with the two early transmitters again displaying the lowest milk IgG titers (Table 3). SIV-specific IgA responses in milk were 5-fold lower than IgG titers in milk of all monkeys, with levels ranging from undetectable to 1:10 in early transmitters monkeys T243 and P173, respectively, and varying from 1:10 to 1:500 in all other animals. Low titers, or the absence of virus-specific IgA in milk of HIV-infected women have also been reported [7, 28–32]. SIV envelope specific plasma IgG, milk IgG, and milk IgA titers remained relatively stable throughout the disease course, including time points near transmission of virus to the infant (data not shown). All late transmitters females had IgG titers in milk and plasma similar to non-transmitters, indicating that high titers of SIV-envelope specific antibodies did not protect infants from infection. The two early transmitters failed to produce levels of SIV envelope antibody comparable to other animals by 98 days p.i. a characteristic commonly identified with rapid progression of SIV disease [24]
Discussion
This study is the first to describe the viral and immunological correlates of breast milk transmission in lactating SIV-infected macaques. Following intravenous inoculation of females, transmission through breastfeeding was observed in 10 of 14 macaque mother-infant pairs. By inoculating mothers after delivery with a highly pathogenic strain of SIV, (SIV/DeltaB670) the viral and immunological parameters related solely to breast milk transmission could be evaluated in the absence of potential in utero and peri-partal transmission. With this model, an accelerated disease course was observed coincident with the period of lactation, and is likely responsible for the high rate of transmission that occurred. Despite acute infection of lactating mothers and the accelerated disease course in this model, transmission to infants was not uniform. Transmission occurred at various time points throughout the period of lactation, while four infants remained uninfected. These results are similar to observations made in HIV-infected women, where infant infection through breastfeeding occurs throughout the course of lactation [19, 33]. This model therefore provides a resource for deciphering the mechanisms involved in breast milk transmission of HIV.
Eight mothers transmitted virus to their infants during the chronic phase of the disease course, at time points ranging from 81 to 360 days p.i. These late transmitting mothers had similar plasma viral loads and similar courses of disease progression as compared to non-transmitting mothers. Transmitting mothers, however, had one or more milk samples with greater than 500 copies of viral RNA/ml, and expressed higher average milk viral loads than non-transmitters over the chronic stage of disease. These results are consistent with observations in HIV-infected women that higher milk viral loads and consistent shedding of virus in milk correlate with infant infection [23]. Due to frequent longitudinal sampling and the controlled environment provided by the macaque model, this correlate of transmission was more precisely defined in the SIV model than in cohorts of HIV infected women.
Despite disease progression in the mothers, four infants remained uninfected in this study. Each of the non-transmitters continued to lactate and remained housed with their infant until at end-stage disease. Although plasma viral loads and CD4+ T cell counts were similar to those in late transmitting mothers, milk viral loads were less than 500 copies/ml at each time point evaluated. These results suggest that the dynamics of virus expression in milk are critical to infant infection. Macaques that display a profile of high plasma viral load, with low levels of virus expression in milk will be valuable tools for deciphering the viral properties and mechanisms responsible for expression in milk.
While viral levels in milk could be identified as a correlate of transmission during the chronic stage of disease, milk viral loads never returned to levels as high as those observed during peak viremia at 14 days p.i. This implies that multiple factors, in addition to absolute levels of virus are responsible for infant infection through breastfeeding. During the period of acute viremia only two of 14 infants became SIV-infected through breastfeeding, despite exposure to high levels of virus in milk and the absence of SIV-specific immune responses. Viral loads in milk and plasma at 14 and 21 days p.i. were similar in all mothers, as were CD4+ T cell counts. The two early transmitting females, however, progressed to end stage disease rapidly and were found to have lower titers of envelope-specific antibody by day 98 p.i., as compared to the remaining 12 animals. Early transmitters also had the highest plasma virus levels at 56–98 days p.i., failed to recover numbers of CD4+ T cells after the initial loss observed at 14 days p.i., and were euthanized due to end-stage disease before 5 months. This profile of rapid disease progression in SIV-infected macaques has been reported and characterized by others [34–36].
From these observations it can be hypothesized that the same host responses that are unsuccessful in controlling the initial viremia in the lactating mother are also responsible for transmission of virus to the infant. Similarly, the ability of most infants to resist infection in this experimental model, despite oral exposure to high levels of virus in milk, provides an opportunity to decipher the innate responses that provide protection to the infant.
Breast milk contains numerous factors with antimicrobial and immunomodulatory properties that may affect transmission to the infant and several factors in infant saliva are likely to provide protection against oral virus exposure (reviewed by Kourtis et al.) [37]. Higher levels of secretory leukocyte protease inhibitor (SLPI) in the saliva of infants breast fed by HIV-infected mothers has been correlated with a decreased risk of infection by 1 month of age [38]. Innate protective responses in infant saliva, as well as breast milk were not evaluated in this study due to sample limitations, but should be addressed in future studies with this model.
Titers of envelope specific IgA in milk of SIV-infected macaques were at least five-fold lower than levels of specific IgG in milk. These observations are consistent with those reported in HIV-infected women, where low levels of HIV-specific IgA are commonly found, despite normal levels of total IgA [30–32, 39]. Although the lack of IgA responses against SIV may contribute to transmission, they cannot be directly responsible, as four infants remained SIV-uninfected despite the lack of maternal envelope-specific IgA and similar levels of SIV-specific IgG. Similarly the levels of SIV specific IgG cannot play a direct role in protection, since late transmitters and non transmitters developed similar titers of envelope specific IgG. Future studies in this model can be designed to address the role of immune evasion in breast milk transmission of virus.
Virus expressed in the cell-associated fraction of milk may also play a key role in transmission, however sample limitations did not allow these analyses in this study. Quantitation of the cell-associated viral load in milk and characterization of the viral genotypes/phenotypes expressed in cell-associated and cell-free fractions of milk may help to define the viral factors responsible for infant infection.
Conclusions
This study has examined the viral and immunological factors associated with transmission of virus through breastfeeding in a group of 14 lactating macaques infected with SIV. Mothers that transmitted virus to their infants through breastfeeding during the chronic phase of the disease course exhibited disease correlates similar to those reported in HIV-infected, transmitting women, and thus supports the use of the SIV-infected lactating rhesus macaque as a model. In this well-controlled experimental model, the main correlate of breast milk transmission could be more precisely defined as the persistence of viral expression in milk and the expression of higher viral levels in milk as compared to non-transmitters. The accelerated SIV disease course in macaques resulted in a high rate of transmission, however four infants remained uninfected despite advanced disease in lactating mothers, modeling the range of outcomes observed in humans. Additionally, our observation of rapid transmission by macaques with a rapid progressor phenotype provides additional insights into the factors responsible for control of primary viremia, and the expression of virus in milk. This model is a valuable tool for the characterization of viral and host mechanisms responsible for transmission of SIV/HIV through breastfeeding and will help elucidate the responses that provide protection from breast milk transmission.
Methods
Animals
Eight female rhesus macaques (Macaca mulatta) were selected for the study 15–54 days after vaginal delivery of normal infants. Six additional females were time mated using exogenous progesterone administration and withdrawal as described previously, [40]. Time-mated females were enrolled in this study 7–9 days after vaginal delivery of normal infants. The fourteen lactating dams were inoculated intravenously with 4 TCID50 doses of SIV/DeltaB670, a primary SIV stock amplified on rhesus primary peripheral blood mononuclear cells (PBMC) [26]. Inoculations were performed via cannulation of the saphaneous vein. Lactating females were housed with their infants and observed several times each day for signs of illness and/or maternal neglect. Animals that became moribund were humanely sacrificed.
All animal protocols were approved by the Tulane and LSU Institutional Animal Care and Use Committees and were in accordance with the Guide for the Care and Use of Laboratory Animals [41]. Animals were housed at the Tulane National Primate Research Center, a facility accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International. Animals were housed in standard stainless steel cages in a room with artificial light on a 12:12 hour light-dark cycle. Animals were fed twice a day with Primate Chow and water was provided ad libitum.
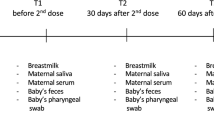
Sample collection
Macaques were anesthetized with ketamine hydrochloride (10 mg/kg) just prior to physical exams and sample collection. Infant macaques were anesthetized for exams when they reached 3–4 months of age. Samples of blood (1–8 ml) were collected from the dams and infants weekly for 8 weeks, then biweekly and monthly.
Blood was collected in tubes with EDTA anticoagulant for enumeration of CD4+ T cells by flow cytometric evaluations as described previously [27]. For analysis of virus and antibody titers, blood was collected in acid citrate dextrose anticoagulant and centrifuged at 1550 rpm for 15 minutes. Plasma was removed and stored at -80°C. PBMCs were purified from blood samples using Lymphocyte Separation Medium from ICN (Aurora, OH) and washed with phosphate buffered saline prior to lysis and DNA purification. DNA was isolated from PBMC of cryopreserved tissues using Bio Rad Genomic DNA Isolation kit, and quantified by A260 measurement. Flow cytometric determination of lymphocyte subsets was performed as described [27].
Approximately 1 ml of milk was collected by manual expression at the same time points as blood and immediately stored on ice. Milk samples were separated into cellular and supernatant fractions by centrifugation at 1550 rpm for 15 minutes. The fat layer was suctioned off, and supernatant and cellular fractions were stored separately at -80°C.
Reverse Transcription of SIV RNA
Viral cDNA was prepared from free virus particles contained in plasma or milk for viral RNA quantitation assays. Virus was purified from the cell-free fraction of milk or blood plasma by centrifugation at 22,000 × g for 1 hour. Viral pellets from 1 ml of sample were solubilized in 1 ml of Trizol Reagent (Life Technologies, Rockville, MD), and RNA was purified as per manufacturer protocols, with the final RNA sample resuspended in 30 μl of water. Reverse transcription (RT) reactions contained 1 × PCR buffer II (50 mM KCl, 10 mM Tris-HCl, Ph 8.3), 5.0 mM MgCl2, 0.5 mM dNTPs, 2.5 uM random hexamers, 10 U Rnase inhibitor 25 U MultiScribe reverse transcriptase and 3 μl of sample RNA (10% of total). Reaction conditions were 15 min. at 42°C, 5 minutes at 95°C, and 5 minutes at 4°C.
Real Time RT-PCR Taq-Man assay
SIV RNA copy number in plasma and milk samples was quantitated by real-time RT-PCR amplification based on a previously described assay [42] that amplifies a region in the SIV LTR using a 7700 ABI PRISM Sequence Detector (Applied Biosystems, Foster City, CA). Virions expressed in milk and plasma were purified and reverse-transcribed to cDNA in a 10 μl total reaction volume as described above. Quantitation reactions were done with duplicate cDNA samples, each prepared from 10% of total sample RNA. The cDNA was added to a PCR master mix containing 5.5 mM MgCl2, 1 × TaqMan buffer A, 0.5 mM dNTPs, 600 mM each of forward and reverse primers, 150 nM of TaqMan probe, and 1.25 U AmpliTaq Gold, yielding a 25 μl total reaction volume. Primer sequences were -5'TTGAGCCCTGGGAGGTTCT3', and 5'GCCAAGTGCTGGTGAGAGTCT3' and Probe -6FAM-AACACCCAGGCTCTACCTGCTAGTGCTG-TAMRA. All reagents were from Applied Biosystems. Following a 10 minute incubation at 95°C, 40 cycles of amplification were performed (94°C for 15 sec., and 60°C for 60 sec.) in a 7700 ABI PRISM Sequence Detector. SIV copy numbers in unknown samples were calculated from a standard curve generated from serial dilutions of a RNA standard amplified in each assay. A plasmid containing SIV LTR sequences (kindly provided by M. Murphey-Corb, University of Pittsburgh) was transcribed in vitro to generate the RNA standard. Purified, standard RNA was quantified by A260 measurements, and based on the calculated extinction coefficient for the transcript sequence/length was serially diluted from 107 to O copies. The dilution series was amplified in the real time RT-PCR assay in triplicate for generation of the standard curve. This assay can reliably detect 5 copies of SIV/ml and has a linear dynamic range of 8 logs.
SIV PCR Amplification
For detection of SIV infection in infant and adult macaques, a 480 base pair fragment in the SIV envelope was amplified in a nested PCR assay. In these amplification assays, 1 μg of DNA from PBMC, or cDNA (prepared as described above) was added to a reaction mixture as previously described [40]. First round primers of nucleotides 6709 to 6728 and 7406 to 7385 (numbering from SIVmac239 sequence) were used. Two microliters of the first round reaction were added to a second round of PCR with an internal set of primers of nucleotides 6845 to 6868 and 7327 to 7305(SIVmac239 reference).
SIV-specific antibody titers
SIV specific antibodies were determined by enzyme linked immunosorbent assays (ELISA) as described by Tryphonas et al., [43] with the following modifications. Plates were coated with 3 μg/ml of a recombinant SIVmac239 gp130 (Quality Biologicals, Gaithersburg, MD) diluted in PBS. Blocking was done at 4°C overnight with 4% whey and 10% goat serum in PBS. Plasma dilutions started at 1:5000 and were serially diluted four fold. Milk was initially diluted 1:50 then serially diluted four fold. Peroxidase or biotin conjugated rhesus antisera (0.5 ug/ml) (Rockland Immunochemicals, Inc., Gilbertsville, PA) was added after washing and incubated for 1 hour at room temperature. TMB developing solution (KPL, Gaithersburg, MD) was added and incubated for 3 minutes followed by addition of 1 M H3PO4 to stop the reaction. Absorbance values (at 450 nm) were determined by use of a microplate reader.
Statistical Analysis
Comparisons between viral loads, average viral loads and CD4+ CD3+ cell counts in different groups of macaques were performed by utilizing the non parametric two tailed Mann Whitney U Test. A p-value of <0.05 was considered significant. Viral loads that were detectable but not quantifiable were set at 50 copies/ml. Undetectable viral loads were set at 1 copy.
References
UNAIDS-WHO: AIDS epidemic update: 2003, http://www.unaids.org/Unaids/EN/Resources/Publications/corporate+publications/aids+epidemic+update+-+december+2003.asp. 2003
Newell ML: Mechanisms and timing of mother-to-child transmission of HIV-1. Aids. 1998, 12: 831-837. 10.1097/00002030-199808000-00004.
Leroy V, Newell ML, Dabis F, Peckham C, Van de Perre P, Bulterys M, Kind C, Simonds RJ, Wiktor S, Msellati P: International multicentre pooled analysis of late postnatal mother-to-child transmission of HIV-1 infection. Ghent International Working Group on Mother-to-Child Transmission of HIV. Lancet. 1998, 352: 597-600. 10.1016/S0140-6736(98)01419-6.
John GC, Richardson BA, Nduati RW, Mbori-Ngacha D, Kreiss JK: Timing of breast milk HIV-1 transmission: a meta-analysis. East Afr Med J. 2001, 78: 75-79.
Dunn DT, Newell ML, Ades AE, Peckham CS: Risk of human immunodeficiency virus type 1 transmission through breastfeeding. Lancet. 1992, 340: 585-588. 10.1016/0140-6736(92)92115-V.
Read JS: Human milk, breastfeeding, and transmission of human immunodeficiency virus type 1 in the United States. American Academy of Pediatrics Committee on Pediatric AIDS. Pediatrics. 2003, 112: 1196-1205.
Van de Perre P., Simonon, A., Hitimana, D.G., Dabis, F., Msellati, P., Mukamabano, B., Butera, J-B., Van Goethem, C., Karita, E., and Lepage, P.: Infective and anti-infective properties of breast milk from HIV-1-infected women. Lancet. 1993, 341: 914-918. 10.1016/0140-6736(93)91210-D.
Hocini H, Becquart P, Bouhlal H, Adle-Biassette H, Kazatchkine MD, Belec L: Secretory leukocyte protease inhibitor inhibits infection of monocytes and lymphocytes with human immunodeficiency virus type 1 but does not interfere with transcytosis of cell-associated virus across tight epithelial barriers. Clin Diagn Lab Immunol. 2000, 7: 515-518. 10.1128/CDLI.7.3.515-518.2000.
Swart PJ, Kuipers ME, Smit C, Pauwels R, deBethune MP, de Clercq E, Meijer DK, Huisman JG: Antiviral effects of milk proteins: acylation results in polyanionic compounds with potent activity against human immunodeficiency virus types 1 and 2 in vitro. AIDS Res Hum Retroviruses. 1996, 12: 769-775.
Harmsen MC, Swart PJ, de Bethune MP, Pauwels R, De Clercq E, The TH, Meijer DK: Antiviral effects of plasma and milk proteins: lactoferrin shows potent activity against both human immunodeficiency virus and human cytomegalovirus replication in vitro. J Infect Dis. 1995, 172: 380-388.
Semba RD: Mastitis and transmission of human immunodeficiency virus through breast milk. Ann N Y Acad Sci. 2000, 918: 156-162.
Embree JE, Njenga S, Datta P, Nagelkerke NJ, Ndinya-Achola JO, Mohammed Z, Ramdahin S, Bwayo JJ, Plummer FA: Risk factors for postnatal mother-child transmission of HIV-1. Aids. 2000, 14: 2535-2541. 10.1097/00002030-200011100-00016.
Ekpini E.R., Wiktor, S.Z., Satten, G.A., Adjorlolo-Johnson, G.T., Sibailly, T.S., Ou, C-Y., Karon, J.M., Brattegaard, K., Whitaker, J.P., Gnaore, E., De Cock, K.M., and Greenberg, A.E.: Late postnatal mother-to-child transmission of HIV-1 in Abidjan, Cote d’Ivoire. Lancet. 1997, 1054-1059. 10.1016/S0140-6736(96)06444-6.
de Martino M, Tovo PA, Tozzi AE, Pezzotti P, Galli L, Livadiotti S, Caselli D, Massironi E, Ruga E, Fioredda F, et al.: HIV-1 transmission through breast-milk: appraisal of risk according to duration of feeding. Aids. 1992, 6: 991-997.
Miotti PG, Taha TE, Kumwenda NI, Broadhead R, Mtimavalye LA, Van der Hoeven L, Chiphangwi JD, Liomba G, Biggar RJ: HIV transmission through breastfeeding: a study in Malawi. Jama. 1999, 282: 744-749. 10.1001/jama.282.8.744.
Bobat R, Moodley D, Coutsoudis A, Coovadia H: Breastfeeding by HIV-1-infected women and outcome in their infants: a cohort study from Durban, South Africa. Aids. 1997, 11: 1627-1633. 10.1097/00002030-199713000-00012.
Pillay K, Coutsoudis A, York D, Kuhn L, Coovadia HM: Cell-free virus in breast milk of HIV-1-seropositive women. J Acquir Immune Defic Syndr. 2000, 24: 330-336.
Semba RD, Kumwenda N, Hoover DR, Taha TE, Quinn TC, Mtimavalye L, Biggar RJ, Broadhead R, Miotti PG, Sokoll LJ, van der Hoeven L, Chiphangwi JD: Human immunodeficiency virus load in breast milk, mastitis, and mother-to-child transmission of human immunodeficiency virus type 1. J Infect Dis. 1999, 180: 93-98. 10.1086/314854.
Richardson BA, John-Stewart GC, Hughes JP, Nduati R, Mbori-Ngacha D, Overbaugh J, Kreiss JK: Breast-milk infectivity in human immunodeficiency virus type 1-infected mothers. J Infect Dis. 2003, 187: 736-740. 10.1086/374272.
Ioannidis JP, Abrams EJ, Ammann A, Bulterys M, Goedert JJ, Gray L, Korber BT, Mayaux MJ, Mofenson LM, Newell ML, Shapiro DE, Teglas JP, Wilfert CM: Perinatal transmission of human immunodeficiency virus type 1 by pregnant women with RNA virus loads <1000 copies/ml. J Infect Dis. 2001, 183: 539-545. 10.1086/318530.
Euorpean_Collaborative_Study: Maternal viral load and vertical transmission of HIV-1: an important factor but not the only one. European Collaborative Study. Aids. 1999, 13: 1377-1385. 10.1097/00002030-199907300-00016.
John GC, Nduati RW, Mbori-Ngacha DA, Richardson BA, Panteleeff D, Mwatha A, Overbaugh J, Bwayo J, Ndinya-Achola JO, Kreiss JK: Correlates of mother-to-child human immunodeficiency virus type 1 (HIV-1) transmission: association with maternal plasma HIV-1 RNA load, genital HIV-1 DNA shedding, and breast infections. J Infect Dis. 2001, 183: 206-212. 10.1086/317918.
Rousseau CM, Nduati RW, Richardson BA, Steele MS, John-Stewart GC, Mbori-Ngacha DA, Kreiss JK, Overbaugh J: Longitudinal analysis of human immunodeficiency virus type 1 RNA in breast milk and of its relationship to infant infection and maternal disease. J Infect Dis. 2003, 187: 741-747. 10.1086/374273.
Hirsch VM, Johnson PR: Pathogenic diversity of simian immunodeficiency viruses. Virus Res. 1994, 32: 183-203. 10.1016/0168-1702(94)90041-8.
Amedee AM, Lacour N, Ratterree M: Mother-to-infant transmission of SIV via breast-feeding in rhesus macaques. J Med Primatol. 2003, 32: 187-193. 10.1034/j.1600-0684.2003.00024.x.
Murphey-Corb M., Martin, L.N., Rangan, S.R.S., Baskin, G.B., Gormus, B.J., Wolf, R.H., Andes, W.A., West, M., and Montelaro, R.C.: Isolation of an HTLV-III related retrovirus from macaques with simian AIDS and its possible origin in asymptomatic mangabeys. Nature. 1986, 435-437.
Martin L. N., M. Murphey-Corb, K. F. Soike, B. Davison-Fairburn, and G. B. Baskin.: Effects of initiation of 3'-azido,3'-deoxythymidine (zidovudine) treatment at different times after infection of rhesus monkeys with simian immunodeficiency virus. Journal of Infectious Diseases. 1993, 825-
Becquart P, Hocini H, Levy M, Sepou A, Kazatchkine MD, Belec L: Secretory anti-human immunodeficiency virus (HIV) antibodies in colostrum and breast milk are not a major determinant of the protection of early postnatal transmission of HIV. J Infect Dis. 2000, 181: 532-539. 10.1086/315255.
Van de Perre P: Breast milk transmission of HIV-1. Laboratory and clinical studies. Ann N Y Acad Sci. 2000, 918: 122-127.
Duprat C., Mohammed, Z., Dtta, P., Stackiw, W., Ndinya-Achola, J.O., Kreiss, J.K., Holmes, K.K., Plummer, F.A., and Embree, J.E.: Human immunodeficiency virus type 1 IgA antibody in breast milk and serum. Pediatr Infect Dis J. 1994, 603-608.
Belec L, Dupre T, Prazuck T, Tevi-Benissan C, Kanga JM, Pathey O, Lu XS, Pillot J: Cervicovaginal overproduction of specific IgG to human immunodeficiency virus (HIV) contrasts with normal or impaired IgA local response in HIV infection. J Infect Dis. 1995, 172: 691-697.
Lu FX: Predominate HIV1-specific IgG activity in various mucosal compartments of HIV1-infected individuals. Clin Immunol. 2000, 97: 59-68. 10.1006/clim.2000.4910.
Fawzi W, Msamanga G, Spiegelman D, Renjifo B, Bang H, Kapiga S, Coley J, Hertzmark E, Essex M, Hunter D: Transmission of HIV-1 through breastfeeding among women in Dar es Salaam, Tanzania. J Acquir Immune Defic Syndr. 2002, 31: 331-338.
Hirsch VM, Santra S, Goldstein S, Plishka R, Buckler-White A, Seth A, Ourmanov I, Brown CR, Engle R, Montefiori D, Glowczwskie J, Kunstman K, Wolinsky S, Letvin NL: Immune failure in the absence of profound CD4+ T-lymphocyte depletion in simian immunodeficiency virus-infected rapid progressor macaques. J Virol. 2004, 78: 275-284. 10.1128/JVI.78.1.275-284.2004.
Orandle MS, Williams KC, MacLean AG, Westmoreland SV, Lackner AA: Macaques with rapid disease progression and simian immunodeficiency virus encephalitis have a unique cytokine profile in peripheral lymphoid tissues. J Virol. 2001, 75: 4448-4452. 10.1128/JVI.75.9.4448-4452.2001.
Zhang J-Y., Martin, L.N., Watson, E.A., Montelaro, R.C., West, M., Epstein, L., and Murphey-Corb, M.: Simian immunodeficiency virus/Delta-induced immunodeficiency disease in rhesus monkeys: Relationship of antibody response and antigenemia. J Infect Dis. 1988, 158: 1277-1286.
Kourtis AP, Butera S, Ibegbu C, Beled L, Duerr A: Breast milk and HIV-1: vector of transmission or vehicle of protection?. Lancet Infect Dis. 2003, 3: 786-793. 10.1016/S1473-3099(03)00832-6.
Farquhar C, VanCott TC, Mbori-Ngacha DA, Horani L, Bosire RK, Kreiss JK, Richardson BA, John-Stewart GC: Salivary secretory leukocyte protease inhibitor is associated with reduced transmission of human immunodeficiency virus type 1 through breast milk. J Infect Dis. 2002, 186: 1173-1176. 10.1086/343805.
Becquart P, Chomont N, Roques P, Ayouba A, Kazatchkine MD, Belec L, Hocini H: Compartmentalization of HIV-1 between breast milk and blood of HIV-infected mothers. Virology. 2002, 300: 109-117. 10.1006/viro.2002.1537.
Amedee A.M., Lacour, N., Gierman, J.L., Martin, L.N., Clements, J.E., Bohm, Jr., R.B., Harrison, R., and Murphey-Corb, M.: Genotypic Selection of Simian Immunodeficiency Virus (SIV) in Macaque Infants Infected Transplacentally. J Virol. 1995, 69: 7982-7990.
National-Research-Council: Guide for the care and use of laboratory animals. Edited by: National Research Council. 1996, Washington, D.C., National Academiy of Sciences
Fuller DH, Rajakumar PA, Wilson LA, Trichel AM, Fuller JT, Shipley T, Wu MS, Weis K, Rinaldo CR, Haynes JR, Murphey-Corb M: Induction of mucosal protection against primary, heterologous simian immunodeficiency virus by a DNA vaccine. J Virol. 2002, 76: 3309-3317. 10.1128/JVI.76.7.3309-3317.2002.
Tryphonas H, Karpinski K, O'Grady L, Hayward S: Quantitation of serum immunoglobulins G, M, and A in the rhesus monkey (M. mulatta) using human monospecific antisera in the enzyme-linked immunosorbent assay: developmental aspects. J Med Primatol. 1991, 20: 58-66.
Acknowledgements
We thank Richard Martin and Victoria Williams for technical work and Tara Randolph and William Gallaher for helpful discussions. This work was supported by NIH/NIDCR R01 DE12916 and NIH/NCRR P51 RR00164-39. The following reagent was obtained through the AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH: SIVmac239 gp130 from Quality Biologicals, Gaithersburg, MD.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
AMA conceived and designed the study, supervised all technical work, analysed and compiled data, and drafted the manuscript. JR performed the antibody titers, analysed data and helped draft the manuscript. NL performed diagnostic PCR, designed and performed viral quantitation assays and participated in the design of the study. LF coordinated blood and milk sample collection and processing, and participated in the design of the study. MR participated in the design of the study and was responsible for clinical care of all animals and sample collection procedures. All authors read and approved the final manuscript.
Competing interests
None declared.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Amedee, A.M., Rychert, J., Lacour, N. et al. Viral and immunological factors associated with breast milk transmission of SIV in rhesus macaques. Retrovirology 1, 17 (2004). https://doi.org/10.1186/1742-4690-1-17
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1742-4690-1-17